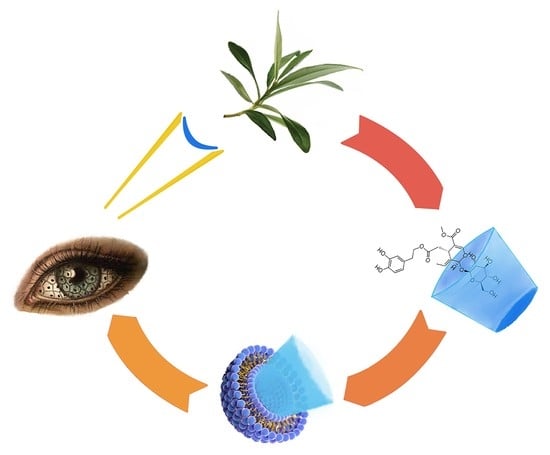
Ocular Application of Oleuropein in Dry Eye Treatment: Formulation Studies and Biological Evaluation
Abstract
:1. Introduction
2. Results and Discussion
2.1. Preparation and Physicochemical Characterization of OLE Formulation
2.2. Stability Evaluation
2.3. Biological Assessment
3. Materials and Methods
3.1. Materials
3.2. Cell Culture
3.3. Preparation of Formulations
3.3.1. Complexation by Cyclodextrin
3.3.2. Preparation of Liposomal Formulations
3.4. Physicochemical Characterization
3.4.1. Differential Scanning Calorimetry (DSC) Analysis
3.4.2. ATR-FTIR Analysis and Focal Plane Array Imaging
3.4.3. Dynamic Light Scattering Analysis
3.4.4. Entrapment Efficiency
3.4.5. Microscopy
3.5. Oleuropein Quantitative Analysis
- a.
- y = 27,000x − 1304; R2 = 0.9987, at a concentration ranging from 0.425 to 4.000 μg/mL in methanol (Limit Of Quantification = 0.093 μg/mL), to determine the entrapment efficiency;
- b.
- y = 39,780x + 982; R2 = 0.9980, at a concentration ranging from 1.00 to 11.60 μg/mL in water (Limit Of Quantification = 0.322 μg/mL), for stability studies.
3.6. Stability Evaluation
3.7. Biological Assessment
3.7.1. Cytotoxicity Studies
3.7.2. Evaluation of the Protective Activity against Hyperosmotic Stress
3.7.3. Evaluation of Antioxidant Activity
3.8. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Omar, S.H. Oleuropein in Olive and its Pharmacological Effects. Sci. Pharm. 2010, 78, 133–154. [Google Scholar] [CrossRef] [Green Version]
- Barbaro, B.; Toietta, G.; Maggio, R.; Arciello, M.; Tarocchi, M.; Galli, A.; Balsano, C. Effects of the Olive-Derived Polyphenol Oleuropein on Human Health. Int. J. Mol. Sci. 2014, 15, 18508–18524. [Google Scholar] [CrossRef]
- Messmer, E.M. The pathophysiology, diagnosis, and treatment of dry eye disease. Dtsch. Arrztebl. Int. 2015, 112, 71–82. [Google Scholar] [CrossRef] [Green Version]
- Akpek, E.K.; Amescua, G.; Farid, M.; Garcia-Ferrer, F.J.; Lin, A.; Rhee, M.K.; Varu, D.M.; Musch, D.C.; Dunn, S.P.; Mah, F.S. Dry Eye Syndrome Preferred Practice Pattern®. Ophthalmology 2019, 126, P286–P334. [Google Scholar] [CrossRef] [Green Version]
- Stern, M.E.; Pflugfelder, S. Inflammation in dry eye. Ocul. Surf. 2004, 2, 124–130. [Google Scholar] [CrossRef]
- Baudouin, C.; Aragona, P.; Messmer, E.M.; Tomlinson, A.; Calonge, M.; Boboridis, K.G.; Akova, Y.A.; Geerling, G.; Labetoulle, M.; Rolando, M. Role of Hyperosmolarity in the Pathogenesis and Management of Dry Eye Disease: Proceedings of the OCEAN Group Meeting. Ocul. Surf. 2013, 11, 246–258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.; Li, M.; Li, B.; Wang, W.; Lin, A.; Sheng, M. Effect of reactive oxygen species generation in rabbit corneal epithelial cells on inflammatory and apoptotic signaling pathways in the presence of high osmotic pressure. PLoS ONE 2013, 8, e0072900. [Google Scholar] [CrossRef] [Green Version]
- Seen, S.; Tong, L. Dry eye disease and oxidative stress. Acta Ophthalmol. 2018, 96, e412–e420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dogru, M.; Kojima, T.; Simsek, C.; Tsubota, K. Potential role of oxidative stress in ocular surface inflammation and dry eye disease. Investig. Ophthalmol. Vis. Sci. 2018, 59, DES163–DES168. [Google Scholar] [CrossRef] [Green Version]
- Pflugfelder, S.C.; Geerling, G.; Kinoshita, S.; Lemp, M.A.; McCulley, J.; Nelson, D.; Novack, G.N.; Shimazaki, J.; Wilson, C. Management and therapy of dry eye disease: Report of the management and therapy subcommittee of the International Dry Eye WorkShop. Ocul. Surf. 2007, 5, 163–176. [Google Scholar] [CrossRef]
- Garrett, Q.; Khandekar, N.; Shih, S.; Flanagan, J.L.; Simmons, P.; Vehige, J.; Willcox, M.D. Betaine stabilizes cell volume and protects against apoptosis in human corneal epithelial cells under hyperosmotic stress. Exp. Eye Res. 2013, 108, 33–41. [Google Scholar] [CrossRef]
- Hua, X.; Su, Z.; Deng, R.; Lin, J.; Li, D.; Pflugfelder, S.C. Effects of L-carnitine, Erythritol and Betaine on pro-inflammatory markers in primary human corneal epithelial cells exposed to hyperosmotic stress. Curr. Eye Res. 2015, 40, 657–667. [Google Scholar] [CrossRef] [PubMed]
- Orobia, A.J.M.; Saa, J.; Lorenzo, A.O.; Herreras, J.M. Combination of hyaluronic acid, carmellose, and osmoprotectants for the treatment of dry eye disease. Clin. Ophthalmol. 2018, 12, 453–461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, W.; Kim, J.C.; Kim, W.S.; Oh, H.J.; Yang, J.M.; Lee, J.B.; Yoon, K.C. Clinical effect of antioxidant glasses containing extracts of medicinal plants in patients with dry eye disease: A multi-center, prospective, randomized, double-blind, placebo-controlled trial. PLoS ONE 2015, 10, e0139761. [Google Scholar] [CrossRef]
- Bucolo, C.; Fidilio, A.; Platania, C.B.M.; Geraci, F.; Lazzara, F.; Drago, F. Antioxidant and osmoprotecting activity of taurine in dry eye models. J. Ocul. Pharmacol. Ther. 2018, 34, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Malik, N.S.A.; Bradford, J.M. Recovery and stability of oleuropein and other phenolic compounds during extraction and processing of olive (Olea europaea L.) leaves. J. Food Agric. Environ. 2008, 6, 8–13. [Google Scholar]
- Tylkowski, B.; Tsibranska, I. Polyphenols encapsulation-application of innovation technologies to improve stability of natural products. Phys. Sci. Rev. 2016, 1, 20150005. [Google Scholar] [CrossRef] [Green Version]
- Bilia, A.R.; Piazzini, V.; Guccione, C.; Risaliti, L.; Asprea, M.; Capecchi, G.; Bergonzi, M.C. Improving on nature: The role of nanomedicine in the development of clinical natural drugs. Planta Med. 2017, 83, 366–381. [Google Scholar] [CrossRef] [Green Version]
- Munin, A.; Edwards-Lévy, F. Encapsulation of Natural Polyphenolic Compounds; A Review. Pharmaceutics 2011, 3, 793–829. [Google Scholar] [CrossRef] [Green Version]
- Musthaba, S.M.; Ahmad, S.; Ahuja, A.; Ali, J.; Baboota, S. Nano approaches to enhance pharmacokinetic and pharmacodynamic activity of plant origin drugs. Curr. Nanosci. 2009, 5, 344–352. [Google Scholar] [CrossRef]
- Coimbra, M.; Isacchi, B.; van Bloois, L.; Torano, J.S.; Ket, A.; Wu, X.; Broere, F.; Metselaar, J.M.; Rijcken, C.J.; Storm, G.; et al. Improving solubility and chemical stability of natural compounds for medicinal use by incorporation into liposomes. Int. J. Pharm. 2011, 416, 433–442. [Google Scholar] [CrossRef]
- Badwaik, H.R.; Kumari, L.; Nakhate, K.; Verma, V.S.; Sakure, K. Chapter 13—Phytoconstituent plumbagin: Chemical, biotechnological and pharmaceutical aspects. Stud. Nat. Prod. Chem. 2019, 63, 415–460. [Google Scholar] [CrossRef]
- Mourtzinos, I.; Salta, F.; Yannakopoulou, K.; Chiou, A.; Karathanos, V.T. Encapsulation of olive leaf extract in β-Cyclodextrin. J. Agric. Food Chem. 2007, 55, 8088–8094. [Google Scholar] [CrossRef]
- Kesente, M.; Kavetsou, E.; Roussaki, M.; Blidi, S.; Loupassaki, S.; Chanioti, S.; Siamandoura, P.; Stamatogianni, C.; Philippou, E.; Papaspyrides, C.; et al. Encapsulation of olive leaves extracts in biodegradable PLA nanoparticles for use in cosmetic formulation. Bioengineering 2017, 4, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nassir, A.M.; Ibrahim, I.A.A.; Tanuja, S.W.; Ain, M.R.; Ahmad, I.; Shahzad, N. Surface functionalized folate targeted oleuropein nano-liposomes for prostate tumor targeting: In vitro and in vivo activity. Life Sci. 2019, 220, 136–146. [Google Scholar] [CrossRef]
- Davis, M.E.; Brewster, M.E. Cyclodextrin-based pharmaceutics: Past, present and future. Nat. Rev. Drug Discov. 2004, 3, 1023. [Google Scholar] [CrossRef]
- Efmorfopoulou, E.; Rodis, P. Complexation of oleuropein and trans-cinnamic acid with cyclodextrins. Chem. Nat. Compd. 2004, 40, 362–366. [Google Scholar] [CrossRef]
- Szente, L.; Singhal, A.; Domokos, A.; Song, B. Cyclodextrins: Assessing the impact of cavity size, occupancy, and substitutions on cytotoxicity and cholesterol homeostasis. Molecules 2018, 23, 1228. [Google Scholar] [CrossRef] [Green Version]
- Jansen, T.; Xhonneux, B.; Mesens, J.; Borgers, M. Beta-cyclodextrins as vehicles in eye-drop formulations: An evaluation of their effects on rabbit corneal epithelium. Lens Eye Toxic. Res. 1990, 7, 459–468. [Google Scholar] [PubMed]
- EMA; Committee for Human Medicinal Products. Cyclodextrins Used as Excipients. 2017. Available online: https://www.ema.europa.eu/en/cyclodextrins (accessed on 14 August 2021).
- Muankaew, C.; Loftsson, T. Cyclodextrin-based formulations: A non-invasive platform for targeted drug delivery. Basic Clin. Pharmacol. Toxicol. 2018, 122, 46–55. [Google Scholar] [CrossRef] [Green Version]
- Bonechi, C.; Donati, A.; Tamasi, G.; Pardini, A.; Rostom, H.; Leone, G.; Lamponi, S.; Consumi, M.; Magnani, A.; Rossi, C. Chemical characterization of liposomes containing nutraceutical compounds: Tyrosol, hydroxytyrosol and oleuropein. Biophys. Chem. 2019, 246, 25–34. [Google Scholar] [CrossRef]
- McCormack, B.; Gregoriadis, G. Drugs-in-cyclodextrins-in-liposomes: A novel concept in drug delivery. Int. J. Pharm. 1994, 112, 249–258. [Google Scholar] [CrossRef]
- Loukas, Y.L.; Jayasekera, P.; Gregoriadis, G. Characterization and photoprotection studies of a model-cyclodextrin included photolabile drug entrapped in liposomes incorporating light absorbers. J. Phys. Chem. 1995, 99, 11035–11040. [Google Scholar] [CrossRef]
- Maestrelli, F.; Gonzalez-Rodriguez, M.L.; Rabasco, A.M.; Mura, P. Preparation and characterisation of liposomes encapsulating ketoprofen–cyclodextrin complexes for transdermal drug delivery. Int. J. Pharm. 2005, 298, 55–67. [Google Scholar] [CrossRef] [PubMed]
- Piel, G.; Piette, M.; Barillaro, V.; Castagne, D.; Evrard, B.; Delattre, L. Betamethasone-in-cyclodextrin-in-liposome: The effect of cyclodextrins on encapsulation efficiency and release kinetics. Int. J. Pharm. 2006, 312, 75–82. [Google Scholar] [CrossRef]
- Dhule, S.S.; Penfornis, P.; Frazier, T.; Walker, R.; Feldman, J.; Tan, G.; He, J.; Alb, A.; John, V.; Pochampally, R. Curcumin-loaded γ-cyclodextrin liposomal nanoparticles as delivery vehicles for osteosarcoma. Nanomedicine 2012, 8, 440–451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernández-Romero, A.M.; Maestrelli, F.; Mura, P.A.; Rabasco, A.M.; González-Rodríguez, M.L. Novel findings about double-loaded curcumin-in-HP cyclodextrin-in liposomes: Effects on the lipid bilayer and drug release. Pharmaceutics 2018, 10, 256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ozdemir, Y.; Guven, E.; Ozturk, A. Understanding the characteristics of oleuropein for table olive processing. J. Food Process. Technol. 2014, 5, 1. [Google Scholar] [CrossRef] [Green Version]
- Sur, S.; Fries, A.C.; Kinzler, K.W.; Zhou, S.; Vogelstein, B. Remote loading of preencapsulated drugs into stealth liposomes. Proc. Natl. Acad. Sci. USA 2014, 111, 2283–2288. [Google Scholar] [CrossRef] [Green Version]
- Vicario-de-la-Torre, M.; Benitez-del-Castillo, J.M.; Vico, E.; Guzman, M.; de-las-Heras, B. Herrero-Vanrell, R.; Molina-Martínez, I.T. Design and characterization of an ocular topical liposomal preparation to replenish the lipids of the tear film. Investig. Ophthalmol. Vis. Sci. 2014, 55, 7839–7847. [Google Scholar] [CrossRef] [Green Version]
- Holzer, M.; Barnert, S.; Momm, J.; Schubert, R. Preparative size exclusion chromatography combined with detergent removal as a versatile tool to prepare unilamellar and spherical liposomes of highly uniform size distribution. J. Chromatogr. A 2009, 1216, 5838–5848. [Google Scholar] [CrossRef] [PubMed]
- Crawford, R.; Dogdas, B.; Keough, E.; Haas, R.M.; Wepukhulu, W.; Krotzer, S.; Burke, P.A.; Sepp-Lorenzino, L.; Bagchi, A.; Howell, B.J. Analysis of lipid nanoparticles by Cryo-EM for characterizing siRNA delivery vehicles. Int. J. Pharm. 2011, 403, 237–244. [Google Scholar] [CrossRef]
- Lemp, M.A.; Baudouin, C.; Baum, J.; Dogru, M.; Foulks, G.N.; Kinoshita, S.; Laibson, P.; McCulley, J.; Murube, J.; Pflugfelder, S.C.; et al. The definition and classification of dry eye disease: Report of the definition and classification subcommittee of the International Dry Eye WorkShop. Ocul. Surf. 2007, 5, 75–92. [Google Scholar] [CrossRef]
- Shi, C.; Chen, X.; Liu, Z.; Meng, R.; Zhao, X.; Liu, Z.; Guo, N. Oleuropein protects L-02 cells against H2O2-induced oxidative stress by increasing SOD1, GPx1 and CAT expression. Biomed. Pharmacother. 2017, 85, 740–748. [Google Scholar] [CrossRef] [PubMed]
- Cejková, J.; Ardan, T.; Simonová, Z.; Cejka, C.; Malec, J.; Dotrelová, D.; Brunová, B. Decreased expression of antioxidant enzymes in the conjunctival epithelium of dry eye (Sjogren’s syndrome) and its possible contribution to the development of ocular surface oxidative injuries. Histol. Histopathol. 2008, 23, 1477–1483. [Google Scholar] [CrossRef]
- Wakamatsu, T.H.; Dogru, M.; Matsumoto, Y.; Kojima, T.; Kaido, M.; Ibrahim, O.M.A.; Sato, E.A.; Igarashi, A.; Ichihashi, Y.; Satake, Y.; et al. Evaluation of lipid oxidative stress status in Sjogren syndrome patients. Investig. Ophthalmol. Vis. Sci. 2013, 54, 201–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCormack, B.; Gregoriadis, G. Entrapment of cyclodextrin-drug complexes into liposomes: Potential advantages in drug delivery. J. Drug Target. 1994, 2, 449–454. [Google Scholar] [CrossRef]
- Loukas, Y.; Vraka, V.; Gregoriadis, G. Drugs, in cyclodextrins, in liposomes: A novel approach to the chemical stability of drugs sensitive to hydrolysis. Int. J. Pharm. 1998, 162, 137–142. [Google Scholar] [CrossRef]
- Fatouros, D.; Hatzidimitiou, K.; Antimisiaris, S. Liposomes encapsulating prednisolone and prednisolone-cyclodextrin complexes: Comparison of membrane integrity and drug release. Eur. J. Pharm. Sci. 2001, 13, 287–296. [Google Scholar] [CrossRef]
- Gharib, R.; Greige-Gerges, H.; Fourmentin, S.; Charcosset, C.; Auezova, L. Liposomes incorporating cyclodextrin–drug inclusion complexes: Current state of knowledge. Carbohydr. Polym. 2015, 129, 175–186. [Google Scholar] [CrossRef]







| Label | Hydration Buffer | Sizing Method |
|---|---|---|
| F7.4-u | PBS 1 | Ultrasonication |
| F7.4-e | PBS | Extrusion |
| F5.5-u | CBS 2 | Ultrasonication |
| F5.5-e | CBS | Extrusion |
| Formulation | EE % (±S.E.) | Size (nm ± S.E.) | Polydispersity Index |
|---|---|---|---|
| F7.4-u | 69.63 ± 1.02 | 240.9 ± 53.64 1863 ± 246.0 | |
| F7.4-e | 77.64 ± 3.08 | 268.2 ± 6.53 | 0.362 ± 0.0268 |
| F5.5-u | 72.98 ± 5.62 | 242.4 ± 38.19 2149 ± 388.9 | |
| F5.5-e | 80.77 ± 1.35 | 235.5 ± 14.94 | 0.310 ± 0.0317 |
| Formulation | t50% (days) | |
|---|---|---|
| 4 °C | R.T. | |
| OLE7.4-sol | 67.14 (0.958) | 24.30 (0.998) |
| OLE5.5-sol | 96.61 (0.984) | 79.47 (0.871) |
| F7.4-u | 89.68 (0.991) | 50.82 (0.985) |
| F7.4-e | 156.1 (0.995) | 88.45 (0.936) |
| F5.5-u | 90.93 (0.991) | 50.90 (0.869) |
| F5.5-e | 141.8 (0.946) | 88.42 (0.995) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burgalassi, S.; Zucchetti, E.; Birindelli, E.; Tampucci, S.; Chetoni, P.; Monti, D. Ocular Application of Oleuropein in Dry Eye Treatment: Formulation Studies and Biological Evaluation. Pharmaceuticals 2021, 14, 1151. https://doi.org/10.3390/ph14111151
Burgalassi S, Zucchetti E, Birindelli E, Tampucci S, Chetoni P, Monti D. Ocular Application of Oleuropein in Dry Eye Treatment: Formulation Studies and Biological Evaluation. Pharmaceuticals. 2021; 14(11):1151. https://doi.org/10.3390/ph14111151
Chicago/Turabian StyleBurgalassi, Susi, Erica Zucchetti, Elena Birindelli, Silvia Tampucci, Patrizia Chetoni, and Daniela Monti. 2021. "Ocular Application of Oleuropein in Dry Eye Treatment: Formulation Studies and Biological Evaluation" Pharmaceuticals 14, no. 11: 1151. https://doi.org/10.3390/ph14111151
APA StyleBurgalassi, S., Zucchetti, E., Birindelli, E., Tampucci, S., Chetoni, P., & Monti, D. (2021). Ocular Application of Oleuropein in Dry Eye Treatment: Formulation Studies and Biological Evaluation. Pharmaceuticals, 14(11), 1151. https://doi.org/10.3390/ph14111151