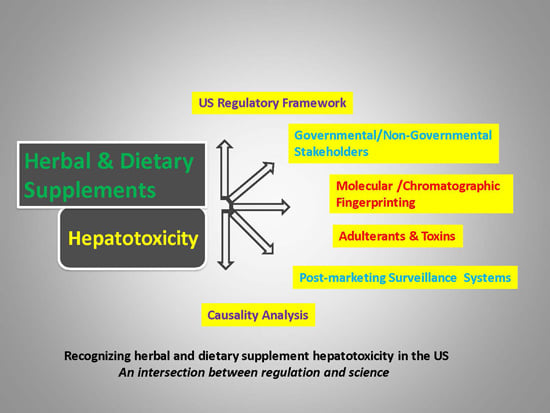
Scientific and Regulatory Perspectives in Herbal and Dietary Supplement Associated Hepatotoxicity in the United States
Abstract
:1. Introduction
Global Challenges in Evaluating Herbal Product Risk for Liver Toxicity
2. Trends of Dietary Supplement Use in the US
3. Regulatory History and Framework for the Legal Marketing of Herbals and Dietary Supplements in the US
3.1. Laws, Guidance and Regulatory Framework
3.2. Path for Approval of Herbal Products by the FDA
4. Manufacturing Dietary Supplements
5. Methods Supporting Dietary Supplement Safety
6. Organizations Inside and Outside of the US Government Who Regulate, Track and/or Scientifically Analyze the Influence of Dietary Supplements in the United States
6.1. Other US Government Organizations
6.1.1. FDA Center for Drug Evaluation and Research (CDER)
6.1.2. US Department of Agriculture’s Agricultural Research Service (USDA/ARS)
6.1.3. National Toxicology Program (NTP)/National Institute of Environmental Health Sciences (NIEHS)
6.1.4. US Federal Trade Commission (FTC)
6.1.5. NIH Office of Dietary Supplements (ODS)
6.1.6. NIH Center for Complementary and Integrative Health (NCCIH)
6.1.7. Environmental Protection Agency (EPA)
6.1.8. US Customs and Border Protection
6.1.9. US Government Accountability Office (GAO)
6.2. Non-Government Organizations
6.2.1. Dietary Supplement Manufacturers and the Food Industry:
6.2.2. US Pharmacopoeia (USP)
6.2.3. Academic Centers and Projects that Study Pharmacognosy and Drug Safety [61]
7. Pre-Clinical Assessment
8. Utility and Limitations of Clinical Trials
9. Characterization of HDS Product Chemical Content
10. In Silico Modeling of Drugs and Other Agents that Cause Idiosyncratic Hepatotoxicity
11. Post-marketing Assessment of Herbal Hepatotoxicity
Surveillance Databases and Tools
12. Challenges in Assessing Suspected Herbal Hepatotoxicity
13. Causality Assessment
13.1. Liver Toxins
13.2. Drug Adulterants with Known or Possible Hepatotoxic Profiles
14. FDA Regulatory Actions for Hepatotoxic Supplements: Anecdotal Examples and Experience
14.1. Lipokinetix (Usnic Acid)
14.2. OxyELITE Pro
14.3. Hydroxycut
14.4. Designer Steroids
15. Global Regulation of Herbals and Dietary Supplements
16. Enhancing Research in the Evaluation and Management of Herbal Hepatotoxicity: Future Directions
Acknowledgments
Conflicts of Interest
Disclaimer
References
- Zheng, E.X.; Navarro, V.J. Liver injury from herbal, dietary, and weight loss supplements: A review. J. Clin. Transl. Hepatol. 2015, 3, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Stickel, F.; Kessebohm, K.; Weimann, R.; Seitz, H.K. Review of liver injury associated with dietary supplements. Liver Int. 2011, 31, 595–605. [Google Scholar] [CrossRef] [PubMed]
- Seeff, L.B.; Bonkovsky, H.L.; Navarro, V.J.; Wang, G. Herbal products and the liver: A review of adverse effects and mechanisms. Gastroenterology 2015, 148, 517–532. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, D.M.; Kessler, R.C.; Foster, C.; Norlock, F.E.; Calkins, D.R.; Delbanco, T.L. Unconventional medicine in the United States: Prevalence, costs, and patterns of use. N. Engl. J. Med. 1993, 328, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Davis, B.; Foster, D.F.; van Rompay, M.I.; Walters, E.E.; Wilkey, S.A.; Kaptchuk, T.J.; Eisenberg, D.M. Long-term trends in the use of complementary and alternative medical therapies in the United States. Ann. Intern. Med. 2001, 135, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, D.M.; Davis, R.B.; Ettner, S.L.; Appel, S.; Wilkey, S.; van Rompay, M.; Kessler, R.C. Trends in alternative medicine use in the United States, 1990–1997: Results of a follow-up national study. JAMA 1998, 280, 1569–1575. [Google Scholar] [CrossRef] [PubMed]
- Fontana, R.J.; Watkins, P.B.; Bonkovsky, H.L.; Chalasani, N.; Davern, T.; Serrano, J.; Rochon, J.; DILIN Study Group. Drug-induced Liver Injury Network (DILIN) prospective study: Rationale, design and conduct. Drug Saf. 2009, 32, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Navarro, V.J.; Barnhart, H.; Bonkovsky, H.L.; Davern, T.; Fontana, R.J.; Grant, L.; Reddy, K.R.; Seeff, L.B.; Serrano, J.; Sherker, A.H.; et al. Liver injury from herbals and dietary supplements in the U.S. Drug-Induced Liver Injury Network. Hepatology 2014, 60, 1399–1408. [Google Scholar] [CrossRef] [PubMed]
- Van Breemen, R.B. Development of safe and effective botanical supplements. J. Med. Chem. 2015, 58, 8360–8372. [Google Scholar] [CrossRef] [PubMed]
- Finley, J.W.; Finley, J.W.; Ellwood, K.; Hoadley, J. Launching a new food product or dietary supplement in the United States: Industrial, regulatory and nutritional considerations. Annu. Rev. Nutr. 2014, 34, 421–447. [Google Scholar] [CrossRef] [PubMed]
- Bauer, R.; Tittel, G. Quality assessment of herbal preparations as precondition of pharmacological and clinical studies. Phytomedicine 1996, 2, 193–198. [Google Scholar] [CrossRef]
- Saper, R.B.; Phillips, R.S.; Sehgal, A.; Khouri, N.; Davis, R.B.; Paquin, J.; Thuppil, V.; Kales, S.N. Lead, mercury, and arsenic in US- and Indian-manufactured Ayurvedic medicines sold over the internet. JAMA 2008, 300, 915–923. [Google Scholar] [CrossRef] [PubMed]
- Ernst, E. Heavy metals in traditional Indian remedies. Eur. J. Clin. Pharmacol. 2002, 57, 891–896. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.K.; Tan, P.; Wee, Y.C. Heavy metals in some Chinese herbal plants. Biol. Trace Elem. Res. 1993, 36, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Van der Voet, G.B.; Sarafanov, A.; Todorov, T.I.; Centeno, J.A.; Jonas, W.B.; Ives, J.A.; Mullick, F.G. Clinical and analytic toxicology of dietary supplements: A case study and review of the literature. Biol. Trace Element Res. 2008, 125, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Stickel, F.; Droz, S.; Patsenker, E.; Bögli-Stuber, K.; Aebi, B.; Leib, S.L. Severe hepatotoxicity following ingestion of Herbalife contaminated with Bacillus subtilis. J. Hepatol. 2009, 50, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Miller, G.M.; Stripp, R. A study of western pharmaceuticals contained within samples of Chinese herbal/patent medicines collected from New York City’s Chinatown. Leg. Med. 2007, 9, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, B.; Ashig, S.; Hussain, A.; Bashir, S.; Hussain, M. Evaluation of mycotoxins, mycobiota, and toxigenic fungi in selected medicinal plants of Khyber Pakhtunkhwa, Pakistan. Fungal Biol. 2014, 118, 776–784. [Google Scholar] [CrossRef] [PubMed]
- Veprikova, Z.; Zachriasova, M.; Dzuman, Z.; Zachariasova, A.; Fenclova, M.; Slavikova, P.; Vaclavikova, M.; Mastovska, K.; Hengst, D.; Hajslova, J. Mycotoxins in plant-based dietary supplements: Hidden health risk for consumers. J. Agric. Food Chem. 2015, 63, 6633–6643. [Google Scholar] [CrossRef] [PubMed]
- Harris, E.S.; Cao, S.; Littlefield, B.A.; Craycroft, J.A.; Scholten, R.; Kaptchuk, T.; Fu, Y.; Wang, W.; Liu, Y.; Chen, H.; et al. Heavy metal and pesticide content in commonly prescribed individual raw Chinese herbal medicines. Sci. Total Environ. 2011, 409, 4297–4305. [Google Scholar] [CrossRef] [PubMed]
- Efferth, T.; Kaina, B. Toxicities by herbal medicines with emphasis to traditional Chinese medicine. Curr. Drug Metab. 2011, 12, 989–996. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). National Policy on Traditional Medicine and Regulation of Herbal Medicines; Report of WHO Global Survey; WHO: Geneva, Switzerland, 2005. [Google Scholar]
- Mou, X.; Kesari, S.; Wen, P.Y.; Huang, X. Crude drugs as anticancer agents. Int. J. Clin. Med. 2011, 4, 17–25. [Google Scholar]
- Gurley, B.J.; Gardner, S.F.; Hubbard, M.A. Content versus label claims in ephedra-containing dietary supplements. Am. J. Health Syst. Pharm. 2000, 57, 963–969. [Google Scholar] [PubMed]
- Harkey, M.R.; Henderson, G.L.; Gershwin, M.E.; Stern, J.S.; Hackman, R.M. Variability in commercial ginseng products: An analysis of 25 preparations. Am. J. Clin. Nutr. 2001, 73, 1101–1106. [Google Scholar] [PubMed]
- Morris, C.A.; Avorn, J. Internet marketing of herbal products. JAMA 2003, 290, 1505–1509. [Google Scholar] [CrossRef] [PubMed]
- Green, G.A.; Catlin, D.H.; Starcevic, B. Analysis of over-the-counter dietary supplements. Clin. J. Sport Med. 2001, 11, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Newmaster, S.G.; Grguric, M.; Shanmughanandhan, D.; Ramalingam, S.; Ragupathy, S. DNA barcoding detects contamination and substitution in North American herbal products. BMC Med. 2013, 11. [Google Scholar] [CrossRef] [PubMed]
- Ervin, R.B.; Wright, J.D.; Kennedy-Stephenson, J. Use of dietary supplements in the United States, 1988–1994. Vital Health Stat. 1999, 11, 1–4. [Google Scholar]
- Gahche, J.; Bailey, R.; Burt, V.; Hughes, J.; Yetley, E.; Dwyer, J.; Picciano, M.F.; McDowell, M.; Sempos, C. Dietary supplement use among US adults has increased since NHANES III (1984–1994). NCHS Data Brief 2011, 61, 1–8. [Google Scholar] [PubMed]
- Ni, H.; Simile, C.; Hardy, A.M. Utilization of complementary and alternative medicine by United States adults: Results from the 1999 national health interview survey. Med. Care 2002, 40, 333–358. [Google Scholar] [CrossRef]
- Kennedy, J. Herb and supplement use in the US adult population. Clin. Ther. 2005, 27, 1847–1858. [Google Scholar] [CrossRef] [PubMed]
- Timbo, B.B.; Ros, M.O.P.P.; McCarthy, P.V.; Lin, C.T. Dietary supplements in a national survey: Prevalence of use and reports of adverse events. J. Am. Diet. Assoc. 2006, 106, 1966–1974. [Google Scholar] [CrossRef] [PubMed]
- Nahin, R.L.; Barnes, P.M.; Stussman, B.J.; Bloom, B. Costs of Complementary and Alternative Medicine (CAM) and Frequency of CAM Visits by CAM Practitioners: United States 2002; National Health Statistic Report: No. 18; National Center for Health Statistics: Hyatsville, MD, USA, 2009. [Google Scholar]
- Lindstrom, A.; Ooyen, C.; Lynch, E.L.; Blumenthal, M.; Kawa, K. Sales of herbal dietary supplements increase by 7.9% in 2013. Marking a decade of rising sales. HerbalGram 2014, 103, 52–56. [Google Scholar]
- Bailey, R.L.; Gahche, J.J.; Miller, P.E.; Thomas, P.R.; Dwyer, J.T. Why US adults use dietary supplements. JAMA Intern. Med. 2013, 173, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Farina, E.K.; Austin, K.G.; Lieberman, H.R. Concomitant dietary supplement and prescription medication use is prevalent among US adults with doctor-informed medical conditions. J. Acad. Nutr. Diet. 2014, 114, 1784–1790. [Google Scholar] [CrossRef] [PubMed]
- Pereira, J.; Arkinson, J.; Li, K. Use of nonvitamin dietary supplements with prescription medications. Can. Fam. Physician 2008, 54, 1142–1144. [Google Scholar] [PubMed]
- Jacobson, I.G.; Horton, J.L.; Smith, B.; Wells, T.S.; Boyko, E.J.; Lieberman, H.R.; Ryan, M.A.; Smith, T.C.; Millenium Cohort Study Team. Bodybuilding, energy, and weight-loss supplements are associated with deployment and physical activity in US military personnel. AEP 2012, 22, 318–330. [Google Scholar] [PubMed]
- Marriott, B.M.; Goertz Choate, C.; Hourani, L.; Bray, R.B. Reported Use of Dietary Supplements in the Last 12 Months among US Active Duty Military Personnel in Four Services Worldwide; The National Academies Press: Washington, DC, USA, 2008. [Google Scholar]
- Hu, Z.; Yang, X.; Ho, P.C.; Chan, S.Y.; Heng, P.W.; Chan, E.; Duan, W.; Koh, H.L.; Zhou, S. Herb-drug interaction: A literature review. Drugs 2005, 65, 1239–1282. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.W.; Sneed, K.B.; Pan, S.Y.; Cao, C.; Kanwar, J.R.; Chew, H.; Zhou, F. Herb-drug interactions and mechanistic and clinical considerations. Curr. Drug Metab. 2012, 13, 640–651. [Google Scholar] [CrossRef] [PubMed]
- Junod, S.W. FDA and Clinical Drug Trials: A Short History. Available online: http://www.fda.gov/AboutFDA/WhatWeDo/History/Overviews/ucm304485.htm (accessed on 24 February 2016).
- US Food and Drug Administration. Dietary Supplement Health and Education Act of 1994; Public Law 103–417; US Food and Drug Administration: Silver Spring, MD, USA, 1994.
- Dietary Supplement and Non-Prescription Drug Act; Public Law 109–462; United States Government Printing Office: Washington, DC, USA, 2006.
- Current Good Manufacturing Practice in Manufacturing, Packaging, Labeling, or Holding Operations for Dietary Supplements: Final Rule. Available online: http://www.gpo.gov/fdsys/pkg/FR-2007-06-25/html/07-3039.htm (accessed on 6 January 2016).
- Petrovska, B.B. Historical review of medicinal plants usage. Pharmacovn. Rev. 2012, 6, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Pan, S.Y.; Litscher, G.; Gao, S.H.; Zhou, S.F.; Yu, Z.L.; Chen, H.Q.; Zhang, S.F.; Tang, M.K.; Sun, J.N.; Ko, K.M. Historical perspective of traditional indigenous medical practices: The current renaissance and conservation of herbal resources. Evid. Based Complement. Altern. Med. 2014, 2014, 525340. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.T.; Dou, J.; Temple, R.; Agarwal, R.; Wu, K.M.; Walker, S. New therapies for old medicines. Nat. Biotechnol. 2008, 26, 1077–1083. [Google Scholar] [CrossRef] [PubMed]
- Newman, D.J.; Cragg, G.M. Natural products a source of new drugs over the 30 years from 1981 to 2010. J. Nat. Prod. 2012, 75, 311–325. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.L.; Dou, J.; Agarwal, R.; Beitz, J.; Wu, C.; Mulberg, A.; Yu, L.X.; Woodcock, J. Evolution of traditional medicines to botanical drugs. Science 2015, 347 (Suppl. 6219), S32–S34. [Google Scholar]
- FDA Guidance for Industry-Botanical Drug Products. Available online: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm070491.pdf (accessed on 6 January 2016).
- US EPA Office of Pesticide Programs. Index to Pesticide types and Families and Parts 180 Tolerance Information of Pesticide Chemicals in Food and Feed Commodities, 2014. Available online: http://www.epa.gov/sites/production/files/2015-01/documents/pesticide-types.pdf (accessed on 7 January 2016).
- Chemical Contaminants, Metals, Natural Toxins & Pesticides Guidance Documents & Regulation. Available online: http://www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/ChemicalContaminantsMetalsNaturalToxinsPesticides/default.htm (accessed on 7 January 2016).
- Institute of Medicine, National Academy of Sciences. Dietary References intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Bioton, and Choline; National Academy Press: Washington, DC, USA, 1998. [Google Scholar]
- Whitton, P.A.; Lau, A.; Salisbury, A.; Whitehouse, J.; Evans, C.S. Kava lactones and the Kava–Kava controversy. Phytochemistry 2003, 64, 673–679. [Google Scholar] [CrossRef]
- Russman, S.; Lauterburg, B.H.; Helbing, A. Kava hepatotoxicity. Ann. Intern. Med. 2001, 135, 68–69. [Google Scholar] [CrossRef]
- Stickel, F.; Baumuller, H.M.; Seitz, K.H.; Vasilakis, D.; Seitz, G.; Seitz, H.K.; Schuppan, D. XHepatitis induced by Kava–Kava (Piper methysticum rhizoma). J. Hepatol. 2003, 39, 62–67. [Google Scholar] [CrossRef]
- Federal Food, Drug, and Cosmetic Act, 21 U.S.C. 301. Available online: https://www.gpo.gov/fdsys/pkg/USCODE-2011-title21/pdf/USCODE-2011-title21-chap9.pdf (accessed on 4 January 2016).
- US Government Accountability Office. Herbal Dietary Supplements: Examples of Deceptive or Questionable Marketing Practices and Potentially Dangerous Advice. Available online: http://www.gao.gov/products/GAO-10-662C (accessed on 4 January 2016).
- De Pasquale, A. Pharmacognosy: The oldest modern science. J. Ethnopharmacol. 1984, 11, 1–16. [Google Scholar] [CrossRef]
- Czeczot, H.; Tudek, B.; Kusztelak, J.; Sczymczk, T.; Dobrowolska, B.; Glinkowska, G.; Malinowski, J.; Strzelecka, H. Isolation and studies of the mutagenic activity in the Ames test of flavonoids naturally occurring in medical herbs. Mutat. Res. 1990, 240, 209–216. [Google Scholar] [CrossRef]
- Seeff, L.B. Drug-induced liver injury is a major risk for new drugs. Dig. Dis. Sci. 2015, 33, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Senior, J.R. Evolution of the Food and Drug Administration to liver assessment of new drugs: Current status and challenges. Drug Saf. 2014, 37 (Suppl. 1), S9–S17. [Google Scholar] [CrossRef] [PubMed]
- Avigan, M.I. “Regulatory Perspectives” in Drug-Induced Liver Injury, 3rd ed.; Kaplowitz, N., DeLeve, L.D., Eds.; Academic Press: Cambridge, MA, USA, 2013; pp. 689–712. [Google Scholar]
- FDA Guidance for Industry-Drug-Induced Liver Injury: Premarketing Clinical Evaluation. July 2009. Available online: http://www.fda.gov/downloads/Drugs/Guidelines/ucm174090.pdf (accessed on 4 January 2016).
- Temple, R. Hy’s law: Predicting serious hepatotoxicity. Pharmacoepidemiol. Drug Saf. 2006, 15, 241–243. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, H.J. The spectrum of hepatotoxicity (Kober Lecture 1966). Perspect. Biol. Med. 1968, 12, 135–161. [Google Scholar] [CrossRef] [PubMed]
- Rosner, B. The binomial distribution. In Fundamentals of Biostatistics; Rosner, B., Ed.; Duxbury Press: Belmont, CA, USA, 1995; pp. 82–85. [Google Scholar]
- ClinicalTrials.gov.: A service of the US National Institutes of Health. Available online: https://clinicaltrials.gov (accessed on 4 January 2016).
- Naser, B.; Schnitker, J.; Minkin, M.J.; de Arriba, S.G.; Nolte, K.U.; Osmers, R. Suspected black cohosh hepatotoxicity: No evidence by meta-analysis of randomized controlled clinical trials for isopropanolic black cohosh extract. Menopause 2011, 18, 366–375. [Google Scholar] [CrossRef] [PubMed]
- Vaclavik, L.; Krynitsky, A.J.; Rader, J.L. Mass spectrometric analysis of pharmaceutical adulterants in foodstuffs labeled as botanical dietary supplements or herbal remedies. Anal. Bioanal. Chem. 2014, 406, 6767–6790. [Google Scholar] [CrossRef] [PubMed]
- NCCIH Policy: Natural Product Integrity. Available online: https://nccih.nih.gov/research/policies/naturalproduct.htm (accessed on 10 November 2015).
- USP Verified Dietary Supplements. Available online: http://www.usp.org/usp-verification-services/usp-verified-dietary-supplements (accessed on 4 January 2016).
- Heubl, G. New aspects of DNA-based authentication of Chinese medicinal plants by molecular biological techniques. Planta Med. 2011, 77, 1963–1974. [Google Scholar] [CrossRef] [PubMed]
- Reich, E.; Shibli, A. Validation of high-performance thin layer chromatographic methods for the identification of botanicals in a c-GMP environment. JAOAC 2008, 91, 13–20. [Google Scholar]
- Zhao, J.; Avula, B. NMR fingerprinting for analysis of hoodia species and hoodia dietary products. Planta Med. 2011, 77, 852–857. [Google Scholar] [CrossRef] [PubMed]
- Przybylak, K.R.; Cronin, M.T. In silico models for drug-induced liver injury—Current status. Expert Opin. Drug Metab. Toxicol. 2012, 8, 201–217. [Google Scholar] [CrossRef] [PubMed]
- 21 U.S.C. 379-aa-1 Serious Adverse Event Reporting for Dietary Supplements. Available online: https://www.gpo.gov/fdsys/pkg/USCODE-2011-title21/pdf/USCODE-2011-title21-chap9.pdf (accessed on 4 January 2016).
- Questions and Answers on FDA’s Adverse Event Reporting System (FAERS). Available online: http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Surveillance/AdverseDrugEffects/ (accessed on 4 January 2016).
- Agarwal, V.; McHutchison, J.G.; Hoofnagle, J.H.; Drug-induced Lver Injury Network. Important Elements for the Diagnosis of Drug-induced Liver Injury. Clin. Gastroenterol. Hepatol. 2010, 8, 463–470. [Google Scholar] [CrossRef] [PubMed]
- American Herbal Products Association (AHPA) New Dietary Ingredient Database. Available online: http://www.ahpa.org/Default.asps?tabid=558 (accessed on 15 August 2015).
- New York Times—New York Attorney General Targets Supplements at Major Retailers, 3 February 2015. Available online: http://well.blogs.nytimes.com/2015/02/03/new-york-attorney-general-targets-supplements-at-major-retailers/ (accessed on 4 January 2016).
- Seeff, L.B.; Stickel, F.; Navarro, V. Hepatotoxicity of herbal and dietary supplements. In Drug-Induced Liver Disease, 3rd ed.; Kaplowitz, N., DeLeve, L., Eds.; Elsevier: Amsterdam, The Netherlands, 2013; pp. 631–657. [Google Scholar]
- Navarro, V.J.; Seeff, L.B. Liver injury induced by herbal complementary and alternative medicine. Clin. Liver Dis. 2013, 17, 715–735. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Zhang, L.; Long, H.; Schwarzenboeck, A.; Schmidt-Taenzer, W.; Genthner, A.; Wolff, A.; Frenzel, C.; Schulze, J.; Eickhoff, A. Traditional Chinese Medicine and herbal hepatotoxicity: A tabular compilation of reported cases. Ann. Hepatol. 2015, 14, 7–19. [Google Scholar] [PubMed]
- Wai, C.T.; Tan, B.H.; Chan, C.L.; Sutedja, D.S.; Lee, Y.M.; Khor, C.; Lim, S.G. Drug-induced liver injury at an Asian Center: A prospective study. Liver Int. 2007, 27, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Suk, K.T.; Kim, D.J.; Kim, C.H.; Park, S.H.; Yoon, J.H.; Kim, Y.S.; Kweon, Y.O.; Kim, B.I.; Kim, S.H.; Kim, I.H.; et al. A prospective nationwide study of drug-induced liver injury in Korea. Am. J. Gastroenterol. 2012, 107, 1380–1387. [Google Scholar] [CrossRef] [PubMed]
- Andrade, R.J.; Lucena, M.I.; Fernandez, M.C.; Palaez, G.; Pachkoria, K.; Garcia-Ruiz, B.; Garcia-Munoz, B.; Gonzalez-Grande, R.; Pizarro, A.; Duran, J.A.; et al. Drug-induced liver injury: An analysis of 461 incidences submitted to the Spanish registry over a 10-year period. Gastroenterology 2005, 129, 512–521. [Google Scholar] [CrossRef] [PubMed]
- De Valle, M.B.; Av Klinteberg, V.; Alem, N.; Olsson, R.; Bjornsson, E. Drug-induced liver injury in a Swedish university hospital out-patient hepatology clinic. Aliment. Pharmacol. Ther. 2006, 24, 1187–1195. [Google Scholar] [CrossRef] [PubMed]
- Bjornsson, E.D.; Bergmann, O.M.; Bjornsson, H.K.; Kvaran, R.B.; Olafsson, S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroentereology 2013, 144, 1410–1425. [Google Scholar] [CrossRef] [PubMed]
- Yuan, L.; Kaplowitz, N. Mechanisms of drug-induced liver injury. Clin. Liver Dis. 2013, 17, 507–518. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Colegate, S.M.; Edgar, J.A. Safety assessment of food and herbal products containing hepatotoxic pyrrolizidine alkaloids: Interlaboratory consistency and the importance of N-oxide determination. Phytochem. Anal. 2008, 19, 526–533. [Google Scholar] [CrossRef] [PubMed]
- Bras, G.; Jeliffe, D.B.; Stuart, K.L. Venoocclusive disease of the liver with non-portal type of cirrhosis occurring in Jamaica. Arch. Pathol. 1954, 57, 285–300. [Google Scholar]
- Datta, D.V.; Khuroo, M.S.; Mattocks, A.R.; Aikat, B.K.; Chhuttani, P.N. Herbal medicines and veno-occlusive disease in India. Postgrad. Med. J. 1978, 54, 511–515. [Google Scholar] [CrossRef] [PubMed]
- Kakar, F.; Akbarian, Z.; Leslie, T.; Mustafa, M.L.; Watson, J.; van Egmond, H.P.; Omar, M.F.; Mofleh, J. An outbreak of hepatic veno-occlusive disease in Western Afghanistan associated with exposure to wheat flour contaminated with pyrrolizidine alkaloids. J. Toxicol. 2010, 2010, 313280. [Google Scholar] [CrossRef] [PubMed]
- Stillman, A.E.; Huxtable, R.J.; Consroe, P.; Kohnen, P.; Smith, S. Hepatic venocclusive disease due to pyrrolizidine (Senecio) poisoning in Arizona. Gastroenterology 1977, 73, 349–352. [Google Scholar] [PubMed]
- DeLeve, L.D. Toxic injury to hepatic sinusoids: Sinusoidal obstruction syndrome (veno-occlusive disease). Semin. Liver Dis. 2002, 22, 27–42. [Google Scholar] [CrossRef] [PubMed]
- Lambert, J.D.; Kennett, M.J.; Sang, S.; Reuhl, K.R.; Ju, J.; Yang, C.S. Hepatotoxicity of high oral dose (−)-epigallocatechin-3-gallate in mice. Food Chem. Toxicol. 2010, 48, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Mazzanti, G.; Mennitti-Ippolito, F.; Moro, P.A.; Cassetti, F.; Raschetti, R.; Santuccio, C.; Mastrangelo, S. Hepatotoxicity from green tea: A review of the literature and two unpublished cases. Eur. J. Clin. Pharmacol. 2009, 65, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.S.; Beer, S.; Kearney, D.L.; Phillips, G.; Carter, B.A. Green tea extract: A potential case for liver failure. World J. Gastroenterol. 2013, 19, 5174–5177. [Google Scholar] [CrossRef] [PubMed]
- Navarro, V.J.; Bonkovsky, H.L.; Hwang, S.I.; Vega, M.; Barnhart, H.; Serrano, J. Catechins in dietary supplements and hepatotoxicity. Dig. Dis. Sci. 2013, 58, 2682–2690. [Google Scholar] [CrossRef] [PubMed]
- Fau, D.; Lekehal, M.; Farrell, G.; Morrau, A.; Moulis, C.; Feldmann, G.; Haouzi, D.; Pessayre, D. Diterpenoids from germander, an herbal medicine induces apoptosis in isolated rat hepatocytes. Gastroenterology 1997, 113, 1334–1346. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, N.M.; Philen, R.M.; Love, L.A. Chaparral-associated hepatotoxicity. Arch. Intern. Med. 1997, 157, 913–919. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, R.; Wang, Z.Y.; Bik, D.P.; Mukhtar, H. Nordihydroguaiaretic acid, an inhibitor of lipoxygenase, also inhibits cytochrome P-450-mediated monooxygenase activity in rat epidermal and hepatic microsomes. Drug Metab. Dispos. 1991, 19, 620–624. [Google Scholar] [PubMed]
- Georgiou, M.; Sianidou, L.; Hatzis, T.; Papadatos, J.; Koutselinis, M. Hepatotoxicity due to Atractylis gummifera-L. J. Toxicol. Clin. Toxicol. 1988, 28, 487–493. [Google Scholar] [CrossRef]
- Popat, A.; Shear, N.H.; Malkiewicz, I.; Stewrart, M.J.; Steenkamp, V.; Thomson, S.; Neuman, M.G. The toxicity of Callilepsis laureola, a South African traditional herbal medicine. Clin. Biochem. 2001, 34, 229–236. [Google Scholar] [CrossRef]
- Rider, C.V.; Carlin, D.J.; Devito, M.J.; Thompson, C.L.; Walker, N.J. Mixtures research at NIEHS: An evolving program. Toxicology 2013, 313, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Mahler, H.; Pasi, A.; Kramer, J.M.; Schulte, P.; Scoging, A.C.; Bar, W.; Krahenbuhl, S. Fulminant liver failure in association with the emetic toxin of Bacillus cereus. N. Engl. J. Med. 1997, 336, 1142–1148. [Google Scholar] [CrossRef] [PubMed]
- Tournas, V.H.; Sapp, C.; Trucksess, M.W. Occurrence of aflatoxins in milk thistle herbal supplements. Food Adult. Contam. A Chem. Anal. Control Expo. Risk Assess. 2012, 29, 994–999. [Google Scholar] [CrossRef] [PubMed]
- Probst, C.; Njapau, H.; Cotty, P.J. Outbreak of an acute aflotoxicosis in Kenya 2004: Identification of the causal agent. Appl. Environ. Microbiol. 2007, 73, 2762–2764. [Google Scholar] [CrossRef] [PubMed]
- Lye, M.S.; Ghazal, A.A.; Mohan, J.; Alwin, N.; Nair, R.C. An outbreak of acute encephalopathy due to severe aflotoxicosis in Malaysia. Am. J. Trop. Med. Hyg. 1995, 53, 68–72. [Google Scholar] [PubMed]
- Nogueira, L.; Foerster, C.; Groopman, J.; Egner, P.; Koshiol, J.; Ferreccio, C.; Gallbladder Cancer Working Group. Association of aflatoxin with gallbladder cancer in Chile. JAMA 2015, 313, 2075–2077. [Google Scholar] [CrossRef] [PubMed]
- Moudgil, V.; Redhu, D.; Dhanda, S.; Singh, J. A review of molecular mechanisms in the development of hepatocellular carcinoma by aflatoxin and hepatitis B and C viruses. J. Environ. Pathol. Toxicol. Oncol. 2013, 32, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Kew, M.C. Aflatoxins as a cause of hepatocellular carcinoma. J. Gastrointest. Liver Dis. 2013, 22, 305–310. [Google Scholar]
- Prado, G.; Altoe, A.F.; Gomes, T.C.; Leal, A.S.; Morais, V.A.; Oliveira, M.S.; Ferreira, M.B.; Gomes, M.B.; Paschoal, F.N.; Souza, R.V.; et al. Occurrence of aflotoxin B1 in natural products. Braz. J. Microbiol. 2012, 43, 1428–1436. [Google Scholar] [CrossRef] [PubMed]
- Felizardo, R.J.; Camara, N.O. Hepatocellular carcinoma and food contamination: Aflatoxins and ochratoxin A as a great prompter. World J. Gastroenterol. 2013, 19, 3723–3725. [Google Scholar] [CrossRef] [PubMed]
- Magnussen, A.; Parsi, M.A. Aflatoxins, hepatocellular carcinoma and public health. World J. Gastroenterol. 2013, 19, 1508–1512. [Google Scholar] [CrossRef] [PubMed]
- Justa Neves, D.B.; Caldas, E.D. Dietary supplements: International legal framework and adulteration profiles, and characteristics of products on the Brazilian clandestine market. Regul. Toxicol. Pharmacol. 2015, 73, 93–104. [Google Scholar] [CrossRef] [PubMed]
- Ulloa, J.; Sambrotta, L.; Redko, F.; Mazza, O.N.; Garrido, G.; Becher, E.F.; Muschietti, L. Detection of tadalafil analogue as an adulterant in a dietary supplement for erectile dysfunction. J. Sex. Med. 2015, 12, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Reeuwijk, N.M.; Venhuis, B.J.; de Kaste, D.; Hoogenboom, L.A.; Rietjens, I.M.; Martena, M.J. Sildenafil and analogous phosphdiesterase type 5 (PDE-5) inhibitors in herbal food supplements sampled on the Dutch market. Food Addit. Contam. A Chem. Anal. Control Expo. Risk Assess. 2013, 30, 2027–2034. [Google Scholar] [CrossRef] [PubMed]
- Damiano, F.; Silva, C.; Gregori, A.; Vacondio, F.; Mor, M.; Menozzi, M.; Di Giorgio, D. Analysis of illicit dietary supplements sold in the Italian market: Identification of a sildenafil thioderivative as adulterant using the UPLC-TOF/MS and GC/MS. Sci. Justice 2014, 54, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.H.; Park, H.J.; Lee, J.H.; Do, J.A.; Heo, S.; Jo, J.H.; Cho, S. Determination of anabolic androgenic steroids adulterants in counterfeit drugs by UHPLC-MS/MS. J. Pharm. Biomed. Anal. 2015, 111, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Cao, Y.; Cao, Y.; Chai, Y.; Lu, F. Rapid on-site TLC-SERS detection of four antidiabetes drugs used as adulterants in botanical dietary supplements. Anal. Bioanal. Chem. 2014, 406, 1877–1884. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; Shi, F.; Jiang, S.; Gong, L.; Zhao, Y.; Zhang, J.; Zeng, S. Simultaneous identification, confirmation and qualification of illegal adulterated antidiabetics in herbal medicines and dietary supplements using high resolution benchtop quadrupole‒Orbitrap mass spectrometry. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2014, 967, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Mathon, C.; Ankli, A.; Reich, E.; Bieri, S.; Christen, P. Screening and determination of sibutramine in adulterated herbal slimming supplements by HPTLC-UV densitometry. Food Addit. Contam. A Chem. Anal. Control Expo. Risk Assess. 2014, 31, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Chan, B.; Yao, S. Analysis of six synthetic adulterants in herbal weight-reducing dietary supplements by LC electrospray ionization-MS. Food Addit. Contam. A Chem. Anal. Control Expo. Risk Assess. 2008, 25, 822–830. [Google Scholar] [CrossRef] [PubMed]
- Campbell, N.; Clark, J.P.; Stecher, V.J.; Thomas, J.W.; Callanan, A.C.; Donnelly, B.F.; Goldstein, J.; Kaminetsky, J.C. Adulteration of purported herbal and natural sexual performance enhancement dietary supplements with synthetic phosphodiesterase type 5 inhibitors. J. Sex. Med. 2013, 10, 1842–1849. [Google Scholar] [CrossRef] [PubMed]
- Song, F.; El-Demerdash, A.; Lee, S.J. Screening for multiple phosphodiesterase type 5 inhibitor drugs in dietary supplement materials by flow injection mass spectrometry and their quantification by liquid chromatography tandem mass spectrometry. J. Pharm. Biomed. Anal. 2012, 70, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Roh, S.H.; Kang, Y.P.; Park, S.; Huh, Y.; Lee, J.; Park, J.H.; Kim, D.; Kwon, S.W. Determination of tadalafil and N-desmethylsibutramine in health and dietary supplement using ultra-performance liquid chromatography (UPLC) coupled with quadropole-time-of-flight mass spectrometry (Q-TOF MS). Food Addit. Contam. A Chem. Anal. Control Expo. Risk Assess. 2011, 28, 1475–1482. [Google Scholar] [CrossRef] [PubMed]
- Kesting, J.R.; Huang, J.; Sorenson, D. Identification of adulterants in Chinese herbal medicine by LC-HRMS and LC-MS-SPE/NMR and comparative in vivo study with standards in a hypertensive rat model. J. Pharm. Biomed. Anal. 2010, 51, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Ernst, E. Toxic heavy metals and undeclared drugs in Asian herbal remedies. Trends Pharmacol. Sci. 2002, 23, 136–139. [Google Scholar] [CrossRef]
- Dunn, J.D.; Gryniewicz-Ruzicka, C.M.; Manns, D.J.; Mecker-Pogue, L.C.; Kauffman, J.F.; Westenberger, B.J.; Buhse, L.F. Qualitative screening for adulterants in weight loss supplements by ion mobility spectrometry. J. Pharm. Biol. Anal. 2012, 71, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Ashiq, S.; Hussain, M.; Ahmad, B. Natural occurrence of mycotoxins in plants: A review. Fungal Genet. Biol. 2014, 66, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Mans, D.J.; Gucinski, A.C.; Dunn, J.D.; Gryniewicz-Ruzicka, C.M.; Mecker-Pogue, L.C.; Kao, J.L.; Ge, X. Rapid screening and structural elucidation of a novel sibutramine analogue in a weight-loss supplement: 11-desisobutyl-11-benzylsibutramine. J. Pharm. Biomed. Anal. 2013, 83, 122–128. [Google Scholar] [CrossRef] [PubMed]
- FDA—Division of Pharmaceutical Analysis Research Programs. Available online: http://www.fda.gov/AboutFDA/CentersOffices/OfficeofMedicalProductsandTobacco/CDER/ucm142466.htm#DrugSafety (accessed on 15 November 2015).
- Favreau, J.T.; Ryu, M.L.; Braunstein, G.; Orshansky, G.; Park, S.S.; Coody, G.L.; Love, L.A.; Fong, T.L. Severe hepatotoxicity associated with the dietary supplement LipoKinetix. Ann. Intern. Med. 2002, 136, 590–595. [Google Scholar] [CrossRef] [PubMed]
- Lipokinetix Dear Healthcare Professional Letter. Available online: http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm174455.htm (accessed on 7 January 2016).
- Neff, G.W.; Reddy, K.R.; Durazo, F.A.; Meyer, D.; Marrero, R.; Kaplowitz, N. Severe hepatotoxicity associated with the use of weight loss diet supplements containing ma huang or usnic acid. J. Hepatol. 2004, 41, 1062–1064. [Google Scholar] [CrossRef] [PubMed]
- Durazo, F.A.; Lassman, C.; Han, S.H.; Saab, S.; Lee, N.P.; Saggi, B.; Gordon, S.; Farmer, D.G.; Yersiz, H.; Goldstein, R.L.; et al. Fulminant liver failure due to usnic acid for weight loss. Am. J. Gastroenterol. 2004, 99, 950–952. [Google Scholar] [CrossRef] [PubMed]
- Ingolfsdottir, K. Usnic acid. Phytochemistry 2002, 61, 729–736. [Google Scholar] [CrossRef]
- Han, D.; Matsumaru, K.; Rettori, D.; Kaplowitz, N. Usnic acid-induced necrosis of cultured mouse hepatocytes: Inhibition of mitochondrial function and oxidative stress. Biochem. Pharmacol. 2004, 67, 439–451. [Google Scholar] [CrossRef] [PubMed]
- Forrester, M. Exposure to 1,3-dimethylamine-containing products reported to Texas poison centers. Hum. Exp. Toxicol. 2013, 32, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Roytman, M.M.; Porzgen, P.; Lee, C.L.; Huddleston, L.; Kuo, T.T.; Bryant-Greenwood, P.; Wong, L.L.; Tsai, N. Outbreak of severe hepatitis linked to weight-loss supplement OxyELITE Pro. Am. J. Gastroenterol. 2014, 109, 1296–1298. [Google Scholar] [CrossRef] [PubMed]
- Foley, S.; Butlin, E.; Shields, W.; Lacey, B. Experience with OxyELITE Pro and acute liver injury in active service members. Dig. Dis. Sci. 2014, 59, 3117–3121. [Google Scholar] [CrossRef] [PubMed]
- FDA News Release. USP Labs LLC Recall OxyELITE Pro Dietary Supplements; Products Linked to Liver Illnesses. 2013. Available online: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm374395.htm (accessed on 7 January 2016). [Google Scholar]
- Klontz, K.C.; DeBeck, H.J.; LeBlanc, P.; Mogen, K.M.; Wolpert, B.J.; Sabo, J.L.; Salter, M.; Seelman, S.L.; Lance, S.E.; Monahan, C.; et al. The role of adverse event reporting in the FDA response to a multistate outbreak of liver disease associated with a dietary supplement. Public Health Rep. 2015, 130, 526–532. [Google Scholar] [PubMed]
- Park, S.Y.; Viray, M.; Johnston, D.; Taylor, E.; Chang, A.; Martin, C.; Schier, J.G.; Lewis, L.S.; Levri, K.M.; Chatham-Stephens, K. Acute hepatitis and liver failure following the use of a dietary supplement intended for weight loss or muscle building. MMWR 2013, 62, 817–819. [Google Scholar]
- Inspection, Compliance, Enforcement, and Criminal Investigations USP Labs, LLC, 4/24/12 Regarding DMAA. Available online: http://www.fda.gov/ICECI/EnforcementActions/WarningLetters/2012/ucm302167.htm (accessed on 25 February 2016).
- Inspection, compliance, enforcement, and criminal investigations USP Labs, 10/11/13. Available online: http://www.fda.gov/ICECI/EnforcementActions/WarningLetters/2013/ucm371203.htm (accessed on 25 February 2016).
- Teschke, R.; Schwarzenboeck, A.; Frenzel, C.; Schulze, J.; Eickhoff, A.; Wolff, A. The mystery of the Hawaii liver disease cluster in summer 2013: A pragmatic and clinical approach to solve the problem. Ann. Hepatol. 2015, 15, 91–109. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Schulze, J.; Eickhoff, A.; Wolff, A.; Frenzel, C. Mysterious Hawaii liver disease case—Naproxen overdose as cause rather than OxyELITE pro? J. Liver Clin. Res. 2015, 2, 1013. [Google Scholar]
- Pro Super Thermogenic Contains Hidden Drug Ingredient. Available online: http://www.fda.gov/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/MedicationHealthFraud/ucm436017.htm (accessed on 7 January 2016).
- FDA News: FDA Issues Regulation Prohibiting Sale of Dietary Supplements Containing Ephedrine Alkaloids and Reiterates Its Advice That Consumers Stop Using These Products. Available online: http://www.fda.gov/NewsEvents/NewRoom/PressAnnouncements/2004/ucm108242.htm (accessed on 25 February 2016).
- Stevens, T.; Qadri, A.; Zein, N.N. Two patients with acute liver injury associated with the use of the herbal weight-loss supplement hydroxycut. Ann. Intern. Med. 2005, 142, 477–478. [Google Scholar] [CrossRef] [PubMed]
- Jones, F.J.; Andrews, H.A. Acute liver injury associated with the herbal supplement hydroxycut in a sodier deployed in Iraq. Am. J. Gastroenterol. 2007, 102, 2357–2358. [Google Scholar] [CrossRef] [PubMed]
- Dara, L.; Hewett, J.; Lim, J.K. Hydroxycut hepatotoxicity: A case series and review of liver toxicity from herbal weight loss supplements. World J. Gastroenterol. 2008, 14, 6999–7004. [Google Scholar] [CrossRef] [PubMed]
- Shim, M.; Saab, S. Severe hepatotoxicity due to Hydroxycut: A case report. Dig. Dis. Sci. 2009, 54, 406–408. [Google Scholar] [CrossRef] [PubMed]
- Sharma, T.; Wong, L.; Tsai, N.; Wong, R.D. Hydroxycut® (herbal weight loss supplement) induced hepatotoxicity; a case report and review of the literature. Hawaii Med. J. 2010, 69, 188–190. [Google Scholar] [PubMed]
- Fong, T.L.; Klontz, K.C.; Canas-Coto, A.; Casper, S.J.; Durazo, F.A.; Davern, T.J., II; Hayashi, P.; Lee, W.M.; Seeff, L.B. Hepatotoxicity due to Hydroxycut: A case series. Am. J. Gastroenterol. 2010, 105, 1561–1566. [Google Scholar] [CrossRef] [PubMed]
- Kaswala, D.H.; Shah, S.; Patel, N.; Raisoni, S.; Swaminathan, S. Hydroxycut-induced liver toxicity. Ann. Med. Health Sci. Res. 2014, 4, 143–145. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.C.; Ramanathan, V.S.; Law, D.; Funchain, P.; Chen, G.C.; French, S.; Shlopov, B.; Eysselein, V.; Chung, D.; Reicher, S.; et al. Acute liver injury induced by weight-loss herbal supplements. World J. Hepatol. 2010, 2, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Bonkovsky, H.L. Hepatotoxicity associated with supplements containing Chinese green tea (Camellia sinensis). Ann. Intern. Med. 2006, 144, 68–71. [Google Scholar] [CrossRef] [PubMed]
- News & Events: FDA News Release—FDA Warns Consumers to Stop Using Hydroxycut Products; Dietary Supplements Linked to One Death: Pose Risk of Liver Injury. Available online: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm149575.htm (accessed on 25 February 2016).
- Araujo, J.L.; Worman, H.J. Acute liver injury associated with a newer formulation of the herbal weight loss supplement Hydroxycut. BMJ Case Rep. 2015. [Google Scholar] [CrossRef] [PubMed]
- HR 4658. Anabolic Steroids Control Act of 1990. Available online: https://www.congress.gov/bill/101st-congress/house-bill/4658 (accessed on 25 February 2016).
- HR 3866. Anabolic Steroid Control Act of 2004. Available online: https://www.govtrack.us/congress/bills/108/s2195 (accessed on 25 February 2016).
- Geyer, H.; Parr, M.K.; Koehler, K.; Mareck, U.; Schänzer, W.; Thevis, M. Nutritional supplements cross-contaminated and faked with doping substances. J. Mass Spectrom. 2008, 43, 892–902. [Google Scholar] [CrossRef] [PubMed]
- Rahnema, C.D.; Crosnoe, L.E.; Kim, E.D. Designer steroids-over-the-counter supplements and their androgenic component: Review of an increasing problem. Andrology 2013, 3, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Kazlaukas, R. Designer steroids. Handb. Exp. Pharmacol. 2010, 195, 153–185. [Google Scholar]
- Van Thuyne, W.; Van Enoo, P.; Delbeke, F.T. Nutritional supplements: Prevalence of use and contamination with doping agents. Nutr. Res. Rev. 2006, 19, 147–158. [Google Scholar] [CrossRef] [PubMed]
- FDA–Public Health Advisory: The FDA Recommends That Consumers Should Not Use Body Building Products Marketed as Containing Steroids or Steroid-Like Substances. 28 July 2009. Available online: http://www.fda.gov/Drugs/ucm173935.htm (accessed on 4 January 2016).
- FDA—Inspections, Compliance, Enforcement, and Criminal Investigations—Warning Letter to American Cellular Labs. July 27 2009. Available online: http://www.fda.gov/ICECI/EnforcementActions/WarningLetters/ucm173874.htm (accessed on 4 January 2016).
- HR 4771. Designer Anabolic Steroid Control Act of 2014. Available online: https://www.govtrack.us/congress/bills/113/hr4771 (accessed on 25 February 2016).
- Robles-Diaz, M.; Gonzalez-Jiminez, A.; Medina-Caliz, I.; Stephens, C.; Garcia-Cortes, M.; Garcia-Munoz, D.; Ortega-Alonso, A.; Blanco-Reina, E.; Gonzalez-Grande, R.; Jiminez-Peres, M.; et al. Distinct phenotype of hepatotoxicity associated with illicit use of anabolic androgenic steroids. Aliment. Pharmacol. Ther. 2015, 41, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Schaffner, F.; Popper, H.; Chesrow, E. Cholestasis produced by the administration of norethandrolone. Am. J. Med. 1959, 26, 249–254. [Google Scholar] [CrossRef]
- Lucey, M.R.; Moseley, R.H. Severe cholestasis associated with methyltestosterone: A case report. Am. J. Gastroenteol. 1987, 82, 461–462. [Google Scholar]
- Gilbert, E.F.; Dasilva, A.Q.; Queen, D.M. Intrahepatic cholestasis with fatal termination following norethandrolone therapy. JAMA 1963, 185, 538–539. [Google Scholar] [CrossRef] [PubMed]
- Farrell, G.C.; Joshua, D.E.; Uren, R.F.; Baird, P.J.; Perkins, K.W.; Kronenberg, H. Androgen-induced hepatoma. Lancet 1975, 1, 430–432. [Google Scholar] [CrossRef]
- Kew, M.C.; van Coller, B.; Prowse, C.M.; Skikne, B.; Wolfsdorf, J.I.; Isdale, J.; KrawiAltman, H.; Levin, S.E.; Bothwell, T.H. Occurrence of primary hepatocellular cancer and peliosis hepatis after treatment with androgenic steroids. S. Afr. Med. J. 1976, 50, 1233–1237. [Google Scholar] [PubMed]
- Boyd, P.R.; Mark, G.J. Multiple hepatic adenomas and a hepatocellular carcinoma in a man on oral methyl testosterone for eleven years. Cancer 1977, 40, 1765–1770. [Google Scholar] [CrossRef]
- Carrasco, D.; Prieto, M.; Pallardo, L.; Moll, J.L.; Cruz, J.M.; Munoz, C.; Berenguer, J. Multiple hepatic adenomas after long-term therapy with testosterone enanthate. Review of the literature. J. Hepatol. 1985, 1, 573–578. [Google Scholar] [CrossRef]
- Bagheri, S.A.; Boyer, J.L. Peliosis hepatis associated with androgenic-anabolic steroid therapy. A severe form of hepatic injury. Ann. Intern. Med. 1974, 81, 610–618. [Google Scholar] [CrossRef] [PubMed]
- McDonald, E.C.; Speicher, C.E. Peliosis hepatis associated with administration of oxymethalone. JAMA 1978, 240, 243–244. [Google Scholar] [CrossRef] [PubMed]
- Kadrouni, M.I.; Anders, R.A.; Verma, S. Hepatotoxicity associated with dietary supplements containing anabolic steroids. Clin. Gastroenterol. Hepatol. 2007, 5, 809–812. [Google Scholar] [CrossRef] [PubMed]
- Shah, N.L.; Zacharias, J.; Khettry, U.; Afdahl, N.; Gordon, F.D. Metasteron-associated cholestatic liver injury: Clinicopathologic findings in 5 cases. Clin. Gastroenterol. Hepatol. 2008, 6, 255–258. [Google Scholar] [CrossRef] [PubMed]
- Nasr, J.; Ahmad, J. Severe cholestasis and renal failure associated with the use of the designer steroid Superdrol (methastereon): A case report and literature review. Dig. Dis. Sci. 2009, 54, 1144–1146. [Google Scholar] [CrossRef] [PubMed]
- Avelar-Escobar, G.; Mendez-Navarro, J.; Ortiz-Alvera, N.X.; Castellanos, G.; Ramos, R.; Gallarda-Cabrera, V.E.; Vargas-Aleman Jde, J.; Diaz de Leon, O.; Rodriguez, E.V.; Dehesa-Violante, M. Hepatotoxicity associated with dietary energy supplements: Use and abuse by young athletes. Ann. Hepatol. 2012, 11, 564–569. [Google Scholar] [PubMed]
- Eisharkawy, A.M.; McPherson, S.; Masson, S.; Burt, A.D.; Dawson, R.T.; Hudson, M. Cholestasis secondary to anabolic steroid use in young men. BMJ 2012, 344, e468. [Google Scholar] [CrossRef] [PubMed]
- El Sherrif, Y.; Potts, J.R.; Howard, M.R.; Barnado, A.; Cairns, S.; Knisely, A.S.; Verma, S. Hepatotoxicity from anabolic androgenic steroids marketed as dietary supplements: Contribution from ATP8B1/ABCB11 mutations? Liver Int. 2013, 33, 1266–1270. [Google Scholar] [CrossRef] [PubMed]
- Villela, A.L.; Limsuwat, C.; Williams, D.R.; Seifert, C.F. Cholestatic jaundice as a result of combination designer supplement ingestion. Ann. Pharmacother. 2013, 47, e33. [Google Scholar] [CrossRef] [PubMed]
- Agbenyefia, P.; Arnold, C.A.; Kirkpatrick, R. Cholestatic jaundice with the use of Methylstenbolone and Dymethazine, designer steroids found in DMZ Rx 2.0 “Nutritional Supplement”: A case report. J. Investig. Med. High Impact Case Rep. 2014, 2. [Google Scholar] [CrossRef] [PubMed]
- Gorayski, P.; Thompson, P.H.; Subhash, H.S.; Thomas, A.C. Hepatocellular carcinoma associated with recreational anabolic steroid use. Br. J. Sports Med. 2008, 42, 74–75. [Google Scholar] [CrossRef] [PubMed]
- Socas, L.; Zumbado, M.; Perez-Luzardo, O.; Ramos, A.; Perez, C.; Hernandez, J.R.; Boada, L.D. Hepatocellular adenomas associated with anabolic androgenic steroid abuse in bodybuilders: A report of two cases and a review of the literature. Br. J. Sports Med. 2005, 39, e27. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Nieto, L.; Bruguera, M.; Bombi, J.; Comacho, L.; Rozman, C. Benign liver-cell adenoma associated with long-term administration of an androgenic-anabolic steroid (methandienone). Cancer 1977, 40, 1761–1764. [Google Scholar] [CrossRef]
- Bagia, S.; Hewitt, P.M.; Morris, D.L. Anabolic steroid-induced hepatic adenoma with spontaneous haemorrhage in a bodybuilder. Aust. N. Z. J. Surg. 2000, 70, 686–687. [Google Scholar] [CrossRef] [PubMed]
- Cabasso, A. Peliosis hepatis in a young adult bodybuilder. Med. Sci. Sports Exerc. 1994, 26, 2–4. [Google Scholar] [CrossRef] [PubMed]
- Abbate, V.; Kicman, A.T.; Evans-Brown, M.; McVeigh, J.; Cowan, D.A.; Wilson, C.; Coles, S.J.; Walker, C.J. Anabolic steroids detected in bodybuilding dietary supplements—A significant risk to public health. Drug Test. Anal. 2015, 7, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Schwingel, P.A.; Cotrim, H.P.; Salles, B.R.; Almeida, C.E.; dos Santos, C.R., Jr.; Nachef, B.; Andrade, A.R.; Zoppi, C.C. Anabolic-androgenic steroids: A possible new risk factor for toxicant-associated fatty liver disease. Liver Int. 2011, 31, 348–353. [Google Scholar] [CrossRef] [PubMed]
- Alazuddin Saraf, S. Legal regulation of complementary and alternative medicines in different countries. Pharmacogn. Rev 2012, 6, 154–160. [Google Scholar]
- World Health Organization. Research Guidelines for Evaluating the Safety and Efficacy of Herbal Medicines; World Health Organization: Manila, Philippines, 1993. [Google Scholar]
- World Health Organization. Regulatory Situation of Herbal Medicines: A Worldwide Review (WHO/trm/98.1); World Health Organization: Geneva, Switzerland, 1998. [Google Scholar]
- Kahn, I.A.; Smillie, T. Implementing a “quality by design” approach to assure the safety and integrity of botanical dietary supplements. J. Nat. Prod. 2012, 75, 1665–1673. [Google Scholar] [CrossRef] [PubMed]
- Betz, J.M.; Fisher, K.D.; Saldanha, L.G.; Coates, P.M. The NIH analytical methods and reference materials program for dietary supplements. Anal. Bioanal. Chem. 2007, 389, 19–25. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Avigan, M.I.; Mozersky, R.P.; Seeff, L.B. Scientific and Regulatory Perspectives in Herbal and Dietary Supplement Associated Hepatotoxicity in the United States. Int. J. Mol. Sci. 2016, 17, 331. https://doi.org/10.3390/ijms17030331
Avigan MI, Mozersky RP, Seeff LB. Scientific and Regulatory Perspectives in Herbal and Dietary Supplement Associated Hepatotoxicity in the United States. International Journal of Molecular Sciences. 2016; 17(3):331. https://doi.org/10.3390/ijms17030331
Chicago/Turabian StyleAvigan, Mark I., Robert P. Mozersky, and Leonard B. Seeff. 2016. "Scientific and Regulatory Perspectives in Herbal and Dietary Supplement Associated Hepatotoxicity in the United States" International Journal of Molecular Sciences 17, no. 3: 331. https://doi.org/10.3390/ijms17030331
APA StyleAvigan, M. I., Mozersky, R. P., & Seeff, L. B. (2016). Scientific and Regulatory Perspectives in Herbal and Dietary Supplement Associated Hepatotoxicity in the United States. International Journal of Molecular Sciences, 17(3), 331. https://doi.org/10.3390/ijms17030331