1. Introduction
Sexually transmitted infections (STIs) are a major global cause of acute illness, infertility, long-term disability, and death, with severe medical and psychological consequences for millions of men, women and infants.
WHO/Europe advocates and assists Member States in promoting and developing human-rights-based policies and practices for STI control and prevention. According to the World Health Organization, sexually transmitted diseases (STDs) and their complications are among the top five diseases in developing countries forcing patients to seek healthcare [
1]. Neonatal diseases acquired by vertical transmission are serious complications associated with significant morbidity and mortality. STDs are also the second cause of disease-related death and loss of years of good health among young women of child-bearing age (excluding HIV).
Genital herpes is one of the most common sexually transmitted infections worldwide, with a global prevalence of 536 million people infected and an annual incidence of 23.6 million new cases [
2,
3]. This chronic disease is caused by the Herpes simplex virus (HSV) type 2, and presents a wide variability in its clinical manifestations, ranging from asymptomatic to mild or severe signs and symptoms with potential complications. There are consequently many non-diagnosed cases of genital HSV, as many people infected with HSV are unaware of their infection [
4]. Over the last thirty years, epidemiologic and molecular studies have highlighted a strong and synergistic relationship between HSV-2 and the Human Immunodeficiency Virus-1 (HIV-1), which clearly points to their capacity for co-infection [
5]. It should be noted that HSV-2 infection, even without recognized lesions, is an independent risk factor for HIV infection, such that the risk of HIV acquisition is three times higher in people with HSV-2. The resulting mucosal disruption caused by genital ulcers offers an effective entry route for HIV-1. This could be prevented by high concentrations of antiviral in the genital mucosa, thereby reducing the increased susceptibility to HIV-1 infection associated with HSV-2 [
6,
7,
8,
9]. While the probability of male-to-female transmission of STDs is alarmingly high, the same is not universally true for female-to-male transmission. Current methods of preventing STDs, such as abstinence, condoms, and monogamy are frequently ineffective and out of women’s control [
10], making it advisable to design novel female-controlled barrier techniques, such as microbicides and female condoms [
11]. Microbicides are currently emerging as a promising tool to protect women from STDs. A vaginal microbicide is any topical agent/formulation intended to prevent sexual pathogens, either by inactivating or killing cellular mechanisms, by forming a physical barrier between cells and pathogens, or by enhancing the natural protective mechanisms of the cervix and vagina. Unfortunately, many vaginal microbicide formulations may fail to elicit a protective response due to their lack of efficacy and inadequate formulation. Some of the most commonly used vaginal dosage forms include creams, gels, tablets, films, tampons, vaginal rings, and douches. Each of these formulations has specific advantages and limitations. Tablets can also be designed to perform a controlled-release of the microbicide over a prolonged period of time.
Several studies reveal that acyclovir (ACV) is a safe and effective drug for vaginal administration, and some clinical benefits have been observed in the treatment of primary or recurrent lesions from genital herpes [
12,
13]. Several studies on the prevention of genital herpes transmission have examined the inclusion of acyclovir as a microbicide drug in vaginal formulations such as gels [
14], intravaginal rings [
15,
16], microporous matrices [
17] or nanoparticles [
18]. Vaginal bioadhesive tablets of acyclovir have been developed using different excipients such as methyl-cellulose, carboxy-methyl-cellulose, hydroxyl-propyl-cellulose, showing the dissolution results an inadequate behavior because of disintegration of tablets in the first 30 min. However, when hydroxyl-propyl-methyl-cellulose was incorporated to tablets, ACV release was prolonged during at least 8 h [
19]. Gurumurthy
et al. designed xanthan gum/Carbopol
® 934P-based acyclovir vaginal tablets obtaining sustained drug release data for 12 h in simulated vaginal fluid [
20].
Mucoadhesive polymers have an excellent binding capacity with mucosal tissues over a considerable period of time. Several studies have been conducted on the incorporation of tragacanth, Carbopol
®, Poloxamer 407
®, pectin, sodium alginate, cellulose derivatives, and chitosan, among others, into vaginal formulations in order to increase the residence time of these formulations at the site of action [
21,
22,
23].
Chitosan is a natural polysaccharide produced by the partial deacetylation of chitin, the structural element in the exoskeleton of crustaceans such as crabs and shrimps. The amino group in chitosan has a pKa value of approximately 6.5, which leads to protonation in an acidic solution with a density of charge dependent on the pH and the % deacetylation value. Chitosan has water soluble and bioadhesive properties with negatively charged surfaces, such as mucosal membranes, and can be used to transport a drug to an acidic environment where it can be degraded, thereby releasing the drug to the desired site. It is biocompatible and biodegradable and is widely used as a pharmaceutical excipient in a range of formulations such as powders, tablets, emulsions, and gels. The use of chitosan as a mucoadhesive polymer for vaginal delivery systems has been studied by several researchers [
24,
25,
26].
Carrageenan is a member of the family of linear sulfated polysaccharides extracted from red edible seaweeds, which are widely used in the pharmaceutical industry for their gelling, thickening, and stabilizing properties. There are three main varieties of carrageenan, with differing degrees of sulfation. Kappa-carrageenan has one sulfate group per disaccharide,
iota-carrageenan has two sulfates per disaccharide and
lambda carrageenan has three. Liu
et al. [
27] developed an
in situ kappa-carrageenan/poloxamer 407 vaginal gel with prolonged local residence. There is also evidence that carrageenan-based gel may offer some protection against HSV-2 transmission by binding with the receptors on the herpes virus, thus preventing the virus from binding to cells [
28].
Cellulose derivatives have also been applied as drug delivery excipients in vaginal formulations. For instance, hydroxyl-ethyl-cellulose is a FDA-approved polymer found in a wide range of applications, because it is non-irritant and non-toxic to the vagina [
29,
30]. Methylcellulose has been used in the development of vaginal hydrogels due to its good biocompatibility and bioadhesion [
31].
Other formulations, such as vaginal rings, gels or creams, vaginal tablets and compacts are easily manufactured, economical, stable under different environmental conditions, and easy to handle. If these solid formulations include the appropriate mucoadhesive polymer, or polymer mixture, an optimum formulation can be obtained for the in situ controlled release of the drug in the area where the transmission of vaginal herpes occurs.
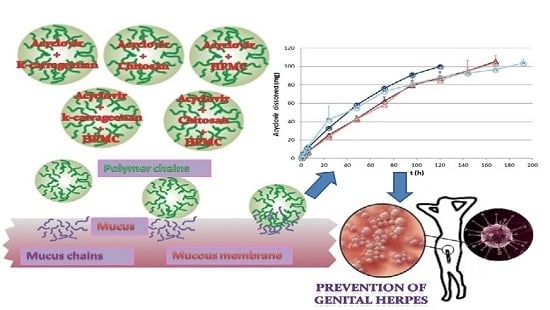
With this background, the aim of this paper is to develop natural polymer-based vaginal mucoadhesive solid formulations for the controlled release of acyclovir, which may prevent the sexual transmission of HSV. Infection with HSV can increase the risk of infection with other pathogens, such as HIV.
2. Results and Discussion
In order to achieve optimal acyclovir controlled release mucoadhesive formulations, two types of solid systems were prepared containing 100 mg of acyclovir and natural and/or semisynthetic mucoadhesive polymers: compacts and compacted granules.
Table 1 shows the composition (mg/unit) of these formulations.
Table 1.
Composition (mg/unit) of prepared compacts and compacted granules.
Table 1.
Composition (mg/unit) of prepared compacts and compacted granules.
| Batch | Chitosan | k-Carrageenan | HPMC100 | ACP | PVP | MgS | Acyclovir |
|---|
| CQ | 225 | | | | | 3 | 100 |
| CK | | 225 | | | | 3 | 100 |
| CH | | | 225 | | | 3 | 100 |
| CQH1 | 135 | | 90 | | | 3 | 100 |
| CQH2 | 90 | | 135 | | | 3 | 100 |
| CKH1 | | 135 | 90 | | | 3 | 100 |
| CKH2 | | 90 | 135 | | | 3 | 100 |
| CGQH1 | 135 | | 90 | 45 | 27 | 3 | 100 |
| CGQH2 | 90 | | 135 | 45 | 27 | 3 | 100 |
| CGKH1 | | 135 | 90 | 45 | 27 | 3 | 100 |
| CGKH2 | | 90 | 135 | 45 | 27 | 3 | 100 |
2.1. Release Studies
Figure 1 shows the release profiles of acyclovir for all formulations assayed in simulated vaginal fluid (SVF) (graphs A, B, and C) and simulated vaginal fluid/simulated seminal fluid mixture (SVF/SSF) (graph D). The data from compacts prepared with polymer/acyclovir binary physical mixtures (CQ, CK, and CH) show that all the polymers control acyclovir release, but at different rates (graph A).
Kappa-carrageenan compacts (CK) produced drug release in 48 h, while samples of chitosan formulation (CQ) extend ACV release to 120 h. In both cases the swelling, disintegration, and dissolution of the formulation—the mechanisms controlling the release of A—were visually observed. Drug release was more prolonged when ACV was formulated with HPMC (CH), and the release was incomplete, as an asymptotic trend was observed in the release profile after 92 h of the test. At the conclusion of the release study it was observed that the CH compact core remained dry. The explanation is that in an aqueous medium HPMC forms a strong gel layer that prevents fluid from accessing the compact and hinders the dissolution of 100% of the dose of acyclovir. In the light of these findings, new formulations were designed combining a marine origin polymer such as chitosan or kappa-carrageenan with HPMC in order to exploit the benefits of both types of polymers. These include the swelling/dissolution—shown by the natural polymers studied—and the robustness of HPMC, which swells but will not dissolve in an aqueous medium.
Figure 1 (graph B) shows the ACV release profiles obtained from the compacts formulated with the marine polymer/HPMC mixtures. As can be noted from the data, chitosan/HPMC compacts (CQH1 and CQH2) allow a complete and sustained release of ACV over a period of 168 h. Moreover, there are no appreciable differences between both profiles although they contain different chitosan/HPMC ratios. In contrast, kappa-carrageenan/HPMC compacts show total ACV release, but the time needed to achieve this depended on the kappa-carrageenan/HPMC ratio. The formulation containing the highest ratio of kappa-carrageenan (CKH1) released 100% of ACV in 120 h, whereas the CKH2 formulation required 192 h to release all of the drug. This may be the result of the ability of the kappa-carrageenan compacts to erode, as has been described by Bettini
et al. [
32] for the metoprolol/λ-carrageenan matrix. The chitosan-based compacts showed a strong interaction between chitosan and HPMC, and a more controlled release of ACV, regardless of the chitosan/HPMC ratio.
Figure 1.
Acyclovir release profiles obtained from compacts and compacted granules in simulated vaginal fluid (A, B, and C) and simulated vaginal fluid/simulated seminal fluid mixture (D). All values represent the mean ± SD (n = 3).
Figure 1.
Acyclovir release profiles obtained from compacts and compacted granules in simulated vaginal fluid (A, B, and C) and simulated vaginal fluid/simulated seminal fluid mixture (D). All values represent the mean ± SD (n = 3).
In order to prolong ACV release time, compacted granules were made by granulating physical ACV/polymer mixtures.
Figure 1C shows the dissolution profiles of ACV for the compacted granule formulations. In all cases total drug release was obtained in a period of nine days (216 h). Although the systems containing the chitosan/HPMC mixture showed better controlled release of ACV, the granulation process can generally be assumed to lead to unitary systems (granules) where the presence of a binder (PVP K30) ensures the ACV+HPMC+marine polymer physical bond. The subsequent granule compaction produced robust formulations which enabled the sustained release of ACV. Since these formulations present superior ACV controlled-release characteristics, they were also tested in the simulated vaginal fluid/simulated seminal fluid mixture (SVF/SSF) to assess how the nature of the medium affected the ACV release process. The results of ACV released from CGQH1, CGQH2, CGKH1, and CGKH2 in the SVF/SSF mixture are shown in
Figure 2D, and indicate that formulations with chitosan (CGQH1 and CGQH2) had a higher ACV controlled release. This is because pH-dependent chitosan dissolves better in an acidic medium (SVF) than in a neutral medium (SVF/SSF). Based on the results of the release studies, it can be concluded that chitosan-based systems may be the most suitable for use in preventing the sexual transmission of genital herpes. Although controlled ACV release was one of the aims of this research, it is also essential to verify whether the formulation has mucoadhesive properties. We, therefore, determined the bioadhesion of all the systems developed.
2.2. Characterization of Bioadhesion
The bioadhesive behavior of the compacts and compacted granules containing chitosan and kappa-carrageenan and HPMC are shown in
Figure 2. All formulations show higher values for bioadhesion work and maximum detachment force in vaginal mucosa than for chitosan- and HPMC-based mucoadhesive acyclovir tablets in gastric mucosa [
33], and for different mucoadhesive semisolid formulations (gel-type, such as Crinone, KYJelly, zidoval, and W/S mucoadhesive emulsions) [
34].
The bioadhesive behavior of the compacts and compacted granules containing chitosan, kappa-carrageenan and/or HPMC are shown in
Figure 2A. As expected, all the formulations had mucoadhesive ability.
The data on maximum detachment (separation) force for all the formulations evaluated are generally more homogeneous than the corresponding data for bioadhesion work (
Figure 2B). This could indicate that once the samples have adhered to the mucosa, the detachment force is similar in all the formulations regardless of their composition, although a reverse behavior can be observed compared to the results for bioadhesion work. In general, greater force was required to separate each sample of chitosan-compacted formulations from vaginal mucosa: CQ > CK, CQH1 > CKH1 and CGQH1 > CGKH1. Moreover, the comparison between the detachment forces of compacted physical mixtures and compacted granule formulations (CQH1
vs. CGQH1, CQH2
vs. CGQH2, CKH1
vs. CGKH1, and CKH2
vs. CGKH2) clearly reveals a decrease in detachment forces for compacted granules with regard to the corresponding compacted physical mixtures; when PVP (binder agent) and ADCP (structural excipient) were included in the formulations, these excipients act as impurities that prevent the polymers from performing their mucoadhesive function.
Figure 2.
Vaginal bioadhesion work and maximum detachment force obtained for compacts and compacted granules (Mean Values + Standard Deviation, n = 6).
Figure 2.
Vaginal bioadhesion work and maximum detachment force obtained for compacts and compacted granules (Mean Values + Standard Deviation, n = 6).
2.3. Bioadhesion Residence Test
Once it was verified that all the prepared formulations had mucoadhesive properties, the next step was to determine how long they remained bonded to the vaginal mucosa.
Table 2 shows the periods of time this adhesion lasted when formulations were immersed in SVF and SVF/SSF. CQ and CK samples remained adhered to the vaginal mucosa for less than 30 min in the case of simulated vaginal fluid, while CH samples remained for 120 h. The mucoadhesive ability of HPMC has been extensively verified, and appears to derive from its stronger hydrogen bonding with the mucin compared to other natural polymers [
35,
36]. Therefore the combination of HPMC with marine polymers (chitosan or kappa-carrageenan) may produce a longer attachment according to data obtained from both natural polymers. As expected, CQH1, CQH2, CKH1, and CKH2 remained adhered to mucosa for a longer period of time (between 72 and 108 h) than CQ and CK samples. The longer bonding time of CKH1 and CKH2 samples compared to CQH1 and CQH2 is due to kappa-carrageenan’s ability to form strong gels in the presence of potassium ions, which are part of the SVF composition. In other words, formulations that contain this polymer remain adhered to vaginal mucosa for longer than systems with chitosan. Chitosan is a polycationic copolymer consisting of glucosamine and
N-acetylglucosamine units that are primarily responsible for swelling and the ensuing dissolution in contact with acidic fluid, and also have OH and NH
2 groups that are considered essential for mucoadhesion [
37].
Table 2.
Bioadhesion residence time of acyclovir compacts and compacted granule formulations in simulated vaginal fluid (SVF) and simulated vaginal fluid/simulated seminal fluid (SVF/SSF) mixture.
Table 2.
Bioadhesion residence time of acyclovir compacts and compacted granule formulations in simulated vaginal fluid (SVF) and simulated vaginal fluid/simulated seminal fluid (SVF/SSF) mixture.
| Sample | Bioadhesion Residence Time in SVF | Bioadhesion Residence Time in SVF/SSF |
|---|
| CQ | <30 min | --- |
| CK | <30 min | --- |
| CH | 120 h | --- |
| CQH1 | 72 h | --- |
| CQH2 | 72 h | --- |
| CKH1 | 96 h | --- |
| CKH2 | 108 h | --- |
| CGQH1 | 72 h | 72 h |
| CGQH2 | 72 h | 96 h |
| CGKH1 | 72 h | 72 h |
| CGKH2 | 72 h | 72 h |
The incorporation of a structural agent—anhydrous calcium hydrogen phosphate (ACP)—and a binder—polyvinyl pyrrolidone (PVP)—into the polymer blend to prepare wet granules produces compacted granules that remained adhered to the vaginal mucosa for the same period of time (72 h), regardless of the formulation composition or the pH of the medium (SFV or SVF/SSF mixture). This indicates that formulations obtained by combining HPMC with a natural polymer are reliable enough to remain adhered to the vaginal site for the time required to achieve ACV release, and consequently prevent the sexual transmission of genital herpes. If formulations were entirely composed of one polymer (chitosan, kappa-carrageenan or HPMC) they would have inappropriate mucoadhesion values, which may be deficient in the case of chitosan or kappa-carrageenan and excessive for HPMC.
2.4. Swelling Behavior
Swelling processes were visually detected during release studies and mucoadhesion tests; however, it is very important to quantify this process, as the swelling curves can help explain the release results. Swelling ratio (SR) values obtained from all formulations determined in SVF are shown in
Figure 3. Each positive SR value indicates that at a given time the swollen matrix weight was higher than that of the dry system weight (
t = 0). Conversely, each negative SR value shows that the weight of the swollen system was lower than the weight of the dry system (
t = 0). The swelling data for CQ and CK formulations reveal that both polymers are erodible in acidic media, while CH has the highest swelling profile. When HPMC is combined with chitosan or carrageenan, the formulations showed intermediate swelling, which would be more acceptable in terms of patient comfort. An analysis of all the formulations made with polymer mixtures showed that their swelling behavior was conditioned by two factors: the nature of the natural polymer (chitosan or kappa-carrageenan), and the type of formulation (compact or compacted granules). Compact formulations with chitosan—CQH1 and CQH2—displayed lower swelling values than the kappa-carrageenan-based samples (CKH1 and CKH2). The explanation is that the presence of chitosan prevents HPMC’s own swelling pattern, as it produces a mixed HPMC/chitosan gel. CKH1 and CKH2 had very similar swelling profiles for the first 48 h of the test, with a subsequent decrease in weight in inverse proportion to their HPMC content (CKH1 weight loss is greater than CKH2 weight loss), as kappa-carrageenan is unable to interact with HPMC. CKH1 and CKH2 swelling curves therefore have a similar shape to the CH swelling curve. The areas under the swelling curve are related to the amount of HPMC in each formulation.
The swelling behavior of all compacted granule formulations is very similar, as they all showed swelling peaks between 350% and 510%, although the chitosan-based formulations CGQH1 and CGQH2 had a lower maximum swelling (350% and 452%, respectively). ACP plays a key role in the swelling process in these formulations. In formulations with kappa-carrageenan (CGKH1 and CGKH2), ACP creates a structure that prevents the free swelling of HPMC. In formulations with chitosan, the ACP structure prevents the formation of the HPMC-chitosan mixed gel. In other words, ACP acts by modulating the swelling of the polymers, resulting in systems with a similar swelling ratio which are very different from those obtained from formulations without this carrier.
Figure 3.
Swelling profiles obtained from compacts and compacted granules in simulated vaginal fluid.
Figure 3.
Swelling profiles obtained from compacts and compacted granules in simulated vaginal fluid.
2.5. Cell Toxicity
The biocompatibility of the different formulations was evaluated through in vitro cellular toxicity assays. The toxicity of the components was studied by incubation at room temperature for 48 h at different concentrations before the assay to ensure that any potential toxic component of the materials would be present in the dilution. The cell culture was then treated with a suspension of the different dilutions. All the components were tested at a maximum concentration of 1000 μg/mL, except for chitosan, which was tested at 250 μg/mL due to solubility problems.
Experiments were performed on a lymphoblastic cell line (MT-2) to evaluate toxicity on the immune cells present in vaginal or uterine mucosae and in the uterus epithelial cell line (HEC-1A) to assess potential damage to mucosae integrity. CC50 were calculated for the drug or empty material when possible.
As shown in
Table 3 and
Figure 4, no toxicity was detected at the concentrations tested except in the case of ACP, which showed mild toxicity in both cell lines, with a CC
50 value of around 1000 μg/mL. Acyclovir and all other materials showed no cytotoxicity at the maximum concentration tested, so CC
50 values were not calculated.
Table 3.
CC50 values of acyclovir, chitosan, kappa-carrageenan, magnesium stearate, HPMC-K100M, ACP and PVP K30 in the cytotoxic assay in both MT-2 and HEC-1A cell lines. CC50: cytotoxic concentration 50%.
Table 3.
CC50 values of acyclovir, chitosan, kappa-carrageenan, magnesium stearate, HPMC-K100M, ACP and PVP K30 in the cytotoxic assay in both MT-2 and HEC-1A cell lines. CC50: cytotoxic concentration 50%.
| Drug | Cell Line | CC50 |
|---|
| Acyclovir | MT-2 | >500 μM |
| HEC-1A | >500 μM |
| Chitosan | MT-2 | >250 μg/mL |
| HEC-1A | >250 μg/mL |
| Kappa-carrageenan | MT-2 | >1000 μg/mL |
| HEC-1A | >1000 μg/mL |
| Magnesium stearate | MT-2 | >1000 μg/mL |
| HEC-1A | >1000 μg/mL |
| HPMC-K100M | MT-2 | >1000 μg/mL |
| HEC-1A | >1000 μg/mL |
| ACP | MT-2 | ≈1000 µg/mL |
| HEC-1A | ≈1000 μg/mL |
| PVP | MT-2 | >1000 μg/mL |
| HEC-1A | >1000 μg/mL |
Figure 4.
Graphic representation of the cytotoxic evaluation of acyclovir, chitosan, kappa-carrageenan, magnesium stearate, HPMC-K100M, ACP, and PVP K30. Cytotoxicity was measured in MT-2 cells and HEC-1A cells for 48 h. Cell viability is expressed as percentage of living cells compared to a non-treated control (100%).
Figure 4.
Graphic representation of the cytotoxic evaluation of acyclovir, chitosan, kappa-carrageenan, magnesium stearate, HPMC-K100M, ACP, and PVP K30. Cytotoxicity was measured in MT-2 cells and HEC-1A cells for 48 h. Cell viability is expressed as percentage of living cells compared to a non-treated control (100%).
3. Experimental Section
3.1. Materials
Acyclovir was obtained from Lab. Reig Jofré (Toledo, Spain). Chitosan with a deacetylation degree of 97% (CH, Lot: 8826900003) was supplied by Nessler (Madrid, Spain). Kappa-carrageenan (k; batch 088K0178) was provided by Sigma-Aldrich (St. Louis, MO, USA). Hydroxyl-propyl-methyl-cellulose Methocel® K 100 M (HPMC; lot: DT352711) was a gift from Colorcon Ltd (Kent, UK). Anhydrous calcium hydrogen phosphate (ACP; batch: K93487944416) was provided by Merck (Darmstadt, Germany). Magnesium stearate PRS-CODEX (MGSt; batch: 85269 ALP) was purchased from Panreac (Barcelona, Spain). Kollidon® 30 (PVP K30; batch: 98-0820) was supplied by BASF (Ludwingshafen, Germany). All other reagents in this study were of analytical grade and used without further purification. Demineralized water was used in all cases.
3.2. Preparation of Compacts and Compacted Granules
Two types of solid formulations, compacts and compacted granules, were prepared containing natural and/or semisynthetic mucoadhesive polymers, and 100 mg of acyclovir. This selected drug amount is based in a common application of a marketed vaginal formulation (acyclovir topical cream 5% w/w). The compacts (CQ, CK, CH, CQH1, CQH2, CKH1, and CKH2) were prepared from physical mixtures of the components, while the compacted granules (CGQH1, CGQH2, CGKH1, and CGKH2) were made from the corresponding granules in a pre-compacted stage. Granules were produced by adding a PVP K30 ethanol solution (binder agent) to a physical mixture of ACV, chitosan or kappa-carrageenan, HPMC, and ACP. ACP acts as structural agent. The wet mass was then passed through a 0.5 mm mesh and dried at 40 °C for 12 h. Magnesium stearate was added to the granules before compaction. Both types of systems were compacted according to the IR spectroscopy technique. A stainless steel disk was placed in a die assembly and the sample (physical mixture or granules) was added. A stainless steel disk was inserted in the cylinder bore on top of the sample. A piston was then placed inside the cavity, and the sample was pressed with a force of 5 t for 4 min. Finally, piston and disks were dismantled from the die and the acyclovir compact was removed and stored in a desiccator until use.
3.3. Release Study
All samples were placed in 100 mL DURAN laboratory borosilicate glass bottles containing 80 mL of release medium and stored in a shaking water bath (37 °C, 15 opm). Aliquots of 5 mL were withdrawn daily and filtered through Millipore
® filters (0.45 μm). The medium was replaced with an equal volume of release medium equilibrated to temperature. Acyclovir concentrations were quantified by UV spectroscopy at a wavelength of 251 nm in a Shimadzu
® UV-1700 spectrophotometer (Kyoto, Japan). The assay was made in triplicate in each case. In order to ensure that the formulations act as effective drug delivery carriers even in the presence of semen, the acyclovir release studies were carried out in two dissolution media: SVF (pH 4.2) and a SVF/SSF mixture (pH 7.6). In the first three hours of assay, the release medium was simulated vaginal fluid which was removed from each bottle and substituted by the SVF/SSF 1:4
v/
v mixture until the end of the assay. Both media were prepared according to the methodology described in the bibliography [
38,
39].
3.4. Characterization of Bioadhesion
The bioadhesive capacity of the compacts and compacted granules was determined by measuring the maximum detachment force and the bioadhesion work using a TA-XT Plus texture analyzer (TA Instruments, Newcastle, UK), and bovine vaginal mucosa as substrate. Samples of bovine vaginal mucosa were obtained from a local slaughterhouse (Compostelana de Carnes S.L., Santiago de Compostela, Spain) immediately after slaughter. Each formulation was fixed to the upper support and the vaginal mucosa samples to the lower support using a cyanoacrylate adhesive. The mucosa was wetted with 0.5 mL of warm simulated vaginal fluid, and the system was equilibrated and maintained at 37 °C for 1 min. Finally a compression/extension stage was applied with an initial contact force of 0.5 N for 60 s to ensure close contact between the substrate and the sample, followed by an extension phase at a rate of 1 mm/s until the total separation of the components. The results were recorded as force versus elongation. Bioadhesion work was calculated as the area under the force-elongation curve. All the formulations were evaluated six-fold.
3.5. Bioadhesion Residence Test
A complementary
ex vivo mucoadhesion test was conducted based on the rotating cylinder technique [
26,
40] to evaluate the permanence of the bioadhesion of the mucoadhesive formulations to the vaginal mucosa. A sample of freshly excised vaginal bovine mucosa obtained from a local slaughterhouse was fixed with acrylic adhesive to a stainless steel prism with a width of 2 cm anda height of 3 cm. In order to provide a homogeneous force of adhesion between the vaginal mucosa and the solid formulation, each sample was placed over the vaginal mucosa and pressed with a weight of 500 g for 30 s. The prism was then placed in a dissolution USP apparatus 1 (the basket was substituted by the prism) containing 500 mL of SVF at 37 ± 0.1 °C. The prism was fully immersed and agitated at 30 rpm. The time elapsed until the complete detachment, dissolution and/or erosion of the dosage forms was visually assessed. To determine whether the presence of semen influences the time the formulation remains attached to the vaginal mucosa, the bioadhesion remanence test was conducted under the same conditions but changing the nature of the medium. The samples were maintained for three hours in SVF and the medium was then exchanged for the SVF/SSF 1:4
v/
v mixture [
26]. Two replicates of each bioadhesion residence test were carried out in all cases.
3.6. Swelling Characterization
The influence of composition on the behavior of compacts and compacted granules was studied by determining the degree of swelling in simulated vaginal fluid according to a method described by Ruiz-Caro and Veiga [
41]. Before the samples were exposed to the SFV they were glued to metallic discs with a diameter of 30 mm. The discs were then placed in beakers containing 100 mL of SFV. These beakers were placed in a thermostated water shaking bath (Selecta
® UNITRONIC320 OR, Barcelona, Spain) with an experimental temperature of 37 ± 0.1 °C and a shaking rate of 15 U/min. At specific time intervals, the samples were extracted from the test medium and blotted with filter paper to absorb the excess liquid on the sample surface before the weight evaluation. The swelling ratio (SR) of each sample was calculated according to the following equation: SR = ((Ts − Td)/Td) × 100, where Ts and Td were the weights of the swollen and dried samples respectively [
42]. All swelling tests were performed in triplicate.
3.7. Cell and Cytotoxicity
Two human cell lines were used: a lymphoblastic cell line, MT-2 [
43] and a uterus/endometrium epithelial cell line, HEC-1-A [
44] (kindly provided by María Angeles Muñoz, Hospital Gregorio Marañón, Madrid). Both cells were grown and propagated in RPMI 1640 medium supplemented with 10% (
v/
v) foetal bovine serum, 2 mM L-glutamine and 50 μg/mL streptomycin at 37 °C with a humidified atmosphere of 5% CO
2. The HEC-1-A cells were detached by removing the medium and rinsing the flask for 10 min with 1 to 2 mL of Trypsin 0.25%—EDTA 0.03% solution. The medium was replaced every third day after cell centrifugation at 1000 rpm for five minutes.
Cell toxicity was measured by the widely-used MTT (3-(4, 5-dimethylthylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) method. Cells were incubated in 96-well plates at a density of 10 × 10
4 cells per well in the case of MT-2, and 2 × 10
4 in the case of HEC-1-A in complete medium. To assess the cytotoxic effects of acyclovir and the excipients used in the different formulations, cells were exposed to fresh medium containing various concentrations of compounds, or with the same concentration of vehicle to dissolved compound (DMSO) for 48 h as controls in triplicate. The particles were suspended in water following a standard method [
45]. After 48 h of incubation, 20 μL of MTT solution (7.5 mg/mL) was added to the plate and incubated for another two hours for MT-2 cells and three hours for HEC-1-A cells. The supernatant was then carefully removed and 100 μL of dimethyl sulfoxide (DMSO) was added to each well. Absorbance at a wavelength of 550 nm was measured in a Labtech LT-4000 microplate spectrophotometer. Values of cytotoxic concentrations 50 (CC
50) were calculated using GraphPad Prism Software (non-linear regression, log inhibitor
versus response). The results of the MTT assay represent the average of at least three individual experiments.