Area-Level Walkability and the Geographic Distribution of High Body Mass in Sydney, Australia: A Spatial Analysis Using the 45 and Up Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Area
2.2. Participants
2.3. Data
2.4. Outcome Variable
2.5. Exposure Variable
2.6. Covariates
2.7. Statistical Analysis
3. Results
3.1. Prevalence Overweight and Obesity
3.2. Individual-Level Factors
3.3. Spatial Analysis
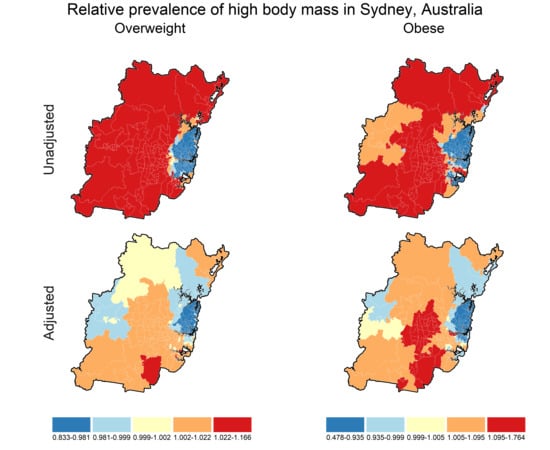
3.4. Prevalence Maps
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Gregg, E.W.; Shaw, J.E. Global Health Effects of Overweight and Obesity. N. Engl. J. Med. 2017, 377, 80–81. [Google Scholar] [CrossRef] [PubMed]
- Gakidou, E.; Afshin, A.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abdulle, A.M.; Abera, S.F.; Aboyans, V.; et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1345–1422. [Google Scholar] [CrossRef]
- Must, A.; Spadano, J.; Coakley, E.H.; Field, A.E.; Colditz, G.; Dietz, W.H. The disease burden associated with overweight and obesity. JAMA 1999, 282, 1523–1529. [Google Scholar] [CrossRef] [PubMed]
- The GBD Obesity Collaborators. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Lehnert, T.; Sonntag, D.; Konnopka, A.; Riedel-Heller, S.; König, H.H. Economic costs of overweight and obesity. Best Pract. Res. Clin. Endocrinol. Metab. 2013, 27, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Speakman, J.R. Obesity: The Integrated Roles of Environment and Genetics. J. Nutr. 2004, 134, 2090S–2105S. [Google Scholar] [CrossRef] [PubMed]
- Rutter, H.; Savona, N.; Glonti, K.; Bibby, J.; Cummins, S.; Finegood, D.T.; Greaves, F.; Harper, L.; Hawe, P.; Moore, L.; et al. The need for a complex systems model of evidence for public health. Lancet 2017, 390, 2602–2604. [Google Scholar] [CrossRef]
- Lakerveld, J.; Mackenbach, J.D.; Rutter, H.; Brug, J. Obesogenic environment and obesogenic behaviours. In Advanced Nutrition and Dietetics in Obesity; Hankey, C., Ed.; John Wiley & Sons, Incorporated: Newark, NJ, USA, 2017; Chapter 3.7; pp. 132–137. [Google Scholar]
- Saelens, B.E.; Sallis, J.F.; Frank, L.D. Environmental correlates of walking and cycling: Findings from the transportation, urban design, and planning literatures. Ann. Behav. Med. 2003, 25, 80–91. [Google Scholar] [CrossRef] [PubMed]
- Rose, G. Sick individuals and sick populations. Int. J. Epidemiol. 2001, 30, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Giles-Corti, B.; Timperio, A.; Bull, F.; Pikora, T. Understanding physical activity environmental correlates: Increased specificity for ecological models. Exerc. Sport Sci. Rev. 2005, 33, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Saelens, B.E.; Handy, S.L. Built environment correlates of walking: A review. Med. Sci. Sports Exerc. 2008, 40, S550–S566. [Google Scholar] [CrossRef] [PubMed]
- Townshend, T.; Lake, A. Obesogenic environments: Current evidence of the built and food environments. Perspect. Public Health 2017, 137, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Glass, T.A.; Curriero, F.C.; Stewart, W.F.; Schwartz, B.S. The built environment and obesity: A systematic review of the epidemiologic evidence. Health Place 2010, 16, 175–190. [Google Scholar] [CrossRef] [PubMed]
- Durand, C.P.; Andalib, M.; Dunton, G.F.; Wolch, J.; Pentz, M.A. A systematic review of built environment factors related to physical activity and obesity risk: Implications for smart growth urban planning. Obes. Rev. 2011, 12, e173–e182. [Google Scholar] [CrossRef] [PubMed]
- Mackenbach, J.D.; Rutter, H.; Compernolle, S.; Glonti, K.; Oppert, J.M.; Charreire, H.; De Bourdeaudhuij, I.; Brug, J.; Nijpels, G.; Lakerveld, J. Obesogenic environments: A systematic review of the association between the physical environment and adult weight status, the SPOTLIGHT project. BMC Public Health 2014, 14, 233. [Google Scholar] [CrossRef] [PubMed]
- Garfinkel-Castro, A.; Kim, K.; Hamidi, S.; Ewing, R. Obesity and the built environment at different urban scales: Examining the literature. Nutr. Rev. 2017, 75, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Ding, D.; Gebel, K. Built environment, physical activity, and obesity: What have we learned from reviewing the literature? Health Place 2012, 18, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Leslie, E.; Coffee, N.; Frank, L.; Owen, N.; Bauman, A.; Hugo, G. Walkability of local communities: Using geographic information systems to objectively assess relevant environmental attributes. Health Place 2007, 13, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Frank, L.D.; Saelens, B.E.; Kraft, M. Active transportation and physical activity: Opportunities for collaboration on transportation and public health research. Transp. Res. Part A Policy Pract. 2004, 38, 249–268. [Google Scholar] [CrossRef]
- Hamer, M.; Chida, Y. Active commuting and cardiovascular risk: A meta-analytic review. Prev. Med. 2008, 46, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Bird, E.L.; Ige, J.O.; Pilkington, P.; Pinto, A.; Petrokofsky, C.; Burgess-Allen, J. Built and natural environment planning principles for promoting health: An umbrella review. BMC Public Health 2018, 18, 930. [Google Scholar] [CrossRef] [PubMed]
- City Planning Department of Helsinki. Helsinki City Plan: Urban Plan—The New Helsinki City Plan, Vision 2050. Available online: https://www.hel.fi/hel2/ksv/julkaisut/yos_2013-23_en.pdf (accessed on 2 February 2019).
- Salt Lake City Council. Pedestrian & Bicycle Master Plan. Available online: https://www.slc.gov/transportation/bike/pbmp/ (accessed on 2 February 2019).
- GreaterSydneyCommission. Greater Sydney Region Plan: A Metropolis of Three Cities—Connecting People. Available online: https://www.planning.nsw.gov.au/plans-for-your-area/a-metropolis-of-three-cities/a-metropolis-of-three-cities (accessed on 17 September 2018).
- Transport for London. Walking Action Plan: Making London the World’S Most Walkable City. Available online: http://content.tfl.gov.uk/mts-walking-action-plan.pdf (accessed on 2 February 2019).
- Grasser, G.; Van Dyck, D.; Titze, S.; Stronegger, W. Objectively measured walkability and active transport and weight-related outcomes in adults: A systematic review. Int. J. Public Health 2013, 58, 615–625. [Google Scholar] [CrossRef] [PubMed]
- Giles-Corti, B.; Macaulay, G.; Middleton, N.; Boruff, B.; Bull, F.; Butterworth, I.; Badland, H.; Mavoa, S.; Roberts, R.; Christian, H. Developing a research and practice tool to measure walkability: A demonstration project. Health Promot. J. Aust. 2014, 25, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Cervero, R.; Kockelman, K. Travel demand and the 3Ds: Density, diversity, and design. Transp. Res. D Transp. Environ. 1997, 2, 199–219. [Google Scholar] [CrossRef]
- Ewing, R.; Schmid, T.; Killingsworth, R.; Zlot, A.; Raudenbush, S. Relationship between urban sprawl and physical activity, obesity, and morbidity. Am. J. Health Promot. 2003, 18, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Krizek, K.J. Operationalizing Neighborhood Accessibility for Land Use-Travel Behavior Research and Regional Modeling. J. Plan. Educ. Res. 2003, 22, 270–287. [Google Scholar] [CrossRef]
- Lopez, R. Urban sprawl and risk for being overweight or obese. Am. J. Public Health 2004, 94, 1574–1579. [Google Scholar] [CrossRef] [PubMed]
- Levine, J.; Inam, A.; Torng, G.W. A Choice-Based Rationale for Land Use and Transportation Alternatives: Evidence from Boston and Atlanta. J. Plan. Educ. Res. 2005, 24, 317–330. [Google Scholar] [CrossRef]
- Lee, C.; Moudon, A.V. The 3Ds + R: Quantifying land use and urban form correlates of walking. Transp. Res. Transp Environ. 2006, 11, 204–215. [Google Scholar] [CrossRef]
- Ross, N.A.; Tremblay, S.; Khan, S.; Crouse, D.; Tremblay, M.; Berthelot, J.M. Body mass index in urban Canada: Neighborhood and metropolitan area effects. Am. J. Public Health 2007, 97, 500–508. [Google Scholar] [CrossRef] [PubMed]
- Carr, L.J.; Dunsiger, S.I.; Marcus, B.H. Validation of Walk Score for estimating access to walkable amenities. Br. J. Sports Med. 2011, 45, 1144–1148. [Google Scholar] [CrossRef] [PubMed]
- Zick, C.D.; Hanson, H.; Fan, J.X.; Smith, K.R.; Kowaleski-Jones, L.; Brown, B.B.; Yamada, I. Re-visiting the relationship between neighbourhood environment and BMI: An instrumental variables approach to correcting for residential selection bias. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 27. [Google Scholar] [CrossRef] [PubMed]
- Frank, L.D.; Sallis, J.F.; Saelens, B.E.; Leary, L.; Cain, K.; Conway, T.L.; Hess, P.M. The development of a walkability index: Application to the Neighborhood Quality of Life Study. Br. J. Sports Med. 2010, 44, 924–933. [Google Scholar] [CrossRef] [PubMed]
- Mayne, D.J.; Morgan, G.G.; Jalaludin, B.B.; Bauman, A.E. Does Walkability Contribute to Geographic Variation in Psychosocial Distress? A Spatial Analysis of 91,142 Members of the 45 and Up Study in Sydney, Australia. Int. J. Environ. Res. Public Health 2018, 15, 275. [Google Scholar] [CrossRef] [PubMed]
- Mayne, D.; Morgan, G.; Willmore, A.; Rose, N.; Jalaludin, B.; Bambrick, H.; Bauman, A. An objective index of walkability for research and planning in the Sydney metropolitan region of New South Wales, Australia: An ecological study. Int. J. Health Geogr. 2013, 12, 61. [Google Scholar] [CrossRef] [PubMed]
- Frank, L.D.; Andresen, M.A.; Schmid, T.L. Obesity relationships with community design, physical activity, and time spent in cars. Am. J. Prev. Med. 2004, 27, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Mayne, D.J.; Morgan, G.G.; Jalaludin, B.B.; Bauman, A.E. The contribution of area-level walkability to geographic variation in physical activity: A spatial analysis of 95,837 participants from the 45 and Up Study living in Sydney, Australia. Popul. Health Metr. 2017, 15, 38. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, T.; Cole, R.; Koohsari, M.J.; Kynn, M.; Sallis, J.F.; Owen, N. Associations of local-area walkability with disparities in residents’ walking and car use. Prev. Med. 2019, 120, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Rydin, Y.; Bleahu, A.; Davies, M.; Dávila, J.D.; Friel, S.; De Grandis, G.; Groce, N.; Hallal, P.C.; Hamilton, I.; Howden-Chapman, P.; et al. Shaping cities for health: Complexity and the planning of urban environments in the 21st century. Lancet 2012, 379, 2079–2108. [Google Scholar] [CrossRef]
- Merom, D.; Ding, D.; Corpuz, G.; Bauman, A. Walking in Sydney: Trends in prevalence by geographic areas using information from transport and health surveillance systems. J. Transp. Health 2015, 2, 350–359. [Google Scholar] [CrossRef]
- Papas, M.A.; Alberg, A.J.; Ewing, R.; Helzlsouer, K.J.; Gary, T.L.; Klassen, A.C. The built environment and obesity. Epidemiol. Rev. 2007, 29, 129–143. [Google Scholar] [CrossRef] [PubMed]
- James, P.; Berrigan, D.; Hart, J.E.; Aaron Hipp, J.; Hoehner, C.M.; Kerr, J.; Major, J.M.; Oka, M.; Laden, F. Effects of buffer size and shape on associations between the built environment and energy balance. Health Place 2014, 27, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, K.; Knuiman, M.; Nathan, A.; Giles-Corti, B.; Christian, H.; Foster, S.; Bull, F. The impact of neighborhood walkability on walking: Does it differ across adult life stage and does neighborhood buffer size matter? Health Place 2014, 25, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Sato, M.; Du, J.; Inoue, Y. Rate of Physical Activity and Community Health: Evidence From U.S. Counties. J. Phys. Act. Health 2016, 13, 640–648. [Google Scholar] [CrossRef] [PubMed]
- Riley, M.W. Special Problems of Sociological Analysis. In Sociological Research: A Case Approach; Riley, M.W., Merton, R.K., Eds.; Harcourt, Brace, and World: New York, NY, USA, 1963; Volume 1, pp. 700–725. [Google Scholar]
- Alker, H.A.J. A Typology of Ecological Fallacies. In Quantitative Ecological Analysis; Dogan, M., Rokkan, S., Eds.; Massachusetts Institute of Technology Press: Cambridge, MA, USA, 1969; pp. 69–86. [Google Scholar]
- Schwartz, S. The fallacy of the ecological fallacy: The potential misuse of a concept and the consequences. Am. J. Public Health 1994, 84, 819–824. [Google Scholar] [CrossRef] [PubMed]
- Ewing, R.; Hamidi, S. Measuring Sprawl 2014; Smart Growth America: Washington, DC, USA, 2014. [Google Scholar]
- Hooper, P.; Knuiman, M.; Foster, S.; Giles-Corti, B. The building blocks of a ‘Liveable Neighbourhood’: Identifying the key performance indicators for walking of an operational planning policy in Perth, Western Australia. Health Place 2015, 36, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Fazli, G.S.; Creatore, M.I.; Matheson, F.I.; Guilcher, S.; Kaufman-Shriqui, V.; Manson, H.; Johns, A.; Booth, G.L. Identifying mechanisms for facilitating knowledge to action strategies targeting the built environment. BMC Public Health 2017, 17, 1. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.H.; Chen, Z.; Eastwood, D.B.; Yen, S.T. The effects of urban sprawl on body mass index: Where people live does matter? Consum. Interest Ann. 2006, 52, 159–169. [Google Scholar]
- Ewing, R.; Hamidi, S. Measuring Urban Sprawl and Validating Sprawl Measures; Metropolitan Research Centre: Salt Lake City, UT, USA, 2010. [Google Scholar]
- Hamidi, S.; Ewing, R.; Preuss, I.; Dodds, A. Measuring Sprawl and Its Impacts: An Update. J. Plan. Educ. Res. 2015, 35, 35–50. [Google Scholar] [CrossRef]
- Kinge, J.M.; Steingrímsdóttir, O.A.; Strand, B.H.; Kravdal, Ø. Can socioeconomic factors explain geographic variation in overweight in Norway? SSM Popul. Health 2016, 2, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Gehlert, S.; Sohmer, D.; Sacks, T.; Mininger, C.; McClintock, M.; Olopade, O. Targeting Health Disparities: A Model Linking Upstream Determinants To Downstream Interventions. Health Aff. (Millwood) 2008, 27, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Pattenden, S.; Casson, K.; Cook, S.; Dolk, H. Geographical variation in infant mortality, stillbirth and low birth weight in Northern Ireland, 1992–2002. J. Epidemiol. Commun. Health 2011, 65, 1159–1165. [Google Scholar] [CrossRef] [PubMed]
- Congdon, P. Variations in obesity rates between US counties: Impacts of activity access, food environments, and settlement patterns. Int. J. Environ. Res. Public Health 2017, 14, 1023. [Google Scholar] [CrossRef] [PubMed]
- Sichieri, R.; Coitinho, D.C.; Leão, M.M.; Recine, E.; Everhart, J.E. High temporal, geographic, and income variation in body mass index among adults in Brazil. Am. J. Public Health 1994, 84, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Willms, J.D.; Tremblay, M.S.; Katzmarzyk, P.T. Geographic and Demographic Variation in the Prevalence of Overweight Canadian Children. Obesity 2003, 11, 668–673. [Google Scholar] [CrossRef] [PubMed]
- Ackerson, L.K.; Kawachi, I.; Barbeau, E.M.; Subramanian, S.V. Geography of underweight and overweight among women in India: A multilevel analysis of 3204 neighborhoods in 26 states. Econ. Hum. Biol. 2008, 6, 264–280. [Google Scholar] [CrossRef] [PubMed]
- Lebel, A.; Pampalon, R.; Hamel, D.; Thériault, M. The geography of overweight in Québec: A multilevel perspective. Can. J. Public Health 2009, 100, 18–23. [Google Scholar] [PubMed]
- Simen-Kapeu, A.; Khule, S.; Veugelers, P.J. Geographic Differences in Childhood Overweight, Physical Activity, Nutrition and Neighbourhood Facilities: Implications for Prevention. Can. J. Public Health 2010, 101, 128–132. [Google Scholar] [PubMed]
- El Mouzan, M.; Al Herbish, A.; Al Salloum, A.; Al Omar, A.; Qurachi, M. Regional variation in prevalence of overweight and obesity in Saudi children and adolescents. Saudi J. Gastroenterol. 2012, 18, 129–132. [Google Scholar] [CrossRef] [PubMed]
- Toft, U.; Vinding, A.L.; Larsen, F.B.; Hvidberg, M.F.; Robinson, K.M.; Glümer, C. The development in body mass index, overweight and obesity in three regions in Denmark. Eur. J. Public Health 2015, 25, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Ajayi, I.O.; Adebamowo, C.; Adami, H.O.; Dalal, S.; Diamond, M.B.; Bajunirwe, F.; Guwatudde, D.; Njelekela, M.; Nankya-Mutyoba, J.; Chiwanga, F.S.; et al. Urban–rural and geographic differences in overweight and obesity in four sub-Saharan African adult populations: A multi-country cross-sectional study. BMC Public Health 2016, 16, 1126. [Google Scholar] [CrossRef] [PubMed]
- Adachi-Mejia, A.M.; Lee, C.; Lee, C.; Carlos, H.A.; Saelens, B.E.; Berke, E.M.; Doescher, M.P. Geographic variation in the relationship between body mass index and the built environment. Prev. Med. 2017, 100, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Torres-Roman, J.S.; Urrunaga-Pastor, D.; Avilez, J.L.; Helguero-Santin, L.M.; Malaga, G. Geographic differences in overweight and obesity prevalence in Peruvian children, 2010–2015. BMC Public Health 2018, 18, 353. [Google Scholar] [CrossRef] [PubMed]
- Mayhew, S. A Dictionary of Geography; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Fischer, M.M.; Getis, A. Introduction. In Handbook of Applied Spatial Analysis: Software Tools, Methods and Applications; Fischer, M.M., Getis, A., Eds.; Springer: Berlin/Heidelberg, Germany, 2010; Chapters 1–24. [Google Scholar]
- Lawson, A.; Browne, W.J.; Vidal Rodeiro, C.L. Disease Mapping with WinBUGS and MLwiN; Statistics in Practice; Wiley: Hoboken, NJ, USA, 2003. [Google Scholar]
- Smedley, B.; Amaro, H. Advancing the Science and Practice of Place-Based Intervention. Am. J. Public Health 2016, 106, 197. [Google Scholar] [CrossRef]
- Miranda, M.L.; Edwards, S.E.; Keating, M.H.; Paul, C.J. Making the Environmental Justice Grade: The Relative Burden of Air Pollution Exposure in the United States. Int. J. Environ. Res. Public Health 2011, 8, 1755. [Google Scholar] [CrossRef] [PubMed]
- Jia, P.; Cheng, X.; Xue, H.; Wang, Y. Applications of geographic information systems (GIS) data and methods in obesity-related research. Obes. Rev. 2017, 18, 400–411. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Fisac, J.L.; Rodríguez Artalejo, F.; Guallar-Castillon, P.; Banegas Banegas, J.R.; del Rey Calero, J. Determinants of geographical variations in body mass index (BMI) and obesity in Spain. Int. J. Obes. 1999, 23, 342–347. [Google Scholar] [CrossRef]
- Ford, E.S.; Mokdad, A.H.; Giles, W.H.; Galuska, D.A.; Serdula, M.K. Geographic Variation in the Prevalence of Obesity, Diabetes, and Obesity-Related Behaviors. Obes. Res. 2005, 13, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Lathey, V.; Guhathakurta, S.; Aggarwal, R.M. The Impact of Subregional Variations in Urban Sprawl on the Prevalence of Obesity and Related Morbidity. J. Plan. Educ. Res. 2009, 29, 127–141. [Google Scholar] [CrossRef]
- Schuurman, N.; Peters, P.A.; Oliver, L.N. Are Obesity and Physical Activity Clustered? A Spatial Analysis Linked to Residential Density. Obesity 2009, 17, 2202–2209. [Google Scholar] [CrossRef] [PubMed]
- Þórisdóttir, I.E.; Kristjansson, A.L.; Sigfusdottir, I.D.; Allegrante, J.P. The landscape of overweight and obesity in Icelandic adolescents: Geographic variation in body-mass index between 2000 and 2009. J. Commun. Health 2012, 37, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Myers, C.A.; Slack, T.; Martin, C.K.; Broyles, S.T.; Heymsfield, S.B. Regional disparities in obesity prevalence in the United States: A spatial regime analysis. Obesity 2015, 23, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Dutton, D.J.; McLaren, L. How important are determinants of obesity measured at the individual level for explaining geographic variation in body mass index distributions? Observational evidence from Canada using Quantile Regression and Blinder-Oaxaca Decomposition. J. Epidemiol. Commun. Health 2016, 70, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Paquet, C.; Chaix, B.; Howard, N.; Coffee, N.; Adams, R.; Taylor, A.; Thomas, F.; Daniel, M. Geographic clustering of cardiometabolic risk factors in metropolitan centres in France and Australia. Int. J. Environ. Res. Public Health 2016, 13, 519. [Google Scholar] [CrossRef] [PubMed]
- Alkerwi, A.; Bahi, I.E.; Stranges, S.; Beissel, J.; Delagardelle, C.; Noppe, S.; Kandala, N.B. Geographic variations in cardiometabolic risk factors in Luxembourg. Int. J. Environ. Res. Public Health 2017, 14, 648. [Google Scholar] [CrossRef] [PubMed]
- Smurthwaite, K.; Bagheri, N. Using Geographical Convergence of Obesity, Cardiovascular Disease, and Type 2 Diabetes at the Neighborhood Level to Inform Policy and Practice. Prev. Chronic Dis. 2017, 14, E91. [Google Scholar] [CrossRef] [PubMed]
- Samouda, H.; Ruiz-Castell, M.; Bocquet, V.; Kuemmerle, A.; Chioti, A.; Dadoun, F.; Kandala, N.B.; Stranges, S. Geographical variation of overweight, obesity and related risk factors: Findings from the European Health Examination Survey in Luxembourg, 2013–2015. PLoS ONE 2018, 13, e0197021. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Statistical Geography: Volume 1—Australian Standard Geographical Classification (ASGC), July 2006 (Catalogue No. 1216.0); Commonwealth of Australia: Canberra, Autralia, 2006.
- Australian Bureau of Statistics. TableBuilder Basic. Available online: http://www.abs.gov.au/websitedbs/censushome.nsf/home/tablebuilder (accessed on 31 January 2018).
- Australian Bureau of Statistics. Statistical Geography: Volume 2—Census Geographic Areas, 2006 (Catalogue No. 2905.0); Commonwealth of Australia: Canberra, Australia, 2006.
- 45 and Up Study Collaborators. Cohort profile: The 45 and Up Study. Int. J. Epidemiol. 2008, 37, 941–947. [Google Scholar] [CrossRef] [PubMed]
- 45 and Up Study. Researcher Toolkit. Available online: https://www.saxinstitute.org.au/our-work/45-up-study/for-researchers/ (accessed on 31 January 2018).
- The 45 and Up Study. The 45 and Up Study Data Book—December 2011 Release. Available online: https://www.saxinstitute.org.au/our-work/45-up-study/data-book/ (accessed on 31 January 2018).
- Australian Bureau of Statistics. Socio-Economic Indexes for Areas (SEIFA)—Technical Paper, 2006; Australian Bureau of Statistics: Canberra, Australia, 2008.
- WHO Expert Committee on Physical Status. Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee; WHO Technical Report Series 854; World Health Organisation: Geneva, Switzerland, 1995. [Google Scholar]
- Ng, S.P.; Korda, R.; Clements, M.; Latz, I.; Bauman, A.; Bambrick, H.; Liu, B.; Rogers, K.; Herbert, N.; Banks, E. Validity of self-reported height and weight and derived body mass index in middle-aged and elderly individuals in Australia. Aust. N. Z. J. Public Health 2011, 35, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Van Dyck, D.; Cerin, E.; Conway, T.L.; De Bourdeaudhuij, I.; Owen, N.; Kerr, J.; Cardon, G.; Frank, L.D.; Saelens, B.E.; Sallis, J.F. Perceived neighborhood environmental attributes associated with adults’ transport-related walking and cycling: Findings from the USA, Australia and Belgium. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 70. [Google Scholar] [CrossRef] [PubMed]
- Van Dyck, D.; Cerin, E.; Conway, T.L.; De Bourdeaudhuij, I.; Owen, N.; Kerr, J.; Cardon, G.; Frank, L.D.; Saelens, B.E.; Sallis, J.F. Perceived neighborhood environmental attributes associated with adults’ leisure-time physical activity: Findings from Belgium, Australia and the USA. Health Place 2013, 19, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Cerin, E.; Conway, T.L.; Adams, M.A.; Frank, L.D.; Pratt, M.; Salvo, D.; Schipperijn, J.; Smith, G.; Cain, K.L. Physical activity in relation to urban environments in 14 cities worldwide: A cross-sectional study. Lancet 2016, 387, 2207–2217. [Google Scholar] [CrossRef]
- Astell-Burt, T.; Feng, X.; Kolt, G.S. Greener neighborhoods, slimmer people? Evidence from 246,920 Australians. Int. J. Obes. 2014, 38, 156. [Google Scholar] [CrossRef] [PubMed]
- Buchmueller, T.C.; Johar, M. Obesity and health expenditures: Evidence from Australia. Econ. Hum. Biol. 2015, 17, 42–58. [Google Scholar] [CrossRef] [PubMed]
- Charlton, K.; Kowal, P.; Soriano, M.; Williams, S.; Banks, E.; Vo, K.; Byles, J. Fruit and Vegetable Intake and Body Mass Index in a Large Sample of Middle-Aged Australian Men and Women. Nutrients 2014, 6, 2305. [Google Scholar] [CrossRef] [PubMed]
- Creatore, M.I.; Glazier, R.H.; Moineddin, R.; Fazli, G.S.; Johns, A.; Gozdyra, P.; Matheson, F.I.; Kaufman-Shriqui, V.; Rosella, L.C.; Manuel, D.G.; et al. Association of neighborhood walkability with change in overweight, obesity, and diabetes. JAMA 2016, 315, 2211–2220. [Google Scholar] [CrossRef] [PubMed]
- Joshy, G.; Korda, R.J.; Attia, J.; Liu, B.; Bauman, A.E.; Banks, E. Body mass index and incident hospitalisation for cardiovascular disease in 158,546 participants from the 45 and Up Study. Int. J. Obes. 2014, 38, 848. [Google Scholar] [CrossRef] [PubMed]
- Joshy, G.; Korda, R.J.; Bauman, A.; Van Der Ploeg, H.P.; Chey, T.; Banks, E. Investigation of Methodological Factors Potentially Underlying the Apparently Paradoxical Findings on Body Mass Index and All-Cause Mortality. PLoS ONE 2014, 9, e88641. [Google Scholar] [CrossRef] [PubMed]
- Korda, R.J.; Liu, B.; Clements, M.S.; Bauman, A.E.; Jorm, L.R.; Bambrick, H.J.; Banks, E. Prospective cohort study of body mass index and the risk of hospitalisation: Findings from 246,361 participants in the 45 and Up Study. Int. J. Obes. 2013, 37, 790. [Google Scholar] [CrossRef] [PubMed]
- Korda, R.J.; Joshy, G.; Paige, E.; Butler, J.R.G.; Jorm, L.R.; Liu, B.; Bauman, A.E.; Banks, E. The Relationship between Body Mass Index and Hospitalisation Rates, Days in Hospital and Costs: Findings from a Large Prospective Linked Data Study. PLoS ONE 2015, 10, e0118599. [Google Scholar] [CrossRef] [PubMed]
- Magee, C.A.; Caputi, P.; Iverson, D.C. Is Sleep Duration Associated With Obesity in Older Australian Adults? J. Aging Health 2010, 22, 1235–1255. [Google Scholar] [CrossRef] [PubMed]
- Magee, C.A.; Iverson, D.C.; Caputi, P. Sleep Duration and Obesity in Middle-aged Australian Adults. Obesity 2010, 18, 420–421. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, B.; Bauman, A.; Ding, D. Incident Type 2 Diabetes in a Large Australian Cohort Study: Does Physical Activity or Sitting Time Alter the Risk Associated With Body Mass Index? J. Phys. Act. Health 2017, 14, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Pedisic, Z.; Grunseit, A.; Ding, D.; Chau, J.Y.; Banks, E.; Stamatakis, E.; Jalaludin, B.B.; Bauman, A.E. High sitting time or obesity: Which came first? Bidirectional association in a longitudinal study of 32,787 Australian adults. Obesity 2014, 22, 2126–2130. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.L.T.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Use of the Kessler Psychological Distress Scale in ABS Health Surveys, Australia, 2007-08 (Catalgue No. 4817.0.55.001). Available online: http://www.abs.gov.au/ausstats/[email protected]/mf/4817.0.55.001 (accessed on 31 January 2018).
- Australian Bureau of Statistics. National Survey of Mental Health and Wellbeing: Summary of Results; Commonwealth of Australia: Canberra, Australia, 2007.
- Australian Bureau of Statistics. Australian Health Survey: Users’ Guide, 2011-13 (Catalogue No. 4363.0.55.001). Available online: http://www.abs.gov.au/ausstats/[email protected]/mf/4363.0.55.001 (accessed on 31 January 2018).
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E.; Snow, K.K.; Kosinski, M.; Gandek, B. SF-36 Health Survey: Manual and Interpretation Guide; The Health Institute, New England Medical Center: Boston, MA, USA, 1993. [Google Scholar]
- Banks, E.; Jorm, L.; Rogers, K.; Clements, M.; Bauman, A. Screen-time, obesity, ageing and disability: Findings from 91,266 participants in the 45 and Up Study. Public Health Nutr. 2011, 14, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Waller, L.; Carlin, B. Disease Mapping. In Handbook of Spatial Statistics; Gelfand, A.E., Diggle, P.J., Feuentes, M., Guttorp, P., Eds.; Chapman & Hall/CRC Handbooks of Modern Statistical Methods; CRC Press: Boca Raton, FL, USA, 2010; pp. 217–244. [Google Scholar]
- Leroux, B.G.; Lei, X.; Breslow, N. Estimation of Disease Rates in Small Areas: A new Mixed Model for Spatial Dependence. In Statistical Models in Epidemiology, The Environment, and Clinical Trials; Halloran, M.E., Berry, D., Eds.; Springer: New York, NY, USA, 2000; pp. 179–191. [Google Scholar]
- Klassen, A.C.; Kulldorff, M.; Curriero, F. Geographical clustering of prostate cancer grade and stage at diagnosis, before and after adjustment for risk factors. Int. J. Health Geogr. 2005, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Waldhoer, T.; Wald, M.; Heinzl, H. Analysis of the spatial distribution of infant mortality by cause of death in Austria in 1984 to 2006. Int. J. Health Geogr. 2008, 7, 21. [Google Scholar] [CrossRef] [PubMed]
- Besag, J.; York, J.; Mollié, A. Bayesian image restoration, with two applications in spatial statistics. Ann. Inst. Stat. Math. 1991, 43, 1–20. [Google Scholar] [CrossRef]
- Cowles, M.K.; Carlin, B.P. Markov Chain Monte Carlo Convergence Diagnostics: A Comparative Review. J. Am. Stat. Assoc. 1996, 91, 883–904. [Google Scholar] [CrossRef]
- Spiegelhalter, D.J.; Best, N.G.; Carlin, B.P.; Van Der Linde, A. Bayesian measures of model complexity and fit. J. R. Stat. Soc. Ser. B Stat. Methodol. 2002, 64, 583–639. [Google Scholar] [CrossRef]
- Cramb, S.M.; Mengersen, K.L.; Baade, P.D. Developing the atlas of cancer in Queensland: Methodological issues. Int. J. Health Geogr. 2011, 10, 9. [Google Scholar] [CrossRef] [PubMed]
- Holowaty, E.J.; Norwood, T.A.; Wanigaratne, S.; Abellan, J.J.; Beale, L. Feasibility and utility of mapping disease risk at the neighbourhood level within a Canadian public health unit: An ecological study. Int. J. Health Geogr. 2010, 9, 21. [Google Scholar] [CrossRef] [PubMed]
- Mealing, N.M.; Banks, E.; Jorm, L.R.; Steel, D.G.; Clements, M.S.; Rogers, K.D. Investigation of relative risk estimates from studies of the same population with contrasting response rates and designs. BMC Med. Res. Methodol. 2010, 10, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Mayne, D.J.; Morgan, G.G.; Jalaludin, B.B.; Bauman, A.E. Is it worth the weight? Adjusting physical activity ratio estimates for individual-level non-response is not required in area-level spatial analyses of the 45 and Up Study cohort. In Proceedings of the 45 and Up Study Annual Forum, Sydney, Australia, 24 October 2017. [Google Scholar]
- The 45 and Up Study. The 45 and Up Study Data Book—April 2010 Release. Available online: https://www.saxinstitute.org.au/our-work/45-up-study/data-book/ (accessed on 31 January 2018).
- Wasfi, R.A.; Dasgupta, K.; Orpana, H.; Ross, N.A. Neighborhood Walkability and Body Mass Index Trajectories: Longitudinal Study of Canadians. Am. J. Public Health 2016, 106, 934–940. [Google Scholar] [CrossRef] [PubMed]
- James, P.; Kioumourtzoglou, M.A.; Hart, J.E.; Banay, R.F.; Kloog, I.; Laden, F. Interrelationships Between Walkability, Air Pollution, Greenness, and Body Mass Index. Epidemiololgy 2017, 28, 780–788. [Google Scholar] [CrossRef] [PubMed]
- Kowaleski-Jones, L.; Brown, B.B.; Fan, J.X.; Hanson, H.A.; Smith, K.R.; Zick, C.D. The joint effects of family risk of obesity and neighborhood environment on obesity among women. Soc. Sci. Med. 2017, 195, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Loo, C.K.J.; Greiver, M.; Aliarzadeh, B.; Lewis, D. Association between neighbourhood walkability and metabolic risk factors influenced by physical activity: A cross-sectional study of adults in Toronto, Canada. BMJ Open 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- Méline, J.; Chaix, B.; Pannier, B.; Ogedegbe, G.; Trasande, L.; Athens, J.; Duncan, D.T. Neighborhood walk score and selected Cardiometabolic factors in the French RECORD cohort study. BMC Public Health 2017, 17, 960. [Google Scholar] [CrossRef] [PubMed]
- Australian Urban Research Infrastructure Network (AURIN). Walkability Tools. Available online: https://docs.aurin.org.au/portal-help/analysing-your-data/walkability-tools/ (accessed on 6 February 2019).
- Frank, L.D.; Kerr, J.; Sallis, J.F.; Miles, R.; Chapman, J. A hierarchy of sociodemographic and environmental correlates of walking and obesity. Prev. Med. 2008, 47, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Rutt, C.D.; Coleman, K.J. Examining the relationships among built environment, physical activity, and body mass index in El Paso, TX. Prev. Med. 2005, 40, 831–841. [Google Scholar] [CrossRef] [PubMed]
- Lunn, D.; Jackson, C.; Best, N.; Thomas, A.; Spiegelhalter, D. The BUGS Book: A Practical Introduction to Bayesian Analysis; Texts in Statistical Science; CRC Press: Boca Raton, FL, USA, 2012. [Google Scholar]
- Latouche, A.; Guihenneuc-Jouyaux, C.; Girard, C.; Hémon, D. Robustness of the BYM model in absence of spatial variation in the residuals. Int. J. Health Geogr. 2007, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Fotheringham, A.S.; Brunsdon, C.; Charlton, M. Quantitative Geography: Perspectives on Apatial Data Analysis; Sage Publications: London, UK, 2000; p. xii. 270p. [Google Scholar]
- Fitzpatrick, J.; Griffiths, C.; Goldblatt, P. Introduction to the Volume. In Geographic Variations in Health; Griffiths, C., Fitzpatrick, J., Eds.; Office for National Statistics: London, UK, 2001. [Google Scholar]
- Fontaine, K.R.; Cheskin, L.J.; Barofsky, I. Health-related quality of life in obese persons seeking treatment. J. Fam. Pract. 1996, 43, 265–270. [Google Scholar] [PubMed]
- Katz, D.A.; McHorney, C.A.; Atkinson, R.L. Impact of obesity on health-related quality of life in patients with chronic illness. J. Gen. Intern. Med. 2000, 15, 789–796. [Google Scholar] [CrossRef] [PubMed]
- Jia, H.; Lubetkin, E.I. The impact of obesity on health-related quality-of-life in the general adult US population. J. Public Health 2005, 27, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Frühbeck, G.; Toplak, H.; Woodward, E.; Yumuk, V.; Maislos, M.; Oppert, J.M. Obesity: The Gateway to Ill Health—An EASO Position Statement on a Rising Public Health, Clinical and Scientific Challenge in Europe. Obes. Facts 2013, 6, 117–120. [Google Scholar] [CrossRef] [PubMed]
- Booth, H.P.; Prevost, A.T.; Gulliford, M.C. Impact of body mass index on prevalence of multimorbidity in primary care: Cohort study. Fam. Pract. 2014, 31, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Jackson, C.A.; Dobson, A.; Tooth, L.; Mishra, G.D. Body mass index and socioeconomic position are associated with 9-year trajectories of multimorbidity: A population-based study. Prev. Med. 2015, 81, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Kivimäki, M.; Kuosma, E.; Ferrie, J.E.; Luukkonen, R.; Nyberg, S.T.; Alfredsson, L.; Batty, G.D.; Brunner, E.J.; Fransson, E.; Goldberg, M.; et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: Pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health 2017, 2, e277–e285. [Google Scholar] [CrossRef]
- Katikireddi, S.V.; Skivington, K.; Leyland, A.H.; Hunt, K.; Mercer, S.W. The contribution of risk factors to socioeconomic inequalities in multimorbidity across the lifecourse: A longitudinal analysis of the Twenty-07 cohort. BMC Med. 2017, 15, 152. [Google Scholar] [CrossRef] [PubMed]
- Stafford, M.; Hemingway, H.; Marmot, M. Current obesity, steady weight change and weight fluctuation as predictors of physical functioning in middle aged office workers: The Whitehall II study. Int. J. Obes. 1998, 22, 23–31. [Google Scholar] [CrossRef]
- Dowd, J.B.; Zajacova, A. Long-term obesity and physical functioning in older Americans. Int. J. Obes. 2015, 39, 502–507. [Google Scholar] [CrossRef] [PubMed]
- Academy of Medical Sciences. Multimorbidity: A Priority for Global Health Research; Academy of Medical Sciences: London, UK, 2018. [Google Scholar]
- Byles, J.E.; Gallienne, L.; Blyth, F.M.; Banks, E. Relationship of age and gender to the prevalence and correlates of psychological distress in later life. Int. Psychogeriatr. 2012, 24, 1009–1018. [Google Scholar] [CrossRef] [PubMed]
- Byles, J.E.; Robinson, I.; Banks, E.; Gibson, R.; Leigh, L.; Rodgers, B.; Curryer, C.; Jorm, L. Psychological distress and comorbid physical conditions: Disease or disability? Depress Anxiety 2014, 31, 524–532. [Google Scholar] [CrossRef] [PubMed]
- Ormel, J.; Rijsdijk, F.V.; Sullivan, M.; van Sonderen, E.; Kempen, G.I.J.M. Temporal and Reciprocal Relationship Between IADL/ADL Disability and Depressive Symptoms in Late Life. J. Gerontol. B Psychol. Sci. Soc. Sci. 2002, 57, P338–P347. [Google Scholar] [CrossRef] [PubMed]
- Gaddey, H.L.; Holder, K. Unintentional weight loss in older adults. Am. Fam. Physician 2014, 89, 718–722. [Google Scholar] [PubMed]
- Andrews, G.; Slade, T. Interpreting scores on the Kessler Psychological Distress Scale (K10). Aust. N. Z. J. Public Health 2001, 25, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Criqui, M.H. Response bias and risk ratios in epidemiologic studies. Am. J. Epidemiol. 1979, 109, 394–399. [Google Scholar] [CrossRef] [PubMed]
- Nohr, E.A.; Frydenberg, M.; Henriksen, T.B.; Olsen, J. Does low participation in cohort studies induce bias? Epidemiology 2006, 17, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Centre for Epidemiology and Evidence. Adult Population Health Survey. Available online: http://www.health.nsw.gov.au/surveys/adult/Pages/default.aspx (accessed on 12 December 2018).
- Department of Finance, Services and Innovation. NSW Open Data Policy. Available online: https://www.digital.nsw.gov.au/policy/data-information/making-data-open/nsw-open-data-policy (accessed on 4 February 2019).
- Plantinga, A.J.; Bernell, S. The association between urban sprawl and obesity: Is it a two-way street? J. Reg. Sci. 2007, 47, 857–879. [Google Scholar] [CrossRef]
- Eid, J.; Overman, H.G.; Puga, D.; Turner, M.A. Fat city: Questioning the relationship between urban sprawl and obesity. J. Urban Econ. 2008, 63, 385–404. [Google Scholar] [CrossRef]
- Mokhtarian, P.L.; Cao, X. Examining the impacts of residential self-selection on travel behavior: A focus on methodologies. Trans. Res. Part B Methodol. 2008, 42, 204–228. [Google Scholar] [CrossRef]
- Cao, X.; Mokhtarian, P.L.; Handy, S.L. Examining the Impacts of Residential Self-Selection on Travel Behaviour: A Focus on Empirical Findings. Transp. Rev. 2009, 29, 359–395. [Google Scholar] [CrossRef]
- Kowaleski-Jones, L.; Zick, C.; Smith, K.R.; Brown, B.; Hanson, H.; Fan, J. Walkable neighborhoods and obesity: Evaluating effects with a propensity score approach. SSM Popul. Health 2018, 6, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.R.; Zick, C.D.; Kowaleski-Jones, L.; Brown, B.B.; Fan, J.X.; Yamada, I. Effects of neighborhood walkability on healthy weight: Assessing selection and causal influences. Soc. Sci. Res. 2011, 40, 1445–1455. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.R.; Hanson, H.A.; Brown, B.B.; Zick, C.D.; Kowaleski-Jones, L.; Fan, J.X. Movers and stayers: How residential selection contributes to the association between female body mass index and neighborhood characteristics. Int. J. Obes. 2016, 40, 1384–1391. [Google Scholar] [CrossRef] [PubMed]
- Hausman, J.A.; Abrevaya, J.; Scott-Morton, F.M. Misclassification of the dependent variable in a discrete-response setting. J. Econ. 1998, 87, 239–269. [Google Scholar] [CrossRef]
- Tennekoon, V.; Rosenman, R. Systematically misclassified binary dependent variables. Commun. Stat. Theory Method. 2016, 45, 2538–2555. [Google Scholar] [CrossRef] [PubMed]
- Openshaw, S.; Taylor, P.J. A Million or so Correlation Coefficients: Three Experiments on the Mmodifiable Areal Unit Problem. In Statistical Applications in the Spatial Sciences; Wrigley, N., Ed.; Pion: London, UK, 1979; pp. 127–144. [Google Scholar]
- Openshaw, S. The Modifiable Areal Unit Problem; (CATMOG 38); Geo Books: Norwich, UK, 1984. [Google Scholar]
- Greenland, S. Avoiding power loss associated with categorization and ordinal scores in dose-response and trend analysis. Epidemiology 1995, 6, 450–454. [Google Scholar] [CrossRef] [PubMed]
- Bennette, C.; Vickers, A. Against quantiles: Categorization of continuous variables in epidemiologic research, and its discontents. BMC Med. Res. Methodol. 2012, 12, 21. [Google Scholar] [CrossRef] [PubMed]
- Goovaerts, P.; Gebreab, S. How does Poisson kriging compare to the popular BYM model for mapping disease risks? Int. J. Health Geogr. 2008, 7, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Huque, M.H.; Anderson, C.; Walton, R.; Ryan, L. Individual level covariate adjusted conditional autoregressive (indiCAR) model for disease mapping. Int. J. Health Geogr. 2016, 15, 25. [Google Scholar] [CrossRef] [PubMed]


| Variable | Characteristics | Prevalence | ||||
|---|---|---|---|---|---|---|
| Overweight | Obesity | |||||
| N | % | n | % | n | % | |
| AREA-LEVEL VARIABLES | ||||||
| Walkability | ||||||
| Low | 25,454 | 27.6 | 10,150 | 52.9 | 6251 | 40.8 |
| Low-medium | 31,404 | 34.1 | 12,380 | 50.0 | 6655 | 35.0 |
| Medium-high | 19,449 | 21.1 | 7543 | 47.2 | 3454 | 29.0 |
| High | 15,850 | 17.2 | 5861 | 44.0 | 2516 | 25.2 |
| Socioeconomic disadvantage | ||||||
| Q1—Most | 17,425 | 18.9 | 6697 | 52.1 | 4559 | 42.5 |
| Q2 | 19,517 | 21.2 | 7579 | 51.7 | 4847 | 40.6 |
| Q3—Middling | 14,984 | 16.3 | 5877 | 49.4 | 3082 | 33.8 |
| Q4 | 19,982 | 21.7 | 7938 | 47.8 | 3392 | 28.2 |
| Q5—Least | 20,249 | 22.0 | 7843 | 45.5 | 2996 | 24.1 |
| INDIVIDUAL-LEVEL VARIABLES | ||||||
| Sex | ||||||
| Male | 44,690 | 48.5 | 20,802 | 58.1 | 8912 | 37.3 |
| Female | 47,467 | 51.5 | 15,132 | 40.3 | 9964 | 30.8 |
| Age | ||||||
| 45–49 | 13,550 | 14.7 | 4871 | 45.1 | 2761 | 31.8 |
| 50–54 | 16,723 | 18.1 | 6188 | 47.4 | 3665 | 34.8 |
| 55–59 | 16,717 | 18.1 | 6568 | 51.2 | 3885 | 38.3 |
| 60–64 | 13,742 | 14.9 | 5696 | 53.7 | 3136 | 39.0 |
| 65–69 | 10,188 | 11.1 | 4297 | 54.0 | 2227 | 37.8 |
| 70–74 | 6910 | 7.5 | 2969 | 53.3 | 1341 | 34.0 |
| 75–79 | 4999 | 5.4 | 2047 | 49.0 | 820 | 27.8 |
| 80–84 | 6614 | 7.2 | 2513 | 43.2 | 801 | 19.5 |
| 85+ | 2714 | 2.9 | 785 | 31.7 | 240 | 12.4 |
| Language spoken at home | ||||||
| English | 78,028 | 84.7 | 30,768 | 49.9 | 16,330 | 34.6 |
| Other | 14,129 | 15.3 | 5166 | 44.6 | 2546 | 28.4 |
| Education level | ||||||
| Less than secondary school | 7434 | 8.1 | 2704 | 50.6 | 2086 | 44.1 |
| Secondary school graduation | 26,741 | 29.0 | 10,171 | 49.2 | 6052 | 36.5 |
| Trade, certificate or diploma | 28,932 | 31.4 | 11,814 | 51.8 | 6143 | 35.9 |
| University degree | 29,050 | 31.5 | 11,245 | 46.0 | 4595 | 25.8 |
| Relationship status | ||||||
| Partner | 68,759 | 74.6 | 27,826 | 50.7 | 13,863 | 33.9 |
| No partner | 23,398 | 25.4 | 8108 | 44.1 | 5013 | 32.8 |
| Employment status | ||||||
| Full-time work | 32,716 | 35.5 | 13,622 | 53.5 | 7246 | 37.9 |
| Part-time work | 13,177 | 14.3 | 4418 | 41.0 | 2408 | 27.5 |
| Other work | 1358 | 1.5 | 426 | 39.6 | 281 | 30.2 |
| Not working | 44,906 | 48.7 | 17,468 | 48.6 | 8941 | 32.6 |
| Health insurance type | ||||||
| Private with extras | 54,218 | 58.8 | 21,751 | 50.1 | 10,830 | 33.4 |
| Private without extras | 12,961 | 14.1 | 5058 | 47.2 | 2255 | 28.5 |
| Government health care card | 11,993 | 13.0 | 4351 | 47.8 | 2881 | 37.7 |
| None | 12,985 | 14.1 | 4774 | 47.4 | 2910 | 35.4 |
| Smoking status | ||||||
| Never smoked | 54,117 | 58.7 | 20,518 | 46.6 | 10,072 | 30.0 |
| Past smoker | 31,639 | 34.3 | 13,145 | 54.2 | 7397 | 40.0 |
| Current smoker | 6401 | 6.9 | 2271 | 45.5 | 1407 | 34.1 |
| Psychosocial distress | ||||||
| Low | 70,218 | 76.2 | 27,960 | 49.1 | 13,318 | 31.5 |
| Moderate | 14,573 | 15.8 | 5433 | 49.0 | 3475 | 38.0 |
| High | 5152 | 5.6 | 1828 | 48.4 | 1375 | 41.4 |
| Very high | 2214 | 2.4 | 713 | 47.3 | 708 | 47.2 |
| Diagnosed chronic conditions | ||||||
| 0 | 31,297 | 34.0 | 11,955 | 44.1 | 4218 | 21.8 |
| 1 | 36,917 | 40.1 | 14,726 | 50.2 | 7560 | 34.1 |
| 2 | 18,186 | 19.7 | 7145 | 54.4 | 5040 | 45.6 |
| 3 or more | 5757 | 6.2 | 2108 | 57.0 | 2058 | 56.4 |
| Treated chronic conditions | ||||||
| 0 | 41,580 | 45.1 | 15,904 | 45.5 | 6590 | 25.7 |
| 1 | 30,121 | 32.7 | 12,141 | 51.3 | 6448 | 35.9 |
| 2 | 14,524 | 15.8 | 5721 | 53.5 | 3835 | 43.6 |
| 3 or more | 5932 | 6.4 | 2168 | 55.2 | 2003 | 53.2 |
| Limited physical functioning | ||||||
| None | 32,392 | 35.1 | 12,656 | 44.4 | 3908 | 19.8 |
| Minor | 25,125 | 27.3 | 10,628 | 52.4 | 4838 | 33.4 |
| Moderate | 20,316 | 22.0 | 7801 | 52.8 | 5555 | 44.4 |
| Severe | 14,324 | 15.5 | 4849 | 49.7 | 4575 | 48.3 |
| SENSITIVITY VARIABLES | ||||||
| Total physical activity | ||||||
| 0 min | 5478 | 5.9 | 1868 | 50.9 | 1807 | 50.1 |
| 1–149 min | 15,365 | 16.7 | 5895 | 52.1 | 4053 | 42.8 |
| 150–299 min | 15,833 | 17.2 | 6241 | 50.5 | 3468 | 36.2 |
| ≥300 min | 55,481 | 60.2 | 21,930 | 47.7 | 9548 | 28.5 |
| Overweight | Obese | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Sex | p < 0.0001 | p < 0.0001 | ||
| Male | 1.00 | 1.00 | ||
| Female | 0.47 | 0.46–0.49 | 0.62 | 0.59–0.64 |
| Age | p < 0.0001 | p < 0.0001 | ||
| 45–49 | 1.00 | 1.00 | ||
| 50–54 | 1.00 | 0.95–1.05 | 0.94 | 0.88–1.00 |
| 55–59 | 1.07 | 1.01–1.13 | 0.90 | 0.84–0.97 |
| 60–64 | 1.08 | 1.02–1.15 | 0.76 | 0.70–0.82 |
| 65–69 | 1.00 | 0.93–1.07 | 0.59 | 0.54–0.65 |
| 70–74 | 0.87 | 0.81–0.94 | 0.39 | 0.35–0.43 |
| 75–79 | 0.66 | 0.60–0.72 | 0.23 | 0.21–0.26 |
| 80–84 | 0.50 | 0.46–0.54 | 0.12 | 0.11–0.14 |
| 85+ | 0.31 | 0.28–0.35 | 0.06 | 0.05–0.07 |
| Language spoken at home | p < 0.0001 | p < 0.0001 | ||
| English | 1.00 | 1.00 | ||
| Other | 0.81 | 0.78–0.84 | 0.72 | 0.68–0.77 |
| Education level | p < 0.0001 | p < 0.0001 | ||
| Less than secondary school | 1.53 | 1.43–1.63 | 2.47 | 2.28–2.67 |
| Secondary school graduation | 1.35 | 1.29–1.40 | 1.77 | 1.67–1.86 |
| Trade, certificate or diploma | 1.27 | 1.22–1.32 | 1.54 | 1.46–1.62 |
| University degree | 1.00 | 1.00 | ||
| Relationship status | p < 0.0001 | p = 0.1285 | ||
| Partner | 1.00 | 1.00 | ||
| No partner | 0.89 | 0.86–0.92 | 0.96 | 0.92–1.01 |
| Employment status | p < 0.0001 | p < 0.0001 | ||
| Full-time work | 1.00 | 1.00 | ||
| Part-time work | 0.75 | 0.71–0.79 | 0.61 | 0.57–0.65 |
| Other work | 0.72 | 0.64–0.82 | 0.61 | 0.52–0.71 |
| Not working | 0.78 | 0.75–0.82 | 0.66 | 0.62–0.70 |
| Health insurance type | p < 0.0001 | p < 0.0001 | ||
| Private with extras | 1.00 | 1.00 | ||
| Private without extras | 0.90 | 0.86–0.94 | 0.83 | 0.78–0.88 |
| Government health care card | 0.94 | 0.89–0.99 | 1.02 | 0.96–1.09 |
| None | 0.91 | 0.87–0.95 | 0.99 | 0.93–1.05 |
| Smoking status | p < 0.0001 | p < 0.0001 | ||
| Never smoked | 1.00 | 1.00 | ||
| Past smoker | 1.17 | 1.13–1.21 | 1.28 | 1.23–1.34 |
| Current smoker | 0.78 | 0.74–0.84 | 0.73 | 0.68–0.79 |
| Psychosocial distress | p < 0.0001 | p < 0.0001 | ||
| Low | 1.00 | 1.00 | ||
| Moderate | 0.94 | 0.90–0.98 | 0.91 | 0.86–0.96 |
| High | 0.88 | 0.82–0.95 | 0.82 | 0.76–0.89 |
| Very high | 0.83 | 0.74–0.92 | 0.88 | 0.78–1.00 |
| Diagnosed chronic conditions | p < 0.0001 | p < 0.0001 | ||
| 0 | 1.00 | 1.00 | ||
| 1 | 1.19 | 1.15–1.24 | 1.58 | 1.51–1.66 |
| 2 | 1.35 | 1.29–1.42 | 2.13 | 2.01–2.27 |
| 3 or more | 1.48 | 1.37–1.60 | 2.69 | 2.46–2.93 |
| Treated chronic conditions | p < 0.0001 | p < 0.0001 | ||
| 0 | 1.00 | 1.00 | ||
| 1 | 1.22 | 1.18–1.27 | 1.47 | 1.40–1.54 |
| 2 | 1.38 | 1.31–1.45 | 1.89 | 1.77–2.01 |
| 3 or more | 1.57 | 1.45–1.69 | 2.48 | 2.27–2.71 |
| Limited physical functioning | p < 0.0001 | p < 0.0001 | ||
| None | 1.00 | 1.00 | ||
| Minor | 1.36 | 1.30–1.41 | 2.10 | 1.99–2.21 |
| Moderate | 1.58 | 1.51–1.65 | 3.77 | 3.56–4.00 |
| Severe | 1.61 | 1.52–1.70 | 5.31 | 4.96–5.68 |
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| Individual-level adjustment | No | Yes | Yes | Yes | Yes |
| Prevalence ratios (95% CrI) | |||||
| Constant | 0.99 (0.98–1.00) | 1.00 (0.98–1.01) | 1.03 (1.00–1.06) | 1.01 (0.99–1.04) | 1.07 (1.02–1.11) |
| Walkability | |||||
| Low | – | – | 1.00 | – | 1.00 |
| Low-medium | – | – | 0.98 (0.95–1.01) | – | 0.98 (0.95–1.01) |
| Medium-high | – | – | 0.96 (0.92–1.00) | – | 0.94 (0.91–0.98) |
| High | – | – | 0.91 (0.87–0.97) | – | 0.90 (0.86–0.94) |
| Socioeconomic disadvantage | |||||
| Q1—Most | – | – | – | 1.00 | 1.00 |
| Q2 | – | – | – | 1.01 (0.97–1.05) | 1.01 (0.97–1.04) |
| Q3—Middling | – | – | – | 0.99 (0.95–1.03) | 0.99 (0.95–1.03) |
| Q4 | – | – | – | 0.97 (0.93–1.01) | 0.97 (0.93–1.00) |
| Q5—Least | – | – | – | 0.94 (0.90–0.99) | 0.93 (0.89–0.97) |
| Model diagnostics | |||||
| pD | 55.73 | 37.48 | 33.64 | 35.05 | 27.01 |
| DIC | 1832.77 | 1787.67 | 1787.12 | 1787.85 | 1782.70 |
| Spatial fraction | 0.965 | 0.932 | 0.882 | 0.900 | 0.673 |
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| Individual-level adjustment | No | Yes | Yes | Yes | Yes |
| Prevalence ratios (95% CrI) | |||||
| Constant | 0.95 (0.93–0.97) | 0.96 (0.95–0.98) | 1.02 (0.97–1.08) | 1.01 (0.96–1.05) | 1.10 (1.02–1.17) |
| Walkability | |||||
| Low | – | – | 1.00 | – | 1.00 |
| Low-medium | – | – | 0.97 (0.91–1.02) | – | 0.96 (0.91–1.01) |
| Medium-high | – | – | 0.92 (0.85–0.99) | – | 0.89 (0.83–0.96) |
| High | – | – | 0.89 (0.80–0.99) | – | 0.85 (0.78–0.94) |
| Socioeconomic disadvantage | |||||
| Q1—Most | – | – | – | 1.00 | 1.00 |
| Q2 | – | – | – | 1.03 (0.98–1.09) | 1.02 (0.97–1.08) |
| Q3—Middling | – | – | – | 0.97 (0.92–1.03) | 0.97 (0.91–1.03) |
| Q4 | – | – | – | 0.91 (0.85–0.97) | 0.90 (0.85–0.96) |
| Q5—Least | – | – | – | 0.88 (0.82–0.95) | 0.85 (0.79–0.92) |
| Model diagnostics | |||||
| pD | 128.60 | 72.36 | 70.99 | 63.02 | 56.79 |
| DIC | 1794.88 | 1711.26 | 1712.90 | 1705.26 | 1703.00 |
| Spatial fraction | 0.992 | 0.985 | 0.981 | 0.978 | 0.961 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mayne, D.J.; Morgan, G.G.; Jalaludin, B.B.; Bauman, A.E. Area-Level Walkability and the Geographic Distribution of High Body Mass in Sydney, Australia: A Spatial Analysis Using the 45 and Up Study. Int. J. Environ. Res. Public Health 2019, 16, 664. https://doi.org/10.3390/ijerph16040664
Mayne DJ, Morgan GG, Jalaludin BB, Bauman AE. Area-Level Walkability and the Geographic Distribution of High Body Mass in Sydney, Australia: A Spatial Analysis Using the 45 and Up Study. International Journal of Environmental Research and Public Health. 2019; 16(4):664. https://doi.org/10.3390/ijerph16040664
Chicago/Turabian StyleMayne, Darren J., Geoffrey G. Morgan, Bin B. Jalaludin, and Adrian E. Bauman. 2019. "Area-Level Walkability and the Geographic Distribution of High Body Mass in Sydney, Australia: A Spatial Analysis Using the 45 and Up Study" International Journal of Environmental Research and Public Health 16, no. 4: 664. https://doi.org/10.3390/ijerph16040664
APA StyleMayne, D. J., Morgan, G. G., Jalaludin, B. B., & Bauman, A. E. (2019). Area-Level Walkability and the Geographic Distribution of High Body Mass in Sydney, Australia: A Spatial Analysis Using the 45 and Up Study. International Journal of Environmental Research and Public Health, 16(4), 664. https://doi.org/10.3390/ijerph16040664