Concurrent Validity of Four Activity Monitors in Older Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Participant Characteristics
2.3. Instrumentation
2.4. Indirect Calorimetry
2.5. Direct Observation
2.6. Laboratory-Based Activity Protocol
2.7. Algorithms
2.8. MET Data Reliability by Epoch Length
2.9. Statistical Analyses
3. Results
3.1. MET Data Reliability
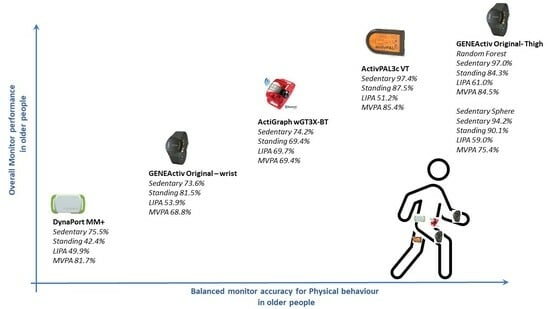
3.2. Overall Monitor Performance
3.3. Monitor Comparison
3.4. Monitor Benchmarking
4. Discussion
4.1. Study Limitations and Strengths
4.2. Recommendations for Future Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- de Rezende, L.F.M.; Lopes, M.R.; Rey-López, J.P.; Matsudo, V.K.R.; do Carmo Luiz, O. Sedentary behavior and health outcomes: An overview of systematic reviews. PLoS ONE 2014, 9, e105620. [Google Scholar] [CrossRef]
- Gorman, E.; Hanson, H.M.; Yang, P.H.; Khan, K.M.; Liu-Ambrose, T.; Ashe, M.C. Accelerometry analysis of physical activity and sedentary behavior in older adults: A systematic review and data analysis. Eur. Rev. Aging Phys. Act. 2014, 11, 35–49. [Google Scholar] [CrossRef]
- Owen, N.; Healy, G.N.; Matthews, C.E.; Dunstan, D.W. Too much sitting: The population health science of sedentary behavior. Exerc. Sport Sci. Rev. 2010, 38, 105–113. [Google Scholar] [CrossRef]
- Kraaijkamp, J.J.M.; Stijntjes, M.; De Groot, J.H.; Chavannes, N.H.; Achterberg, W.P.; van Dam van Isselt, E.F. Movement Patterns in Older Adults Recovering From Hip Fracture. J. Aging Phys. Act. 2024, 12, 1–9. [Google Scholar] [CrossRef]
- Annear, M.; Kidokoro, T.; Shimizu, Y. Physical Activity and Health of Middle-Aged and Older Japanese Across the COVID-19 Pandemic: Differential Outcomes Highlight a Problematic Life Stage. J. Aging Phys. Act. 2024, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Farias, N.; Brown, W.J.; Olds, T.S.; Peeters, G.M.G. Validity of self-report methods for measuring sedentary behaviour in older adults. J. Sci. Med. Sport 2015, 18, 662–666. [Google Scholar] [CrossRef]
- Pedisic, Z.; Bauman, A. Accelerometer-based measures in physical activity surveillance: Current practices and issues. Br. J. Sports Med. 2015, 49, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Wullems, J.A.; Verschueren, S.M.; Degens, H.; Morse, C.I.; Onambele, G.L. A review of the assessment and prevalence of sedentarism in older adults, its physiology/health impact and non-exercise mobility counter-measures. Biogerontology 2016, 17, 547–565. [Google Scholar] [CrossRef] [PubMed]
- Longhini, J.; Marzaro, C.; Bargeri, S.; Palese, A.; Dell’Isola, A.; Turolla, A.; Rossettini, G. Wearable Devices to Improve Physical Activity and Reduce Sedentary Behaviour: An Umbrella Review. Sports Med. Open 2024, 10, 9. [Google Scholar] [CrossRef]
- Van Remoortel, H.; Raste, Y.; Louvaris, Z.; Giavedoni, S.; Burtin, C.; Langer, D.; Wilson, F.; Rabinovich, R.; Vogiatzis, I.; Hopkinson, N.S.; et al. Validity of six activity monitors in chronic obstructive pulmonary disease: A comparison with indirect calorimetry. PLoS ONE 2012, 7, e39198. [Google Scholar] [CrossRef]
- Van Remoortel, H.; Giavedoni, S.; Raste, Y.; Burtin, C.; Louvaris, Z.; Gimeno-Santos, E.; Langer, D.; Glendenning, A.; Hopkinson, N.S.; Vogiatzis, I.; et al. Validity of activity monitors in health and chronic disease: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 84. [Google Scholar] [CrossRef]
- Eke, H.; Bonn, S.E.; Lagerros, Y.T. Wrist-worn accelerometers: Influence of decisions during data collection and processing: A cross-sectional study. Health Sci. Rep. 2024, 7, e1810. [Google Scholar] [CrossRef] [PubMed]
- Byrne, N.M.; Hills, A.P.; Hunter, G.R.; Weinsier, R.L.; Schutz, Y. Metabolic equivalent: One size does not fit all. J. Appl. Physiol. 2005, 99, 1112–1119. (In English) [Google Scholar] [CrossRef] [PubMed]
- Miller, N.E.; Strath, S.J.; Swartz, A.M.; Cashin, S.E. Estimating absolute and relative physical activity intensity across age via accelerometry in adults. J. Aging Phys. Act. 2010, 18, 158–170. [Google Scholar] [CrossRef] [PubMed]
- Clarke, C.L.; Taylor, J.; Crighton, L.J.; Goodbrand, J.A.; McMurdo, M.E.T.; Witham, M.D. Validation of the AX3 triaxial accelerometer in older functionally impaired people. Aging Clin. Exp. Res. 2017, 29, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Löppönen, A.; Delecluse, C.; Suorsa, K.; Karavirta, L.; Leskinen, T.; Meulemans, L.; Portegijs, E.; Finni, T.; Rantanen, T.; Stenholm, S.; et al. Association of Sit-to-Stand Capacity and Free-Living Performance Using Thigh-Worn Accelerometers among 60-to 90-Yr-Old Adults. Med. Sci. Sports Exerc. 2023, 55, 1525–1532. (In English) [Google Scholar] [CrossRef]
- Löppönen, A.; Karavirta, L.; Portegijs, E.; Koivunen, K.; Rantanen, T.; Finni, T.; Delecluse, C.; Van Roie, E.; Rantalainen, T. Day-to-Day Variability and Year-to-Year Reproducibility of Accelerometer-Measured Free-Living Sit-to-Stand Transitions Volume and Intensity among Community-Dwelling Older Adults. Sensors 2021, 21, 6068. (In English) [Google Scholar] [CrossRef] [PubMed]
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical activity in older age: Perspectives for healthy ageing and frailty. Biogerontology 2016, 17, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Grant, D.; Tomlinson, D.; Tsintzas, K.; Kolic, P.; Onambele-Pearson, G.L. The Effects of Displacing Sedentary Behavior with Two Distinct Patterns of Light Activity on Health Outcomes in Older Adults (Implications for COVID-19 Quarantine). Front. Physiol. 2020, 11, 574595. [Google Scholar] [CrossRef]
- Grant, D.; Tomlinson, D.; Tsintzas, K.; Kolic, P.; Onambele-Pearson, G. Minimizing sedentary behavior (without increasing medium-to-vigorous exercise) associated functional improvement in older women is somewhat dependent on a measurable increase in muscle size. Aging 2020, 12, 24081–24100. [Google Scholar] [CrossRef]
- Kerr, J.; Patterson, R.E.; Ellis, K.; Godbole, S.; Johnson, E.; Lanckriet, G.; Staudenmayer, J. Objective Assessment of Physical Activity: Classifiers for Public Health. Med. Sci. Sports Exerc. 2016, 48, 951–957. [Google Scholar] [CrossRef]
- Edwardson, C.L.; Rowlands, A.V.; Bunnewell, S.; Sanders, J.; Esliger, D.W.; Gorely, T.; O’connell, S.; Davies, M.J.; Khunti, K.; Yates, T. Accuracy of Posture Allocation Algorithms for Thigh- and Waist-Worn Accelerometers. Med. Sci. Sports Exerc. 2016, 48, 1085–1090. [Google Scholar] [CrossRef]
- Rowlands, A.V.; Yates, T.; Olds, T.S.; Davies, M.; Khunti, K.; Edwardson, C.L. Sedentary Sphere: Wrist-Worn Accelerometer-Brand Independent Posture Classification. Med. Sci. Sport. Exerc. 2016, 48, 748–754. (In English) [Google Scholar] [CrossRef] [PubMed]
- Hollewand, A.M.; Spijkerman, A.G.; Bilo, H.J.G.; Kleefstra, N.; Kamsma, Y.; van Hateren, K.J.J. Validity of an Accelerometer-Based Activity Monitor System for Measuring Physical Activity in Frail Older Adults. J. Aging Phys. Act. 2016, 24, 555–558. (In English) [Google Scholar] [CrossRef] [PubMed]
- Rowlands, A.V.; Olds, T.S.; Hillsdon, M.; Pulsford, R.; Hurst, T.L.; Eston, R.G.; Gomersall, S.R.; Johnston, K.; Langford, J. Assessing Sedentary Behavior with the GENEActiv: Introducing the Sedentary Sphere. Med. Sci. Sport Exerc. 2014, 46, 1235–1247. (In English) [Google Scholar] [CrossRef]
- Becker, M.L.; Hurkmans, H.L.P.; Verhaar, J.A.N.; Bussmann, J.B.J. Validation of the Activ8 Activity Monitor for Monitoring Postures, Motions, Transfers, and Steps of Hospitalized Patients. Sensors 2023, 24, 180. [Google Scholar] [CrossRef]
- Reeves, M.M.; Davies, P.S.; Bauer, J.; Battistutta, D. Reducing the time period of steady state does not affect the accuracy of energy expenditure measurements by indirect calorimetry. J. Appl. Physiol. 2004, 97, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, T.I.; Jeon, J.Y.; Lindsay, T.; Westgate, K.; Perez-Pozuelo, I.; Hollidge, S.; Wijndaele, K.; Rennie, K.; Forouhi, N.; Griffin, S.; et al. Resting heart rate is a population-level biomarker of cardiorespiratory fitness: The Fenland Study. PLoS ONE 2023, 18, e0285272. (In English) [Google Scholar] [CrossRef] [PubMed]
- Nandy, S.; Parsons, S.; Cryer, C.; Underwood, M.; Rashbrook, E.; Carter, Y.; Eldridge, S.; Close, J.; Skelton, D.; Taylor, S.; et al. Development and preliminary examination of the predictive validity of the Falls Risk Assessment Tool (FRAT) for use in primary care. J. Public Health 2004, 26, 138–143. [Google Scholar] [CrossRef]
- da Rocha, E.E.M.; Alves, V.G.F.; Silva, M.H.N.; Chiesa, C.A.; da Fonseca, R.B.V. Can measured resting energy expenditure be estimated by formulae in daily clinical nutrition practice? Curr. Opin. Clin. Nutr. 2005, 8, 319–328. (In English) [Google Scholar] [CrossRef]
- Wullems, J.A.; Verschueren, S.M.P.; Degens, H.; Morse, C.I.; Onambele, G.L. Performance of thigh-mounted triaxial accelerometer algorithms in objective quantification of sedentary behaviour and physical activity in older adults. PLoS ONE 2017, 12, e0188215. [Google Scholar] [CrossRef]
- Sasaki, J.E.; Hickey, A.M.; Staudenmayer, J.W.; John, D.; Kent, J.A.; Freedson, P.S. Performance of Activity Classification Algorithms in Free-Living Older Adults. Med. Sci. Sport. Exerc. 2016, 48, 941–950. (In English) [Google Scholar] [CrossRef]
- Brady, R.; Brown, W.J.; Mielke, G.I. Day-to-day variability in accelerometer-measured physical activity in mid-aged Australian adults. BMC Public Health 2023, 23, 1880. (In English) [Google Scholar] [CrossRef]
- Crouter, S.E.; Clowers, K.G.; Bassett, D.R. A novel method for using accelerometer data to predict energy expenditure. J. Appl. Physiol. 2006, 100, 1324–1331. (In English) [Google Scholar] [CrossRef] [PubMed]
- Jefferis, B.J.; Sartini, C.; Lee, I.-M.; Choi, M.; Amuzu, A.; Gutierrez, C.; Casas, J.P.; Ash, S.; Lennnon, L.T.; Wannamethee, S.G.; et al. Adherence to physical activity guidelines in older adults, using objectively measured physical activity in a population-based study. BMC Public Health 2014, 14, 382. (In English) [Google Scholar] [CrossRef] [PubMed]
- Laufer, Y. Effect of age on characteristics of forward and backward gait at preferred and accelerated walking speed. J. Gerontol. A-Biol. 2005, 60, 627–632. (In English) [Google Scholar] [CrossRef]
- Onambele, G.L.; Narici, M.V.; Maganaris, C.N. Calf muscle-tendon properties and postural balance in old age. J. Appl. Physiol. 2006, 100, 2048–2056. (In English) [Google Scholar] [CrossRef]
- Kozey-Keadle, S.; Libertine, A.; Lyden, K.; Staudenmayer, J.; Freedson, P.S. Validation of Wearable Monitors for Assessing Sedentary Behavior. Med. Sci. Sport Exerc. 2011, 43, 1561–1567. (In English) [Google Scholar] [CrossRef]
- Gabriel, K.P.; McClain, J.J.; Schmid, K.K.; Storti, K.L.; High, R.R.; Underwood, D.A.; Kuller, L.H.; Kriska, A.M. Isssus in accelerometer methodology: The role of epoch length on estimates of physical activity and relationships with health outcomes in overweight, post-menopausal women. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 53. (In English) [Google Scholar] [CrossRef] [PubMed]
- Ellis, K.; Kerr, J.; Godbole, S.; Staudenmayer, J.; Lanckriet, G. Hip and Wrist Accelerometer Algorithms for Free-Living Behavior Classification. Med. Sci. Sports Exerc. 2016, 48, 933–940. (In English) [Google Scholar] [CrossRef]
- Trost, S.G.; Zheng, Y.L.; Wong, W.K. Machine learning for activity recognition: Hip versus wrist data. Physiol. Meas. 2014, 35, 2183–2189. (In English) [Google Scholar] [CrossRef] [PubMed]
- Lyden, K.; Keadle, S.L.K.; Staudenmayer, J.W.; Freedson, P.S. Validity of Two Wearable Monitors to Estimate Breaks from Sedentary Time. Med. Sci. Sport Exerc. 2012, 44, 2243–2252. (In English) [Google Scholar] [CrossRef] [PubMed]
- Steeves, J.A.; Bowles, H.R.; Mcclain, J.J.; Dodd, K.W.; Brychta, R.J.; Wang, J.; Chen, K.Y. Ability of Thigh-Worn ActiGraph and activPAL Monitors to Classify Posture and Motion. Med. Sci. Sport Exerc. 2015, 47, 952–959. (In English) [Google Scholar] [CrossRef] [PubMed]
- Amri, M.M.; Abed, S.A. The Data-Driven Future of Healthcare: A Review. Mesopotamian J. Big Data 2023, 2023, 68–74. [Google Scholar] [CrossRef]




| Age (years) | 70.0 (12.0) ¶ | |
| Sex | 10 Women | 10 Men |
| Body mass (kg) | 73.4 (13.0) | |
| Body height (cm) | 165.6 (8.1) | |
| BMI (kg∙m−2) | 26.7 (3.6) | |
| RVO2 (ml∙kg−1∙min−1) | 2.87 (0.52) | |
| Physical fitness level * | 3 Less than good | 11 Good or better |
| Preferred walking speed (km∙h−1) | 2.6 (2.0) ¶ | |
| Falls risk | 19 Low | 1 Medium or high |
| Rules | Intensity Classification |
|---|---|
| 1. If MET ≤ 1.5 and posture = sedentary, then | Sedentary |
| 2. Else: If MET ≤ 1.5 and posture ≠ sedentary, then | Standing |
| 3. Else: If MET > 1.5 and <3, then | LIPA |
| 4. Else: If MET ≥ 3, then | MVPA |
| Rules | Classification |
|---|---|
| ActivPAL | |
| If epoch time predominantly = Sedentary, then | Sedentary |
| Else: If epoch time predominantly = Upright, then | Standing |
| Else: If epoch time predominantly = Stepping and MET < 3, then | LIPA |
| Else: If epoch time predominantly = Stepping and MET ≥ 3, then | MVPA |
| ActiGraph | |
| If epoch time predominantly = Sitting or Lying, then | Sedentary |
| Else: If epoch time predominantly = Standing and VM = 0, then | Standing |
| Else: If epoch time predominantly = Standing and VM < 2690, then | LIPA |
| Else: If epoch time predominantly = Standing and VM ≥ 2690, then | MVPA |
| DynaPort MM+ | |
| If epoch class = Sitting or Lying, then | Sedentary |
| Else: If epoch class = Standing, then | Standing |
| Else: If epoch class = Shuffling or Walking and MET < 3, then | LIPA |
| Else: If epoch class = Shuffling or Walking and MET ≥ 3, then | MVPA |
| GENEActiv Original—Thigh—Random Forest | |
| Classifications of this monitor are in line with the criterion measure | N/a |
| GENEActiv Original—Thigh and Wrist—Sedentary Sphere | |
| If epoch intensity/activity = Sleep, then | Sedentary |
| Else: If epoch intensity/activity = Sedentary or Light and posture = Sit/lie, then | Sedentary |
| Else: If epoch intensity/activity = Sedentary and posture = Standing, then | Standing |
| Else: If epoch intensity/activity = Light and posture = Standing, then | LIPA |
| Else: If epoch intensity/activity = Moderate or Vigorous, then | MVPA |
| Monitor | Intensity | Reference | Sensitivity (%) | Specificity (%) | Balanced Accuracy (%) | Acceptable Level (%) | |||
|---|---|---|---|---|---|---|---|---|---|
| Sedentary | Standing | LIPA | MVPA | ||||||
| ActivPAL | Sedentary | 563 | 0 | 53 | 0 | 99.3 | 95.4 | 97.4 | 100.0 |
| Standing | 4 | 156 | 192 | 102 | 94.0 | 80.9 | 87.5 | 100.0 | |
| LIPA | 0 | 0 | 17 | 37 | 5.0 | 97.3 | 51.2 | 0.0 | |
| MVPA | 0 | 10 | 76 | 519 | 78.9 | 92.0 | 85.4 | 85.0 | |
| ActiGraph | Sedentary | 95 | 11 | 21 | 22 | 68.3 | 80.0 | 74.2 | 52.6 |
| Standing | 8 | 16 | 0 | 0 | 41.0 | 97.8 | 69.4 | 43.8 | |
| LIPA | 8 | 12 | 50 | 71 | 66.7 | 72.8 | 69.7 | 33.3 | |
| MVPA | 0 | 0 | 4 | 63 | 40.4 | 98.4 | 69.4 | 33.3 | |
| DynaPort MM+ | Sedentary | 126 | 37 | 27 | 35 | 85.7 | 65.4 | 75.5 | 40.0 |
| Standing | 21 | 2 | 40 | 18 | 4.9 | 79.8 | 42.4 | 0.0 | |
| LIPA | 0 | 0 | 0 | 1 | 0.0 | 99.7 | 49.9 | 0.0 | |
| MVPA | 0 | 2 | 10 | 114 | 67.9 | 95.5 | 81.7 | 80.0 | |
| Random Forest | Sedentary | 842 | 0 | 103 | 1 | 100.0 | 94.1 | 97.0 | 100.0 |
| Standing | 0 | 173 | 37 | 4 | 70.3 | 98.3 | 84.3 | 85.0 | |
| LIPA | 0 | 45 | 160 | 159 | 31.7 | 90.3 | 61.0 | 5.0 | |
| MVPA | 0 | 28 | 205 | 841 | 83.7 | 85.4 | 84.5 | 95.0 | |
| Sedentary Sphere—Thigh | Sedentary | 566 | 5 | 92 | 37 | 99.8 | 88.5 | 94.2 | 100.0 |
| Standing | 0 | 149 | 97 | 53 | 89.8 | 90.4 | 90.1 | 100.0 | |
| LIPA | 1 | 12 | 116 | 215 | 34.3 | 83.6 | 59.0 | 0.0 | |
| MVPA | 0 | 0 | 33 | 356 | 53.9 | 96.9 | 75.4 | 40.0 | |
| Sedentary Sphere—Wrist | Sedentary | 381 | 17 | 111 | 104 | 67.2 | 80.1 | 73.6 | 40.0 |
| Standing | 178 | 131 | 31 | 40 | 78.9 | 84.1 | 81.5 | 85.0 | |
| LIPA | 8 | 13 | 78 | 193 | 23.1 | 84.6 | 53.9 | 0.0 | |
| MVPA | 0 | 5 | 118 | 324 | 49.0 | 88.5 | 68.8 | 15.0 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wullems, J.A.; Verschueren, S.M.P.; Degens, H.; Morse, C.I.; Onambélé-Pearson, G.L. Concurrent Validity of Four Activity Monitors in Older Adults. Sensors 2024, 24, 895. https://doi.org/10.3390/s24030895
Wullems JA, Verschueren SMP, Degens H, Morse CI, Onambélé-Pearson GL. Concurrent Validity of Four Activity Monitors in Older Adults. Sensors. 2024; 24(3):895. https://doi.org/10.3390/s24030895
Chicago/Turabian StyleWullems, Jorgen A., Sabine M. P. Verschueren, Hans Degens, Christopher I. Morse, and Gladys L. Onambélé-Pearson. 2024. "Concurrent Validity of Four Activity Monitors in Older Adults" Sensors 24, no. 3: 895. https://doi.org/10.3390/s24030895
APA StyleWullems, J. A., Verschueren, S. M. P., Degens, H., Morse, C. I., & Onambélé-Pearson, G. L. (2024). Concurrent Validity of Four Activity Monitors in Older Adults. Sensors, 24(3), 895. https://doi.org/10.3390/s24030895