1. Introduction
For thousands of years, plants have been a source of medicine; people relied on nature to supply their basic needs, including their medicines. Several traditional medicinal systems such as Traditional Chinese Medicine, Indian Ayurvedic and the ancient Greek and Romans systems [
1] have formed and made a substantial contribution to the development of natural medicine [
2]. As a typical ethnomedicinal approach, Traditional Chinese Medicine (TCM) is one of a few ancient medicinal systems still preserved to date. It has gained more acceptance and recognition by other countries due to its affordability, reliable efficacy, local availability and fewer described side effects [
3]. However, the indistinct effects, poor quality control, and the differences concerning the modern medical system restrict its global use.
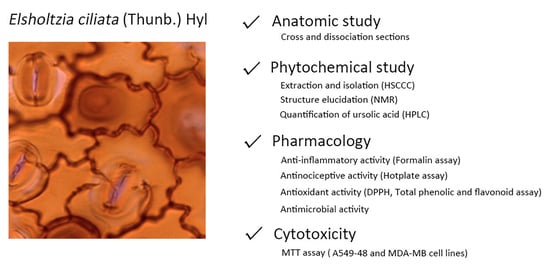
Elsholtzia ciliata (Thunb.) Hyl. (EC), family Lamiaceae is a plant widely used in TCM as an anti-bacterial and anti-inflammatory medicine [
4]. EC occurs widely in Jiangxi, Yunnan Province of China and throughout India, Korea and Europe. EC is an herbaceous plant measuring 30–50 cm in height with thick leaves, an oval leaflet, a growing villus and brownish oblong berry-shaped seeds. The flower is pink and usually contains 3–4 pistils in which the lower lobe is lower than the upper lobe [
5]. EC has been used to treat a range of diseases, such as colds, fever, diarrhea, dysentery, digestion disorders, vomiting, strokes and oedema for thousands of years in folk medicine in China [
4]. There are reports of EC as playing a role in antimicrobial, antioxidant, antinociceptive, anti-inflammatory, febrifuge, sedative, anticancer and antitumor activities [
6,
7]. However, thus far, there has been no testing for these activities but the essential oil of this plant has had its antimicrobial activity evaluated a few times [
5]. A few studies have reported the chemistry of EC, most of them about the chemical composition of the essential oil, and hence, more studies are required to evaluate the non-volatile chemical composition. The main chemical compounds for EC are volatile oil constituents, flavonoids, steroids and triterpenes [
8].
This study dealt with EC’s anatomy, non-volatile composition and pharmacological properties. The study aimed at providing information for the quality control (Botany and Chemistry) of this herbal drug, traditionally used in China for many centuries.
3. Discussion
This study provides important anatomic and morphological information on Elsholtzia ciliata (Thunb.) Hyl. According to this anatomical study, there is little or no difference between the epidermal cells, vascular bundle, palisade parenchyma, spongy parenchyma and collenchyma, while for trichomes and stomata, more attention should be paid for further studies or when carrying out identifications.
The current study on Elsholtzia ciliata (Thunb.) Hyl. provides valuable, useful and reliable information on its anatomy. The presence of the three kinds of trichomes, two kinds of stomata and vascular bundle are species-specific and could be used for identification.
From the chemical point of view, ursolic acid and Oroxylin A were isolated from the crude ethanol extract of
Elsholtzia ciliata. It was the first time Oroxylin A was isolated from this plant. Triterpenes and flavonoids are frequently occurring metabolites in Lamiaceae [
19]. They are also sometimes responsible for some of their pharmacological actions.
Formalin and hot plate were used to evaluate the potential of this plant to act as anti-inflammatory or antinociceptive. The response of licking time in the formalin model shows an early and a late phase. The early phase is short-lasting and responded immediately after the injection, which corresponds to neurogenic pain. The late phase is long and persistent, which is associated with the inflammatory response [
20]. In the current study, crude ethanol extract and its dichloromethane fraction (100 mg/kg,
p < 0.05) possessed a significant reduction of the licking time only at the second phase when comparing with the control group; therefore, this inhibition suggested that the action mainly related with the anti-inflammatory activity. Hexane fraction (100 mg/kg) possessed lick-reducing activity only at the early phase. The response suggested nociception related to the peripheral mechanism.
A previous anti-inflammatory study with ursolic acid indicated its ED
50 value to be 44 mg/kg. Additionally, the nociceptive response was significantly inhibited in rats with the administration of ursolic acid. These results were seen with a dose of 10 mg/kg, both in the neurogenic and the inflammatory phases of the formalin test [
21]. In the current study, it is clear to see that crude ethanol extract and its dichloromethane fraction contain a larger quantity of ursolic acid. This finding agrees with the pharmacological results obtained in the formalin test. Both extract and DCM fraction (100 mg/kg) presented significant pharmacological activity at the later phase of this test, which suggest anti-inflammatory activity.
The result of hexane fraction in the hot plate test was in agreement with the formalin test (first phase) that indicated the antinociceptive potential for this fraction. Although hexane fraction showed a higher increase in baseline % than morphine at 30 and 60 min, they were not active throughout the experiment as morphine was, hence the morphine bar was taller than the bars for this fraction. It is also worth mentioning that these results are preliminary. Further studies using receptor antagonists of different pharmacological pathways need to be carried out in the future. These studies will help the understanding of the mechanism of action for the antinociceptive activity related to hexane and dichloromethane fractions and their constituents.
Benincá and collaborators showed in 2011 that ursolic acid was able to inhibit leukocytes migration, IL-1beta, TNF-alpha, MPO and NOx. These results were also seen by Mueller et al., Ku and Lin and Kim et al. who published in 2013 the capacity of ursolic acid in modulating different cytokines in vitro [
22].
In this way of using the formalin and the hot plate assays, this study proves the potential this plant has to act as antinociceptive and anti-inflammatory. These are valuable findings as this plant is widely used as an anti-inflammatory TCM in China.
In terms of antioxidant potential, in general, the antioxidant activity as measured by the DPPH assay can be well correlated with the content of phenolics and flavonoids. The results presented by the DPPH assay, total phenolic content and flavonoid equivalents in this study suggest that Elsholtzia ciliata possesses high antioxidant activity.
The total phenolic content (TPC), total flavonoid content (TFC), antioxidant activities and anti-inflammatory activities of
Elsholtzia ciliata have been studied previously [
23,
24]. Pudziuvelyte et al. found that the amount of phenolic ranged from 61.25 ± 1.91 to 94.67 ± 1.91 mg gallic acid equivalent (GAE)/g dry weight (DW) in the extracts of different parts of the plant, leaf, stem and flower [
23]. A similar work performed by Liu et al. showed that the quantity of phenolic compounds in the root’s fraction (497.2 ± 24.9) is higher than those found in the stem’s (213.1 ± 6.2) and inflorescence’s (198.2 ± 10.1) fractions [
24]. The content of flavonoids ranged from 5.06 ± 0.08 to 15.43 ± 1.86 mg rutin equivalent (RE) per g/DW with the highest flavonoid level in whole plant and lowest value in the stem. Antioxidant and anti-inflammatory activities were also performed by Pudziuvelyte et al. The DPPH test showed clear evidence of the antioxidant activity of
Elsholtzia ciliata. The anti-inflammatory activity was assessed by measuring the amounts of inflammatory mediators’ reduction. The results achieved in our study agree with the previous studies by showing a similar trend. The difference in the values of TPC and TFC could be due to the solvent used or conditions during the extraction, the quality of plant materials or environment. Our results confirmed
Elsholtzia ciliata to be a rich source of phenolic, flavonoid compounds and to possess high antioxidant and anti-inflammatory potential.
The antimicrobial evaluation performed in the current study dealt with the non-volatile extract, named crude ethanol extract and its hexane and dichloromethane fractions. The results showed that the dichloromethane fraction possessed the highest antimicrobial potential against Candida albicans (62.5 μg/mL) and some moderate activity against Staphylococcus aureus (500 μg/mL). Hexane fraction revealed the highest antimicrobial potential against Escherichia coli (250 μg/mL).
As reported by Dorman and Deans (2000) phenolic compounds, such as flavonoids, may be responsible for the antimicrobial activity of plant extracts [
25]. The specific mechanism involved here is the destabilization of the cytoplasmic membrane by compounds with phenolic groups (OH bound to aromatic rings), which act as proton exchangers, reducing the pH gradient across the cytoplasmic membrane and thus leading to cell death.
The antimicrobial results suggested that the non-volatile (extracts) components also showed potential to be exploited as effective antimicrobial medicines.
The cytotoxicity test with two cancer cell lines showed that the higher activity is observed in 24 h and that the 300 μg/mL concentration of the crude ethanol extract and its fractions decreased the cell viability more than the other doses. The ethanol extract and its fractions showed an anti-proliferative effect on cells except for the concentrations of 10, 100 μg/mL for the hexane and dichloromethane fractions. Generally, a positive correlation was seen between the cell viabilities and the used extract concentrations. The results determined the positive effects of the extract and its fractions on cell viability mainly up to 24 h.
Ursolic acid in synergy with other constituents in the extract and its fractions can be responsible for the observed cytotoxic effect. Gu et al. in 2012 showed that ursolic acid was able to inhibit MCF-7 cells proliferation, increasing p53 and p21WAF1/Cip1 expression. Zhao et al., in 2013, also saw for the same cell type MCF-7 that ursolic acid was able to induce apoptosis of the cells through upregulation of MCL1 and autophagy by MAPK1/3 pathway [
26].
On the other hand, Oroxylin A inhibited the viability of hepatocarcinoma cell line HepG2 by substantially producing H
2O
2 intracellularly and activating the PERK-eIF2-ATF4-CHOP branch of the unfolded protein response (UPR) pathway. These mechanisms resulted in the induction of TRB3 and causal reduction of p-AKT1/2/3 (Ser473) (Xu et al., 2012) [
27].
In the present study, we isolated Oroxylin A from the Hexane fraction, which can contribute for the overall cytotoxic potential of this plant.
4. Materials and Methods
Plant materials. Leaves of Elsholtzia ciliata (Thunb.) Hyl collection (900 g) took place in Jiangxi Province, China, in August 2013. Part of the material suffered herborization. Dr. Hua Yang identified the plant. A voucher number: CPU-2013101802, is registered in the herbarium of the China Pharmaceutical University (CPU).
Animals. This study used Swiss Webster mice (20–25 g), donated by Instituto Vital Brazil (Niteroi, Rio de Janeiro, Brazil). A room with a light-dark cycle of 12 h, 22 ± 2 °C, 60% to 80% humidity and with food and water provided ad libitum were the conditions adopted for the animals. We used mice only one time per experiment after acclimatisation to the laboratory conditions for at least one hour before the beginning of each test. All protocols were conducted per the Guidelines on Ethical Standards for Investigation of Experimental Pain in Animals (Zimmermann, 1983) [
28] and followed the principles and guidelines adopted by the National Council for the Control of Animal Experimentation (CONCEA), approved by the Ethical Committee for Animal Research (# DFBCICB015–04/16, 31/19 and 34/19). All experimental protocols only took place during the light phase. Each group used a minimum number of animals, and at the end of each experiment, we used a ketamine/xylazine overdose to sacrifice the animals.
Cell culture. Human lung alveolar basal carcinoma epithelial cells (A549) and MDA-MB breast cancer cells were cultured at 37 °C under 5% CO2 for 2–3 days in an incubator in RPMI medium supplemented with 10% fetal bovine serum and 1% antibiotics (penicillin and streptomycin). The cells were then sedimented by centrifugation at 1200 rpm for 5 min. After removing the supernatant, the cell pellets were resuspended in a fresh medium.
Microorganisms. This study used three strains of microorganisms, one Gram-positive, one Gram-negative and one fungus. Culture conditions used: Staphylococcus aureus MRSA (BMB9393) and Escherichia coli were clinically isolated from the Clementino Fraga Filho Hospital, UFRJ, Brazil. The bacteria were cultured under the condition of Brain Heart Infusion Agar cattle (BHI) for 24 h at 37 °C. Candida albicans serotype B ATCC 36802 was originally from the Federal University of São Paulo, Brazil and cultured on Sabouraud Agar for 48 h at room temperature.
Reagents and chemicals. Sodium hypochlorite, acetic acid, hydrogen peroxide, dimethyl sulfoxide, deuterated chloroform, acetylsalicylic acid (ASA), 2,2-Diphenyl-1-picrylhydrazyl (DPPH), Folin–Ciocalteu phenol reagent, aluminium trichloride anhydrous, gallic acid 3-[4,5-dimethylthiazol-2-yl]-2,5 diphenyl tetrazolium bromide (MTT) were purchased from Sigma–Aldrich Chemical Co. Sodium carbonate anhydrous was obtained from BDH Chemicals Ltd. Poole England. Formalin was purchased from Merck Inc. Morphine was provided by Cristália (São Paulo, Brazil). Quercetin, hexane, dichloromethane, ethyl acetate, ethanol, methanol, chloroform and n-butanol were obtained from Trinity College Dublin Hazardous Materials Facility solvent store.
Anatomic study. Cross-sections were manually performed on leaves and stems using commercial razor blades. Sections were clarified with sodium hypochlorite 20%, neutralized with acetic acid 0.2%, washed in distilled water and stained with a solution of Astra blue and Safranin [
29]. The dissociation section was prepared by making fragments in a solution of hydrogen peroxide and acetic acid (1:1), washing in distilled water and staining with Safranin 50% [
30]. The sections were mounted with glycerinated gelatin 50%. The images were obtained using a photomicroscope Leica DM750 with the image capture system ICC50 HD and Qwin program.
Preparation of plant extracts and the isolation of bioactive compounds. The crude ethanol extract was prepared by continuous hot extraction of the plant material (900 g) using soxhlet for 72 h. A liquid–liquid extraction of the evaporated total ethanol extract, suspended in water, was executed to obtain the following fractions of increasing polarities: hexane, dichloromethane, ethyl acetate and n-butanol.
In a parallel protocol, the crude ethanol extract was also chromatographed using counter-current chromatography. The HSCCC separation conducted on an IntroPrep TM (Quattro) counter-current chromatography (AECS, Bridgend, UK) equipped with one bobbin containing one polytetrafluoroethylene multi-layer coils (136 mL, 2.0 mm inside diameter); rotation speed at 850 rpm and the column axis horizontal had a flow of 2 mL per minute. A constant flow pump Series II (Scientific Systems Inc., Lab Alliance, Prague, Czech Republic) was connected to the HSCCC system. Four mL fractions were manually collected at an interval of 2 min. The sample was injected into the 95 mL coil using a 5 mL sample loop. The selected solvent system was a classic HEMWat (hexane:ethyl acetate:methanol:water), and the ideal ratio of each solvent was 4:6:5:5. The mobile phase was the upper phase (organic) the stationary phase was the lower phase (aqueous). The sample was dissolved in the selected solvent system and applied to the HSCCC apparatus through a 5 mL loop. The mobile phase was pumped at 2 mL per minute until the tube was 50, the rotation and the pumping of the mobile phase stopped, and we started extrusion. Thin layer chromatography (TLC) was the technique of choice to analyse all the fractions collected from HSCCC, with the mobile phase of chloroform, methanol and water (9:1:1, v/v/v). We then performed the combination of all fractions with a similar pattern on TLC.
High performance liquid chromatography (HPLC) system. The quantification of possible bioactive compounds was performed by the use of a high-performance liquid chromatography (HPLC) system. Standard ursolic acid was purchased from Sigma-Aldrich Ireland Limited (Arklow, Co., Wicklow, Ireland). Standard solutions were prepared in methanol at different concentrations (300, 250, 200, 150, 100, 50 and 25 µg/mL). A volume of 20 µL of each solution was injected in four replicates to allow the plot of a calibration curve. The HPLC system (Waters®) used was comprised of Waters 1525 binary HPLC pump, Waters 2487 dual λ absorbance detector (at λ = 215 nm), Waters 717 plus auto-sampler and breeze software. The column was a Thermo C18 column (250 × 4.6 mm, 5 μm). The mobile phase was a mixture of methanol and distilled water (95:5, v/v). A filter (Nylon66) 0.45 mm was used to filtrate the samples. A methanol solution of each extract was prepared at a final concentration of 500 µg/mL. The condition selected was an isocratic elution with a volume of 0.4 mL/min.
Formalin-induced licking test. The method used in the formalin test was similar to the methodology of Hunskaar and Hole (1987) and Gomes et al., (2007) [
31,
32]. Crude ethanol extract and its fractions were dissolved in Dimethylsulfoxide (DMSO) at a concentration of 100 mg/mL, then diluted according to the weight of mice at doses of 10, 30, 100 mg/kg in PBS. One hundred microlitres of each sample were given through oral gavage, and after one hour, 20 μL of formalin was injected in the right hind paw. Mice, pre-treated with Acetylsalicylic acid (ASA), were used as a positive group. The control group was composed of the mice only injected by formalin, while the vehicle group was composed of the ones pre-treated with PBS. The licking time response at the early phase (Phase I, 0–5 min) suggested analgesic effects, while the late one (Phase II, 15–30 min) suggested anti-inflammatory effects.
Hot plate test. The hot plate test followed the methodology described by Matheus et al., (2005) [
33]. All samples, extracts and fractions were tested for central neuropathic antinociceptive activity. A Group of mice (n = 5) were placed on a hot plate (Insight Equipment, Rio de Janeiro, Brazil) at a temperature of 55 ± 1 °C. The same concentrations of extracts as the ones used for the formalin test (10, 30, 100 mg/kg) were administered through oral gavage. The time spent licking and flicking their paws (reaction time) was recorded at intervals of 30 min. Morphine (5 mg/kg) was used as the positive control. The baseline is defined by the mean reaction time of the animal in the hot plate at 60 and 30 min before extract administration.
There are two ways to quantify the anti-nociception, one is increase in baseline (%), and another one is area under curve (AUC).
where IB = Increase in baseline (%).
Antioxidant Activity. The antioxidant activity of the extracts was by the use of the scavenging free radical potency using the DPPH, the total phenolic content determination and the total-flavonoids content determination. The DPPH assay followed the methodology described by Mensor et al., (2001) [
34]. The total phenolic assay used the Folin–Ciocalteu reagent according to the method described by Gursoy et al., (2009) [
31]. The determination of flavonoid content of the extracts followed the methodology described by Gursoy et al., (2009) [
35]. All three techniques suffered adaptations with modifications to microscale based on the description by Ramos and Boylan (2010) [
36].
Antimicrobial activity. The crude ethanol extract and its fractions were dissolved in DMSO 2% at the concentration of 100 mg/mL and 20 mg/mL; they were then diluted in Mueller–Hinton broth (for bacteria) and RPMI-MOPS (for fungi, pH = 7.2). The pure culture medium was the negative control group, while the medium inoculated with bacteria/fungi with gentamicin (for bacteria)/amphotericin B (for fungi) were the positive control groups.
For bacterial inoculum, 10 μL of inoculum and 100 μL Mueller-Hinton medium with extracts were added to 96-well plates. One hundred μL of inoculum and 200 μL RPMI medium with extracts were added to 96-well plates for fungal inoculum. The final concentration of both fungal and bacterial in each well was 5 × 105 CFU/mL. After incubation for 24 h at 37 °C, the MIC was determined visually by turbidity after adding the microbial stain—resazurin (0.005% in PBS, pH 7.2). The resazurin (blue) oxidises to the resorufin (pink) in the presence of viable cells.
Cytotoxicity by the use of MTT test. Human lung alveolar basal carcinoma epithelial cells (A549) and MDA-MB breast cancer cells received treatment with each extract and fractions (samples) at the concentrations of 1, 10, 30, 100 and 300 µg/mL for 24 and 48 h. One hundred µL of the RPMI medium containing 0.5 mg/mL MTT was added after removing the supernatants. The formed MTT-formazan crystals were dissolved in DMSO and had their absorbance measured on a FlexStation microplate reader at 540 nm. The control group—considered 100% of cell viability—consisted of the medium and cells, with no sample.
Statistical analysis. All experimental groups were performed in triplicate. All experimental groups with mice used six animals per assay. Data were analysed using GraphPad Prism 5.0 software (results described as mean ± SD). The IC50 values were obtained by linear regression and showed an acceptable coefficient of determination (R2 ≥ 0.90). Statistical significance between groups was calculated by analyses of variance (ANOVA), followed by Bonferroni’s test. p values less than 0.05 (p ≤ 0.05) characterized a significant level.