The Honolulu Liver Disease Cluster at the Medical Center: Its Mysteries and Challenges
Abstract
:1. Introduction
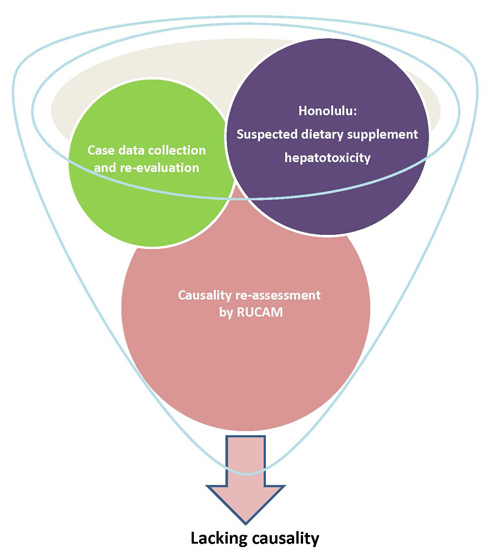
2. Evolution of the Honolulu Queen’s Medical Center (QMC) Mysteries
2.1. Initial Statements and Inconsistencies
2.2. Incriminated Dietary Supplements
2.3. Case and Product Analyses
2.4. Selected Clinical Issues Confronting the QMC
2.5. Temporal versus Causal Association
2.6. Retrospective versus Prospective Analysis
2.7. Quality versus Quantity
2.8. Newspaper and TV Publicity Obscuring Careful Clinical Work
2.9. Remarkably High Use of Dietary Supplements
3. Inconsistencies during QMC Case Analyses
3.1. Product Identification Including Proof of Purchase and Usage
3.2. Question of Therapeutic Options other than Liver Transplantation
3.2.1. Acetaminophen
3.2.2. Hepatitis B Virus Infection
3.2.3. Hepatitis E Virus Infection
3.2.4. Herpes Simplex Virus Infection
3.2.5. Varicella Zoster Virus Infection
3.2.6. Cytomegalovirus
3.2.7. Wilson Disease
3.3. Undeclared QMC Case Definition
3.4. Incomplete Data Presentation
3.5. Diagnostic Uncertainty
3.5.1. Qualification
3.5.2. Lacking Strict Diagnostic Protocol at the QMC
3.6. Choosing RUCAM as the Best Causality Algorithm
3.7. Incorrect Use of RUCAM
3.7.1. Challenge Criteria
3.7.2. Dechallenge Features
3.7.3. Comedication Issue
3.7.4. Alternative Cause Search
3.7.5. Willingly Upgrading of RUCAM Scores
3.8. Diagnosis of Exclusion
3.9. Critical Liver Histology
4. Emerging Problems of the QMC Credibility
5. QMC Challenges
5.1. General Considerations
5.2. Problems with QMC Data and Confounders
6. Centers of Disease Control and Prevention Report
6.1. First Regulatory Report
6.2. Public Health Investigation
6.3. Epidemiological Study Protocol with Missing Control Group
6.4. Lack of Specific Product Identification
6.5. Questionable Causality Assessment Method
6.6. Inadequate Regulatory Case Definition
6.7. Liver Histology
6.8. Confounders
6.9. Variable Case Numbers
7. Hawaii Department of Health Report
7.1. Product Identification
7.2. Causality Assessment Method
7.3. Case Definition
7.4. Inconsistent Data Presentation
7.5. Comorbidities
7.6. Synthetic Drugs as Comedication and Potential Causes
7.7. Additionally Used Dietary Supplements as Potential Causes
7.8. Alcohol Use
7.9. Time of Onset
7.10. Questionable Illustrative Cases
7.10.1. Case 1
7.10.2. Case 2
7.11. Variability of Case Numbers
7.12. Confounders
8. Food and Drug Administration Report
8.1. FDA Cases in the Overview
8.2. FDA and Its Case Definition
8.3. FDA Report and Its Problematic MedWatch System
8.4. FDA and the Lack of a Sufficiently Sophisticated Causality Assessment Algorithm
8.5. FDA and the 21 Honolulu QMC Liver Cases
8.6. FDA and the 12 Nationwide Liver Cases
8.7. Variability of Case Numbers
8.8. Confounders
9. Limitation of this Review
10. Conclusions
Author Contributions
Conflicts of Interest
Abbreviations
| AAP | acetaminophen |
| ALF | acute liver failure |
| HAV | hepatitis A virus |
| HBV | hepatitis B virus |
| HBc | hepatitis B core |
| HBs | hepatitis B surface |
| HCV | hepatitis C virus |
| HDOH | Hawaii Department of Health |
| HDS | herbal dietary supplement |
| HEV | hepatitis E virus |
| HILI | herb induced liver injury |
| FDA | Food and Drug Administration in Washington DC, USA |
| HAV | hepatitis A virus |
| HBV | hepatitis B virus |
| HBc | hepatitis B core |
| HBs | hepatitis B surface |
| HCV | hepatitis C virus |
| HDOH | Hawaii Department of Health |
| HDS | herbal dietary supplement |
| HEV | hepatitis E virus |
| HILI | herb induced liver injury |
| HSV | herpes simplex virus |
| LTs | liver tests |
| N | normal range as multiple of its upper limit |
| NAFLD | non-alcoholic fatty liver disease |
| NSAID | non-steroidal antiinflammatory drugs |
| OC | Oxy Cleanse |
| OEP | OxyELITE Pro |
| OLT | orthotopic liver transplantation |
| OTC | over the counter |
| PCP | primary care provider |
| PCR | polymerase chain reaction |
| PMH | past medical history |
| QMC | Queen’s Medical Center in Honolulu |
| RUCAM | Roussel Uclaf Causality Assessment Method |
| VZV | varicella zoster virus |
References
- Sanico, M.; Soria, R. Legends of the Pali. Available online: http://www.abstracthawaii.com/journal/legends-of-the-pali (accessed on 12 March 2016).
- Chiles, W.P. The Secrets and Mysteries of Hawaii; Health Communications, Inc.: Honolulu, HI, USA, 1995. [Google Scholar]
- CDC, Centers for Disease Control and Prevention. Acute hepatitis and liver failure following use of a dietary supplement intended for weight loss or muscle building—May–October 2013. MMWR Morb Mortal Wkly. Rep. 2013, 62, 817–819. [Google Scholar]
- Cohen, P.A. Hazards of hindsight—Monitoring the safety of nutritional supplements. N. Engl. J. Med. 2014, 370, 1277–1280. [Google Scholar] [CrossRef] [PubMed]
- Roytman, M.M.; Pörzgen, P.; Lee, C.L.; Huddleston, L.; Kuo, T.T.; Bryant-Greenwood, P.; Wong, L.L.; Tsai, N. Letter to the Editor: Outbreak of severe hepatitis linked to weight-loss supplement OxyELITE Pro. Am. J. Gastroenterol. 2014, 109, 1296–1298. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Schulze, J.; Eickhoff, A.; Wolff, A.; Frenzel, C. Mysterious Hawaii liver disease case—Naproxen overdose as cause rather than OxyELITE Pro? J. Liver Clin. Res. 2015, 2, 1013. Available online: http://www.jscimedcentral.com/Liver/liver-2-1013.pdf (accessed on 12 March 2016). [Google Scholar]
- Klontz, K.C.; DeBeck, H.J.; LeBlanc, P.; Mogen, K.M.; Wolpert, B.J.; Sabo, J.L.; Salter, M.; Seelman, S.L.; Lance, S.E.; Monahan, C.; et al. The role of adverse event reporting in the FDA response to multistate outbreak of liver disease associated with a dietary supplement. Public Health Rep. 2015, 130, 526–532. [Google Scholar] [PubMed]
- Johnston, D.I.; Chang, A.; Viray, M.; Chatham-Stephens, K.; He, H.; Taylor, E.; Wong, L.L.; Schier, J.; Martin, C.; Fabricant, D.; et al. Hepatotoxicity associated with the dietary supplement OxyELITE Pro TM—Hawaii 2013. Drug Test Anal. 2015. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Schwarzenboeck, A.; Frenzel, C.; Schulze, J.; Eickhoff, A.; Wolff, A. The mystery of the Hawaii liver disease cluster in summer 2013: A pragmatic and clinical approach to solve the problem. Ann. Hepatol. 2016, 15, 91–119. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Agency for Toxic Substances and Disease Registry, Division of Toxicology and Environmental Medicine. Disease clusters: An overview. Available online: http://www.atsdr.cdc.gov/HEC/CSEM/cluster/docs/clusters.pdf (accessed on 12 March 2016).
- CDC, Centers for Disease Control and Prevention. Guidelines for investing clusters of health events. MMWR 1990, 39, 1–23. [Google Scholar]
- Fares, A. Seasonable of viral hepatitis. J. Acad. Med. Sci. 2012, 2, 110–114. [Google Scholar] [CrossRef]
- Nainan, O.V.; Xia, G.; Vaughan, G.; Harold, S.; Margolis, H.S. Diagnosis of hepatitis A virus infection: A molecular approach. Clin. Microbiol. Rev. 2006, 19, 63–79. [Google Scholar] [CrossRef] [PubMed]
- Hoofnagle, J.H.; Nelson, K.E.; Purcell, R.H. Review article: Hepatitis E. N. Engl. J. Med. 2012, 367, 1237–1244. [Google Scholar] [CrossRef] [PubMed]
- Pavio, N.; Meng, X.J.; Renou, C. Zoonotic hepatitis E: Animal reservoirs and emerging risks. Vet. Res. 2010, 41. [Google Scholar] [CrossRef] [PubMed]
- Fujiwara, S.; Yokokawa, Y.; Morino, K.; Hayasaka, K.; Kawabata, M.; Shimizu, T. Chronic hepatitis E: A review of the literature. J. Viral. Hepat. 2014, 2, 78–89. [Google Scholar] [CrossRef] [PubMed]
- Li, T.C.; Chijiwa, K.; Sera, N.; Ishibashi, T.; Etoh, Y.; Shinohara, Y.; Kurata, Y.; Ishida, M.; Sakamoto, S.; Takeda, N.; et al. Hepatitis E virus transmission from wild boar meat. Emerg. Infect. Dis. 2005, 11, 1958–1960. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.J. Zoonotic and xenozoonotic risks of the hepatitis E virus. Infect. Dis. Rev. 2000, 2, 35–41. [Google Scholar]
- Tei, S.; Kitajima, N.; Takahashi, K.; Mishiro, S. Zoonotic transmission of hepatitis E virus from deer to human beings. Lancet 2003, 362, 371–373. [Google Scholar] [CrossRef]
- WHO: Hepatitis E. Available online: http://www.who.int/mediacentre/factsheets/fs280/en/ (accessed on 12 March 2016).
- Masuda, J.I.; Yano, K.; Tamada, Y.; Takii, Y.; Ito, M.; Omagari, K.; Kohno, S. Acute hepatitis E of a man who consumed wild boar meat prior to the onset of illness in Nagasaki, Japan. Hepatol. Res. 2005, 31, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, H.; Okada, K.; Takahashi, K.; Mishiro, S. Severe hepatitis E virus infection after ingestion of uncooked liver from a wild boar. J. Infect. Dis. 2003, 188. [Google Scholar] [CrossRef] [PubMed]
- Kabrane-Lazizi, Y.; Fine, J.B.; Elm, J.; Glass, G.E.; Higa, H.; Diwan, A.; Gibbs, C.J., Jr.; Meng, X.J.; Emerson, S.U.; Purcell, R.H. Evidence for widespread infection of wild rats with hepatitis E virus in the United States. Am. J. Trop. Med. Hyg. 1999, 61, 331–335. [Google Scholar] [PubMed]
- Davern, T.J.; Chalasani, N.; Fontana, R.J.; Hayashi, P.H.; Protiva, P.; Kleiner, D.E.; Engle, R.E.; Nguyen, H.; Emerson, S.U.; Purcell, R.H.; et al. for the Drug-Induced Liver Injury Network (DILIN). Acute hepatitis E infection accounts for some cases of suspected drug-induced liver injury. Gastroenterology 2011, 141, 1665–1672. [Google Scholar] [CrossRef] [PubMed]
- Dalton, H.R.; Fellows, H.J.; Stableforth, W.; Josph, M.; Thurairajah, P.H.; Warshow, U.; Hazeldine, S.; Remnarace, R.; Ijaz, S.; Hussaini, S.H.; et al. The role of hepatitis E virus testing in drug-induced liver injury. Aliment. Pharmacol. Ther. 2007, 26, 1429–1435. [Google Scholar] [CrossRef] [PubMed]
- Hawaii Department of Health: What is leptospirosis? Available online: http://health.hawaii.gov/about/files/2013/06/leptobrochure.pdf (accessed on 12 March 2016).
- Bharti, A.R.; Nally, J.E.; Ricaldi, J.N.; Matthias, M.A.; Diaz, M.M.; Lovett, M.A.; Levett, P.N.; Gilman, R.H.; Willig, M.R.; Gotuzzo, E.; et al. Peru-United States Leptospirosis Consortium. Leptospirosis: A zoonotic disease of global importance. Lancet Infect. Dis. 2003, 3, 757–771. [Google Scholar] [CrossRef]
- Tandon, H.D.; Tandon, B.N.; Ramalingaswami, V. Epidemic of toxic hepatitis in India of possible mycotoxic origin. Arch. Pathol. Lab. Med. 1978, 102, 372–376. [Google Scholar] [PubMed]
- Anfossi, L.; Calderara, M.; Baggiani, C.; Giovannoli, C.; Arletti, E.; Giraudi, G. Development and application of solvent-free extraction for the detection of aflatoxin M1 in dairy products by enzyme immunoassay. J. Agric. Food Chem. 2008, 56, 1852–1857. [Google Scholar] [CrossRef] [PubMed]
- Azziz-Baumgartner, E.; Lindblade, K.; Gieseker, K.; Schurz Rogers, H.; Kieszak, S.; Njapau, H.; Schleicher, R.; McCoy, L.F.; Misore, A.; DeCock, K.; et al. Case-control study of an acute aflatoxicosis outbreak, Kenya, 2004. Environ/ Health Perspect. 2005, 113, 1779–1783. [Google Scholar] [CrossRef]
- Ferrer Amate, C.; Unterluggauer, H.; Fischer, R.J.; Fernández-Alba, A.R.; Masselter, S. Development and validation of a LC-MS/MS method for the simultaneous determination of aflatoxins, dyes and pesticides in spices. Anal. Bioanal. Chem. 2010, 397, 93–107. [Google Scholar] [CrossRef] [PubMed]
- Garon, D.; El Kaddoumi, A.; Carayon, A.; Amiel, C. FT-IR spectroscopy for rapid differentiation of Aspergillus flavus, Aspergillus fumigatus, Aspergillus parasiticus and characterization of aflatoxigenic isolates collected from agricultural environments. Mycopathologica 2010, 170, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Huang, B.; Han, Z.; Cai, Z.; Wu, Y.; Ren, Y. Simultaneous determination of aflatoxins B1, B2, G1, G2, M1 and M2 in peanuts and their derivative products by ultra-high-performance liquid chromatography-tandem mass spectrometry. Anal. Chim. Acta 2010, 662, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Lupo, A.; Roebuck, C.; Dutcher, M.; Kennedy, J.; Abouzied, M. Validation study of a rapid ELISA for detection of aflatoxin in corn. Performance Tested Method 050901. AOAC Int. 2010, 93, 587–599. [Google Scholar]
- Ngindu, A.; Johnson, B.K.; Ngira, J.A.; Nandwa, H.; Jansen, A.J.; Kaviti, J.N.; Siongok, T.A. Outbreak of acute hepatitis caused by aflatoxin poisoning in Kenya. Lancet 1982, 319, 1346–1348. [Google Scholar] [CrossRef]
- Quinto, M.; Spadaccino, G.; Palermo, C.; Centonze, D. Determination of aflatoxins in cereal flours by solid-phase microextraction coupled with liquid chromatography and post-column photochemical derivatization-fluorescence detection. J. Chromatogr. A 2009, 1216, 8636–8641. [Google Scholar] [CrossRef] [PubMed]
- Kakar, F.; Akbarian, Z.; Leslie, T.; Mustafa, M.L.; Watson, J.; van Egmond, H.P.; Omar, M.F.; Mofleh, J. An outbreak of hepatic veno-occlusive disease in western Afghanistan associated with exposure to wheat flour contaminated with pyrrolizidine alkaloids. J. Toxicol. 2010, 2010. [Google Scholar] [CrossRef] [PubMed]
- Tandon, B.N.; Tandon, H.D.; Tandon, R.K.; Narndranathan, M.; Joshi, Y.K. An epidemic of veno-occlusive disease of the liver in central India. Lancet 1976, 308, 271–272. [Google Scholar] [CrossRef]
- Tandon, H.D.; Tandon, B.; Weston, C.F.M.; Cooper, B.T.; Davies, J.D.; Levine, D.F. Veno-occlusive disease of the liver secondary to ingestion of comfrey. Br. Med. J. (Clin. Res. Ed.) 1987, 295, 183. [Google Scholar]
- Tandon, R.K.; Tandon, B.N.; Tandon, H.D. Study of an epidemic of venoocclusive disease in India. Gut 1976, 17, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Zhang, L.; Melzer, L.; Schulze, J.; Eickhoff, A. Green tea extract and the risk of drug-induced liver injury. Expert Opin. Drug Metab. Toxicol. 2014, 10, 1663–1676. [Google Scholar] [CrossRef] [PubMed]
- Millonig, G.; Stadlmann, S.; Vogel, W. Herbal hepatotoxicity: Acute hepatitis caused by a Noni preparation (Morinda citrifolia). Eur. J. Gastroenterol. Hepatol. 2005, 17, 445–447. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.C.; Johnston, E.; Xing, C.; Hegeman, A.D. Measuring the chemical and cytotoxic variability of commercially available kava (Piper methysticum G. Forster). PLoS ONE 2014, 9, e111572. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M. Quality criteria for kava. Herbal. Gram 2007, 73, 45–49. [Google Scholar]
- Teschke, R.; Lebot, V. Proposal for a Kava Quality Standardization Code. Food Chem. Toxicol. 2011, 49, 2503–2516. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Schulze, J. Risk of kava hepatotoxicity and the FDA consumer advisory. J. Am. Med. Assoc. 2010, 304, 2174–2175. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Sarris, J.; Schweitzer, I. Kava hepatotoxicity in traditional and modern use: The presumed Pacific kava paradox hypothesis revisited. Br. J. Clin. Pharmacol. 2012, 73, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Sarris, J.; Glass, X.; Schulze, J. Kava, the anxiolytic herb: Back to basics to prevent liver injury? Br. J. Clin. Pharmacol. 2011, 71, 445–448. [Google Scholar] [CrossRef] [PubMed]
- Watkins, P.B. How to diagnose and exclude drug-induced liver injury. Dig. Dis. 2015, 33, 472–476. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Frenzel, C.; Wolff, A.; Eickhoff, A.; Schulze, J. Drug induced liver injury: Accuracy of diagnosis in published reports. Ann. Hepatol. 2014, 13, 248–255. [Google Scholar] [PubMed]
- Teschke, R.; Andrade, R. (Eds.) Drug-induced liver injury: Expanding our knowledge by enlarging population analysis with prospective and scoring causality assessment. Gastroenterology 2015, 148, 1271–1273. [CrossRef] [PubMed]
- Teschke, R.; Frenzel, C. Drug induced liver injury: Do we still need a routine liver biopsy for diagnosis today? Ann. Hepatol. 2014, 13, 121–126. [Google Scholar]
- Danan, G.; Teschke, R. RUCAM in drug and herb induced liver injury: The update. Special issue: Drug, herb, and dietary supplement hepatotoxicity. Int. J. Mol. Sci. 2016, 17. [Google Scholar] [CrossRef]
- Bunchorntavakul, C.; Reddy, K.R. Review article: Herbal and dietary supplement hepatotoxicity. Aliment Pharmacol. Ther. 2013, 37, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Navarro, V.J.; Barnhart, H.; Bonkovsky, H.L.; Davern, T.; Fontana, R.J.; Grant, L.; Reddy, K.R.; Seeff, L.B.; Serrano, J.; Sherker, A.H.; et al. Liver injury from herbals and dietary supplements in the U.S. Drug-Induced Liver Injury Network. Hepatology 2014, 60, 1399–1408. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Schwarzenboeck, A.; Eickhoff, A.; Frenzel, C.; Wolff, A.; Schulze, J. Clinical and causality assessment in herbal hepatotoxicity. Expert Opin. Drug Saf. 2013, 12. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Eickhoff, A. Herbal hepatotoxicity in traditional and modern medicine: Actual key issues and new encouraging steps. Front. Pharmacol. 2015, 6. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Eickhoff, A.; Schwarzenboeck, A.; Schmidt-Taenzer, W.; Genthner, A.; Frenzel, C.; Wolff, A.; Schulze, J. Clinical review: Herbal hepatotoxicity and the call for systematic data documentation of individual cases. J. Liver Clin. Res. 2015, 2, 1–14. [Google Scholar]
- Teschke, R.; Schulze, J.; Schwarzenboeck, A.; Eickhoff, A.; Frenzel, C. Herbal hepatotoxicity: Suspected cases assessed for alternative causes. Eur. J. Gastroenterol. Hepatol. 2013, 25, 1093–1098. [Google Scholar] [CrossRef] [PubMed]
- Pereira, A. Interview about OEP: Doctors at center of liver disease cluster still unsure about cause. Posted on 10/10/2013. Available online: http://www.kitv.com/news/hawaii/doctors-at-center-of-liver-disease-cluster-still-unsure-about-cause/22382214 (accessed on 12 March 2016).
- Huffpost Healthy Living: Aegeline identified as harmful ingredient in OEP. Posted on 1/18/2014. Available online: http://www.huffingtonpost.com/2014/01/28/aegeline-oxyelite-pro_n_4683990.html (accessed on 12 March 2016).
- Bailey, R.L.; Gahche, J.J.; Miller, P.E.; Thomas, P.R.; Dwyer, J.T. Why US adults use dietary supplements. JAMA Intern. Med. 2013, 173, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Radimer, K.; Bindewald, B.; Hughes, J.; Ervin, B.; Swanson, C.; Picciano, M.F. Dietary supplement use by US adults: Data from a National Health and Nutrition examination survey, 1999–2000. Am. J. Epidemiol. 2004, 160, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Murphy, S.P.; Wilkens, L.R.; Monroe, K.R.; Steffen, A.D.; Yonemori, K.M.; Morimoto, Y.; Albright, C.L. Dietary supplement use within a multiethnic population as measured by a unique inventory method. J. Am. Diet. Assoc. 2011, 111, 1065–1072. [Google Scholar] [CrossRef] [PubMed]
- Mahady, G.B.; Low Dog, T.; Barrett, M.L.; Chavez, M.L.; Gardiner, P.; Ko, R.; Marles, R.J.; Pellicore, L.S.; Giancaspro, G.I.; Sarma, D.N. United States Pharmacopeia review of the black cohosh case reports of hepatotoxicity. Menopause 2008, 15, 628–638. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Schmidt-Taenzer, W.; Wolff, A. Spontaneous reports of assumed herbal hepatotoxicity by black cohosh: Is the liver unspecific Naranjo scale precise enough to ascertain causality? Pharmacoepidemiol. Drug Saf. 2011, 20, 567–582. [Google Scholar] [CrossRef] [PubMed]
- Smilkstein, M.J.; Knapp, G.L.; Kulig, K.W.; Rumack, B.H. Efficacy of oral N-acetylcysteine in the treatment of acetaminophen overdose. N. Engl. J. Med. 1988, 319, 1557–1562. [Google Scholar] [CrossRef] [PubMed]
- Mason, A.; Sallie, R. What causes fulminant hepatic failure of unknown etiology? Am. J. Clin. Pathol. 1995, 104, 491–494. [Google Scholar] [CrossRef] [PubMed]
- Shakil, A.O.; Kramer, D.; Mazariegos, G.V.; Fung, J.J.; Rakela, J. Acute liver failure: Clinical features, outcome analysis, and applicability of prognostic criteria. Liver Transpl. 2000, 6, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Larson, A.M.; Polson, J.; Fontana, R.J.; Davern, T.J.; Lalani, E.; Hynan, L.S.; Reisch, J.S.; Schiødt, F.V.; Ostapowicz, G.; Shakil, A.O.; et al. Acetaminophen-induced acute liver failure: Results of a United States multicentre, prospective study. Hepatology 2005, 42, 1364–1372. [Google Scholar] [CrossRef] [PubMed]
- Bower, W.A.; Johns, M.; Margolis, H.S.; Williams, I.T.; Bell, B. Population-based surveillance for acute liver failure. Am. J. Gastroenterol. 2007, 102, 2459–2463. [Google Scholar] [CrossRef] [PubMed]
- Bernal, W.; Auzinger, G.; Dhawan, A.; Wendon, J. Acute liver failure. Lancet 2010, 376, 190–201. [Google Scholar] [CrossRef]
- Reuben, A.; Koch, D.G.; Lee, W.M.; the Acute Liver Failure Study Group. Drug-induced acute liver failure: Results of a U.S. multicenter, prospective study. Hepatology 2010, 52, 2065–2076. [Google Scholar] [CrossRef] [PubMed]
- Khandelwal, N.; James, L.P.; Sanders, C.; Larson, A.M.; Lee, W.M.; the Acute Liver Failure Study Group. Unrecognized acetaminophen toxicity as a cause of indeterminate acute liver failure. Hepatology 2011, 53, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.M.; Larson, A.M.; Stravitz, R.T. AASLD position paper: The management of acute liver failure: Update 2011. Available online: https://www.aasld.org/sites/default/files/guideline_documents/alfenhanced.pdf (accessed on 12 March 2016).
- Nakayama, N.; Oketani, M.; Kawamura, Y.; Inao, M.; Nagoshi, S.; Fujiwara, K. Algorithm to determine the outcome of patients with acute liver failure: A data-mining analysis using decision trees. J. Gastroenterol. 2012, 47, 664–677. [Google Scholar] [CrossRef] [PubMed]
- Sgro, C.; Clinard, F.; Ouazir, K.; Chanay, H.; Allard, C.; Guilleminet, C.; Lenoir, C.; Lemoine, A.; Hillon, P. Incidence of drug-induced hepatic injuries: A French population-based study. Hepatology 2002, 36, 451–455. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Stutz, G.; Strohmeyer, G. Increased paracetamol-induced hepatotoxicity after chronic alcohol consumption. Biochem. Biophys. Res. Commun. 1979, 91, 368–374. [Google Scholar] [CrossRef]
- Lok, A.S.F.; McMahon, B.J. Chronic hepatitis B: Update 2009. Hepatology 2009, 50, 1–36. [Google Scholar] [CrossRef] [PubMed]
- Kamar, N.; Izopet, J.; Tripon, S.; Bismuth, M.; Hillaire, S.; Dumortier, J.; Radenne, S.; Coilly, A.; Garrigue, V.; D’Alteroche, L.; et al. Ribavirin for chronic hepatitis E virus infection in transplant recipients. N. Engl. J. Med. 2014, 370, 1111–1120. [Google Scholar] [CrossRef] [PubMed]
- Wedemeyer, H.; Pischke, S.; Manns, M.P. Pathogenesis and treatment of hepatitis E virus infection. Gastroenterology 2012, 142, 1388–1397. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; Ali, I.A.; Ghazal, H.; Fazili, J.; Nusrat, S. Mystery of hepatitis E virus: Recent advances in its diagnosis and management. Int. J. Hepatol. 2015, 2015. [Google Scholar] [CrossRef] [PubMed]
- Focus Diagnostics: Reference laboratory tests: 2071–2073 Hepatitis E antibodies (IgG, IgM), (IgG), and (IgM). Available online: https://www.focusdx.com/focus/1-reference_laboratory/search_frame.asp?f=8 (accessed on 12 March 2016).
- Zuckerman, R.A.; Limaye, A.P. Varicella zoster virus (VZV) and herpes simplex virus (HSV) in solid organ transplant patients. Am. J. Transpl. 2013, 13, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Luzar, B.; Ferlan-Marolt, V.; Poljak, M.; Sojar, V.; Stanisavlevic, D.; Bucovac, T.; Makoviv, S. Acute fatty liver of pregnancy—An underlying condition of herpes simplex type 2 fulminant hepatitis necessitating liver transplantation. Z. Gastroenterol. 2005, 43, 451–454. [Google Scholar] [CrossRef] [PubMed]
- Velasco, M.; Llamas, E.; Guijarro-Rojas, M.; Ruiz-Yague, M. Fulminant herpes hepatitis in a healthy adult. A treatable disease? J. Clin. Gastroenterol. 1999, 28, 386–389. [Google Scholar] [CrossRef] [PubMed]
- Pinna, A.D.; Rakela, J.; Demetris, A.J.; Fung, J.J. Five cases of fulminant hepatitis due to herpes simplex virus in adults. Dig. Dis. Sci. 2002, 47, 750–754. [Google Scholar] [CrossRef] [PubMed]
- Rimawi, B.H.; Meserve, J.; Rimawi, R.H.; Min, Z.; Gnann, J.W. Disseminated herpes simplex virus with fulminant hepatitis. Case Rep. Hepatol. 2015, 2015. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Schwarzenboeck, A. Suspected hepatotoxicity by cimicifugae racemosae rhizoma (black cohosh, root): Critical analysis and structured causality assessment. Phytomedicine 2009, 16, 72–84. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Schulze, J. Suspected herbal hepatotoxicity: Requirements for appropriate causality assessment by the US Pharmacopeia. Drug Saf. 2012, 35, 1091–1097. [Google Scholar] [CrossRef] [PubMed]
- Pishvaian, A.C.; Bahrain, M.; Lewis, J.H. Fatal varicella-zoster hepatitis presenting with severe abdominal pain: A case report and review of the literature. Dig. Dis. Sci. 2006, 51, 1221–1225. [Google Scholar] [CrossRef] [PubMed]
- Dits, H.; Frans, E.; Wilmer, A.; van Ranst, M.; Fevery, J.; Bobbaers, H. Varicella-zoster virus infection associated with acute liver failure. Clin. Infect. Dis. 1998, 27, 209–210. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.R.; Hunter, N.J.; Cottrill, C.; Bissacia, E.; Klainer, A.S. Varicella hepatitis: A fatal case in a previously healthy immunocompetent adult. Report of a case, autopsy, and review of the literature. Arch. Intern. Med. 1994, 154, 2101–2106. [Google Scholar] [CrossRef] [PubMed]
- Vartian, C.V. Varicella-zoster virus infection associated with acute liver failure. Clin. Infect. Dis. 1999, 28, 412–123. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A. Antiviral treatment of cytomegalovirus infection. Infect. Disord Drug Targets 2011, 11, 475–503. [Google Scholar] [CrossRef] [PubMed]
- Jain, M.; Duggal, S.; Chugh, T.D. Cytomegalovirus infection in non-immunosuppressed critically ill patients. J. Infect. Dev. Ctries 2011, 5, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Boeckh, M.; Geballe, A.P. Cytomegalovirus: Pathogen, paradigm, and puzzle. J. Clin. Investig. 2011, 121, 1673–1680. [Google Scholar] [CrossRef] [PubMed]
- Korman, J.D.; Volenberg, I.; Balko, J.; Webster, J.; Schiodt, F.V.; Squires, R.H.; Fontana, R.J.; Lee, W.M.; Schilsky, M.I.; the Pediatric and Adult Acute Liver Failure Study Groups. Screening for Wilson disease in acute liver failure: A comparison on currently available diagnostic tests. Hepatology 2008, 48, 1167–1174. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, A.; Williams, R. Rapid diagnosis of Wilson disease in acute liver failure: No more waiting for the ceruloplasmin level? Hepatology 2008, 48, 1030–1032. [Google Scholar]
- Teschke, R.; Frenzel, C.; Schulze, J.; Eickhoff, A. Herbal hepatotoxicity: Challenges and pitfalls of causality assessment methods. World J. Gastroenterol. 2013, 19, 2864–2882. [Google Scholar] [CrossRef] [PubMed]
- Danan, G.; Bénichou, C. Causality assessment of adverse reactions to drugs—I. A novel method based on the conclusions of international consensus meetings: Application to drug-induced liver injuries. J. Clin. Epidemiol. 1993, 46, 1323–1330. [Google Scholar] [CrossRef]
- Bénichou, C.; Danan, G.; Flahault, A. Causality assessment of adverse reactions to drugs—II. An original model for validation of drug causality assessment methods: Case reports with positive rechallenge. J. Clin. Epidemiol. 1993, 46, 1331–1336. [Google Scholar] [CrossRef]
- Chalasani, N.; Bonkovsky, H.L.; Fontana, R.; Lee, W.; Stolz, A.; Talwalkar, J.; Reddy, K.R.; Watkins, P.B.; Navarro, V.; Barnhart, H.; et al. Features and outcomes of 889 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015, 148, 1340–1352. [Google Scholar] [CrossRef] [PubMed]
- Chen, E.Y.; Baum, K.; Collins, W.; Löve, A.; Merz, M.; Olafsson, S.; Björnsson, E.S.; Lee, W.M. Hepatitis E masquerading as drug–induced liver injury. Hepatology 2012, 56, 2420–2423. [Google Scholar] [CrossRef] [PubMed]
- Aithal, G.P.; Watkins, P.B.; Andrade, R.J.; Larrey, D.; Molokhia, M.; Takikawa, H.; Hunt, C.M.; Wilke, R.A.; Avigan, M.; Kaplowitz, N.; et al. Case definition and phenotype standardization in drug-induced liver injury. Clin. Pharmacol. Ther. 2011, 89, 806–815. [Google Scholar] [CrossRef] [PubMed]
- BfArM (Bundesinstitut für Arzneimittel und Medizinprodukte, Bonn. Federal Institute for Drugs and Medicinal Products in Germany). Rejection of Drug Risks, Step II. As related to: Kava-Kava (Piper methysticum)-containing, and kavain-containing drugs, including homeopathic preparations with a final concentration up to, and including D4. 14 June 2002. Available online: http://www.spc.int/cis/documents/02_0714_BfArM_Kava_Removal.pdf (accessed on 12 March 2016).
- Teschke, R.; Schwarzenboeck, A.; Hennermann, K.H. Kava hepatotoxicity: A clinical survey and critical analysis of 26 suspected cases. Eur. J. Gastroenterol. Hepatol. 2008, 20, 1182–1193. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R. Kava hepatotoxicity: A clinical review. Ann. Hepatol. 2010, 9, 251–265. [Google Scholar] [PubMed]
- Kuchta, K.; Schmidt, M.; Nahrstedt, A. German kava ban lifted by court: The alleged hepatotoxicity of kava (Piper methysticum) of ill- defined herbal drug identity, lacking quality control, and misguided regulatory politics. Planta Med. 2015, 81, 1647–1653. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Frenzel, C.; Schulze, J.; Eickhoff, A. Spontaneous reports of primarily suspected herbal hepatotoxicity by Pelargonium sidoides: Was causality adequately ascertained? Regul. Toxicol. Pharmacol. 2012, 63, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Eickhoff, A.; Wolff, A.; Frenzel, C.; Schulze, J. Herbal hepatotoxicity and WHO global introspection method. Ann. Hepatol. 2013, 12, 11–21. [Google Scholar] [PubMed]
- Teschke, R.; Frenzel, C.; Wolff, A.; Herzog, J.; Glass, X.; Schulze, J.; Eickhoff, A. Initially purported hepatotoxicity by Pelargonium sidoides: The dilemma of pharmacovigilance and proposals for improvements. Ann. Hepatol. 2012, 11, 500–512. [Google Scholar] [PubMed]
- Teschke, R.; Glass, X.; Schulze, J. Herbal hepatotoxicity by Greater Celandine (Chelidonium majus): Causality assessment of 22 spontaneous reports. Regul. Toxicol. Pharmacol. 2011, 61, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Calitz, C.; du Plessis, L.; Gouws, C.; Steyn, D.; Steenkamp, J.; Muller, C.; Hamman, S. Herbal hepatotoxicity: Current status, examples, and challenges. Expert Opin. Drug Metab. Toxicol. 2015, 11, 1551–1565. [Google Scholar] [CrossRef] [PubMed]
| Patients | Final Diagnoses and Alternative or other Important Diagnoses | References |
|---|---|---|
| Case 1 | Final diagnosis | [9] |
| Decompensated liver cirrhosis by alcohol, AAP, or HEV; highly probable hepatitis E. | ||
| Decompensated liver cirrhosis of clinically unassessed etiology, preexisting and likely due to alcohol, acetaminophen, or HEV. HEV highly probable, suggested by high ALT values, lack of ALT dechallenge, and patient’s specific HEV risks. Presumably, physicians missed the tentative HEV diagnosis and effective antiviral drug therapy by ribavirin prior to OLT. | ||
| Alternative diagnoses | ||
| 1. Suspected acetaminophen hepatotoxicity, connected with alcohol use. | ||
| Acetaminophen hepatotoxicity and liver cirrhosis with alcohol as predisposing factor remained unconsidered by regulatory or clinical assessments, as was the possible specific treatment by N-acetylcysteine to circumvent ALF and OLT. | ||
| 2. Possible acute acalculous cholecystitis. | ||
| 3. Possible resolving acute hepatitis by CMV and VZV coinfection. | ||
| 4. Morbid obesity. | ||
| Case 2 | Final diagnosis | [9] |
| Acute liver failure by accidental chronic acetaminophen overdose. | ||
| This diagnosis was clinically missed, and timely specific therapy by N-acetylcysteine was not given which could have prevented OLT. In his liver histology report, the pathologist reminded the physicians that consideration of AAP toxicity is warranted, a suggestion the physicians did not seriously consider. Mainstream opinion suggests this kind of treatment in any case of acute liver failure, independent of the cause. Tentative probable causality for AAP. | ||
| Alternative diagnoses | ||
| 1. Acute liver failure by the known potentially hepatotoxic nonsteroidal antiinflammatory drug ibuprofen. | ||
| Tentative possible causality for ibuprofen, a known hepatotoxic NSAID. Some key features are poorly documented. | ||
| 2. Possible resolving acute EBV infection. | ||
| Documented are high anti-EBV IgG titers, suggesting a resolving acute EBV infection in which IgM has vanished. Titers of anti-EBV IgG were not followed in the further course to confirm or disprove the assumed resolving acute EBV infection. | ||
| 3. Possible, not sufficiently excluded hepatitis E. | ||
| High ALT values and clinical features are compatible with and suggestive of HEV infection. HEV exclusion is fragmentary and likely done using antibody tests that are not FDA approved due to overt problems of specificity and sensitivity. HEV PCR was not assessed in blood, stool, and the explanted liver. | ||
| 4. Morbid obesity. | ||
| Case 3 | Final diagnosis | [9] |
| Acute hepatitis by HBV and VZV coinfection. | ||
| The medical records substantiate the diagnosis of acute HBV and VZV coinfection: anti-HBs and anti HBc were positive; HBV immunization is not documented. Acute VZV hepatitis is ascertained by positive tests for anti-VZV IgM and IgG; microgranulomata are described in virus hepatitis including VZV. Both infections might have been occurred around or after June 2013. In June, the patient was on a trip in California for one week. Both diagnoses were missed, also potential therapy; prolonged clinical course under lacking therapy. Recovery was not documented in the files [9] and not published [5]. | ||
| Alternative diagnoses | ||
| 1. Acute cholecystitis. | ||
| Ultrasound and abdomen MRT presented results of a thickening of the gallbladder wall, according to assessors suggestive of cholecystitis with pericholecystic fluids and consistent with acute versus chronic gallbladder disease. Clinical signs including prolonged abdominal pains and prolonged increase of LTs are compatible with cholecystitis. No therapy is documented in the files. | ||
| 2. Possible DILI by acetaminophen. | ||
| 3. Obesity. | ||
| Case 4 | Final diagnosis | [9] |
| Acute HSV hepatitis due to genital herpes; acute cholecystitis with multiple gallbladder stones. | ||
| Clinical symptoms, high ALT values, liver histology, and antiviral HSV treatment by prolonged high dosed aciclovir therapy for genital herpes are suggestive of acute HSV hepatitis. | ||
| Alternative diagnoses | ||
| 1. Resolving acute CMV hepatitis. | ||
| Anti-CMV IgG titers increased with normal IgM titers, a constellation compatible with a resolving acute CMV infection where IgM had already disappeared. It was forgotten to determine IgG in the further clinical course with assessment of quantitative titers to evaluate titer changes. | ||
| 2. Acute hepatitis, preferentially by hepatitis E virus (HEV) infection (not yet excluded). | ||
| Liver histology suggests acute virus hepatitis and testing for HEV, but clinicians discounted this advice. | ||
| 3. Overweight. | ||
| Case 5 | Final diagnosis | - |
| Unlikely OEP hepatotoxicity. Possible hepatitis by HEV, EBV, HSV, or VZV, none yet excluded. | ||
| MedWatch report did not specify that one of these infections were ruled out. Limited data from MedWatch report, not reported by a physician but by a pharmacist. Raw clinical and case data were not provided by the QMC. | ||
| Alternative diagnoses | ||
| 1. Fatty liver. | ||
| Diagnosis based on CT report. | ||
| 2. Unspecified pain syndrome. | ||
| Question of additional, yet undeclared pain medication. | ||
| 3. Obesity. | ||
| Case 6 | Final diagnosis | - |
| Undetermined due to lack of raw data. | ||
| Raw clinical and case data were not provided by the QMC. | ||
| Alternative diagnoses | ||
| 1. High alcohol consumption. | ||
| Alcohol use: up to 10–12 beers per occasion. | ||
| 2. HEV not excluded. | ||
| Anti-HEV IgM, anti-HEV IgG, and HEV PCR not assessed. | ||
| 3. Obesity. | ||
| Case 7 | Final diagnosis | - |
| Undetermined due to uncertainty of used product. | ||
| Uncertainty about the used DS does not allow a causal attribution to any DS (Table 4): Oxy Cleanse (OC) or OxyELITE Pro (OEP). The probable causality initially claimed for OEP by the QMC physicians [5] cannot be accepted as valid any more due to unjustifiable upgrading of the causality levels of all eight QMC patients including this case 7, as admitted at a trial [9]. As an exclusion diagnosis, a thorough exclusion of other potential causes was not done and not documented in the analyzed medical records. | ||
| Alternative diagnoses | ||
| 1. Suspected hepatitis by varicella zoster virus (VZV) infection. | ||
| Anti-VZV IgG was positive, but titer changes in the further course were not assessed. VZV PCR was not assessed in the blood and in the liver at autopsy. | ||
| 2. Suspected hepatitis E virus (HEV) infection. | ||
| HEV remained unconsidered by the QMC physicians. HEV PCR was not done in blood, stool, and the liver at autopsy. Anti-HEV IgM and IgG antibodies were not determined, not with FDA unapproved or approved HEV antibody tests. | ||
| 3. Suspected Wilson disease (WD). | ||
| WD is a known cause of ALF, which was not carefully excluded by QMC physicians. | ||
| 4. Obesity. | ||
| Case 8 | Final diagnosis | [6] |
| Recurrent toxic hepatitis by naproxen (Aleve) overdose 8–9/2013 and 4/2014, with lacking causality for dietary supplements including both OEP products. | ||
| Alternative diagnoses | ||
| 1. Acute acalculous cholecystitis associated with gallbladder sludge. | ||
| Suggested by clinical symptoms and imaging data. | ||
| 2. Acute hepatitis, preferentially suspected hepatitis E virus infection (not yet excluded). | ||
| HEV not considered as potential cause. | ||
| 3. Nonalcoholic fatty liver disease (NAFLD) due to morbid obesity with BMI 40–45 kg/m2. | ||
| 4. Suspected DILI by one of the abundant used synthetic drugs. | ||
| 5. Well documented multimorbidity. | ||
| 6. Chronic pain syndrome, headaches, and intractable migraine. |
| Product | Main Ingredients * | Other Ingredients * | Total Weight |
|---|---|---|---|
| Old OEP: OxyELITE Pro | Caffeine (100 mg), Bauhinia purpurea L. Extract, Bacopa Monnieri Extract, 1,3-Dimethylamylamine HCl (20 mg), Cirsium Oligophyllum Extract, Yohimbe Extract | Modified Starch, Gelatin, Vegetable Stearate, Silicon Dioxide, Red 3, Blue 1, Red 40, Titanium Dioxide Color | 1 capsule: 380 mg |
| New OEP (I): OxyELITE Pro New Formula | Caffeine (135 mg), Bauhinia purpurea L. Extract, Aegeline (40 mg), Norcoclaurine HCl, Hemerocallis fulva Extract, Yohimbe Extract | Modified Starch, Gelatine, Vegetable Stearate, Silicon Dioxide, Red 3, Blue 1, Red 40, Titanium Dioxide Color | 1 capsule: 405 mg |
| New OEP (II): OxyELITE Pro Advanced | Caffeine (100 mg), Cynanchum auriculatum Extract, Olea Europaea Extract, Aegeline (50 mg), Yohimbe Extract, Coleus Forskohlii Extract | Gelatine, Modified Starch, Silicon Dioxide, Vegetable Magnesium Stearate, Red 3, Blue 1, Red 40, Titanium Dioxide Color | 1 capsule: 460 mg |
| New OEP (III): OxyELITE Pro Super Thermo | Choline Bitartrate, l-Carnitine-Tartrate, Caffeine (125 mg), Aegeline (90 mg), Norcoclaurine HCl, Yohimbe Extract, Oleoylethanolamide, Eriobotrya Japonica Extract | Malic Acid, Silicon Dioxide, Sucralose, Acesulfame Potassium, natural and artificial Flavors | 1 Scoop: 2167 mg |
| Patients | Narratives | References for Additional Details |
|---|---|---|
| Case 1 Male, 22 years | Narrative | [9] |
| Patient with liver cirrhosis and ascites of clinically unassessed etiology but possibly related to alcohol or acetaminophen use, or HEV. Significant outdoor activities with HEV risk: hunter, wild hog meat consumer, and coffee farmer. History of illicit drug and heavy alcohol use/abuse some years ago, with present monthly use of 6–12 beers or a 6 pack of beer and 1–2 shots of hard liquor each time the patient drank. First symptoms of illness emerged within 24 h after a restaurant meal. At hospital admission on 25 August 2013: ALT 1970 U/L, AST 1308 U/L, ALP 107 U/L, and bilirubin 33.6 mg/dL. Significant PMH (Table 5). Documented prior use of synthetic drugs (Table 6). Additionally, acetaminophen-oxycodone in early 2013 for pain in neck and paresthesia in the arm, possibly an early extrahepatic, neurological manifestation of HEV myelitis with polyradiculopathy, bilateral brachial neuritis, or peripheral neuropathy, which can overshadow the liver injury. Use of overall 14 DS’s (Table 5): old OEP use for one year, intermittently on an off and on basis and stopped 3 weeks prior to admission; subsequently, new OEP, Amplified Wheybolic Extreme-60, and Versa-1, all used for only one week until symptoms emerged two weeks prior to admission, unlikely causes of decompensated liver cirrhosis and ALF due to short duration of use. | ||
| Clinical features and laboratory results are highly suggestive of HEV infection, but lacking results of HEV PCR and anti-HEV IgG; invalid negative anti-HEV IgM as assessed by a test that is not FDA approved. Negative anti-CMV IgM and anti-VZV IgM. Positive anti-CMV IgG and anti-VZV IgG without assessed IgG titer changes in further course; possibly resolving acute hepatitis by CMV and VZV coinfection. ALT decrease not continuously straight but variable and undulating with intermittent spikes, possibly caused by limited HEV episodes or intermittent acute cholecystitis bouts. Positive Murphy sign, imaging data with up to 1 cm thickening of the gallbladder wall and surrounding fluids, suggestive of acute acalculous cholecystitis with discussed surgical consultation. Patient required OLT: decompensated liver cirrhosis with ascites, confirming prior CT result. Explanted liver not assessed for HEV PCR. After OLT, increased LTs by rejection or HEV episodes. | ||
| Causality assessment: Poor case data quality. Used algorithm applicable only to acute and not chronic liver injury such as decompensated liver cirrhosis. Tentative excluded causality for old and new OEP, all additional DS’s, and AAP. Intermittent use of old OEP and the large interval of 2–3 weeks from stop to admission impedes a valid assessment of the natural dechallenge course of ALT. Diagnoses: Decompensated liver cirrhosis by alcohol, AAP, or HEV; highly probable hepatitis E. | ||
| Case 2 Female, 31 years | Narrative | [9] |
| Patient with initial admission on 25 August 2013 and later transferal to the liver transplantation center due to ALF with liver transplantation on 9 September 2013. The day prior to admission: ALT 1416 U/L, AST 936 U/L, ALP 107 U/L, bilirubin 7.9 mg/dL. Two week history of vomiting and inability to eat prior to admission, yellowing of her eyes. Significant PMH (Table 6). Use of multivitamins, multiple DS’s including possibly OEP (Table 5), also multiple synthetic drugs and phentermine (Table 6). | ||
| High titers for anti-EBV IgG, suggestive of resolving acute EBV infection with already normal IgM; anti-EBV IgG titers not assessed in the further course to confirm the resolving EBV infection. Anti-HEV IgM and IgG negative, but applied antibody tests not described with their characteristics of sensitivity and specificity. HEV PCR not done in blood, stool, and liver. Upon ultrasound examination, initially some intrahepatic biliary duct dilatation in the right hepatic lobe and about the gallbladder fossa, but not persisting. Liver histology: Massive confluent necrosis, the etiology of the acute liver failure is uncertain, but consideration of acetaminophen (AAP) toxicity is warranted given the patient’s history of gastric sleeve/gastric bypass procedure—a known risk factor for such toxicity. | ||
| Causality assessment: Insufficient data quality. Excluded causality for new OEP, phentermine, multivitamins, and various DS’s, probable for acetaminophen, possible for ibuprofen, and likely for the multiple unidentified headache medicines. Diagnosis: Acute liver failure by accidental chronic overdosed acetaminophen. | ||
| Case 3 Female, 43 years | Narrative | [9] |
| The patient used several drugs (Table 6), including ferrous sulfate in 6–7/2013: prescription is well documented, but not the indication, likely blood-loss-related anemia of unknown etiology. On 12 June 2013, start with 50 doses of tramadol-acetaminophen with unknown daily dose and duration, likely for pain relief, which may have emerged as initial symptoms of the later established acute hepatitis by HBV and VZV coinfection. Normal blood tests in 7/2013 claimed, but details not documented. On 12 August 2013, admission with diagnosis of obstructive jaundice, anemia, and abnormal LTs. Subsequent diagnoses included acute liver failure (lacking criteria), hepatitis, or simple transaminitis. OEP use was mentioned only late in the clinical course. Inconsistently described use of new OEP for 3 or 6 weeks, or a couple of months, possible prior use of old OEP for 3 and 2 years; proof of purchase not documented, also no documentation in the PCP files. On admission, AST 736 U/L, ALT 636 U/L, ratio AST/ALT constantly >1, ALP 156 U/L, and bilirubin 6.5. Hgb 9.9 g/dL, cholesterol 272 mg/dL, BMI 33 kg/m2. Without specific treatment, her liver values failed to decline, as ALT was with 867 U/L on 30 November 2013 even higher than at admission, suggesting ongoing hepatitis. Unclear outcome in face of missed diagnosis and lacking specific therapy. | ||
| Imaging report suggests acute versus chronic gallbladder disease. Immunization records: empty. Hepatitis B serologies obtained after admission and later establish acute hepatitis B virus infection: anti-HBs were twice positive within 4 weeks, while anti-HBc undulated and was positive, negative, and finally negative/positive. Hepatitis B surface antigen was already negative. Coinfection with acute VZV infection, confirmed by positive anti-VZV IgM and IgG. Anti-HEV IgM negative by a kit from Focus Diagnostics that has not been approved by the FDA. HEV PCR assessment was not done in blood or stool. Liver histology includes microgranulomata and shows acute confluent necrosis. | ||
| Causality assessment: Excluded causality for old and new OEP, unlikely for ferrous sulfate, possible for AAP, and excluded for additional drugs. Diagnosis: Acute hepatitis by HBV and VZV coinfection. | ||
| Case 4 Female, 54 years | Narrative | [9] |
| Symptoms started with pruritus on 18 May 2013 and progressed to jaundice, dark urine, nausea, stomach pain, and rash, before LTs were assessed. On 6 December 2013: ALT 1750 U/L, AST 1847 U/L, ALP 190 U/L, bilirubin 14.1 mg/dL. ALT declined slowly, undulating and with spikes, suggesting some hepatitis or cholecystitis episodes. Documented multimorbidity (Table 5) and multimedication (Table 6). Documented use of OEP and abundant herbs and DS’s. After the liver illness, this patient continued to purchase dietary supplements, including new OEP in 9/2013 as well as Hydroxycut, which might have been used also before. Prolonged and high dosed aciclovir therapy, genital herpes as likely origin of HSV hepatitis. | ||
| Abdominal ultrasound with contracted gallbladder and wall thickness of 8 to 9 mm, multiple stones, or sludge. Negative Murphy sign. MRCP: spleen 10.8 cm, trace periscystic fluid and ascites. Autoimmune parameters negative. Negative results for anti-HAV IgM, anti-HAV total, Monoscreen EBV antibody test, HBsAg, anti-HBc IgM, and anti HCV; HBV and HCV PCR not done. Anti-CMV IgM negative, anti-CMV IgG positive but titer changes in the further course not assessed. HEV, HSV, and VZV not assessed. Liver histology report mentions severe cholestasis and that the most likely etiologies include adverse drug reaction, acute viral hepatitis, and AIH, testing for HEV can be considered. | ||
| Causality assessment: Excluded causality for the old and new OEP and many additional DS’s, unlikely for drugs including AAP. Diagnosis: Acute HSV hepatitis due to genital herpes; acute cholecystitis with multiple gallbladder stones. | ||
| Case 5 Female, 34 years | Narrative | - |
| Patient with two weeks nausea, decreased appetite, mild epigastric pain, brown urine and jaundice. On 2 June 2013, ALT 1244 U/L. Consumed an unspecified OEP product with an unknown dose for 3 months. Used product was not available for evaluation. OEP use in combination with linoleic acid and General Nutrition Corporation (GNC) protein shakes. Prolonged clinical course [5], suggestive of an infection by a not yet excluded hepatitis virus. Report from a pharmacist with vague and limited information. Pain medication (Table 6). | ||
| Causality assessment: For OEP: challenge + 2 points, for dechallenge due to lack of information and long time interval between stop of use and first ALT value 0 points, for DS comedication −1, for insufficient exclusion of alternative causes +1, total +2 points corresponding to an unlikely causality, not considering possible alternative causes of virus infections by HEV, EBV, HSV, or VZV, none yet excluded (Table 1). Diagnosis: Unlikely OEP hepatotoxicity. Possible hepatitis by HEV, EBV, HSV, or VZV, none yet excluded. | ||
| Case 6 Female, 35 years | Narrative | - |
| No raw data available, limited access to other data. Alcohol use: up to 10–12 beers per occasion. | ||
| Causality assessment: Not done. Diagnosis: Undetermined due to lack of raw data. | ||
| Case 7 Female, 48 years | Narrative | - |
| This patient reported prior use of Oxy Cleanse (OC) as documented in the medical charts at hospital admission (Table 4). Significant PMH (Table 5) with prior use of various synthetic drugs (Table 6). Upon our reassessment of her case files, we found that she had a localized cancer of the left breast. This diagnosis remained undisclosed in the QMC case report [5]. Our analyses revealed that OLT was refuted due to her malignancy and in fact was not performed, well documented in the medical records of the QMC. This was not attended to by the QMC physicians, who stated in their case report that the patient did receive an OLT [5]. | ||
| The patient initially received NAC which could have altered the natural ALT course after product cessation and impeded assessment of dechallenge. She was diagnosed with ALF, which she survived for 17 days [5]. Hospital admission with prior symptoms for about 3 weeks: nausea, vomiting, diarrhea and flu-like symptoms, so gastroenteritis was initially suspected. The patient has been on OEP for 3–6 weeks according to variable statements in the files, but the exact date of beginning OEP remained undisclosed. During OEP use, she experienced a dramatic weight loss of 1 pound daily, which persisted when she terminated OEP use on 7 September 2013, possibly caused by preexisting or developing liver disease. On 22 September 2013, ALT 986 U/L. Dechallenge ALT features as key diagnostic items were not assessable since first laboratory values were obtained only on 22 September 2013, two weeks after cessation. Despite OC or OEP cessation, synthetic hepatic dysfunction deteriorated in the further clinical course associated with a lack of clinical improvement. These conditions may indicate that the ALF was not due to OC or OEP but causally related otherwise. As an example, WD and HEV were not excluded, and claims that acute VZV was excluded were not substantiated by negative VZV IgM in face of positive IgG. Good alternative diagnoses may include WD, HEV, and acute VZV; for all these three diseases effective therapies exist. | ||
| Causality assessment: Regarding OC or OEP use, inconsistencies are documented in the files. First, it is unclear whether OC was consumed rather than OEP. For OEP, there is no documented proof of product purchase in a regular shop versus via internet. After her death, claims focused on two bottles of OEP that were found, one was empty and the other one was sealed. However, she might not have lived alone in her apartment/house, and it is not clear whether these two bottles were those of the patient. Documented in the files is also that she was not the only one in the family who used OEP. There is also the documentation that she distributed OEP to other family members, none of these were reported as becoming sick. Therefore, retrospect assessment of her OC or OEP use is difficult and disputed. Diagnosis: Undetermined due to uncertainty of used product. | ||
| Case 8 Female, 34 years | Narrative | [6] |
| Increased aminotransferases since 5 September 2013 of initially undetermined etiology. Her significant PMH (Table 5) included chronic multipain syndrome with headaches and intractable migraine is also well documented in the files, with headaches originating in her childhood. Consequently, an abundancy of pain medications is documented which included the hepatotoxic NSAID naproxen and previous multimedication (Table 6). As a typical NSAID, naproxen is known for its potential hepatotoxicity. The usual dose is 250–500 mg taken orally twice a day. As recommended by her physician, the patient took naproxen at daily overdoses of at least 1500 mg, and this treatment now was identified as culprit of her liver disease. Actually, five months after the first disease onset, overdosed naproxen was reused to treat daily headaches for a month, and this treatment again caused scleral icterus as at the first disease bout, confirming this drug as the causative agent. | ||
| Assessing conditions are further complicated by the use of multiple DS‘s including OEP (Table 4). The patient stopped the use of new OEP, because she was feeling unwell, possibly at around 3 September 2013 when she first noted dark urine and experienced symptoms of fatigue, nausea, abdominal pain, and anorexia, followed by jaundice of her skin and eyes on 7 September 2013. At first presentation to her PCP on 5 September 2013, her LTs were increased, with ALT 633 U/L, AST 329 U/L, ALP 123 U/L, and bilirubin 1.4 mg/dL. In the further course of the disease, ALT values were variable in a range between 105 U/L and 794 U/L, which represented a second peak, and normalized within 84 days on 1 December 2014. The variable ALT values are suggestive of an ongoing liver disease; of hepatitis E, which was forgotten to be excluded; of a not yet resolved acute acalculous cholecystitis with gallbladder sludge, which was suspected on clinical grounds, the positive Murphy sign, and the ultrasonic description of an abnormal appearance of the thickened gallbladder wall; of the action of still used synthetic drugs. Reuse of the new OEP was reported on 19 September 2013, but concurrent use of potentially hepatotoxic synthetic medications, with their documented discontinuation only on 30 September 2013, impedes a valid assessment; in particular, the claimed positive reexposure test result for OEP is not substantiated due to these confounding variables. | ||
| Causality assessment: Unlikely and excluded causality for new and old OEP, excluded for the other DS’s. Lack of appropriate drug use details impedes a valid assessment of causality for most drugs. Diagnosis: Recurrent toxic hepatitis by naproxen overdose. |
| Patients | Documented or Assumed Use of Dietary Supplements | References |
|---|---|---|
| Case 1 | Used overall 14 DS’s, with some information for 4 DS’s: old OEP use for one year, intermittently on and off basis, and stopped 3 weeks prior to admission; subsequently, new OEP, Amplified Wheybolic Extreme-60, and Versa-1 were used for only one week until symptoms emerged two weeks prior to admission. According to purchase records and additional medical records, he consumed since March 2013 prior to liver illness these 10 DS’s: Pro Performance AMP Wheybolic Extreme 60, CLK with Conjugated Linoleic Acid (CLA)/ Super Hd Combo Kit; Ripped Freak; Kre-Alkalyn EFX; Pump-HD; Green Coffee Bean; Super HD; CLK; and Beyond Raw Chocolate Re-Grow. | [9] |
| Case 2 | Documented that the patient mentioned multivitamins prescribed by her PCP, but denied despite multiple specific questionings use of any DS at numerous occasions prior to OLT. There is also a note that she might have used new OEP for 3 or 6 weeks or a couple of months, possibly also since beginning of July 2013 and until two weeks before admission (vomiting, inability to eat) and phentermine for weight loss. Consumers purchase documents for OEP were not provided. The purchase records and medical records only support the consumption of the following DS’s prior to liver illness: Mega Men Perform & Vitality; Mega Men Sport Vitapak; Amino Energy; Stby Isopure; and Alph Isopure. No customer purchase records for OEP available. The information on this case as documented in the clinical records is inconsistent, fragmentary, and difficult to assess since it appears that the patient did not tell correct details; results of this assessment are therefore tentative. | [9] |
| Case 3 | OEP use was mentioned only late in the clinical course. Inconsistently described use of new OEP for 3 or 6 weeks, or a couple of months, possible prior use of old OEP for 3 and 2 years; proof of purchase not documented, also no documentation in the PCP files. | [9] |
| Case 4 | Regarding documented use of herbs and DS’s, she has been on numerous undefined herbal supplements for months. This patient’s medical history states that the patient was taking the DS Amberen, Garcinia cambogia, Super HD, Raspberry Ketone Chews, Vita Chews, and HCA Supreme. The medical records also noted that the patient may have taken some other DS’s, but she does not know the names of all of these. At the time of illness, the patient reported being on multiple undefined herbal supplements for months. The purchase history of DS’s before the liver illness includes not only OEP but also Vitamin Code Raw Calcium, Mega V products energy products, Hydro Pure, Amp 100% Whey Protein, Pre-Diet Cleanse, Meta Ignite, R3 Extreme Chrome, C4 Xtreme Blue, CLK, Compound 20, and many others. After the liver illness, this patient continued to purchase dietary supplements, including new OEP in 9/2013 as well as Hydroxycut, which she might have used also before, Total Body Rapid Cleanse Renew, Keto-Xt, and Premium Detox 7 day Cleanser. | [9] |
| Case 5 | Used unspecified OEP product for 3 months in combination with conjugated linoleic acid and GNC protein shakes. | - |
| Case 6 | No raw data available. Used Alli (Orlistat). | - |
| Case 7 | Medical records of the QMC documented in the beginning of the hospital stay that the patient reported the use of Oxy Cleanse (OC). Following discussion of OEP in the media and along with the upcoming OEP discussions in the media and QMC physicians with their patients, the DS used switched from Oxy Cleanse to the similar word OxyELITE Pro in the medical records. Purchase documents were not provided by the patient and her family members. At court, this uncertainty remained. This was not outlined in the QMC publication, which claimed OEP use and assessed causality for this DS and not for OC [5]. | - |
| Case 8 | Documentation of DS use prior and subsequent to disease onset is inconsistent but includes four different DS’s at different times and in different combinations. Among these are GNC bleaching protein powder and GNC woman’s active multivitamin, which were taken each for at least 2.5 years without any side effects, but the date of cessation is not documented. In addition, the well tolerated use of the first OEP product, the old OEP, is documented for approximately 2.5 or 3 years with reported cessation sometime in 7/2013 and switching to a second OEP formula, the new OEP. The patient stopped the use of the new OEP, because she was feeling unwell, possibly at around 3 September 2013 when she first noted dark urine and experienced symptoms of fatigue, nausea, abdominal pain, and anorexia, followed by jaundice of her skin and eyes. | [6] |
| Patients | Documented Prior and Present Diseases | References |
|---|---|---|
| Case 1 | Asthma, suspected prior alcohol abuse, suspected cervical spinal syndrome or neurological HEV prodromi, atopia, fungal infections on both feet. Morbid obesity, BMI maximum 42.9 kg/m2. | [9] |
| Case 2 | Bariatric surgery for morbid obesity, fatty liver, asthma (as child), hypertension, kidney stones left side, ovarian cyst right, cholecystolithiasis, laparoscopic cholecystectomy, choledocholithiasis-sphincterotomy, migraine, fracture right ring finger, treatment with ibuprofen, disc bulges. Morbid obesity, BMI 47 kg/m2. | [9] |
| Case 3 | Unspecified pain syndrome, treated by AAP. At admission: anemia. Obesity, BMI 33 kg/m2. | [9] |
| Case 4 | Morbidities include recurrent HSV infections, gallbladder stones, essential hypertension, menopause, hypercholesterolemia, insomnia, mild cataracts, polyp in rectum, pseudomelanosis coli, anxiety, migraine, cancer of left breast, with local simple mastectomy. Overweight, 25.6 kg/m2. | [9] |
| Case 5 | Asthma. Unspecified pain syndrome. Obesity. | - |
| Case 6 | No raw data available. Alcohol abuse with 10–12 beers at an occasion. Obesity. | - |
| Case 7 | Remote methamphetamine use and alcohol abuse. Documented are earlier multiple hair and urine tests. Obesity. For the past decades, multiple injuries and illnesses are documented in the files, including multiple staphylococcus abscesses, E. coli in the blood, disc disease at L4–5 and L5–S1, left shoulder impingement syndrome, acromioplasty. Documented as Problem List includes: Nail avulsion of finger, laceration, open FX finger, train of lumbar region, Tinea pedis, Acne, strain of the knee, lump breast, current tear knee, medial meniscus, arthralgia of knee, contusion of the chest, and abrasion of back. Obesity, BMI 31.7 kg/m2. | - |
| Case 8 | Morbid obesity, nonalcoholic fatty liver disease (NAFLD); attention deficit hyperactivity disorder (ADHD); schizophrenia; chronic pain syndrome, headaches, migraine (intractable); phobia; epilepsy and recurrent seizures; asthma; chronic otitis externa right ear; obstructive sleep apnea syndrome; latent tuberculosis; multiple tattoos; kidney stones; menorrhagia; esophageal reflux; lumbar disc degeneration; surgical history of insert posterior spine process distract device, spinal cord stimulator, laminectomy decompressive up to two lumbar segments; two surgeries L3–4, L4–5, L5–L1; partial meniscectomy left knee; and others. Morbid obesity, BMI 40–45 kg/m2. | [6] |
| Patients | Documented Past and Current Medication | References |
|---|---|---|
| Case 1 | Inhalation and synthetic medications for asthma. Vicodin (acetaminophen-hydrocodone), Percocet (acetaminophen-oxycodone); Bactrim (Trimethoprim and Sulfamethoxazole). | [9] |
| Case 2 | Tylenol (acetaminophen) contained in an empty bottle found in her car, large amounts of ibuprofen, possibly other unidentified drugs or DS’s, lacking any further details. “Lot of unidentified medications for headaches”. | [9] |
| Case 3 | Before onset: acetaminophen-tramadol, 50 doses; ferrous sulfate. After onset: Amoxicillin, ibuprofen, clarithromycin, omeprazole, and promethazine. | [9] |
| Case 4 | Aciclovir high dosed, lisinopril, hydroxyzine hydrochloride. Obviously numerous drugs, insufficiently documented. | [9] |
| Case 5 | Fluticasone/salmeterol 1 puff twice daily. Hydromorphone I mg injection as needed for pain. | - |
| Case 6 | No raw data available. | - |
| Case 7 | Previous drug use as documented in the medical and insurance files included baclophen, diclofenac, acetaminophen, Tylenol, Xanax, Benadryl, cephalexin, but no use of new medications was reported at admission. | - |
| Case 8 | Naproxen, ibuprofen, ritalin, hydrocodone-acetaminophen, diazepam, claritin, and omeprazole. Documented allergies by aspirin, celebrex, celeXa, doxycycline, NSAIDs, and penicillins. | [6] |
| Data | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 |
|---|---|---|---|---|---|---|---|---|
| HAV | Anti-HAV IgM negative. | Anti-HAV IgM negative. | Negative result for anti-HAV total. | Anti-HAV total and IgM negative. | Reported as excluded, but no details provided. | n.a. | Anti-HAV IgM negative and total positive. | Anti-HAV IgM negative. |
| HBV | Anti-HBs positive, HBV vaccination documented. | Excluded. | Positive tests for anti-HBc and anti-HBs: later stage of acute HBV infection. | Incompletely excluded, missing PCR data. | Reported as excluded, but no details provided. | n.a. | Anti-HBc IgM negative. HBs antigen negative. Anti HBs negative and later positive. Not documented: immunization. | Anti-HBc negative; HBs Ag negative; Anti-HBs positive; no immunization (patient’s refusal). |
| HCV | Excluded. | Excluded. | Excluded. | Incompletely excluded, missing PCR data. | Reported as excluded, but no details provided. | n.a. | Excluded. | Anti-HCV negative; HCV PCR n.a. |
| HEV | Anti-HEV IgM negative; anti-HEV-IgG and HEV PCR n.a. | Anti-HEV IgM and IgG negative. | Anti-HEV IgM negative reported at a single time point late in the clinical course. Anti-HEV IgG and HEV PCR n.a. | n.a. | n.a. | n.a. | n.a. | n.a. |
| CMV | Anti-CMV IgG positive without assessed titer changes in the further course; anti-CMV negative. | Excluded. | Excluded. | Incompletely diagnosed, anti-CMV IgG with high titer, lacking titer change follow up. | Reported as excluded, but no details provided. | Anti-CMV IgG positive. | Anti-CMV IgM negative; CMV DNA <200 | Anti-CMV IgM negative. |
| EBV | Excluded. | Anti-EBV IgG with high titer, subsequent titer changes not evaluated, anti-EBV IgM negative. | Excluded. | Monoscreen negative. | n.a. | n.a. | Excluded. | Anti-EBV IgM negative, anti-EBV IgG positive but no follow up of titer change. |
| HSV | Excluded. | Excluded. | Excluded. | Not done. | n.a. | n.a. | Excluded. | n.a. |
| VZV | Anti-VZV IgG positive without assessed titer changes in the further course; anti–CMV IgM negative. | Excluded. | Anti-VZV IgM and IgG, both positive. | Not done. | n.a. | n.a. | Anti-VZV IgM n.a., anti-VZV IgG positive without assessed titer changes in the further course. | n.a. |
| Report | Major Confounding Variables Presented as Examples | Additional References |
|---|---|---|
| CDC, 2013 [3] | 1. Type of incriminated OEP product is not identified and confounds assessments. | [6,9] |
| 2. Lacking details of patients’ interviews, and questionnaires and their analyses. | ||
| 3. Vague case definition, not in line with mainstream clinical hepatology. | ||
| 4. Unclear how negative evaluation of infections including viral hepatitis was achieved. | ||
| 5. Lacking specific and valid exclusion of HEV infection. | ||
| 6. Unclear how preexisting autoimmune hepatitis, chronic alcohol use, and chronic liver diseases were excluded. | ||
| 7. Concomitant use of multiple DS’s as confounders and lacking causality assessment for each used DS. | ||
| 8. Missing reported use of a liver-specific causality assessment such as RUCAM. | ||
| 9. Patients were declared as previously healthy, ignoring documented PMH of significant diseases. | ||
| NEJM, 2014 [4] | 1. Upgrading of FDA case numbers by adding non-liver cases to liver cases is a problematic approach and confounds the Perspective article of the NEJM. | [6,9] |
| 2. Assumed liver cases were not stratified for a specific OEP product. | ||
| 3. The claimed case cluster remained unverified since criterion of one product causing one disease was not satisfied. Patients used two different types of OEP products, many different DS’s, and many different drugs, which confound the cluster concept. This is also not supported as patients experienced not a single type of liver disease but many different ones. | ||
| QMC, 2014 [5] | 1. Biased case evaluations, triggered by initial unsubstantiated claims that OEP is hepatotoxic, and premature search for publicity. | [6,9] |
| 2. Willingly upgrading of causality levels to “probable” causality to let cases appear stronger and suitable for publication, circumventing rejection. | ||
| 3. Case data manipulations invalidate conclusions of the publication and biased case assessment by regulators such as CDC, HDOH, and FDA. | ||
| 4. Neither criteria for case inclusion nor stringent diagnostic protocol at the QMC were provided. | ||
| 5. PMH incompletely presented. | ||
| 6. OLT was erroneously described in one patient (case 7) who never was transplanted according to our review of medical files. | ||
| 7. Most patients were polymedicated by synthetic drugs, not reported in the publication. | ||
| 8. The high number of DS’s used by most patients remained unpublished. | ||
| 9. Case 3 was reported as remaining on the transplantation list for over five months without mentioning that this patient had an acute hepatitis by HBV and VZV coinfection (positive anti-HBs, positive anti-HBc, and positive anti-VZV IgM and IgG), not recognized and treated by QMC physicians. | ||
| 10. Lack of a prospective clinical and causality evaluation. | ||
| 11. Failure to establish and evaluate a control group. | ||
| 12. Selective data presentation in the published report with substantial gap between documented case details and published data with suppression of data not supporting initial claims regarding OEP. | ||
| 13. Use of the outdated RUCAM instead of the updated version. | ||
| 14. Significant misconception of RUCAM assessment for challenge and dechallenge criteria. | ||
| 15. Neglect of individual RUCAM assessment patient by patient, DS by DS, drug by drug, herb by herb, and item by item. | ||
| 16. Publication of four different liver histology cross-sections without attribution to specific patients. | ||
| 17. Before evaluation, the pathologists were told that the patient used OEP, which impeded an unbiased evaluation. | ||
| 18. Rarely valid exclusion of Wilson disease. | ||
| 19. Invalid exclusion of HEV in all QMC cases. Lacking HEV PCR use and application of HEV antibody tests, not approved by the FDA. | ||
| HDOH, 2015 [8] | 1. Confounders are vague case definitions, outside mainstream clinical hepatology. | [6,9] |
| 2. Presented illustrative cases 1 and 2 showed poor case data quality and unprofessional analysis with major confounding variables. | ||
| 3. Irritating statements on “probable” cases, not connected with RUCAM scoring, confound and lead to confusion. | ||
| 4. Comorbidity in half of the cases confounds valid case assessments. | ||
| 5. Alcohol consumption as is described as confounding variable but remained unconsidered for case assessment. | ||
| 6. OEP was used together with another DS by 22/36 patients, not considered as confounders in case assessment and not provided with individual causality gradings for OEP and the other DS’s. | ||
| 7. High frequency of concomitant use of hepatotoxic drugs such as acetaminophen or NSAIDs in 31/44 cases. | ||
| 8. Probable causality for unidentified OEP product by RUCAM assessment in only10/36 cases, whereas in the overwhelming majority clinically relevant causality levels were not established. | ||
| 9. For RUCAM assessment, only OEP was considered, not the other DS’s, herbs and drugs used concomitantly. | ||
| 10. Not accounting for any comedication as possible cause of DILI or HILI confounds case assessments. | ||
| FDA, 2015 [7] | 1. MedWatch reports are at risk being incomplete and confounded if not submitted by the caring physicians but provided by patients, their family members, or other non-physicians. | [6,9] |
| 2. MedWatch system confounds assessment of most HILI and DILI cases. | ||
| 3. MedWatch reports commonly provide high case numbers of low quality. | ||
| 4. The FDA publishes hepatotoxicity cases, not considering mainstream case criteria. | ||
| 5. Causality assessment ignores the use of a liver-specific, validated, and quantitative causality assessment algorithm such as RUCAM. | ||
| 6. The FDA avoids presentation of causality gradings for each suspected product and instead relies on high case numbers. | ||
| 7. The FDA claimed having reviewed patients’ records but overlooked many alternative diagnoses documented in the files. | ||
| 8. The FDA seemed to rely on the statements of the QMC physicians and thereby promoted their biased conclusions. | ||
| 9. The FDA did not realize the willingly and unjustifiable upgrading of causality levels by the QMC physicians, which represents not just a misadventure but a scientific fraud. |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Teschke, R.; Eickhoff, A. The Honolulu Liver Disease Cluster at the Medical Center: Its Mysteries and Challenges. Int. J. Mol. Sci. 2016, 17, 476. https://doi.org/10.3390/ijms17040476
Teschke R, Eickhoff A. The Honolulu Liver Disease Cluster at the Medical Center: Its Mysteries and Challenges. International Journal of Molecular Sciences. 2016; 17(4):476. https://doi.org/10.3390/ijms17040476
Chicago/Turabian StyleTeschke, Rolf, and Axel Eickhoff. 2016. "The Honolulu Liver Disease Cluster at the Medical Center: Its Mysteries and Challenges" International Journal of Molecular Sciences 17, no. 4: 476. https://doi.org/10.3390/ijms17040476
APA StyleTeschke, R., & Eickhoff, A. (2016). The Honolulu Liver Disease Cluster at the Medical Center: Its Mysteries and Challenges. International Journal of Molecular Sciences, 17(4), 476. https://doi.org/10.3390/ijms17040476