The Impact of Nonalcoholic Fatty Liver Disease on Renal Function in Children with Overweight/Obesity
Abstract
:1. Introduction
2. Results
2.1. Clinical and Laboratory Data from the Study Population
2.2. Findings in Children with Biopsy-Proven Nonalcoholic Fatty Liver Disease (NAFLD)
3. Discussion
4. Materials and Methods
4.1. Study Subjects
4.2. Laboratory Mmeasurements
4.3. Liver Ultrasound Eexamination and Magnetic Resonance Imaging
4.4. Liver Biopsy
4.5. Definitions
4.6. Statistical Analysis
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Vanni, E.; Marengo, A.; Mezzabotta, L.; Bugianesi, E. Systemic complications of nonalcoholic fatty liver disease: When the liver is not an innocent bystander. Semin. Liver Dis. 2015, 35, 236–249. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, R.; Mitra, A. An overview of effective therapies and recent advances in biomarkers for chronic liver diseases and associated liver cancer. Int. Immunopharmacol. 2015, 24, 335–345. [Google Scholar] [CrossRef] [PubMed]
- Schwimmer, J.B.; Pardee, P.E.; Lavine, J.E.; Blumkin, A.K.; Cook, S. Cardiovascular risk factors and the metabolic syndrome in pediatric nonalcoholic fatty liver disease. Circulation 2008, 118, 277–283. [Google Scholar] [CrossRef] [PubMed]
- D’Adamo, E.; Cali, A.M.; Weiss, R.; Santoro, N.; Pierpont, B.; Northrup, V.; Caprio, S. Central role of fatty liver in the pathogenesis of insulin resistance in obese adolescents. Diabetes Care 2010, 33, 1817–1822. [Google Scholar] [CrossRef] [PubMed]
- Targher, G.; Day, C.P.; Bonora, E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N. Engl. J. Med. 2010, 363, 1341–1350. [Google Scholar] [CrossRef] [PubMed]
- Pacifico, L.; Anania, C.; Martino, F.; Cantisani, V.; Pascone, R.; Marcantonio, A.; Chiesa, C. Functional and morphological vascular changes in pediatric nonalcoholic fatty liver disease. Hepatology 2010, 52, 1643–1651. [Google Scholar] [CrossRef] [PubMed]
- Pacifico, L.; Di Martino, M.; De Merulis, A.; Bezzi, M.; Osborn, J.F.; Catalano, C.; Chiesa, C. Left ventricular dysfunction in obese children and adolescents with nonalcoholic fatty liver disease. Hepatology 2014, 59, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Musso, G.; Gambino, R.; Tabibian, J.H.; Ekstedt, M.; Kechagias, S.; Hamaguchi, M.; Hultcrantz, R.; Hagström, H.; Yoon, S.K.; Charatcharoenwitthaya, P.; et al. Association of non-alcoholic fatty liver disease with chronic kidney disease: A systematic review and meta-analysis. PLoS Med. 2014, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sesti, G.; Fiorentino, T.V.; Arturi, F.; Perticone, M.; Sciacqua, A.; Perticone, F. Association between noninvasive fibrosis markers and chronic kidney disease among adults with nonalcoholic fatty liver disease. PLoS ONE 2014, 9, e88569. [Google Scholar] [CrossRef] [PubMed]
- Machado, M.V.; Gonçalves, S.; Carepa, F.; Coutinho, J.; Costa, A.; Cortez-Pinto, H. Impaired renal function in morbid obese patients with nonalcoholic fatty liver disease. Liver Int. 2012, 32, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Targher, G.; Mantovani, A.; Pichiri, I.; Mingolla, L.; Cavalieri, V.; Mantovani, W.; Pancheri, S.; Trombetta, M.; Zoppini, G.; Chonchol, M.; et al. Nonalcoholic fatty liver disease is independently associated with an increased incidence of chronic kidney disease in patients with type 1 diabetes. Diabetes Care 2014, 37, 1729–1736. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.L.; Zhang, H.J.; Huang, Z.F.; Sun, Q.; Chen, Z.; Li, Z.B.; Yang, S.Y.; Li, X.Y.; Li, X.J. Intrahepatic triglyceride content is independently associated with chronic kidney disease in obese adults: A cross-sectional study. Metabolism 2015, 64, 1077–1085. [Google Scholar] [CrossRef] [PubMed]
- Gansevoort, R.T.; Matsushita, K.; van der Velde, M.; Astor, B.C.; Woodward, M.; Levey, A.S.; de Jong, P.E.; Coresh, J.; Chronic Kidney Disease Prognosis Consortium. Lower estimated GFR and higher albuminuria are associated with adverse kidney outcomes. A collaborative meta-analysis of general and high-risk population cohorts. Kidney Int. 2011, 80, 93–104. [Google Scholar] [CrossRef] [PubMed]
- Fox, C.S.; Larson, M.G.; Leip, E.P.; Culleton, B.; Wilson, P.W.F.; Levy, D. Predictors of new-onset kidney disease in a community-based population. JAMA 2004, 291, 844–850. [Google Scholar] [CrossRef] [PubMed]
- Kramer, H.; Luke, A.; Bidani, A.; Cao, G.; Cooper, R.; McGee, D. Obesity and prevalent and incident CKD: The Hypertension Detection and Follow-Up Program. Am. J. Kidney Dis. 2005, 46, 587–594. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.Y.; McCulloch, C.E.; Iribarren, C.; Darbinian, J.; Go, A.S. Body mass index and risk for end-stage renal disease. Ann. Intern. Med. 2006, 144, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Muntner, P.; Hamm, L.L.; Jones, D.W.; Batuman, V.; Fonseca, V.; Whelton, P.K.; He, J. The metabolic syndrome and chronic kidney disease in U.S. adults. Ann. Intern. Med. 2004, 140, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Hoehner, C.M.; Greenlund, K.J.; Rith-Najarian, S.; Casper, M.L.; McClellan, W.M. Association of the insulin resistance syndrome and microalbuminuria among nondiabetic native Americans. The Inter-Tribal Heart Project. J. Am. Soc. Nephrol. 2002, 13, 1626–1634. [Google Scholar] [CrossRef] [PubMed]
- Speliotes, E.K.; Massaro, J.M.; Hoffmann, U.; Vasan, R.S.; Meigs, J.B.; Sahani, D.V.; Hirschhorn, J.N.; O’Donnell, C.J.; Fox, C.S. Fatty liver is associated with dyslipidemia and dysglycemia independent of visceral fat: The Framingham Heart Study. Hepatology 2010, 51, 1979–1987. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M. Metabolic syndrome pandemic. Arterioscler. Thromb. Vasc. Biol. 2008, 28, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Bugianesi, E.; Moscatiello, S.; Ciaravella, M.F.; Marchesini, G. Insulin resistance in nonalcoholic fatty liver disease. Curr. Pharm. Des. 2010, 16, 1941–1951. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.T.; Huang, J.W.; Chiang, C.K.; Yen, C.J.; Hung, K.Y.; Wu, K.D. Metabolic syndrome and insulin resistance as risk factors for development of chronic kidney disease and rapid decline in renal function in elderly. J. Clin. Endocrinol. Metab. 2012, 97, 1268–1276. [Google Scholar] [CrossRef] [PubMed]
- Vlagopoulos, P.T.; Sarnak, M.J. Traditional and non-traditional cardiovascular risk factors in chronic kidney disease. Med. Clin. N. Am. 2005, 89, 587–611. [Google Scholar] [CrossRef] [PubMed]
- Athyros, V.G.; Tziomalos, K.; Katsiki, N.; Doumas, M.; Karagiannis, A.; Mikhailidis, D.P. Cardiovascular risk across the histological spectrum and the clinical manifestations of non-alcoholic fatty liver disease: An update. World J. Gastroenterol. 2015, 21, 6820–6834. [Google Scholar] [PubMed]
- Wuerzner, G.; Pruijm, M.; Maillard, M.; Bovet, P.; Renaud, C.; Burnier, M.; Boshud, M. Marked association between obesity and glomerular hyperfiltration: A cross-sectional study in an African population. Am. J. Kidney Dis. 2010, 56, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Xiao, N.; Jenkins, T.M.; Nehus, E.; Inge, T.H.; Michalsky, M.P.; Harmon, C.M.; Helmrath, M.A.; Brandt, M.L.; Courcoulas, A.; Moxey-Mims, M.; et al. Kidney function in severely obese adolescents undergoing bariatric surgery. Obesity 2014, 22, 2319–2325. [Google Scholar] [CrossRef] [PubMed]
- Franchini, S.; Savino, A.; Marcovecchio, M.L.; Tumini, S.; Chiarelli, F.; Mohn, A. The effect of obesity and type 1 diabetes on renal function in children and adolescents. Pediatr. Diabetes 2015, 16, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Palatini, P. Glomerular hyperfiltration: A marker of early renal damage in prediabetes and pre-hypertension. Nephrol. Dial. Transplant. 2012, 27, 1708–1714. [Google Scholar] [CrossRef] [PubMed]
- Bacchetta, J.; Cochat, P.; Rognant, N.; Ranchin, B.; Hadj-Aissa, A.; Dubourg, L. Which creatinine and cystatin C equations can be reliably used in children? Clin. J. Am. Soc. Nephrol. 2011, 6, 552–560. [Google Scholar] [CrossRef] [PubMed]
- Staples, A.; LeBlond, R.; Watkins, S.; Wong, C.; Brandt, J. Validation of the revised Schwartz estimating equation in a predominantly non-CKD population. Pediatr. Nephrol. 2010, 25, 2321–2326. [Google Scholar] [CrossRef] [PubMed]
- Fadrowski, J.J.; Neu, A.M.; Schwartz, G.J.; Furth, S.L. Pediatric GFR estimating equations applied to adolescents in the general population. Clin. J. Am. Soc. Nephrol. 2011, 6, 1427–1435. [Google Scholar] [CrossRef] [PubMed]
- Pacifico, L.; Di Martino, M.; Catalano, C.; Panebianco, V.; Bezzi, M.; Anania, C.; Chiesa, C. T1-weighted dual-echo MRI for fat quantification in pediatric nonalcoholic fatty liver disease. World J. Gastroenterol. 2011, 17, 3012–3019. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef] [PubMed]
- DeFronzo, R.A.; Matsuda, M. Reduced time points to calculate the composite index. Diabetes Care 2010, 33, e93. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, G.J.; Muñoz, A.; Schneider, M.F.; Mak, R.H.; Kaskel, F.; Warady, B.A.; Furth, S.L. New equations to estimate GFR in children with CKD. J. Am. Soc. Nephrol. 2009, 20, 629–637. [Google Scholar] [CrossRef] [PubMed]
- Hamer, O.W.; Aguirre, D.A.; Casola, G.; Lavine, J.E.; Woenckhaus, M.; Sirlin, C.B. Fatty liver: Imaging patterns and pitfalls. Radiographics 2006, 26, 1637–1653. [Google Scholar] [CrossRef] [PubMed]
- Fishbein, M.H.; Gardner, K.G.; Potter, C.J.; Schmalbrock, P.; Smith, M.A. Introduction of fast MR imaging in the assessment of hepatic steatosis. Magn. Reson. Imaging 1997, 15, 287–293. [Google Scholar] [CrossRef]
- Pacifico, L.; Di Martino, M.; Anania, C.; Andreoli, G.M.; Bezzi, M.; Catalano, C.; Chiesa, C. Pancreatic fat and β-cell function in overweight/obese children with nonalcoholic fatty liver disease. World J. Gastroenterol. 2015, 21, 4688–4695. [Google Scholar] [PubMed]
- Kleiner, D.E.; Brunt, E.M.; van Natta, M.; Behling, C.; Contos, M.J.; Cummings, O.W.; Ferrell, L.D.; Liu, Y.C.; Torbenson, M.S.; Unalp-Arida, A.; et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005, 41, 1313–1321. [Google Scholar] [CrossRef] [PubMed]
- National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004, 114 (Suppl. 2), 555–576. [Google Scholar]
- Cook, S.; Auinger, P.; Huang, T.T. Growth curves for cardio-metabolic risk factors in children and adolescents. J. Pediatr. 2009, 155 (Suppl. 6), e15–e26. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; de Jong, P.E.; Coresh, J.; Nahas, M.E.; Astor, B.C.; Matsushita, K.; Gansevoort, R.T.; Kasiske, B.L.; Eckardt, K.U. The definition, classification, and prognosis of chronic kidney disease: A KDIGO controversities conference report. Kidney Int. 2011, 80, 17–28. [Google Scholar] [CrossRef] [PubMed]
| Normal Weight | NO NAFLD | NAFLD | p Value * | |
|---|---|---|---|---|
| No. patients | 130 | 328 | 268 | <0.0001 |
| Age, years | 10.6 (3.5) | 10.1 (2.9) | 11.2 (2.9) d | <0.0001 |
| Male sex, n (%) | 61 (46.9) | 151 (46.0) | 166 (61.9) a,d | <0.0001 |
| BMI-SD score | 0.17 (0.85) | 1.85 (0.45) a | 2.0 (0.45) a,d | <0.0001 |
| Waist circumference, cm | 65 (10) | 82 (12) a | 92 (13) a,d | <0.0001 |
| Systolic BP, mmHg | 102 (11) | 107 (12) b | 114 (12) a,d | <0.0001 |
| Diastolic BP, mmHg | 63 (7) | 65 (9) c | 69 (8) a,d | <0.0001 |
| Total cholesterol, mg/dL | 166 (145–186) | 161 (139–187) | 159 (137–181) | 0.077 |
| LDL-C | 92 (72–118) | 94 (76–115) | 94 (74–111) | 0.78 |
| HDL-C, mg/dL | 56 (50–83) | 51 (44–60) a | 46 (38–53) a,d | <0.0001 |
| Triglycerides, mg/dL | 62 (50–83) | 70 (50–99) | 89 (58–127) a,d | <0.0001 |
| AST, U/L | 22 (20–30) | 23 (20–27) c | 26 (21–35) a,d | <0.0001 |
| ALT, U/L | 16 (13–20) | 18 (14–23) b | 31 (19–54) a,d | <0.0001 |
| Uric acid | 0.21 (0.18–0.25) | 0.25 (0.22–0.29) a | 0.28 (0.24–0.34) a,d | <0.0001 |
| Glucose, mg/dL | 83 (7) | 83 (7) | 85 (11) | 0.002 |
| Insulin, μU/mL | 7.5 (4.3–10.5) | 11.1 (7.5–15.4) a | 15.2 (10.1–23.2) a,d | <0.0001 |
| HOMA-IR | 1.58 (0.90–2.20) | 2.30 (1.55–3.22) a | 3.23 (2.05–5.0) a,d | <0.0001 |
| WBISI | - | 6.5 (4.5–9.0) | 3.5 (2.4–5.6) d | - |
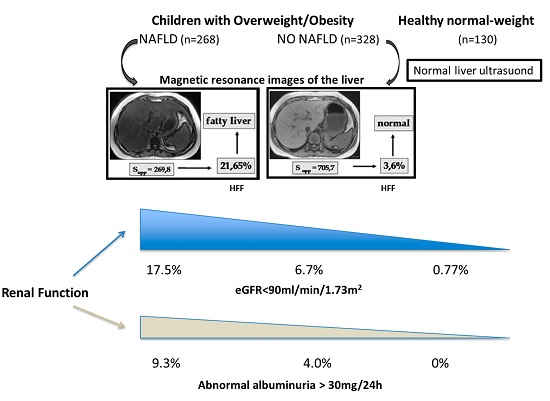
| eGFR, mL/min/1.73 m2 | 108 (100–118) | 115 (104–134) a | 115 (96–132) a | <0.0001 |
| eGFR < 90 mL/min/1.73 m2, n (%) | 1 (0.77) | 22 (6.7) b | 47 (17.5) a,d | <0.0001 |
| eGFR > 139 mL/min/1.73 m2, n (%) | 6 (4.6) | 56 (17.0) a | 46 (17.2) a | 0.002 |
| Microalbuminuria, n (%) | 0 | 13 (4.0) a | 25 (9.3) a,d | <0.0001 |
| Variables | Odds Ratio (95% CI) | p Value |
|---|---|---|
| Adjusted model 1: age, gender, pubertal status | 2.34 (1.31–4.16) | 0.004 |
| Adjusted model 2: model 1 plus BMI-SD score, WC, High BP, High TG, low HDL-C, and high FG | 2.54 (1.16–5.57) | 0.02 |
| Adjusted model 3: model 1 plus BMI-SD score, WC, High BP, High TG, low HDL-C, and IR | 2.30 (1.02–5.17) | 0.04 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pacifico, L.; Bonci, E.; Andreoli, G.M.; Di Martino, M.; Gallozzi, A.; De Luca, E.; Chiesa, C. The Impact of Nonalcoholic Fatty Liver Disease on Renal Function in Children with Overweight/Obesity. Int. J. Mol. Sci. 2016, 17, 1218. https://doi.org/10.3390/ijms17081218
Pacifico L, Bonci E, Andreoli GM, Di Martino M, Gallozzi A, De Luca E, Chiesa C. The Impact of Nonalcoholic Fatty Liver Disease on Renal Function in Children with Overweight/Obesity. International Journal of Molecular Sciences. 2016; 17(8):1218. https://doi.org/10.3390/ijms17081218
Chicago/Turabian StylePacifico, Lucia, Enea Bonci, Gian Marco Andreoli, Michele Di Martino, Alessia Gallozzi, Ester De Luca, and Claudio Chiesa. 2016. "The Impact of Nonalcoholic Fatty Liver Disease on Renal Function in Children with Overweight/Obesity" International Journal of Molecular Sciences 17, no. 8: 1218. https://doi.org/10.3390/ijms17081218
APA StylePacifico, L., Bonci, E., Andreoli, G. M., Di Martino, M., Gallozzi, A., De Luca, E., & Chiesa, C. (2016). The Impact of Nonalcoholic Fatty Liver Disease on Renal Function in Children with Overweight/Obesity. International Journal of Molecular Sciences, 17(8), 1218. https://doi.org/10.3390/ijms17081218