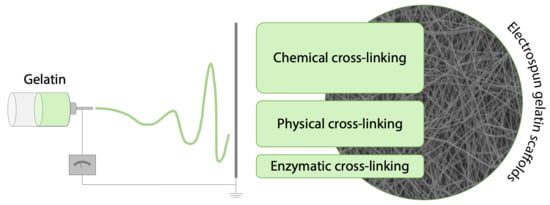
Cross-Linking Strategies for Electrospun Gelatin Scaffolds
Abstract
:1. Introduction
2. Gelatin
3. Cross-Linking Methods for Gelatin
3.1. Physical Methods
3.2. Chemical Methods
3.3. Enzymatic Methods
4. Cross-Linking Strategies for Electrospun Gelatin Fibers
4.1. Physical Strategies to Cross-Link Electrospun Matrices
4.2. Chemical Strategies to Cross-Link Electrospun Matrices
4.3. In Situ Cross-Linking Strategies
5. Biomedical Applications
6. Concluding Remarks and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Jiang, T.; Carbone, E.J.; Lo, K.W.H.; Laurencin, C.T. Electrospinning of polymer nanofibers for tissue regeneration. Prog. Polym. Sci. 2015, 46, 1–24. [Google Scholar] [CrossRef] [Green Version]
- Brown, T.D.; Dalton, P.D.; Hutmacher, D.W. Melt electrospinning today: An opportune time for an emerging polymer process. Prog. Polym. Sci. 2016, 56, 116–166. [Google Scholar] [CrossRef]
- Wang, C.; Wang, J.; Zeng, L.; Qiao, Z.; Liu, X.; Liu, H.; Zhang, J.; Ding, J. Fabrication of electrospun polymer nanofibers with diverse morphologies. Molecules 2019, 24, 834. [Google Scholar] [CrossRef] [PubMed]
- Haider, A.; Haider, S.; Kang, I.K. A comprehensive review summarizing the effect of electrospinning parameters and potential applications of nanofibers in biomedical and biotechnology. Arab. J. Chem. 2018, 11, 1165–1188. [Google Scholar] [CrossRef]
- Cheng, J.; Jun, Y.; Qin, J.; Lee, S.H. Electrospinning versus microfluidic spinning of functional fibers for biomedical applications. Biomaterials 2017, 114, 121–143. [Google Scholar] [CrossRef] [PubMed]
- Soares, R.M.D.; Siqueira, N.M.; Prabhakaram, M.P.; Ramakrishna, S. Electrospinning and electrospray of bio-based and natural polymers for biomaterials development. Mater. Sci. Eng. C 2018, 92, 969–982. [Google Scholar] [CrossRef]
- Rinoldi, C.; Kijeńska, E.; Chlanda, A.; Choinska, E.; Khenoussi, N.; Tamayol, A.; Khademhosseini, A.; Swieszkowski, W. Nanobead-on-string composites for tendon tissue engineering. J. Mater. Chem. B 2018, 6, 3116–3127. [Google Scholar] [CrossRef]
- Magin, C.M.; Alge, D.L.; Anseth, K.S. Bio-inspired 3D microenvironments: A new dimension in tissue engineering. Biomed. Mater. 2016, 11, 022001. [Google Scholar] [CrossRef]
- Xue, J.; Wu, T.; Dai, Y.; Xia, Y. Electrospinning and electrospun nanofibers: Methods, materials, and applications. Chem. Rev. 2019, 119, 5298–5415. [Google Scholar] [CrossRef]
- Su, K.; Wang, C. Recent advances in the use of gelatin in biomedical research. Biotechnol. Lett. 2015, 37, 2139–2145. [Google Scholar] [CrossRef]
- Gorgieva, S.; Kokol, V. Collagen- vs. Gelatine-Based Biomaterials and Their Biocompatibility: Review and Perspectives. In Biomaterials Applications for Nanomedicine; BoD–Books on Demand: Norderstedt, Germany, 2011; pp. 17–52. ISBN 978-953-51-0296-0. [Google Scholar]
- Shoulders, M.D.; Raines, R.T. Collagen Structure and Stability. Annu. Rev. Biochem. 2009, 78, 929–958. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sell, S.A.; Wolfe, P.S.; Garg, K.; McCool, J.M.; Rodriguez, I.A.; Bowlin, G.L. The Use of Natural Polymers in Tissue Engineering: A Focus on Electrospun Extracellular Matrix Analogues. Polymers 2010, 2, 522–553. [Google Scholar] [CrossRef]
- Gomez-Guillen, M.C.; Gimenez, B.; Lopez-Caballero, M.E.; Montero, M.P. Functional and bioactive properties of collagen and gelatin from alternative sources: A review. Food Hydrocoll. 2011, 25, 1813–1827. [Google Scholar] [CrossRef] [Green Version]
- Schmidt, M.M.; Dornelles, R.C.P.; Mello, R.O.; Kubota, E.H.; Mazutti, M.A.; Kempka, A.P.; Demiate, I.M. Collagen extraction process. Int. Food Res. J. 2016, 23, 913–922. [Google Scholar]
- Duconseille, A.; Astruc, T.; Quintana, N.; Meersman, F.; Sante-Lhoutellier, V. Gelatin structure and composition linked to hard capsule dissolution: A review. Food Hydrocoll. 2015, 43, 360–376. [Google Scholar] [CrossRef]
- Scott, G. Degradable Polymers: Principles and Applications, 2nd ed.; Scott, G., Ed.; Springer: Berlin, Germany, 2002; ISBN 978-94-017-1217-0. [Google Scholar]
- Emma Campiglio, C.; Marcolin, C.; Draghi, L. Electrospun ECM macromolecules as biomimetic scaffold for regenerative medicine: Challenges for preserving conformation and bioactivity. AIMS Mater. Sci. 2017, 4, 638–669. [Google Scholar] [CrossRef]
- Forero, J.C.; Roa, E.; Reyes, J.G.; Acevedo, C.; Osses, N. Development of useful biomaterial for bone tissue Engineering by incorporating Nano-Copper-Zinc Alloy (nCuZn) in Chitosan/Gelatin/Nano-Hydroxyapatite (Ch/G/nHAp) scaffold. Materials 2017, 10, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Feyen, D.A.M.; Gaetani, R.; Deddens, J.; Van Keulen, D.; Van Opbergen, C.; Poldervaart, M.; Alblas, J.; Chamuleau, S.; Van Laake, L.W.; Doevendans, P.A.; et al. Gelatin Microspheres as Vehicle for Cardiac Progenitor Cells Delivery to the Myocardium. Adv. Healthc. Mater. 2016, 5, 1071–1079. [Google Scholar] [CrossRef]
- Milazzo, M.; Contessi Negrini, N.; Scialla, S.; Marelli, B.; Farè, S.; Danti, S.; Buehler, M.J. Additive Manufacturing Approaches for Hydroxyapatite-Reinforced Composites. Adv. Funct. Mater. 2019, 1–26. [Google Scholar] [CrossRef]
- Wisotzki, E.I.; Hennes, M.; Schuldt, C.; Engert, F.; Knolle, W.; Decker, U.; Käs, J.A.; Zink, M.; Mayr, S.G. Tailoring the material properties of gelatin hydrogels by high energy electron irradiation. J. Mater. Chem. B 2014, 2, 4297. [Google Scholar] [CrossRef]
- van Vlierberghe, S. Crosslinking strategies for porous gelatin scaffolds. J. Mater. Sci. 2016, 51, 1–9. [Google Scholar] [CrossRef]
- Terao, K.; Nagasawa, N.; Nishida, H.; Furusawa, K.; Mori, Y.; Yoshii, F.; Dobashi, T. Reagent-free crosslinking of aqueous gelatin: Manufacture and characteristics of gelatin gels irradiated with gamma-ray and electron beam. J. Biomater. Sci. Polym. Ed. 2003, 14, 1197–1208. [Google Scholar] [CrossRef]
- Cataldo, F.; Ursini, O.; Lilla, E.; Angelini, G. Radiation-induced crosslinking of collagen gelatin into a stable hydrogel. J. Radioanal. Nucl. Chem. 2008, 275, 125–131. [Google Scholar] [CrossRef]
- Kojima, T.; Bessho, M.; Furuta, M.; Okuda, S. Characterization of biopolymer hydrogels produced by g -ray irradiation. Radiat. Phys. Chem. 2004, 71, 233–236. [Google Scholar] [CrossRef]
- Prasertsung, I.; Damrongsakkul, S.; Saito, N. Crosslinking of a gelatin solutions induced by pulsed electrical discharges in solutions. Plasma Process. Polym. 2013, 10, 792–797. [Google Scholar] [CrossRef]
- Hussain, A.; Takahashi, K.; Sonobe, J.; Tabata, Y.; Bessho, K. Bone Regeneration of Rat Calvarial Defect by Magnesium Calcium Phosphate Gelatin Scaffolds with or without Bone Morphogenetic Protein-2. J. Maxillofac. Oral Surg. 2014, 13, 29–35. [Google Scholar] [CrossRef]
- Omata, K.; Matsuno, T.; Asano, K.; Hashimoto, Y.; Tabata, Y.; Satoh, T. Enhanced bone regeneration by gelatin–b-tricalcium phosphate composites enabling controlled release of bFGF. J. Tissue Eng. Regen. Med. 2014, 8, 604–611. [Google Scholar] [CrossRef]
- Prasertsung, I.; Mongkolnavin, R.; Kanokpanont, S.; Damrongsakkul, S. The effects of pulsed inductively coupled plasma (PICP) on physical properties and biocompatibility of crosslinked gelatin films. Int. J. Biol. Macromol. 2010, 46, 72–78. [Google Scholar] [CrossRef]
- Kuijpers, A.J.; Engbers, G.H.; Krijgsveld, J.; Zaat, S.A.; Dankert, J.; Feijen, J. Cross-linking and characterisation of gelatin matrices for biomedical applications. J. Biomater. Sci. Polym. Ed. 2012, 11, 225–243. [Google Scholar] [CrossRef]
- Claaßen, C.; Sewald, L.; Tovar, G.; Borchers, K. Controlled Release of Vascular Endothelial Growth Factor from Heparin-Functionalized Gelatin Type A and Albumin Hydrogels. Gels 2017, 3, 35. [Google Scholar] [CrossRef]
- Rodriguez, I.A.; Saxena, G.; Hixon, K.R.; Sell, S.A.; Bowlin, G.L. In vitro characterization of MG-63 osteoblast-like cells cultured on organic-inorganic lyophilized gelatin sponges for early bone healing. J. Biomed. Mater. Res. Part A 2016, 104, 2011–2019. [Google Scholar] [CrossRef]
- Gorgieva, S.; Štrancar, J.; Kokol, V. Evaluation of surface/interface-related physicochemical and microstructural properties of gelatin 3D scaffolds, and their influence on fibroblast growth and morphology. J. Biomed. Mater. Res. Part A 2014, 102, 3986–3997. [Google Scholar] [CrossRef]
- Ninan, N.; Grohens, Y.; Elain, A.; Kalarikkal, N.; Thomas, S. Synthesis and characterisation of gelatin/zeolite porous scaffold. Eur. Polym. J. 2013, 49, 2433–2445. [Google Scholar] [CrossRef]
- Fan, H.Y.; Duquette, D.; Dumont, M.J.; Simpson, B.K. Salmon skin gelatin-corn zein composite films produced via crosslinking with glutaraldehyde: Optimization using response surface methodology and characterization. Int. J. Biol. Macromol. 2018, 120, 263–273. [Google Scholar] [CrossRef]
- Poursamar, S.A.; Lehner, A.N.; Azami, M.; Ebrahimi-Barough, S.; Samadikuchaksaraei, A.; Antunes, A.P.M. The effects of crosslinkers on physical, mechanical, and cytotoxic properties of gelatin sponge prepared via in-situ gas foaming method as a tissue engineering scaffold. Mater. Sci. Eng. C 2016, 63, 1–9. [Google Scholar] [CrossRef]
- Kirchmajer, D.M.; Watson, C.A.; Ranson, M. Gelapin, a degradable genipin cross-linked gelatin hydrogel. RSC Adv. 2012, 3, 1073–1081. [Google Scholar] [CrossRef] [Green Version]
- Wu, T.; Zhang, Q.; Ren, W.; Yi, X.; Zhou, Z.; Peng, X.; Yu, X.; Lang, M. Controlled release of gentamicin from gelatin/genipin reinforced beta-tricalcium phosphate scaffold for the treatment of osteomyelitis. J. Mater. Chem. B 2013, 1, 3304. [Google Scholar] [CrossRef]
- Liang, H.C.; Chang, W.H.; Liang, H.F.; Lee, M.H.; Sung, H.W. Crosslinking structures of gelatin hydrogels crosslinked with genipin or a water-soluble carbodiimide. J. Appl. Polym. Sci. 2004, 91, 4017–4026. [Google Scholar] [CrossRef]
- Focaroli, S.; Teti, G.; Salvatore, V.; Durante, S.; Belmonte, M.M.; Giardino, R.; Mazzotti, A.; Bigi, A.; Falconi, M. Chondrogenic differentiation of human adipose mesenchimal stem cells: Influence of a biomimetic gelatin genipin crosslinked porous scaffold. Microsc. Res. Tech. 2014, 77, 928–934. [Google Scholar] [CrossRef]
- Zhao, X.; Lang, Q.; Yildirimer, L.; Lin, Z.Y.; Cui, W.; Annabi, N.; Ng, K.W.; Dokmeci, M.R.; Ghaemmaghami, A.M.; Khademhosseini, A. Photocrosslinkable Gelatin Hydrogel for Epidermal Tissue Engineering. Adv. Healthc. Mater. 2016, 5, 108–118. [Google Scholar] [CrossRef]
- Van Nieuwenhove, I.; Salamon, A.; Peters, K.; Graulus, G.J.; Martins, J.C.; Frankel, D.; Kersemans, K.; De Vos, F.; Van Vlierberghe, S.; Dubruel, P. Gelatin- and starch-based hydrogels. Part A: Hydrogel development, characterization and coating. Carbohydr. Polym. 2016, 152, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Tan, G.; Tan, Y.; Wang, H.; Liao, J.; Ning, C. Biomimetic mineralization of anionic gelatin hydrogels: Effect of degree of methacrylation. RSC Adv. 2014, 4, 21997–22008. [Google Scholar] [CrossRef]
- Celikkin, N.; Mastrogiacomo, S.; Jaroszewicz, J.; Walboomers, X.F.; Swieszkowski, W. Gelatin methacrylate scaffold for bone tissue engineering: The influence of polymer concentration. J. Biomed. Mater. Res. Part A 2017, 106, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Contessi Negrini, N.; Tarsini, P.; Tanzi, M.C.; Farè, S. Chemically crosslinked gelatin hydrogels as scaffolding materials for adipose tissue engineering. J. Appl. Polym. Sci. 2019, 47104, 1–12. [Google Scholar] [CrossRef]
- Contessi Negrini, N.; Bonnetier, M.; Giatsidis, G.; Orgill, D.P.; Farè, S.; Marelli, B. Tissue-mimicking gelatin scaffolds by alginate sacrificial templates for adipose tissue engineering. Acta Biomater. 2019, 87, 61–75. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, K. Evaluation of isophorone diisocyanate crosslinked gelatin as a carrier for controlled delivery of drugs. Polym. Bull. 2013, 70, 733–753. [Google Scholar] [CrossRef]
- Vargas, G.; Acevedo, J.L.; López, J.; Romero, J. Study of cross-linking of gelatin by ethylene glycol diglycidyl ether. Mater. Lett. 2008, 62, 3656–3658. [Google Scholar] [CrossRef]
- Yung, W.A.; Wu, L.Q.; Tullman, J.A.; Payne, G.F.; Bentley, W.E.; Barbari, T.A. Transglutaminase crosslinked gelatin as a tissue engineering scaffold. J. Biomed. Mater. Res. Part A 2007, 83, 1039–1046. [Google Scholar] [CrossRef]
- Broderick, E.P.; O’Halloran, D.M.; Rochev, Y.A.; Griffin, M.; Collighan, R.J.; Pandit, A.S. Enzymatic stabilization of gelatin-based scaffolds. J. Biomed. Mater. Res. Part B Appl. Biomater. 2005, 72, 37–42. [Google Scholar] [CrossRef]
- Yang, G.; Xiao, Z.; Ren, X.; Long, H.; Qian, H.; Ma, K.; Guo, Y. Enzymatically crosslinked gelatin hydrogel promotes the proliferation of adipose tissue-derived stromal cells. PeerJ 2016, 4, e2497. [Google Scholar] [CrossRef]
- Lee, J.B.; Ko, Y.G.; Cho, D.; Park, W.H.; Kwon, O.H. Modification and optimization of electrospun gelatin sheets by electronbeam irradiation for soft tissue engineering. Biomater. Res. 2017, 21, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Gomes, S.R.; Rodrigues, G.; Martins, G.G.; Henriques, C.M.R.; Silva, J.C. In vitro evaluation of crosslinked electrospun fish gelatin scaffolds. Mater. Sci. Eng. C 2013, 33, 1219–1227. [Google Scholar] [CrossRef] [PubMed]
- Tungtasana, H.; Damrongsakkul, S.; Shuangshoti, S.; Kanokpanont, S.; Kaplan, D.L.; Bunaprasert, T. Tissue response and biodegradation of composite scaffolds prepared from Thai silk fibroin, gelatin and hydroxyapatite. J. Mater. Sci. Mater. Med. 2010, 21, 3151–3162. [Google Scholar] [CrossRef] [PubMed]
- Ratanavaraporn, J.; Rangkupan, R.; Jeeratawatchai, H.; Kanokpanont, S.; Damrongsakkul, S. Influences of physical and chemical crosslinking techniques on electrospun type A and B gelatin fiber mats. Int. J. Biol. Macromol. 2010, 47, 431–438. [Google Scholar] [CrossRef] [PubMed]
- Rose, J.B.; Pacelli, S.; El Haj, A.J.; Dua, H.S.; Hopkinson, A.; White, L.J.; Rose, F.R.A.J. Gelatin-based materials in ocular tissue engineering. Materials 2014, 7, 3106–3135. [Google Scholar] [CrossRef]
- Chou, S.F.; Luo, L.J.; Lai, J.Y.; Ma, D.H.K. Role of solvent-mediated carbodiimide cross-linking in fabrication of electrospun gelatin nanofibrous membranes as ophthalmic biomaterials. Mater. Sci. Eng. C 2017, 71, 1145–1155. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Yan, Q.; Liu, H.B.; Zhou, X.H.; Xiao, S.J. Different EDC/NHS activation mechanisms between PAA and PMAA brushes and the following amidation reactions. Langmuir 2011, 27, 12058–12068. [Google Scholar] [CrossRef]
- Gorgieva, S.; Kokol, V. Processing of gelatin-based cryogels with improved thermomechanical resistance, pore size gradient, and high potential for sustainable protein drug release. J. Biomed. Mater. Res. Part A 2015, 103, 1119–1130. [Google Scholar] [CrossRef]
- Chang, J.Y.; Lin, J.H.; Yao, C.H.; Chen, J.H.; Lai, T.Y.; Chen, Y.S. In vivo evaluation of a biodegradable EDC/NHS-cross-linked gelatin peripheral nerve guide conduit material. Macromol. Biosci. 2007, 7, 500–507. [Google Scholar] [CrossRef]
- Kavoosi, G.; Bordbar, Z.; Dadfar, S.M.; Dadfar, S.M.M. Preparation and characterization of a novel gelatin–poly(vinyl alcohol) hydrogel film loaded with Zataria multiflora essential oil for antibacterial–antioxidant wound-dressing applications. J. Appl. Polym. Sci. 2017, 134, 1–9. [Google Scholar] [CrossRef]
- Cañas, A.I.; Delgado, J.P.; Gartner, C. Biocompatible scaffolds composed of chemically crosslinked chitosan and gelatin for tissue engineering. J. Appl. Polym. Sci. 2016, 133, 1–10. [Google Scholar] [CrossRef]
- Manickam, B.; Sreedharan, R.; Elumalai, M. ‘Genipin’–The Natural Water Soluble Cross-linking Agent and Its Importance in the Modified Drug Delivery Systems: An Overview. Curr. Drug Deliv. 2014, 11, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Pal, K.; Paulson, A.T.; Rousseau, D. Biopolymers in Controlled-Release Delivery Systems; Academic Press: Cambridge, MA, USA, 2009; ISBN 9780123741950. [Google Scholar]
- Echave, M.C.; Pimenta-Lopes, C.; Pedraz, J.L.; Mehrali, M.; Dolatshahi-Pirouz, A.; Ventura, F.; Orive, G. Enzymatic crosslinked gelatin 3D scaffolds for bone tissue engineering. Int. J. Pharm. 2019, 562, 151–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jus, S.; Stachel, I.; Fairhead, M.; Meyer, M.; Thöny-Meyer, L.; Guebitz, G.M. Enzymatic cross-linking of gelatine with laccase and tyrosinase. Biocatal. Biotransform. 2012, 30, 86–95. [Google Scholar] [CrossRef]
- Choi, Y.R.; Kim, E.H.; Lim, S.; Choi, Y.S. Efficient preparation of a permanent chitosan/gelatin hydrogel using an acid-tolerant tyrosinase. Biochem. Eng. J. 2018, 129, 50–56. [Google Scholar] [CrossRef]
- Chen, T.; Embree, H.D.; Brown, E.M.; Taylor, M.M.; Payne, G.F. Enzyme-catalyzed gel formation of gelatin and chitosan: Potential for in situ applications. Biomaterials 2003, 24, 2831–2841. [Google Scholar] [CrossRef]
- Sisson, K.; Zhang, C.; Farach-Carson, M.C.; Chase, D.B.; Rabolt, J.F. Evaluation of cross-linking methods for electrospun gelatin on cell growth and viability. Biomacromolecules 2009, 10, 1675–1680. [Google Scholar] [CrossRef]
- Liguori, A.; Bigi, A.; Colombo, V.; Focarete, M.L.; Gherardi, M.; Gualandi, C.; Oleari, M.C.; Panzavolta, S. Atmospheric Pressure Non-Equilibrium Plasma as a Green Tool to Crosslink Gelatin Nanofibers. Sci. Rep. 2016, 6, 1–11. [Google Scholar] [CrossRef]
- Ghassemi, Z.; Slaughter, G. Storage stability of electrospun pure gelatin stabilized with EDC/Sulfo-NHS. Biopolymers 2018, 109, e23232. [Google Scholar] [CrossRef]
- Li, J.; He, A.; Zheng, J.; Han, C.C. Gelatin and gelatin—Hyaluronic acid nanofibrous membranes produced by electrospinning of their aqueous solutions. Biomacromolecules 2006, 7, 2243–2247. [Google Scholar] [CrossRef]
- Zhang, S.; Huang, Y.; Yang, X.; Mei, F.; Ma, Q.; Chen, G.; Ryu, S.; Deng, X. Gelatin nanofibrous membrane fabricated by electrospinning of aqueous gelatin solution for guided tissue regeneration. J. Biomed. Mater. Res. A 2009, 90, 671–679. [Google Scholar] [CrossRef] [PubMed]
- Tonsomboon, K.; Oyen, M.L. Composite electrospun gelatin fiber-alginate gel scaffolds for mechanically robust tissue engineered cornea. J. Mech. Behav. Biomed. Mater. 2013, 21, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Panzavolta, S.; Gioffrè, M.; Focarete, M.L.; Gualandi, C.; Foroni, L.; Bigi, A. Electrospun gelatin nanofibers: Optimization of genipin cross-linking to preserve fiber morphology after exposure to water. Acta Biomater. 2011, 7, 1702–1709. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Wang, L.; Jiang, H. The effect of procyanidine crosslinking on the properties of the electrospun gelatin membranes. Biofabrication 2012, 4, 035007. [Google Scholar] [CrossRef] [PubMed]
- Del Gaudio, C.; Baiguera, S.; Boieri, M.; Mazzanti, B.; Ribatti, D.; Bianco, A.; Macchiarini, P. Induction of angiogenesis using VEGF releasing genipin-crosslinked electrospun gelatin mats. Biomaterials 2013, 34, 7754–7765. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.Z.; Venugopal, J.; Huang, Z.M.; Lim, C.T.; Ramakrishna, S. Crosslinking of the electrospun gelatin nanofibers. Polymer 2006, 47, 2911–2917. [Google Scholar] [CrossRef]
- Vardiani, M.; Gholipourmalekabadi, M.; Ghaffari Novin, M.; Koruji, M.; Ghasemi Hamidabadi, H.; Salimi, M.; Nazarian, H. Three-dimensional electrospun gelatin scaffold coseeded with embryonic stem cells and sertoli cells: A promising substrate for in vitro coculture system. J. Cell. Biochem. 2019, 120, 12508–12518. [Google Scholar] [CrossRef]
- Laha, A.; Yadav, S.; Majumdar, S.; Sharma, C.S. In-vitro release study of hydrophobic drug using electrospun cross-linked gelatin nanofibers. Biochem. Eng. J. 2016, 105, 481–488. [Google Scholar] [CrossRef]
- Elsayed, Y.; Lekakou, C.; Labeed, F.; Tomlins, P. Fabrication and characterisation of biomimetic, electrospun gelatin fibre scaffolds for tunica media-equivalent, tissue engineered vascular grafts. Mater. Sci. Eng. C 2016, 61, 473–483. [Google Scholar] [CrossRef] [Green Version]
- Elsayed, Y.; Lekakou, C.; Labeed, F.; Tomlins, P. Smooth muscle tissue engineering in crosslinked electrospun gelatin scaffolds. J. Biomed. Mater. Res. Part A 2016, 104, 313–321. [Google Scholar] [CrossRef]
- Zhan, J.; Morsi, Y.; Ei-Hamshary, H.; Al-Deyab, S.S.; Mo, X. In vitro evaluation of electrospun gelatin–glutaraldehyde nanofibers. Front. Mater. Sci. 2016, 10, 90–100. [Google Scholar] [CrossRef]
- Gomes, S.R.; Rodrigues, G.; Martins, G.G.; Roberto, M.A.; Mafra, M.; Henriques, C.M.R.; Silva, J.C. In vitro and in vivo evaluation of electrospun nanofibers of PCL, chitosan and gelatin: A comparative study. Mater. Sci. Eng. C 2015, 46, 348–358. [Google Scholar] [CrossRef] [PubMed]
- Rujitanaroj, P.O.; Pimpha, N.; Supaphol, P. Wound-dressing materials with antibacterial activity from electrospun gelatin fiber mats containing silver nanoparticles. Polymer 2008, 49, 4723–4732. [Google Scholar] [CrossRef]
- Nguyen, T.-H.; Lee, B.-T. Fabrication and characterization of cross-linked gelatin electro-spun nano-fibers. J. Biomed. Sci. Eng. 2010, 3, 1117–1124. [Google Scholar] [CrossRef] [Green Version]
- Lakshminarayanan, R.; Sridhar, R.; Loh, X.J.; Nandhakumar, M.; Barathi, V.A.; Kalaipriya, M.; Kwan, J.L.; Liu, S.P.; Beuerman, R.W.; Ramakrishna, S. Interaction of gelatin with polyenes modulates antifungal activity and biocompatibility of electrospun fiber mats. Int. J. Nanomed. 2014, 9, 2439–2458. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.C.; Chang, W.H.; Dong, G.C.; Chen, K.Y.; Chen, Y.S.; Yao, C.H. Cell adhesion and proliferation enhancement by gelatin nanofiber scaffolds. J. Bioact. Compat. Polym. 2011, 26, 565–577. [Google Scholar] [CrossRef]
- Skotak, M.; Noriega, S.; Larsen, G.; Subramanian, A. Electrospun cross-linked gelatin fibers with controlled diameter: The effect of matrix stiffness on proliferative and biosynthetic activity of chondrocytes cultured in vitro. J. Biomed. Mater. Res. Part A 2010, 95, 828–836. [Google Scholar] [CrossRef] [PubMed]
- Skotak, M.; Ragusa, J.; Gonzalez, D.; Subramanian, A. Improved cellular infiltration into nanofibrous electrospun cross-linked gelatin scaffolds templated with micrometer-sized polyethylene glycol fibers. Biomed. Mater. 2011, 6, 55012. [Google Scholar] [CrossRef]
- Binan, L.; Tendey, C.; De Crescenzo, G.; El Ayoubi, R.; Ajji, A.; Jolicoeur, M. Differentiation of neuronal stem cells into motor neurons using electrospun poly-l-lactic acid/gelatin scaffold. Biomaterials 2014, 35, 664–674. [Google Scholar] [CrossRef]
- Dias, J.R.; Baptista-Silva, S.; de Oliveira, C.M.T.; Sousa, A.; Oliveira, A.L.; Bártolo, P.J.; Granja, P.L. In situ crosslinked electrospun gelatin nanofibers for skin regeneration. Eur. Polym. J. 2017, 95, 161–173. [Google Scholar] [CrossRef] [Green Version]
- Kishan, A.P.; Nezarati, R.M.; Radzicki, C.M.; Renfro, A.L.; Robinson, J.L.; Whitely, M.E.; Cosgriff-Hernandez, E.M. In situ crosslinking of electrospun gelatin for improved fiber morphology retention and tunable degradation. J. Mater. Chem. B 2015, 3, 7930–7938. [Google Scholar] [CrossRef]
- Jalaja, K.; James, N.R. Electrospun gelatin nanofibers: A facile cross-linking approach using oxidized sucrose. Int. J. Biol. Macromol. 2015, 73, 270–278. [Google Scholar] [CrossRef] [PubMed]
- Tonda-Turo, C.; Cipriani, E.; Gnavi, S.; Chiono, V.; Mattu, C.; Gentile, P.; Perroteau, I.; Zanetti, M.; Ciardelli, G. Crosslinked gelatin nanofibres: Preparation, characterisation and in vitro studies using glial-like cells. Mater. Sci. Eng. C 2013, 33, 2723–2735. [Google Scholar] [CrossRef] [PubMed]
- Gnavi, S.; Elena Fornasari, B.; Tonda-Turo, C.; Laurano, R.; Zanetti, M.; Ciardelli, G.; Geuna, S. The effect of electrospun gelatin fibers alignment on schwann cell and axon behavior and organization in the perspective of artificial nerve design. Int. J. Mol. Sci. 2015, 16, 12925–12942. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Lang, Q.; Zhang, H.; Cheng, L.; Zhang, Y.; Pan, G.; Zhao, X.; Yang, H.; Zhang, Y.; Santos, H.A.; et al. Electrospun Photocrosslinkable Hydrogel Fibrous Scaffolds for Rapid In Vivo Vascularized Skin Flap Regeneration. Adv. Funct. Mater. 2017, 27, 1–12. [Google Scholar] [CrossRef]
- Ferreira, P.; Santos, P.; Alves, P.; Carvalho, M.P.; de Sá, K.D.; Miguel, S.P.; Correia, I.J.; Coimbra, P. Photocrosslinkable electrospun fiber meshes for tissue engineering applications. Eur. Polym. J. 2017, 97, 210–219. [Google Scholar] [CrossRef]
- Zhao, X.; Sun, X.; Yildirimer, L.; Lang, Q.; Lin, Z.Y.W.; Zheng, R.; Zhang, Y.; Cui, W.; Annabi, N.; Khademhosseini, A. Cell infiltrative hydrogel fibrous scaffolds for accelerated wound healing. Acta Biomater. 2017, 49, 66–77. [Google Scholar] [CrossRef]
- Lin, W.H.; Tsai, W.B. In situ UV-crosslinking gelatin electrospun fibers for tissue engineering applications. Biofabrication 2013, 5, 035008. [Google Scholar] [CrossRef]
- Jiang, Q.; Reddy, N.; Zhang, S.; Roscioli, N.; Yang, Y. Water-stable electrospun collagen fibers from a non-toxic solvent and crosslinking system. J. Biomed. Mater. Res. Part A 2013, 101, 1237–1247. [Google Scholar] [CrossRef]
- Lai, J.-Y. Interrelationship between cross-linking structure, molecular stability, and cytocompatibility of amniotic membranes cross-linked with glutaraldehyde of varying concentrations. RSC Adv. 2014, 4, 18871–18880. [Google Scholar] [CrossRef]
- Gao, S.; Yuan, Z.; Guo, W.; Chen, M.; Liu, S.; Xi, T.; Guo, Q. Comparison of glutaraldehyde and carbodiimides to crosslink tissue engineering scaffolds fabricated by decellularized porcine menisci. Mater. Sci. Eng. C 2017, 71, 891–900. [Google Scholar] [CrossRef] [PubMed]
- Barnes, C.P.; Pemble, C.W.; Brand, D.D.; Simpson, D.G.; Bowlin, G.L. Cross-Linking Electrospun Type II Collagen Tissue Engineering Scaffolds with Carbodiimide in Ethanol. Tissue Eng. 2007, 13, 1593–1605. [Google Scholar] [CrossRef] [PubMed]
- Kai, D.; Liow, S.S.; Loh, X.J. Biodegradable polymers for electrospinning: Towards biomedical applications. Mater. Sci. Eng. C 2015, 45, 659–670. [Google Scholar] [CrossRef] [PubMed]
- Taylor, B.L.; Limaye, A.; Yarborough, J.; Freeman, J.W. Investigating processing techniques for bovine gelatin electrospun scaffolds for bone tissue regeneration. J. Biomed. Mater. Res. Part B Appl. Biomater. 2017, 105, 1131–1140. [Google Scholar] [CrossRef] [PubMed]
- Mi, S.; Kong, B.; Wu, Z.; Sun, W.; Xu, Y.; Su, X. A novel electrospinning setup for the fabrication of thickness-controllable 3D scaffolds with an ordered nanofibrous structure. Mater. Lett. 2015, 160, 343–346. [Google Scholar] [CrossRef]
- Hejazi, F.; Mirzadeh, H.; Contessi, N.; Tanzi, M.C.; Faré, S.; Farè, S. Novel class of collector in electrospinning device for the fabrication of 3D nanofibrous structure for large defect load-bearing tissue engineering application. J. Biomed. Mater. Res. Part A 2017, 105, 1535–1548. [Google Scholar] [CrossRef] [PubMed]
- Poologasundarampillai, G.; Wang, D.; Li, S.; Nakamura, J.; Bradley, R.; Lee, P.D.; Stevens, M.M.; McPhail, D.S.; Kasuga, T.; Jones, J.R. Cotton-wool-like bioactive glasses for bone regeneration. Acta Biomater. 2014, 10, 3733–3746. [Google Scholar] [CrossRef] [PubMed]
- Baker, B.M.; Gee, A.O.; Metter, R.B.; Nathan, A.S.; Marklein, R.A.; Burdick, J.A.; Mauck, R.L. The potential to improve cell infiltration in composite fiber-aligned electrospun scaffolds by the selective removal of sacrificial fibers. Biomaterials 2008, 29, 2348–2358. [Google Scholar] [CrossRef] [Green Version]
- Ameer, J.M.; Kasoju, N. Strategies to Tune Electrospun Sca ff old Porosity for E ff ective Cell Response in Tissue Engineering. J. Funct. Biomater. 2019, 10, 30. [Google Scholar] [CrossRef]






| Cross-Linking Method | Gelatin Type | Gelatin Concentration (w/v) | Reference |
|---|---|---|---|
| Physical Methods | |||
| High energy electron beam | type A | 2–20% | Wisotzki et al. 2014 [22] |
| type B | 10% | Van Vlierberghe 2016 [23] | |
| type A, type B and cold fish skin gelatin | 1–30% | Terao et al. 2012 [24] | |
| γ-irradiation | type A | 3% | Cataldo et al. 2008 [25] |
| type B | 1–20% | Kojima et al. 2004 [26] | |
| Plasma treatment | type A | 1.25–2.5% | Prasertsung et al. 2013 [27] |
| Dehydrothermal treatment | type A | 3% | Hussain et al. 2014 [28] |
| type B | 10% | Omata et al. 2014 [29] | |
| type A | 10% | Prasertsung et al. 2010 [30] | |
| Chemical Methods | |||
| EDC/NHS 1 | type A and B | 10% | Kuijpers et al. 2012 [31] |
| type A | 10% | Claaßen et al. 2017 [32] | |
| type B | 3% | Rodriguez et al. 2016 [33] | |
| type B | 10% | Gorgieva et al. 2014 [34] | |
| Formaldehyde | type B | 2% | Ninan et al. 2013 [35] |
| Glutaraldehyde | - | 5% | Fan et al. 2018 [36] |
| type B | 20% | Poursamar et al. 2016 [37] | |
| Genipin | type A | 2–10% | Kirchmajer et al. 2013 [38] |
| - | 10% | Wu et al. 2013 [39] | |
| - | 8% | Liang et al. 2004 [40] | |
| - | 10% | Focaroli et al. 2014 [41] | |
| Irgacure 2959 + UV light 2 | type B | 5–20% | Zhao et al. 2016 [42] |
| type B | 10% | Van Nieuwenhove et al. 2016 [43] | |
| type B | 10% | Zhou et al. 2014 [44] | |
| type A | 5–10% | Celikkin et al. 2017 [45] | |
| N,N′-methylenebis (acrylamide) | type A | 15–25% | Contessi Negrini et al. 2019 [46,47] |
| Isophorone diisocyanate | - | 6% | Subramanian et al. 2013 [48] |
| Ethylene glycol diglycidyl ether | type B | 15% | Vargas et al. 2008 [49] |
| Enzymatic Methods | |||
| Microbial transglutaminase | type A | 10% | Yung et al. 2007 [50] |
| type A | 4% | Broderick et al. 2004 [51] | |
| type A | 1–10% | Yang et al. 2016 [52] | |
| Physical Methods | |||||||
| Gelatin | Parameters | Application | Reference | ||||
| Irradiation Dose | Accelerating Voltage | Current | Dose Rate | ||||
| Electron Beam Irradiation | type B | 10–300 kGy | 1 MeV | 17 mA | 8.33 kGy/s | Soft tissue engineering | Lee et al. [53] |
| Gelatin | Parameters | Application | Reference | ||||
| Pressure | Gas | Reaction Time | Type of Plasma | ||||
| Plasma Treatment | - | Low | Oxygen | 2 min | Non-equilibrium | Tissue engineering | Sisson et al. 2009 [70] |
| type A, B | Low | Argon | - | Non-equilibrium Pulsed inductively coupled | Biomedical | Ratanavaraporn et al. 2010 [56] | |
| type A | Atmospheric | Air | 20 min | Non-equilibrium | Tissue engineering | Liguori et al. 2016 [71] | |
| Gelatin | Parameters | Application | Reference | ||||
| Reaction Temperature | Reaction Time | ||||||
| Dehydrothermal Treatment | type A, B | 140 °C | 48 h | Biomedical | Ratanavaraporn et al. 2010 [56] | ||
| Fish | 140 °C | 24/48/72 h | Tissue engineering | Gomes et al. 2013 [54] | |||
| type A | 160 °C | 48 h | Tissue engineering | Ghassemi and Slaughter 2018 [72] | |||
| Chemical Methods | |||||||
| Gelatin | Parameters | Application | Reference | ||||
| Cross-Linker Concentration | Solvent | Reaction Time | Reaction Temperature | ||||
| EDC/NHS | type A | EDC = 50 mM | EtOH/dH2O 8/2 | 24 h | 4 °C | Biomedical | Li et al. 2006 [73] |
| - | EDC = 5/25/50/75 mM EDC/NHS = 2.5/1 | EtOH/dH2O 9/1 | 24 h | 4 °C | Periodontal tissue regeneration/Cornea regeneration | Zhang et al. 2009 [74] Tonsomboon et al. 2013 [75] | |
| type A, B | EDC = 14 mM NHS = 5.5 mM | EtOH or dH2O | 2 h | - | Biomedical | Ratanavaraporn et al. 2010 [56] | |
| type B | EDC = 2 M NHS = 1 M | EtOH/dH2O 9/1 | 7 h | - | Tissue engineering | Ghassemi and Slaughter 2018 [72] | |
| type A | EDC = 5 mM/mg sample EDC/NHS = 5/1 | EtOH/dH2O (80–99.5 vol%) | 48 h | 25 °C | Ophthalmic | Chou et al. [58] | |
| Genipin | type A | 5–7% | EtOH | 3–7 days | 37 °C | Tissue engineering | Panzavolta et al. 2011 [76]; Chen et al. [77] |
| - | 0.1–0.5% | EtOH | 3 days | 37 °C | Angiogenesis in Tissue engineering | Del Gaudio et al. 2013 [78] | |
| - | 0.1–2% | EtOH/dH2O 70% | 19 h | - | Tissue engineering | Sisson et al. 2009 [70] | |
| Fish | 2% | EtOH/dH2O 90% | 1–5 days | - | Tissue engineering | Gomes et al. 2013 [54] | |
| Glutaraldehyde Vapor | type A | 25% | 10 mL dH2O | 6–12 h 1–2–3–4 days | - | Biomedical | Zhang et al. 2006 [79]; Vardiani et al. 2019 [80]; Chen et al. 2012 [77] |
| - | 0.5% | - | 19 h | - | Tissue engineering | Sisson et al. 2009 [70] | |
| type A | 25% | 20 mL dH2O | 2–4–6–8–10 min | - | Drug delivery | Laha et al. 2016 [81] | |
| type A | 10% | - | 2 h | - | Vascular tissue engineering | Y. Elsayed et al. 2016 [82] | |
| type A | 25% | - | 2 h | - | Vascular tissue engineering | Yahya Elsayed et al. 2016 [83] | |
| Fish | 2.5% | In situ | 8 h | - | Tissue engineering | Zhan et al. 2016 [84] | |
| Fish | 5% | 10 mL dH2O | 1–24 h | 40 °C | Tissue engineering/Skin regeneration | Gomes et al. 2013 [54,85] | |
| type A | 50% | 20 mL dH2O | 1–3 h | 37 °C | Wound healing | Rujitanaroj et al. 2008 [86] | |
| type A | 0.05% | In situ | - | - | Tissue engineering | Nguyen et al. 2010 [87] | |
| - | 50% | - | 3–24 h | - | Drug delivery | Lakshminarayanan et al. 2014 [88] | |
| - | 50% | - | 15–45–90–360 min | 25 °C | Tissue engineering | Wu et al. 2011 [89] | |
| Glutaraldehyde Solution | type B | 0.1–5% | 10 mL t-BuOH | 1 h crosslink + freeze-dry | 30 °C | Cartilage tissue regeneration | Skotak et al. 2010 [90]; Skotak et al. 2011 [91] |
| Glyceraldehyde | - | 0.1–0.5% | EtOH 70% | 19 h | Room temp | Tissue engineering | Sisson et al. 2009 [70] |
| Gelatin + PLLA | 0.5–0.7% | EtOH 70% | 19 h | Room temp | Nervous tissue regeneration | Binan et al. 2014 [92] | |
| 1,4-Butanediol Diglycidyl Ether (BDDGE) | type A | 2–4–6% | In situ | 24–48–72 h | Room temp | Skin regeneration | Dias et al. 2017 [93] |
| Hexamethylene Diisocyanate | type A | 1x, 5x, 10x ratio of isocyanate/amine | In situ | 3 h | Room temp | Tissue engineering | Kishan et al. 2015 [94] |
| Procyanidine | type A | 0.5–1–2–3–4–5% | EtOH 75% | 1–6 days | 20–30–40–50–60 °C | Tissue engineering | Chen et al. [77] |
| Oxidized Sucrose | type A | 0.1–0.5–1–2% | EtOH | 1–3–5 days | 37 °C | - | Jalaja et al. 2015 [95] |
| Gelatin | Parameters | Application | Reference | ||||
| Cross-Linker Concentration | Reaction Time | ||||||
| γ-Glycidoxypropyltrimethoxysilane (GPTMS) | type A | 92 μL/gramgelatin | In situ | Peripheral nerve regeneration | Tonda-Turo et al. 2013 [96]; Gnavi et al. 2015 [97] | ||
| Irgacure 2959 + UV Light | type A | 10% | 30 min (immersion + UV light) | Skin regeneration | Sun et al. 2017 [98] | ||
| GelMA + PCL | 0.015% | 20 min (immersion) 10 min/side (UV light) | Tissue engineering | Ferreira et al. 2017 [99] | |||
| type A | 10% | 2 h (immersion) 2–6–10 min/side (UV light) | Wound healing | Zhao et al. 2017 [100] | |||
| Gelatin | Parameters | Application | Reference | ||||
| UV | Gel + Poly (acrylic acid-g-azidoaniline) | Two UV lamp (18 W) during electrospinning process (in situ) | Tissue engineering | Lin and Tsai 2013 [101] | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campiglio, C.E.; Contessi Negrini, N.; Farè, S.; Draghi, L. Cross-Linking Strategies for Electrospun Gelatin Scaffolds. Materials 2019, 12, 2476. https://doi.org/10.3390/ma12152476
Campiglio CE, Contessi Negrini N, Farè S, Draghi L. Cross-Linking Strategies for Electrospun Gelatin Scaffolds. Materials. 2019; 12(15):2476. https://doi.org/10.3390/ma12152476
Chicago/Turabian StyleCampiglio, Chiara Emma, Nicola Contessi Negrini, Silvia Farè, and Lorenza Draghi. 2019. "Cross-Linking Strategies for Electrospun Gelatin Scaffolds" Materials 12, no. 15: 2476. https://doi.org/10.3390/ma12152476
APA StyleCampiglio, C. E., Contessi Negrini, N., Farè, S., & Draghi, L. (2019). Cross-Linking Strategies for Electrospun Gelatin Scaffolds. Materials, 12(15), 2476. https://doi.org/10.3390/ma12152476