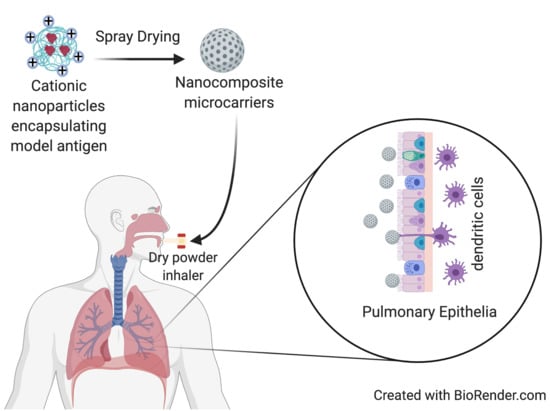
In Vitro Characterization of Inhalable Cationic Hybrid Nanoparticles as Potential Vaccine Carriers
Abstract
:1. Introduction
2. Results
2.1. Chitosan Hydrochloride Adsorption Isotherm Model
2.2. Characterization of Nanoparticles
2.3. Characterization of Nanocomposite Microparticles
2.4. In Vitro Release Analysis
2.5. Analysis of BSA Structure
2.6. Cell Viability, Nanoparticle Uptake, and Surface Marker Upregulation by DCs
3. Discussion
3.1. Chitosan Hydrochloride Adsorption Isotherm Model
3.2. Nanoparticle Characterization
3.3. Nanocomposite Microparticles Characterization
4. Materials and Methods
4.1. Materials
4.2. Methods
4.2.1. Preparation of Hybrid Cationic Chitosan Hydrochloride Nanoparticles
4.2.2. Quantification of Chitosan Hydrochloride Adsorption
4.2.3. Adsorption Isotherms Models
4.2.4. Characterization of Nanoparticles
- Size, Zeta Potential, and Polydispersity Index (PDI)
- Encapsulation efficiency and protein loading
4.2.5. Nanocomposite Microparticles Production by Spray Drying
4.2.6. Characterization of Nanocomposite Microparticles
- Morphology and particle size
- Theoretical aerodynamic diameter
4.2.7. In Vitro Aerosolization Analysis
4.2.8. In Vitro Release Study
4.2.9. Analysis of BSA Structure
4.2.10. Cell Viability Studies
4.2.11. Nanoparticle Uptake by DCs Using Confocal Microscopy
4.2.12. Nanoparticle Uptake/Adherence by DCs Using Flow Cytometry
4.2.13. DC Activation by Nanoparticles
4.2.14. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tonnis, W.F.; Kersten, G.F.; Frijlink, H.W.; Hinrichs, W.L.; de Boer, A.H.; Amorij, J.P. Pulmonary vaccine delivery: A realistic approach? J. Aerosol Med. Pulm. Drug Deliv. 2012, 25, 249–260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saleem, I.; Petkar, K.; Somavarapu, S. Chapter Nineteen—Rationale for Pulmonary Vaccine Delivery: Formulation and Device Considerations. In Micro and Nanotechnology in Vaccine Development; Skwarczynski, M., Toth, I., Eds.; William Andrew Publishing: Norwich, NY, USA, 2017; pp. 357–371. [Google Scholar]
- Irvine, D.J.; Hanson, M.C.; Rakhra, K.; Tokatlian, T. Synthetic Nanoparticles for Vaccines and Immunotherapy. Chem. Rev. 2015, 115, 11109–11146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhardwaj, V.; Ankola, D.; Gupta, S.; Schneider, M.; Lehr, C.; Kumar, M. PLGA nanoparticles stabilized with cationic surfactant: Safety studies and application in oral delivery of paclitaxel to treat chemical-induced breast cancer in rat. Pharm. Res. 2009, 26, 2495–2503. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Zheng, Y.; Tian, G.; Tian, Y.; Zeng, X.; Liu, G. Oral delivery of DMAB-modified docetaxel-loaded PLGA-TPGS nanoparticles for cancer chemotherapy. Nanoscale Res. Lett. 2011, 6, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kunda, N.; Alfagih, I.; Dennison, S.; Somavarapu, S.; Merchant, Z.; Hutcheon, G.; Saleem, I. Dry powder pulmonary delivery of cationic PGA-co-PDL nanoparticles with surface adsorbed model protein. Int. J. Pharm. 2015, 492, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Lv, H.; Zhang, S.; Wang, B.; Cui, S.; Yan, J. Toxicity of cationic lipids and cationic polymers in gene delivery. J. Control. Release 2006, 114, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Golan-Paz, S.; Frizzell, H.; Woodrow, K.A. Cross-Platform Comparison of Therapeutic Delivery from Multilamellar Lipid-Coated Polymer Nanoparticles. Macrom. Biosci. 2019, 19, 1800362. [Google Scholar] [CrossRef]
- Paecharoenchai, O.; Niyomtham, N.; Ngawhirunpat, T.; Rojanarata, T.; Yingyongnarongkul, B.-E.; Opanasopit, P. Cationic niosomes composed of spermine-based cationic lipids mediate high gene transfection efficiency. J. Drug Target 2012, 20, 783–792. [Google Scholar] [CrossRef]
- Sayın, B.; Somavarapu, S.; Li, X.; Thanou, M.; Sesardic, D.; Alpar, H.; Senel, S. Mono-N-carboxymethyl chitosan (MCC) and N-trimethyl chitosan (TMC) nanoparticles for non-invasive vaccine delivery. Int. J. Pharm. 2008, 363, 139–148. [Google Scholar] [CrossRef]
- Zhang, Y.; Niu, Y.; Luo, Y.; Ge, M.; Yang, T.; Yu, L.; Wang, Q. Fabrication, characterization and antimicrobial activities of thymol-loaded loaded zein nanoparticles stabilized by sodium caseinate–chitosan hydrochloride double layers. Food Chem. 2014, 142, 269–275. [Google Scholar] [CrossRef]
- Wei, X.; Shao, B.; He, Z.; Ye, T.; Luo, M.; Sang, Y.; Liang, X.; Wang, W.; Luo, S.; Yang, S.; et al. Cationic nanocarriers induce cell necrosis through impairment of Na+/K+-ATPase and cause subsequent inflammatory response. Cell Res. 2015, 25, 237–253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Messai, I.; Delair, T. Adsorption of Chitosan onto Poly(D,L-lactic acid) Particles: A Physico-Chemical Investigation. Macromol. Chem. Phys. 2005, 206, 1665–1674. [Google Scholar] [CrossRef]
- Mohamed, A.; Pekoz, A.Y.; Ross, K.; Hutcheon, G.A.; Saleem, I.Y. Pulmonary delivery of Nanocomposite Microparticles (NCMPs) incorporating miR-146a for treatment of COPD. Int. J. Pharm. 2019, 569, 118524. [Google Scholar] [CrossRef] [PubMed]
- Ungaro, F.; d’ Angelo, I.; Miro, A.; La Rotonda, M.; Quaglia, F. Engineered PLGA nano- and micro-carriers for pulmonary delivery: Challenges and promises. J. Pharm. Pharmacol. 2012, 64, 1217–1235. [Google Scholar] [CrossRef]
- Vranic, S.; Boggetto, N.; Contremoulins, V.; Mornet, S.; Reinhardt, N.; Marano, F.; Baeza-Squiban, A.; Boland, S. Deciphering the mechanisms of cellular uptake of engineered nanoparticles by accurate evaluation of internalization using imaging flow cytometry. Part. Fibre Toxicol. 2013, 10, 1–16. [Google Scholar] [CrossRef]
- Fröhlich, E. The role of surface charge in cellular uptake and cytotoxicity of medical nanoparticles. Int. J. Nanomed. 2012, 7, 5577–5591. [Google Scholar] [CrossRef] [Green Version]
- Langmuir, I. The constitution and fundamental properties of solids and liquids. Part1. Solids. J. Am. Chem. Soc. 1916, 38, 2221–2295. [Google Scholar] [CrossRef] [Green Version]
- Haring, M.M. Colloid and Capillary Chemistry (Freundlich, Herbert). J. Chem. Educ. 1926, 3, 1454. [Google Scholar] [CrossRef] [Green Version]
- Muherei, M.; Junin, R. Equilibrium Adsorption Isotherms of Anionic, Nonionic Surfactants and Their Mixtures to Shale and Sandstone. Mod. App. Sci. 2009, 3, 158–167. [Google Scholar] [CrossRef] [Green Version]
- Chirife, J.; Iglesias, H.A. Equations for fitting water sorption isotherms of foods: Part 1—A review. Int. J. Food Sci. Technol. 1978, 13, 159–174. [Google Scholar] [CrossRef]
- Croll, T.I.; O’Connor, A.J.; Stevens, G.W.; Cooper-White, J.J. A Blank Slate? Layer-by-Layer Deposition of Hyaluronic Acid and Chitosan onto Various Surfaces. Biomacromolecules 2006, 7, 1610–1622. [Google Scholar] [CrossRef]
- Mura, S.; Hillaireau, H.; Nicolas, J.; Le Droumaguet, B.; Gueutin, C.; Zanna, S.; Tsapis, N.; Fattal, E. Influence of surface charge on the potential toxicity of PLGA nanoparticles towards Calu-3 cells. Int. J. Nanomed. 2011, 6, 2591–2605. [Google Scholar]
- Wang, M.; Zhang, Y.; Feng, J.; Gu, T.; Dong, Q.; Yang, X.; Sun, Y.; Wu, Y.; Chen, Y.; Kong, W. Preparation, characterization, and in vitro and in vivo investigation of chitosan-coated poly (d,l-lactide-co-glycolide) nanoparticles for intestinal delivery of exendin-4. Int. J. Nanomed. 2013, 8, 1141–1154. [Google Scholar]
- Tawfeek, H.; Khidr, S.; Samy, E.; Ahmed, S.; Murphy, M.; Mohammed, A.; Shabir, A.; Hutcheon, G.; Saleem, I. Poly(Glycerol Adipate-co-ω-Pentadecalactone) Spray-Dried Microparticles as Sustained Release Carriers for Pulmonary Delivery. Pharm. Res. 2011, 28, 2086–2097. [Google Scholar] [CrossRef] [Green Version]
- Chronopoulou, L.; Massimi, M.; Giardi, M.F.; Cametti, C.; Devirgiliis, L.C.; Dentini, M.; Palocci, C. Chitosan-coated PLGA nanoparticles: A sustained drug release strategy for cell cultures. Colloids Surf. B Biointerfaces 2013, 103, 310–317. [Google Scholar] [CrossRef]
- He, J.; Feng, M.; Zhou, X.; Ma, S.; Jiang, Y.; Wang, Y.; Zhang, H. Stabilization and encapsulation of recombinant human erythropoietin into PLGA microspheres using human serum albumin as a stabilizer. Int. J. Pharm. 2011, 416, 69–76. [Google Scholar] [CrossRef]
- Slutter, B.; Bal, S.; Keijzer, C.; Mallants, R.; Hagenaars, N.; Que, I.; Kaijzel, E.; van Eden, W.; Augustijns, P.; Lowik, C.; et al. Nasal vaccination with N-trimethyl chitosan and PLGA based nanoparticles: Nanoparticle characteristics determine quality and strength of the antibody response in mice against the encapsulated antigen. Vaccine 2010, 28, 6282–6291. [Google Scholar] [CrossRef] [PubMed]
- Abo-Elseoud, W.S.; Hassan, M.L.; Sabaa, M.W.; Basha, M.; Hassan, E.A.; Fadel, S.M. Chitosan nanoparticles/cellulose nanocrystals nanocomposites as a carrier system for the controlled release of repaglinide. Int. J. Biol. Macromol. 2018, 111, 604–613. [Google Scholar] [CrossRef]
- Paul, P.; Sengupta, S.; Mukherjee, B.; Shaw, T.K.; Gaonkar, R.H.; Debnath, M.C. Chitosan-coated nanoparticles enhanced lung pharmacokinetic profile of voriconazole upon pulmonary delivery in mice. Nanomedicine 2018, 13, 501–520. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Yang, L.; Wan, F.; Bera, H.; Cun, D.; Rantanen, J.; Yang, M. Quality by design thinking in the development of long-acting injectable PLGA/PLA-based microspheres for peptide and protein drug delivery. Int. J. Pharm. 2020, 585, 119441. [Google Scholar] [CrossRef] [PubMed]
- Thompson, C.J.; Hansford, D.; Munday, D.L.; Higgins, S.; Rostron, C.; Hutcheon, G.A. Synthesis and Evaluation of Novel Polyester-Ibuprofen Conjugates for Modified Drug Release. Drug Dev. Ind. Pharm. 2008, 34, 877–884. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Ma, X.; Guo, Y.; Yang, L.; Shen, Q.; Wang, H.; Ma, Z. Size-controllable preparation of bovine serum albumin-conjugated PbS nanoparticles. Mat. Chem. Phys. 2010, 119, 112–117. [Google Scholar] [CrossRef]
- Abbate, V.; Kong, X.; Bansal, S.S. Photocrosslinked bovine serum albumin hydrogels with partial retention of esterase activity. Enzym. Microb. Technol. 2012, 50, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Scheiblhofer, S.; Laimer, J.; Machado, Y.; Weiss, R.; Thalhamer, J. Influence of protein fold stability on immunogenicity and its implications for vaccine design. Expert Rev. Vaccines 2017, 16, 479–489. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.; Zhang, Z.; Liu, H.; Tian, M.; Zhu, X.; Zhang, Z.; Wang, W.; Zhou, X.; Zhang, F.; Ge, Q.; et al. B Cells Are the Dominant Antigen-Presenting Cells that Activate Naive CD4(+) T Cells upon Immunization with a Virus-Derived Nanoparticle Antigen. Immunity 2018, 49, 695–708.e694. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fox, C.B.; Kramer, R.M.; Barnes, V.L.; Dowling, Q.M.; Vedvick, T.S. Working together: Interactions between vaccine antigens and adjuvants. Adv. Vaccines 2013, 1, 7–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwon, Y.; Standley, S.; Goh, S.; Frechet, J. Enhanced antigen presentation and immunostimulation of dendritic cells using acid-degradable cationic nanoparticles. J. Control. Release 2005, 105, 199–212. [Google Scholar] [CrossRef]
- Wischke, C.; Lorenzen, D.; Zimmermann, J.; Borchert, H. Preparation of protein loaded poly(D,L-lactide-co-glycolide) microparticles for the antigen delivery to dendritic cells using a static micromixer. Eur. J. Pharm. Biopharm. 2006, 62, 247–253. [Google Scholar] [CrossRef]
- Planelles, L.; Thomas, M.C.; Marañón, C.; Morell, M.; López, M.C. Differential CD86 and CD40 co-stimulatory molecules and cytokine expression pattern induced by Trypanosoma cruzi in APCs from resistant or susceptible mice. Clin. Exp. Immunol. 2003, 131, 41–47. [Google Scholar] [CrossRef]
- McGruder, E.D.; Moore, G.M. Use of lipopolysaccharide (LPS) as a positive control for the evaluation of immunopotentiating drug candidates in experimental avian colibacillosis models. Res. Vet. Sci. 1999, 66, 33–37. [Google Scholar] [CrossRef]
- Haase, C.; Michelsen, B.K.; Jorgensen, T.N. CD40 is necessary for activation of naive T cells by a dendritic cell line in vivo but not in vitro. Scand. J. Immunol. 2004, 59, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Sansom, D.M. CD28, CTLA-4 and their ligands: Who does what and to whom? Immunology 2000, 101, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Villadangos, J.A.; Cardoso, M.A.; Steptoe, R.J.; van Berkel, D.; Pooley, J.; Carbone, F.R.; Shortman, K. MHC Class II Expression Is Regulated in Dendritic Cells Independently of Invariant Chain Degradation. Immunity 2001, 14, 739–749. [Google Scholar] [CrossRef] [Green Version]
- Udenfriend, S.; Stein, S.; Bohlen, P.; Dairman, W.; Leimgruber, W.; Weigele, M. Fluorescamine: A reagent for assay of amino acids, peptides, proteins, and primary amines in the picomole range. Science 1972, 178, 871–872. [Google Scholar] [CrossRef]
- Brunauer, S.; Emmett, P.H.; Teller, E. Adsorption of Gases in Multimolecular Layers. J. Am. Chem. Soc. 1938, 60, 309–319. [Google Scholar] [CrossRef]
- Halsey, G. Physical Adsorption on Non-Uniform Surfaces. J. Chem. Phys. 1948, 16, 931–937. [Google Scholar] [CrossRef]
- Greenfield, N. Using circular dichroism spectra to estimate protein secondary structure. Nat. Protoc. 2006, 6, 2876–2890. [Google Scholar] [CrossRef]
- Henzler Wildman, K.; Lee, D.-K.; Ramamoorthy, A. Mechanism of Lipid Bilayer Disruption by the Human Antimicrobial Peptide, LL-37. Biochemistry 2003, 42, 6545–6558. [Google Scholar] [CrossRef]
- Whitmore, L.; Woollett, B.; Miles, A.; Janes, R.; Wallance, B. The protein circular dichrosim data bank, a Web-based site for access to circular dichrosim spectroscopic data. Structure 2010, 18, 1267–1269. [Google Scholar] [CrossRef] [Green Version]
- Whitmore, L.; Wallace, B. DICHROWEB, an online server for protein secondary structure analyses from circular dichroism spectroscopic data. Nucleic Acids Res. 2004, 32, W668–W673. [Google Scholar] [CrossRef] [Green Version]









| Isotherm Equations | Adsorption Capacity | Adsorption Intensity | Regression Coefficient |
|---|---|---|---|
| Langmuir * | qm = 1.2366 | b = −0.2149 | 0.9167 |
| Langmuir | qm = 2.28 | b = 0.146 | 0.8415 |
| BET | qm = 0.4288 | b = 0.8561 | 0.0015 |
| Freundlich | k = 0.2893 | n = 0.5434 | 0.9988 |
| Halsey | k = 1.9422 | n = 0.5406 | 0.9974 |
| Formulation | Zero Order | First Order | Higuchi | |||
|---|---|---|---|---|---|---|
| r2 | ko (h−1) | r2 | K1 (h−1) | r2 | k1 (h−½) | |
| Cationic CHL NPs/NCMPs | 0.777 | 1.218 | 0.919 | −0.016 | 0.928 | 9.316 |
| BSA | Helix | Strands | Turns | Unordered |
|---|---|---|---|---|
| Standard | 51.5 ± 0.007 | 21.5 ± 0.007 | 9.0 ± 0 | 17.5 ± 0.007 |
| Released | 43.0 ± 0.007 | 29.0 ± 0.014 | 7.0 ± 0 | 20.5 ± 0.007 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfagih, I.M.; Kaneko, K.; Kunda, N.K.; Alanazi, F.; Dennison, S.R.; Tawfeek, H.M.; Saleem, I.Y. In Vitro Characterization of Inhalable Cationic Hybrid Nanoparticles as Potential Vaccine Carriers. Pharmaceuticals 2021, 14, 164. https://doi.org/10.3390/ph14020164
Alfagih IM, Kaneko K, Kunda NK, Alanazi F, Dennison SR, Tawfeek HM, Saleem IY. In Vitro Characterization of Inhalable Cationic Hybrid Nanoparticles as Potential Vaccine Carriers. Pharmaceuticals. 2021; 14(2):164. https://doi.org/10.3390/ph14020164
Chicago/Turabian StyleAlfagih, Iman M., Kan Kaneko, Nitesh K. Kunda, Fars Alanazi, Sarah R. Dennison, Hesham M. Tawfeek, and Imran Y. Saleem. 2021. "In Vitro Characterization of Inhalable Cationic Hybrid Nanoparticles as Potential Vaccine Carriers" Pharmaceuticals 14, no. 2: 164. https://doi.org/10.3390/ph14020164
APA StyleAlfagih, I. M., Kaneko, K., Kunda, N. K., Alanazi, F., Dennison, S. R., Tawfeek, H. M., & Saleem, I. Y. (2021). In Vitro Characterization of Inhalable Cationic Hybrid Nanoparticles as Potential Vaccine Carriers. Pharmaceuticals, 14(2), 164. https://doi.org/10.3390/ph14020164