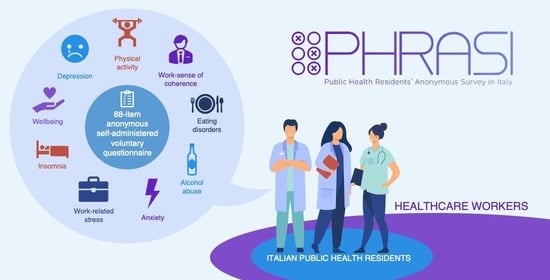
Public Health Residents’ Anonymous Survey in Italy (PHRASI): Study Protocol for a Cross-Sectional Study for a Multidimensional Assessment of Mental Health and Its Determinants
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design of the Survey
2.2. Eligibility
2.3. Data Collection
2.4. Questionnaire
2.5. Sample Size
2.6. Ethical Considerations, Patient Information and Written Informed Consent
3. Results
4. Discussion
4.1. Practical Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

References
- World Health Organization (WHO). Mental Health: Strengthening Our Response. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response (accessed on 29 November 2022).
- Lund, C.; Brooke-Sumner, C.; Baingana, F.; Baron, E.C.; Breuer, E.; Chandra, P.; Haushofer, J.; Herrman, H.; Jordans, M.; Kieling, C.; et al. Social Determinants of Mental Disorders and the Sustainable Development Goals: A Systematic Review of Reviews. Lancet Psychiatry 2018, 5, 357–369. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.; Saxena, S.; Lund, C.; Thornicroft, G.; Baingana, F.; Bolton, P.; Chisholm, D.; Collins, P.Y.; Cooper, J.L.; Eaton, J.; et al. The Lancet Commission on Global Mental Health and Sustainable Development. Lancet 2018, 392, 1553–1598. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- GBD 2019 Mental Disorders Collaborators. Global, Regional, and National Burden of 12 Mental Disorders in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Longo, R.; Bessone, M.; Bartolomei, G.; Brancato, S.; Grandi, B.; Gyppaz, D.; Zazzara, M.B. (Eds.) I Determinanti Sociali Della Salute Mentale; Centro Regionale di Documentazione per la Promozione della Salute: Grugliasco, Italy, 2017. [Google Scholar]
- Mathieson, A.; Koller, T.; Weltgesundheitsorganisation (Eds.) Social Cohesion for Mental Well-Being among Adolescents: Was Then Held on 5–6 October 2007 in Viareggio, Tuscany Region, Italy; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2008; ISBN 978-92-890-4288-8. [Google Scholar]
- Gigantesco, A.; Ferrante, G.; Baldissera, S.; Masocco, M. Depressive Symptoms and Behavior-Related Risk Factors, Italian Population-Based Surveillance System, 2013. Prev. Chronic Dis. 2015, 12, E183. [Google Scholar] [CrossRef] [Green Version]
- Santomauro, D.F.; Mantilla Herrera, A.M.; Shadid, J.; Zheng, P.; Ashbaugh, C.; Pigott, D.M.; Abbafati, C.; Adolph, C.; Amlag, J.O.; Aravkin, A.Y.; et al. Global Prevalence and Burden of Depressive and Anxiety Disorders in 204 Countries and Territories in 2020 Due to the COVID-19 Pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef] [PubMed]
- Bacaro, V.; Chiabudini, M.; Buonanno, C.; De Bartolo, P.; Riemann, D.; Mancini, F.; Baglioni, C. Insomnia in the Italian Population During Covid-19 Outbreak: A Snapshot on One Major Risk Factor for Depression and Anxiety. Front. Psychiatry 2020, 11, 579107. [Google Scholar] [CrossRef] [PubMed]
- Killgore, W.D.S.; Cloonan, S.A.; Taylor, E.C.; Lucas, D.A.; Dailey, N.S. Alcohol Dependence during COVID-19 Lockdowns. Psychiatry Res. 2021, 296, 113676. [Google Scholar] [CrossRef]
- Baenas, I.; Etxandi, M.; Munguía, L.; Granero, R.; Mestre-Bach, G.; Sánchez, I.; Ortega, E.; Andreu, A.; Moize, V.L.; Fernández-Real, J.-M.; et al. Impact of COVID-19 Lockdown in Eating Disorders: A Multicentre Collaborative International Study. Nutrients 2022, 14, 100. [Google Scholar] [CrossRef]
- Salari, N.; Khazaie, H.; Hosseinian-Far, A.; Khaledi-Paveh, B.; Kazeminia, M.; Mohammadi, M.; Shohaimi, S.; Daneshkhah, A.; Eskandari, S. The Prevalence of Stress, Anxiety and Depression within Front-Line Healthcare Workers Caring for COVID-19 Patients: A Systematic Review and Meta-Regression. Hum. Resour. Health 2020, 18, 100. [Google Scholar] [CrossRef]
- Policy Brief: COVID-19 and the Need for Action on Mental Health; United Nation: New York, NY, USA, 2020.
- Unicef. The Impact of COVID-19 on the Mental Health of Adolescents and Youth. Available online: https://www.unicef.org/lac/en/impact-covid-19-mental-health-adolescents-and-youth (accessed on 30 November 2022).
- Deeker, W. The Covid Generation: The Effects of the Pandemic on Youth Mental Health | Research and Innovation. Available online: https://ec.europa.eu/research-and-innovation/en/horizon-magazine/covid-generation-effects-pandemic-youth-mental-health (accessed on 30 November 2022).
- Van Ness, M. COVID-19 and Women’s Mental Health: The Impact on Wellbeing, Disparities, and Future Implications. Available online: https://www.baylor.edu/communityconnection/news.php?action=story&story=222809 (accessed on 30 November 2022).
- da Silva Neto, R.M.; Benjamim, C.J.R.; de Medeiros Carvalho, P.M.; Neto, M.L.R. Psychological Effects Caused by the COVID-19 Pandemic in Health Professionals: A Systematic Review with Meta-Analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 104, 110062. [Google Scholar] [CrossRef] [PubMed]
- Salazar de Pablo, G.; Vaquerizo-Serrano, J.; Catalan, A.; Arango, C.; Moreno, C.; Ferre, F.; Shin, J.I.; Sullivan, S.; Brondino, N.; Solmi, M.; et al. Impact of Coronavirus Syndromes on Physical and Mental Health of Health Care Workers: Systematic Review and Meta-Analysis. J. Affect. Disord. 2020, 275, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Lasalvia, A.; Bonetto, C.; Porru, S.; Carta, A.; Tardivo, S.; Bovo, C.; Ruggeri, M.; Amaddeo, F. Psychological Impact of COVID-19 Pandemic on Healthcare Workers in a Highly Burdened Area of North-East Italy. Epidemiol. Psychiatr. Sci. 2021, 30, e1. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E.J.; Sherbourne, C.D. The MOS 36-Item Short-Form Health Survey (SF-36). I. Conceptual Framework and Item Selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Cislaghi, B.; Cislaghi, C. Self-Rated Health as a Valid Indicator for Health-Equity Analyses: Evidence from the Italian Health Interview Survey. BMC Public Health 2019, 19, 533. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Wellbeing Measures in Primary Health Care/the DEPCARE Project; WHO Regional Office for Europe: Stockholm, Sweden, 1998; p. 45. [Google Scholar]
- Nicolucci, A.; Giorgino, R.; Cucinotta, D.; Zoppini, G.; Muggeo, M.; Squatrito, S.; Corsi, A.; Lostia, S.; Pappalardo, L.; Benaduce, E.; et al. Validation of the Italian Version of the WHO-Well-Being Questionnaire (WHO-WBQ) and the WHO-Diabetes Treatment Satisfaction Questionnaire (WHO-DTSQ). Diabetes Nutr. Metab. 2004, 17, 235–243. [Google Scholar]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [Green Version]
- Minetto, M.A.; Motta, G.; Gorji, N.E.; Lucini, D.; Biolo, G.; Pigozzi, F.; Portincasa, P.; Maffiuletti, N.A. Reproducibility and Validity of the Italian Version of the International Physical Activity Questionnaire in Obese and Diabetic Patients. J. Endocrinol. Investig. 2018, 41, 343–349. [Google Scholar] [CrossRef]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; de la Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption–II. Addict. Abingdon Engl. 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Vogt, K.; Jenny, G.J.; Bauer, G.F. Comprehensibility, Manageability and Meaningfulness at Work: Construct Validity of a Scale Measuring Work-Related Sense of Coherence: Original Research. SA J. Ind. Psychol. 2013, 39, 1–8. [Google Scholar] [CrossRef]
- De Sio, S.; Cedrone, F.; Perri, R.; Nieto, H.A.; Greco, E.; Buomprisco, G.; Stansfeld, S. Work-Related Stress Questionnaire (WRSQ): A New Tool to Assess Psychosocial Risks at Workplaces. Clin. Ter. 2020, 171, e316–e320. [Google Scholar] [CrossRef]
- Morgan, J.F.; Reid, F.; Lacey, J.H. The SCOFF Questionnaire: A New Screening Tool for Eating Disorders. West. J. Med. 2000, 172, 164–165. [Google Scholar] [CrossRef] [Green Version]
- Pannocchia, L.; Di Fiorino, M.; Giannini, M.; Vanderlinden, J. A Psychometric Exploration of an Italian Translation of the SCOFF Questionnaire. Eur. Eat. Disord. Rev. 2011, 19, 371–373. [Google Scholar] [CrossRef] [PubMed]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an Outcome Measure for Insomnia Research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Castronovo, V.; Galbiati, A.; Marelli, S.; Brombin, C.; Cugnata, F.; Giarolli, L.; Anelli, M.M.; Rinaldi, F.; Ferini-Strambi, L. Validation Study of the Italian Version of the Insomnia Severity Index (ISI). Neurol. Sci. 2016, 37, 1517–1524. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Mazzotti, E.; Fassone, G.; Picardi, A.; Sagoni, E.; Ramieri, L.; Lega, I.; Camaioni, D.; Abeni, D.; Pasquini, P. II Patient Health Questionnaire (PHQ) per Lo Screening Dei Disturbi Psichiatrici. Uno Studio Validazione Nei Confronti Della Intervista Clin. Strutt. Il DSM-IV Asse SCID-I 2003, 9, 235–242. [Google Scholar]
- Mata, D.A.; Ramos, M.A.; Bansal, N.; Khan, R.; Guille, C.; Di Angelantonio, E.; Sen, S. Prevalence of Depression and Depressive Symptoms Among Resident Physicians: A Systematic Review and Meta-Analysis. JAMA 2015, 314, 2373–2383. [Google Scholar] [CrossRef] [Green Version]
- Charan, J.; Biswas, T. How to Calculate Sample Size for Different Study Designs in Medical Research? Indian J. Psychol. Med. 2013, 35, 121–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pasqualucci, P.L.; Damaso, L.L.M.; Danila, A.H.; Fatori, D.; Lotufo Neto, F.; Koch, V.H.K. Prevalence and Correlates of Depression, Anxiety, and Stress in Medical Residents of a Brazilian Academic Health System. BMC Med. Educ. 2019, 19, 193. [Google Scholar] [CrossRef]
- AlJahwari, B.; AlKamli, A.; Al-Huseini, S.; Chan, M.F.; AlMahroqi, B.; Al Saadoon, M.; Ambusaidi, A.; Ganesh, A.; Al-Adawi, S. The Prevalence and Factors Associated with Anxiety Symptoms among Resident Physicians in Oman: A Cross-Sectional Study. Middle East Curr. Psychiatry 2022, 29, 47. [Google Scholar] [CrossRef]
- Italia. Decreto Legislativo 30 giugno 2003, n. 196. Codice in materia di protezione dei dati personali. In Supplemento Ordinario Alla “Gazzetta Ufficiale Della Repubblica Italiana”; Ministero della Giustizia—Ufficio pubblicazioni leggi e decreti, Ed.; Serie Generale; Istituto Poligrafico e Zecca dello Stato: Roma, Italy, 2003; Volume 123/L, pp. 11–207. Available online: https://www.gazzettaufficiale.it/atto/serie_generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta=2003-07-29&atto.codiceRedazionale=003G0218 (accessed on 14 January 2023).
- Italia. Decreto Legislativo 10 Agosto 2018 , n. 101. Disposizioni per l’adeguamento Della Normativa Nazionale Alle Disposizioni Del Regolamento (UE) 2016/679 Del Parlamento Europeo e Del Consiglio, Del 27 Aprile 2016, Relativo Alla Protezione Delle Persone Fisiche Con Riguardo al Trattamento Dei Dati Personali, Nonché Alla Libera Circolazione Di Tali Dati e Che Abroga La Direttiva 95/46/CE (Regolamento Generale Sulla Protezione Dei Dati). In Gazzetta Ufficiale Della Repubblica Italiana; Serie Generale; Istituto Poligrafico e Zecca dello Stato: Roma, Italy, 2018; Volume 159, pp. 1–43. Available online: www.gazzettaufficiale.it/eli/id/2018/09/04/18G00129/sg (accessed on 14 January 2023).
- European Union. Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the Protection of Natural Persons with Regard to the Processing of Personal Data and on the Free Movement of Such Data, and Repealing Directive 95/46/EC (General Data Protection Regulation) (Text with EEA Relevance). Off. J. Eur. Union 2016, 59, L119/1–L119/88. [CrossRef]
- Agenzia italiana del farmaco. Determinazione 20 marzo 2008. Linee guida per la classificazione e conduzione degli studi osservazionali sui farmaci. In Gazzetta Ufficiale Della Repubblica Italiana; Ministero della Giustizia—Ufficio pubblicazioni leggi e decreti, Ed.; Serie Generale—Parte Prima; Istituto Poligrafico e Zecca dello Stato: Roma, Italy, 2008; Volume 149, pp. 68–74. Available online: www.gazzettaufficiale.it/eli/id/2008/03/31/08A02109/sg (accessed on 14 January 2023).
- Bush, K.; Kivlahan, D.R.; McDonell, M.B.; Fihn, S.D.; Bradley, K.A. Ambulatory Care Quality Improvement Project (ACQUIP) The AUDIT Alcohol Consumption Questions (AUDIT-C): An Effective Brief Screening Test for Problem Drinking. Arch. Intern. Med. 1998, 158, 1789–1795. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A Systematic Review of the Literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Twenge, J.M.; Gentile, B.; DeWall, C.N.; Ma, D.; Lacefield, K.; Schurtz, D.R. Birth Cohort Increases in Psychopathology among Young Americans, 1938–2007: A Cross-Temporal Meta-Analysis of the MMPI. Clin. Psychol. Rev. 2010, 30, 145–154. [Google Scholar] [CrossRef]
- Hidaka, B.H. Depression as a Disease of Modernity: Explanations for Increasing Prevalence. J. Affect. Disord. 2012, 140, 205–214. [Google Scholar] [CrossRef] [Green Version]
- Rajkumar, R.P. COVID-19 and Mental Health: A Review of the Existing Literature. Asian J. Psychiatry 2020, 52, 102066. [Google Scholar] [CrossRef]
- Sultana, A.; Sharma, R.; Hossain, M.M.; Bhattacharya, S.; Purohit, N. Burnout Among Healthcare Providers During COVID-19 Pandemic: Challenges and Evidence-Based Interventions. Indian J. Med. Ethics. 2020, 5, 1–6. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of Depression, Anxiety, and Insomnia among Healthcare Workers during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Brain. Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Vanhaecht, K.; Seys, D.; Bruyneel, L.; Cox, B.; Kaesemans, G.; Cloet, M.; Van Den Broeck, K.; Cools, O.; De Witte, A.; Lowet, K.; et al. COVID-19 Is Having a Destructive Impact on Health-Care Workers’ Mental Well-Being. Int. J. Qual. Health Care 2021, 33, mzaa158. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Nayar, K.R. COVID 19 and Its Mental Health Consequences. J. Ment. Health 2021, 30, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, C.M.; Flanagan, E.M. Self-Care as a Professional Imperative: Physician Burnout, Depression, and Suicide. Can. J. Anesth. Can. Anesth. 2017, 64, 158–168. [Google Scholar] [CrossRef] [Green Version]
- Gold, K.J.; Andrew, L.B.; Goldman, E.B.; Schwenk, T.L. “I Would Never Want to Have a Mental Health Diagnosis on My Record”: A Survey of Female Physicians on Mental Health Diagnosis, Treatment, and Reporting. Gen. Hosp. Psychiatry 2016, 43, 51–57. [Google Scholar] [CrossRef]
- Schwenk, T.L.; Gorenflo, D.W.; Leja, L.M. A Survey on the Impact of Being Depressed on the Professional Status and Mental Health Care of Physicians. J. Clin. Psychiatry 2008, 69, 617–620. [Google Scholar] [CrossRef] [PubMed]
- Compton, M.T.; Shim, R.S. The Social Determinants of Mental Health. Focus 2015, 13, 419–425. [Google Scholar] [CrossRef] [Green Version]
- Alegría, M.; NeMoyer, A.; Falgàs Bagué, I.; Wang, Y.; Alvarez, K. Social Determinants of Mental Health: Where We Are and Where We Need to Go. Curr. Psychiatry Rep. 2018, 20, 95. [Google Scholar] [CrossRef] [PubMed]
- Stubbs, B.; Vancampfort, D.; Smith, L.; Rosenbaum, S.; Schuch, F.; Firth, J. Physical Activity and Mental Health. Lancet Psychiatry 2018, 5, 873. [Google Scholar] [CrossRef] [Green Version]
- Chekroud, S.R.; Gueorguieva, R.; Zheutlin, A.B.; Paulus, M.; Krumholz, H.M.; Krystal, J.H.; Chekroud, A.M. Association between Physical Exercise and Mental Health in 1·2 million Individuals in the USA between 2011 and 2015: A Cross-Sectional Study. Lancet Psychiatry 2018, 5, 739–746. [Google Scholar] [CrossRef]
- Robinson, L.R.; Holbrook, J.R.; Bitsko, R.H.; Hartwig, S.A.; Kaminski, J.W.; Ghandour, R.M.; Peacock, G.; Heggs, A.; Boyle, C.A. Differences in Health Care, Family, and Community Factors Associated with Mental, Behavioral, and Developmental Disorders Among Children Aged 2–8 Years in Rural and Urban Areas—United States, 2011–2012. Morb. Mortal. Wkly. Rep. Surveill. Summ. Wash. DC 2002 2017, 66, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hwang, W.J.; Jo, H.H. Impact of Mental Health on Wellness in Adult Workers. Front. Public Health 2021, 9, 743344. [Google Scholar] [CrossRef] [PubMed]
- Gunnell, D.; Appleby, L.; Arensman, E.; Hawton, K.; John, A.; Kapur, N.; Khan, M.; O’Connor, R.C.; Pirkis, J.; Appleby, L.; et al. Suicide Risk and Prevention during the COVID-19 Pandemic. Lancet Psychiatry 2020, 7, 468–471. [Google Scholar] [CrossRef] [PubMed]
- Gray, P.; Senabe, S.; Naicker, N.; Kgalamono, S.; Yassi, A.; Spiegel, J.M. Workplace-Based Organizational Interventions Promoting Mental Health and Happiness among Healthcare Workers: A Realist Review. Int. J. Environ. Res. Public. Health 2019, 16, 4396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jorm, A.F.; Korten, A.E.; Jacomb, P.A.; Rodgers, B.; Pollitt, P.; Christensen, H.; Henderson, S. Helpfulness of Interventions for Mental Disorders: Beliefs of Health Professionals Compared with the General Public. Br. J. Psychiatry 1997, 171, 233–237. [Google Scholar] [CrossRef]
- Reja, U.; Manfreda, K.L.; Hlebec, V.; Vehovar, V. Open-Ended vs. Close-Ended Questions in Web Questionnaires. In Developments in Applied Statistics; Ferligoj, A., Mrvar, A., Eds.; FDV: Ljubljana, Slovenia, 2003; Volume 19, pp. 159–177. ISBN 961-235-123-6. [Google Scholar]
- Carlson, M.D.A.; Morrison, R.S. Study Design, Precision, and Validity in Observational Studies. J. Palliat. Med. 2009, 12, 77–82. [Google Scholar] [CrossRef] [Green Version]
- Santos, I.; Tavares, B.; Munhoz, T.; Almeida, L.; Tessele Barreto da Silva, N.; Tams, B.; Patella, A.; Matijasevich, A. Sensitivity and Specificity of the Patient Health Questionnaire-9 (PHQ-9) among Adults from the General Population. Cad. Saúde Pública 2013, 29, 1533–1543. [Google Scholar] [CrossRef]
- Levis, B.; Benedetti, A.; Thombs, B.D. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for Screening to Detect Major Depression: Individual Participant Data Meta-Analysis. BMJ 2019, 365, l1476. [Google Scholar] [CrossRef] [Green Version]
- Costantini, L.; Pasquarella, C.; Odone, A.; Colucci, M.E.; Costanza, A.; Serafini, G.; Aguglia, A.; Belvederi Murri, M.; Brakoulias, V.; Amore, M.; et al. Screening for Depression in Primary Care with Patient Health Questionnaire-9 (PHQ-9): A Systematic Review. J. Affect. Disord. 2021, 279, 473–483. [Google Scholar] [CrossRef]
- Patel, J.S.; Oh, Y.; Rand, K.L.; Wu, W.; Cyders, M.A.; Kroenke, K.; Stewart, J.C. Measurement Invariance of the Patient Health Questionnaire-9 (PHQ-9) Depression Screener in U.S. Adults across Sex, Race/Ethnicity, and Education Level: NHANES 2005–2016. Depress. Anxiety 2019, 36, 813–823. [Google Scholar] [CrossRef]
- Boruch, R.F. Assuring Confidentiality of Responses in Social Research: A Note on Strategies. Am. Sociol. 1971, 6, 308–311. [Google Scholar]
- Paulhus, D.L. Measurement and Control of Response Bias. In Measures of Personality and Social Psychological Attitudes; Robinson, J.P., Shaver, P.R., Wrightsman, L.S., Eds.; Academic Press: San Diego, CA, USA, 1991; pp. 17–59. [Google Scholar]
- Tourangeau, R.; Yan, T. Sensitive Questions in Surveys. Psychol. Bull. 2007, 133, 859–883. [Google Scholar] [CrossRef] [PubMed]
- Joinson, A. Social Desirability, Anonymity, and Internet-Based Questionnaires. Behav. Res. Methods Instrum. Comput. 1999, 31, 433–438. [Google Scholar] [CrossRef] [PubMed]
| Name of the Questionnaire | Validation Article Reference | Validation for Italian Population | Free of Charge | Number of Items | Estimated Time of Completion (min) | Aim | Further References and Notes |
|---|---|---|---|---|---|---|---|
| General Anxiety Disorder -7 | Spitzer RL et al., 2006 [35] | not present | Yes | 7 | 0:45 | Screening for generalized anxiety disorder | Italian version available at https://www.ecfs.eu/sites/default/files/general-content-files/working-groups/Mental%20Health/GAD7_Italian%20for%20Italy.pdf (accessed on 4 November 2022) |
| Patient health Questionnaire -9 | Kroenke K et al., 2001 [36] | Mazzotti E et al., 2003 [37] | Yes | 9 | 1:00 | Screening of depression | Italian version available at https://www.demenzemedicinagenerale.net/images/test/PHQ-9_Ok_20-2-2016.pdf (accessed on 4 November 2022) |
| Alcohol Use Disorders Identification Test -c | Bush K et al., 1998 [46] | not present | Yes | 3 | 0:30 | Screening for dangerous use of alcohol | Translated italian version by the National Institute of health at https://www.epicentro.iss.it/alcol/apd2014/scheda%20test%20audit%20c.pdf (accessed on 4 November 2022) |
| International Physical Activity Questionnaire | Lee PH et al., 2011 [26] | Minetto MA et al., 2018 [27] | Yes | 7 | 3:30 | Measuring type and quantity of physical activity | http://www.societaitalianadiendocrinologia.it/public/pdf/questionario_ipaq.pdf (accessed on 4 November 2022) |
| World Health Organisation-5 Wellbeing index | Topp CW et al., 2015 [47] | Nicolucci A et al., 2004 [25] | Yes | 5 | 0:30 | Measuring perceived wellbeing | High negative predictive value for the diagnosis of depression; Italian version available at https://www.psykiatri-regionh.dk/who-5/Documents/WHO5_Italian.pdf (accessed on 4 November 2022) |
| Sick, Control, One, Fat, Food Test | Morgan JF et al., 2000 [31] | Pannocchia L et al., 2011 [32] | Yes | 5 | 0:30 | Screening for eating disorders | Italian version available at https://www.sisdca.it/public/pdf/Scoff-Q.pdf (accessed on 4 November 2022) |
| Work-Sense of Coherence Questionnaire | Vogt K et al., 2013 [29] | not present | Yes | 9 | 1:00 | Investigating sense of coherence dimensions (Comprehensibility, Manageability and Meaningfulness) in the work-related context | Related to health literacy. Ongoing validation study in an Italian population. |
| Insomnia Severity index | Bastien CH et al., 2001 [33] | Castronovo V et al., 2016 [34] | Yes | 7 | 0:50 | Evaluating the perceived severity of insomnia symptoms | There are numerous questionnaires for sleep quality, but this one is short, so it could be more applicable to our goal |
| Work-related Stress Questionnaire | not validated | not present | Yes | 13 | 1:30 | Screening for work-related stress | https://pubmed.ncbi.nlm.nih.gov/32614365/ (accessed on 4 November 2022) |
| Self-related Health | Ware JE Jr, Sherbourne CD 1992 [22] | Cislaghi B, Cislaghi C 2019 [23] | Yes | 1 | 0:05 | Brief evaluation of perceived general health | / |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Catalini, A.; Mazza, C.; Cosma, C.; Minutolo, G.; De Nicolò, V.; Gallinoro, V.; Caminiti, M.; Ancona, A.; Stacchini, L.; Berselli, N.; et al. Public Health Residents’ Anonymous Survey in Italy (PHRASI): Study Protocol for a Cross-Sectional Study for a Multidimensional Assessment of Mental Health and Its Determinants. Int. J. Environ. Res. Public Health 2023, 20, 2003. https://doi.org/10.3390/ijerph20032003
Catalini A, Mazza C, Cosma C, Minutolo G, De Nicolò V, Gallinoro V, Caminiti M, Ancona A, Stacchini L, Berselli N, et al. Public Health Residents’ Anonymous Survey in Italy (PHRASI): Study Protocol for a Cross-Sectional Study for a Multidimensional Assessment of Mental Health and Its Determinants. International Journal of Environmental Research and Public Health. 2023; 20(3):2003. https://doi.org/10.3390/ijerph20032003
Chicago/Turabian StyleCatalini, Alessandro, Clara Mazza, Claudia Cosma, Giuseppa Minutolo, Valentina De Nicolò, Veronica Gallinoro, Marta Caminiti, Angela Ancona, Lorenzo Stacchini, Nausicaa Berselli, and et al. 2023. "Public Health Residents’ Anonymous Survey in Italy (PHRASI): Study Protocol for a Cross-Sectional Study for a Multidimensional Assessment of Mental Health and Its Determinants" International Journal of Environmental Research and Public Health 20, no. 3: 2003. https://doi.org/10.3390/ijerph20032003
APA StyleCatalini, A., Mazza, C., Cosma, C., Minutolo, G., De Nicolò, V., Gallinoro, V., Caminiti, M., Ancona, A., Stacchini, L., Berselli, N., Ferrari, E., Cedrone, F., Gianfredi, V., & on behalf of the Working Group on “Public Mental Health” of the Medical Residents’ Assembly of the Italian Society of Hygiene and Preventive Medicine. (2023). Public Health Residents’ Anonymous Survey in Italy (PHRASI): Study Protocol for a Cross-Sectional Study for a Multidimensional Assessment of Mental Health and Its Determinants. International Journal of Environmental Research and Public Health, 20(3), 2003. https://doi.org/10.3390/ijerph20032003