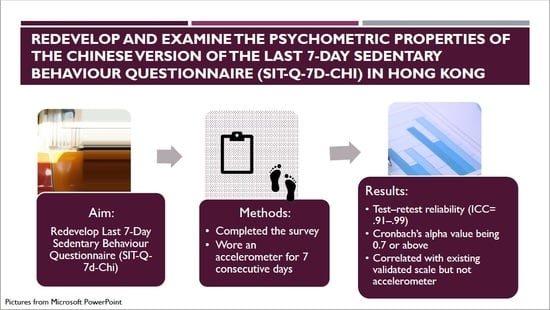
Redevelopment and Examination of the Psychometric Properties of the Chinese Version of the Last 7-Day Sedentary Behaviour Questionnaire (SIT-Q-7d-Chi) in Hong Kong Older Adults
Abstract
:1. Introduction
1.1. Hong Kong Aging Population and the Phenomenon of Physical Activity
1.2. The Relationship between Sedentary Behavior and Physical Health
1.3. Sedentary Behavior Measurements
1.4. The Last 7-Day Sedentary Behaviour Questionnaire (SIT-Q-7d)
1.5. Purpose of Study
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.2.1. Study 1: Reliability Test
2.2.2. Study 2: Validity Test
2.3. Measures
2.3.1. Subjective Sedentary Behaviour Measure
Chinese Version of the Last 7-Day Sedentary Behaviour Questionnaire (SIT-Q-7d-Chi)
Sedentary Behaviour Questionnaire for Older Adults
2.3.2. Objective Sedentary Behaviour Measure
2.4. Statistical Analysis
3. Results
3.1. Study 1: Reliability
3.2. Study 2: Validity
4. Discussion
4.1. Reliability
4.2. Validity
4.3. Strengths and Limitations
4.4. Implications for Future Practice
- The SIT-Q-7d-Chi is a specific and reliable sedentary behaviour scale that measures Chinese older adults’ sedentary behaviour in different domains.
- The field of nursing older adults is given an alternative viewpoint to investigate and examine older adults’ daily activities and habits, thus enabling better day-care and health services for older adults
- The redevelopment of the scale also provides Chinese older adults a self-awareness of the high level of sedentary behaviour, as well as the importance of physical activity during daily practice.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Census and Statistics Department, HKSAR. Hong Kong Population Projections for 2017 to 2066. 2017. Available online: https://www.statistics.gov.hk/pub/B1120015072017XXXXB0100.pdf (accessed on 5 December 2019).
- Census and Statistics Department, HKSAR. Healthy Exercise for All Campaign–Physical Fitness Test for the Community. 2013. Available online: https://www.statistics.gov.hk/pub/B71302FA2013XXXXB0100.pdf (accessed on 5 December 2019).
- Department of Health, HKSAR. Behavioral Risk Factor Survey. 2011. Available online: https://www.chp.gov.hk/files/pdf/brfs_2010apr_en.pdf (accessed on 5 December 2019).
- Kasović, M.; Štefan, L.; Zvonař, M. Domain-Specific and Total Sedentary Behavior Associated with Gait Velocity in Older Adults: The Mediating Role of Physical Fitness. Int. J. Environ. Res. Public Health 2020, 17, 593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silva, F.M.; Petrica, J.; Serrano, J.; Paulo, R.; Ramalho, A.; Lucas, D.; Ferreira, J.P.; Duarte-Mendes, P. The sedentary time and physical activity levels on physical fitness in the elderly: A comparative cross sectional study. Int. J. Environ. Res. Public Health 2019, 16, 3697. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Noncommunicable Diseases and Their Risk Factors. 2010. Available online: https://www.who.int/ncds/prevention/physical-activity/introduction/en/ (accessed on 5 December 2019).
- González, K.; Fuentes, J.; Márquez, J.L. Physical Inactivity, Sedentary Behavior and Chronic Diseases. Korean J. Fam. Med. 2017, 38, 111–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Warren, T.Y.; Barry, V.; Hooker, S.P.; Sui, X.; Church, T.S.; Blair, S.N. Sedentary Behaviors Increase Risk of Cardiovascular Disease Mortality in Men. Med. Sci. Sports Exerc. 2010, 42, 879–885. [Google Scholar] [CrossRef] [Green Version]
- Byun, W.; Dowda, M.; Pate, R.R. Associations between screen-based sedentary behavior and cardiovascular disease risk factors in Korean youth. J. Korean Med. Sci. 2012, 27, 388–394. [Google Scholar] [CrossRef] [Green Version]
- Copeland, J.L.; Ashe, M.C.; Biddle, S.J.; Brown, W.J.; Buman, M.P.; Chastin, S.; Gardiner, P.A.; Inoue, S.; Jefferis, B.J.; Oka, K.; et al. Sedentary time in older adults: A critical review of measurement, associations with health, and interventions. Br. J. Sports Med. 2017, 51, 1539. [Google Scholar] [CrossRef] [Green Version]
- Dogra, S.; Stathokostas, L. Sedentary behaviour and physical activity are independent predictors of successful aging in middle-aged and older adults. J. Aging Phys. Act. 2012, 2012, S250–S251. [Google Scholar]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1094. [Google Scholar] [CrossRef] [Green Version]
- van der Ploeg, H.P.; Hillsdon, M. Is sedentary behaviour just physical inactivity by another name? Int. J. Behav. Nutr. Phys. Act. 2017, 14, 1–8. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.; Altenburg, T.M.; Chinapaw, M.J. Sedentary behavior research network (SBRN)–terminology consensus project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Department of Health, HKSAR. Promoting Health in Hong Kong. 2018. Available online: https://www.dh.gov.hk/english/pub_rec/pub_rec_ar/pdf/ncd/ENG%20whole%20DOC%2016-10-08.pdf (accessed on 5 December 2019).
- Yu, H.; Schwingel, A. Associations between Sedentary Behavior, Physical Activity, and Out-of-Pocket Health Care Expenditure: Evidence from Chinese Older Adults. J. Aging Phys. Act. 2019, 27, 108–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gorman, E.; Hanson, H.M.; Yang, P.H.; Khan, K.M.; Liu-Ambrose, T.; Ashe, M.C. Accelerometry analysis of physical activity and sedentary behavior in older adults: A systematic review and data analysis. Eur. Rev. Aging Phys. Act. 2013, 11, 35–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sallis, J.F.; Saelens, B.E. Assessment of Physical Activity by Self-Report: Status, Limitations, and Future Directions. Res. Q. Exerc. Sport 2000, 71 (Suppl. S2), 1–14. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.; Rowe, D.A. Issues and challenges in sedentary behavior measurement. Meas. Phys. Educ. Exerc. Sci. 2015, 19, 105–115. [Google Scholar] [CrossRef] [Green Version]
- Marshall, A.L.; Miller, Y.D.; Burton, N.W.; Brown, W.J. Measuring total and domain-specific sitting: A study of reliability and validity. Med. Sci. Sports Exerc. 2010, 42, 1094–1102. [Google Scholar] [CrossRef]
- Clark, B.K.; Healy, G.N.; Winkler, E.A.; Gardiner, P.A.; Sugiyama, T.; Dunstan, D.W.; Matthews, C.E.; Owen, N. Relationship of television time with accelerometer-derived sedentary time: NHANES. Med. Sci. Sports Exerc. 2011, 43, 822. [Google Scholar] [CrossRef] [Green Version]
- Visser, M.; Koster, A. Development of a questionnaire to assess sedentary time in older persons–a comparative study using accelerometry. BMC Geriatr. 2013, 13, 80. [Google Scholar] [CrossRef]
- Van Cauwenberg, J.; Van Holle, V.; De Bourdeaudhuij, I.; Owen, N.; Deforche, B. Older adults’ reporting of specific sedentary behaviors: Validity and reliability. BMC Public Health 2014, 14, 734. [Google Scholar] [CrossRef] [Green Version]
- Felez-Nobrega, M.; Hillman, C.H.; Dowd, K.P.; Cirera, E.; Puig-Ribera, A. ActivPAL™ determined sedentary behaviour, physical activity and academic achievement in college students. J. Sports Sci. 2018, 36, 2311–2316. [Google Scholar] [CrossRef]
- Wijndaele, K.; DE Bourdeaudhuij, I.; Godino, J.G.; Lynch, B.; Griffin, S.J.; Westgate, K.; Brage, S. Reliability and Validity of a Domain-Specific Last 7-d Sedentary Time Questionnaire. Med. Sci. Sports Exerc. 2014, 46, 1248–1260. [Google Scholar] [CrossRef] [Green Version]
- Bao, R.; Chen, S.-T.; Wang, Y.; Xu, J.; Wang, L.; Zou, L.; Cai, Y. Sedentary Behavior Research in the Chinese Population: A Systematic Scoping Review. Int. J. Environ. Res. Public Health 2020, 17, 3576. [Google Scholar] [CrossRef] [PubMed]
- Chu, L.; Pei, C.; Ho, M.; Chan, P. Validation of the abbreviated mental test (Hong Kong version) in the elderly medical patient. Hong Kong Med. J. 1995, 1, 207–211. [Google Scholar]
- Prince, S.A.; Cardilli, L.; Reed, J.L.; Saunders, T.J.; Kite, C.; Douillette, K.; Fournier, K.; Buckley, J.P. A comparison of self-reported and device measured sedentary behaviour in adults: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 31. [Google Scholar] [CrossRef] [PubMed]
- Hambleton, R.K.; Kanjee, A. Increasing the validity of cross-cultural assessments: Use of improved methods for test adaptations. Eur. J. Psychol. Assess. 1995, 11, 147–157. [Google Scholar] [CrossRef]
- Ku, P.-W.; Sun, W.-J.; Chen, L.-J. Development of the Sedentary Behavior Questionnaire for the Elderly. Sports Exerc. Res. 2016, 18, 41–55. [Google Scholar] [CrossRef]
- Choi, L.; Ward, S.; Schnelle, J.F.; Buchowski, M. Assessment of Wear/Nonwear Time Classification Algorithms for Triaxial Accelerometer. Med. Sci. Sports Exerc. 2012, 44, 2009–2016. [Google Scholar] [CrossRef] [Green Version]
- Heesch, K.C.; Hill, R.L.; Aguilar-Farias, N.; Van Uffelen, J.G.Z.; Pavey, T. Validity of objective methods for measuring sedentary behaviour in older adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 119. [Google Scholar] [CrossRef]
- Aguilar-Farias, N.; Brown, W.J.; Peeters, G. ActiGraph GT3X+ cut-points for identifying sedentary behaviour in older adults in free-living environments. J. Sci. Med. Sport 2013, 17, 293–299. [Google Scholar] [CrossRef]
- Nunnally, J.C. Psychometric Theory 3E; Tata McGraw-Hill Education: New York, NY, USA, 1994. [Google Scholar]
- Field, A. Discovering Statistics Using IBM SPSS Statistics; Sage: London, UK, 2013. [Google Scholar]
- Biddle, G.J.H.; Edwardson, C.L.; Rowlands, A.V.; Davies, M.; Bodicoat, D.H.; Hardeman, W.; Eborall, H.; Sutton, S.; Griffin, S.; Khunti, K.; et al. Differences in objectively measured physical activity and sedentary behaviour between white Europeans and south Asians recruited from primary care: Cross-sectional analysis of the PROPELS trial. BMC Public Health 2019, 19, 95. [Google Scholar] [CrossRef] [Green Version]
- McGoldrick, M.; Giordano, J.; Garcia-Preto, N. Ethnicity and Family Therapy; Guilford Press: New York, NY, USA, 2005. [Google Scholar]
- Cullinane, S.; Cullinane, K. Car dependence in a public transport dominated city: Evidence from Hong Kong. Transp. Res. Part D: Transp. Environ. 2003, 8, 129–138. [Google Scholar] [CrossRef]
- Zhang, M.; Chen, X.; Wang, Z.; Wang, L.; Jiang, Y. Leisure-time physical exercise and sedentary behavior among Chinese elderly, in 2010. Zhonghua Liu Xing Bing Xue Za Zhi 2014, 35, 242–245. [Google Scholar] [PubMed]
- Ng, L.; Koh, Y.; Tan, N. Physical activity and sedentary behaviour of ambulatory older adults in a developed Asian community: A cross-sectional study. Singap. Med. J. 2020, 61, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Colley, R.C.; Garriguet, D.; Janssen, I.; Craig, C.L.; Clarke, J.; Tremblay, M.S. Physical activity of Canadian adults: Accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 2011, 22, 7. [Google Scholar] [PubMed]
- Arnardottir, N.Y.; Koster, A.; Van Domelen, D.R.; Brychta, R.J.; Caserotti, P.; Eiriksdottir, G.; Sverrisdottir, J.E.; Launer, L.J.; Gudnason, V.; Johannsson, E.; et al. Objective measurements of daily physical activity patterns and sedentary behaviour in older adults: Age, Gene/Environment Susceptibility-Reykjavik Study. Age Ageing 2013, 42, 222–229. [Google Scholar] [CrossRef] [Green Version]
- Van Der Berg, J.D.; Bosma, H.; Caserotti, P.; Eiriksdottir, G.; Arnardottir, N.Y.; Martin, K.R.; Brychta, R.J.; Chen, K.Y.; Sveinsson, T.; Johannsson, E.; et al. Midlife determinants associated with sedentary behavior in old age. Med. Sci. Sports Exerc. 2014, 46, 1359. [Google Scholar] [CrossRef] [Green Version]
- Matthews, C.E.; Chen, K.Y.; Freedson, P.S.; Buchowski, M.S.; Beech, B.M.; Pate, R.R.; Troiano, R.P. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am. J. Epidemiol. 2008, 167, 875–881. [Google Scholar] [CrossRef] [Green Version]
- Bankoski, A.; Harris, T.B.; McClain, J.J.; Brychta, R.J.; Caserotti, P.; Chen, K.Y.; Berrigan, D.; Troiano, R.P.; Koster, A. Sedentary activity associated with metabolic syndrome independent of physical activity. Diabetes Care 2011, 34, 497–503. [Google Scholar] [CrossRef] [Green Version]
- Koster, A.; Caserotti, P.; Patel, K.V.; Matthews, C.E.; Berrigan, D.; Van Domelen, D.R.; Brychta, R.J.; Chen, K.Y.; Harris, T.B. Association of sedentary time with mortality independent of moderate to vigorous physical activity. PLoS ONE 2012, 7, e37696. [Google Scholar] [CrossRef]
- Mathie, M.; Basilakis, J.; Celler, B. A system for monitoring posture and physical activity using accelerometers. In Proceedings of the 2001 Conference Proceedings of the 23rd Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Istanbul, Turkey, 25–28 October 2001; pp. 3654–3657. [Google Scholar]
- Westerterp, K.R. Physical activity assessment with accelerometers. Int. J. Obes. 1999, 23, S45–S49. [Google Scholar] [CrossRef] [Green Version]
- Gong, W.-J.; Fong, D.Y.-T.; Wang, M.-P.; Lam, T.-H.; Chung, T.W.-H.; Ho, S.-Y. Increasing socioeconomic disparities in sedentary behaviors in Chinese children. BMC Public Health 2019, 19, 754. [Google Scholar] [CrossRef]
- Lyden, K.; Keadle, S.K.; Staudenmayer, J.; Freedson, P.S. The activPAL™ accurately classifies activity intensity categories in healthy adults. Med. Sci. Sports Exerc. 2017, 49, 1022. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Study 1 (N = 84) | Study 2 (N = 38) | |
|---|---|---|
| % | % | |
| Age | ||
| 60–64 | 0 | 2.6 |
| 65–69 | 39.3 | 15.8 |
| 70–74 | 23.8 | 7.9 |
| 75–80 | 21.4 | 31.6 |
| 81–84 | 6 | 18.4 |
| 85–90 | 9.5 | 18.4 |
| 90 or above | 0 | 2.6 |
| Gender | ||
| Male | 38.1 | 18.4 |
| Female | 61.9 | 81.6 |
| Education Level | ||
| Primary or below | - | 78.9 |
| Secondary school | - | 18.4 |
| Tertiary education or above | - | 0 |
| Housing type | ||
| Public Housing | 40.5 | 44.7 |
| Home Ownership Scheme | 26.2 | 5.3 |
| Private Housing | 16.7 | 42.1 |
| Others | 16.7 | 5.3 |
| Cronbach’s Alpha Value | ICC | 95%CI | |
|---|---|---|---|
| Time 1 | Time 2 | ||
| 0.822 | 0.812 | 0.986 | 0.979–0.991 |
| 0.866 | 0.851 | 0.987 | 0.981–0.992 |
| 0.584 | 0.593 | 0.914 | 0.870–0.943 |
| 0.604 | 0.619 | 1 | 1.0–1.0 |
| 0.757 | 0.761 | 0.984 | 0.975–0.990 |
| 0.698 | 0.730 | 0.997 | 0.995–0.998 |
| N = 38 | Mean ± Std. Deviation |
|---|---|
| Total Sedentary Behaviour (min·d−7) | 3345.58 ± 1126.32 |
| Average 7 Days (min·d−1) | 477.94 ± 160.90 |
| N = 38 | Mean ± Std. Deviation |
|---|---|
| Sitting Time during watching TV | 163.91 ± 110.73 |
| Sitting Time during using computer | 49.87 ± 74.35 |
| Sitting Time during reading | 22.21 ± 41.46 |
| Sitting Time during chatting | 21.13 ± 39.74 |
| Sitting Time during transportation | 17.35 ± 41.73 |
| Sitting Time during meal | 107.70 ± 52.20 |
| Sitting Time during hobbies | 32.54 ± 60.91 |
| Sitting Time during nap | 49.61 ± 96.72 |
| Sitting Time during work or volunteer | 28.87 ± 62.44 |
| Sitting Time during other activities | 4.17 ± 9.79 |
| Total Sitting Time | 518.99 ± 249.95 |
| N = 38 | Mean ± Std. Deviation |
|---|---|
| Sleeping time | |
| Weekday (min·d−1) | 514.08 ± 77.97 |
| Weekend Day (min·d−1) | 509.13 ± 77.81 |
| Average 7 Day (min·d−1) | 512.67 ± 77.64 |
| Sitting Time during Meals | |
| Weekday (mins·d−1) | 87.38 ± 38.59 |
| Weekend Day (min·d−1) | 86.97 ± 37.88 |
| Average 7 Day (min·d−1) | 87.27 ± 38.29 |
| Sitting Time during transportation (*7) (min·d−1) | 287.83 ± 399.68 |
| Sitting Time during transportation (*day) (min·d−1) | 65.78 ± 172.97 |
| Sitting Time during work (*7) (min·d−1) | 356.17 ± 529.85 |
| Sitting Time during work (*day) (min·d−1) | 224.72 ± 465.70 |
| Screen-based Leisure Sitting Time | |
| Weekday (min·d−1) | 227.62 ± 117.73 |
| Weekend Day (min·d−1) | 223.67 ± 117.32 |
| Average 7 Day (min·d−1) | 226.49 ± 116.66 |
| Other Sitting Time | |
| Weekday (min·d−1) | 152.32 ± 148.51 |
| Weekend Day (min·d−1) | 173.57 ± 165.99 |
| Average 7 Day (min·d−1) | 158.39 ± 149.59 |
| Subscale | A | B | C | D | E | F | G | H |
|---|---|---|---|---|---|---|---|---|
| A | 1 | |||||||
| B | 0.121 | 1 | ||||||
| C | 0.153 | 0.944 ** | 1 | |||||
| D | 0.166 | 0.249 | 0.291 | 1 | ||||
| E | 0.210 | 0.476 ** | 0.501 ** | 0.065 | 1 | |||
| F | 0.411 * | 0.454 ** | 0.419 ** | 0.537 ** | 0.581 ** | 1 | ||
| G | −0.003 | 0.695 ** | 0.693 ** | 0.467 ** | 0.573 ** | 0.483 ** | 1 | |
| H | −0.066 | −0.148 | −0.063 | −0.141 | −0.180 | −0.271 | −0.144 | 1 |
| Author | Average Sedentary Time (min/per day) | Cut-off Point |
|---|---|---|
| Colley et al., 2011 [41] | 600 | <100 counts/min |
| Arnardottir et al., 2013 [42] | 624 | <100 counts/min |
| Van der Berg et al., 2014 [43] | 618 | <100 counts/min |
| Matthews et al., 2008 [44] | 528 | <100 counts/min |
| Clark et al., 2011 [21] | 552 | <100 counts/min |
| Bankoski et al., 2012 [45] | 570 | <100 counts/min |
| Koster et al., 2012 [46] | 540 | <100 counts/min |
| Current paper | 477.9 | <200 counts/min |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leung, K.M.; Wong, M.Y.C. Redevelopment and Examination of the Psychometric Properties of the Chinese Version of the Last 7-Day Sedentary Behaviour Questionnaire (SIT-Q-7d-Chi) in Hong Kong Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 5958. https://doi.org/10.3390/ijerph19105958
Leung KM, Wong MYC. Redevelopment and Examination of the Psychometric Properties of the Chinese Version of the Last 7-Day Sedentary Behaviour Questionnaire (SIT-Q-7d-Chi) in Hong Kong Older Adults. International Journal of Environmental Research and Public Health. 2022; 19(10):5958. https://doi.org/10.3390/ijerph19105958
Chicago/Turabian StyleLeung, Ka Man, and Ming Yu Claudia Wong. 2022. "Redevelopment and Examination of the Psychometric Properties of the Chinese Version of the Last 7-Day Sedentary Behaviour Questionnaire (SIT-Q-7d-Chi) in Hong Kong Older Adults" International Journal of Environmental Research and Public Health 19, no. 10: 5958. https://doi.org/10.3390/ijerph19105958
APA StyleLeung, K. M., & Wong, M. Y. C. (2022). Redevelopment and Examination of the Psychometric Properties of the Chinese Version of the Last 7-Day Sedentary Behaviour Questionnaire (SIT-Q-7d-Chi) in Hong Kong Older Adults. International Journal of Environmental Research and Public Health, 19(10), 5958. https://doi.org/10.3390/ijerph19105958