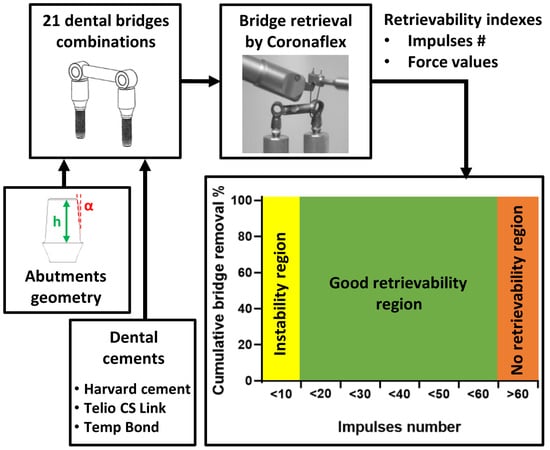
In Vitro Simulation of Dental Implant Bridges Removal: Influence of Luting Agent and Abutments Geometry on Retrievability
Abstract
:1. Introduction
2. Materials and Methods
2.1. Specimen Preparation
2.2. Test Setup
2.3. Test Protocol
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
- (1)
- The number of impulses, performed on the bridge with a clinical removal tool, is a more reliable index of retrievability, compared to the measured force.
- (2)
- The abutment height and taper angle have a higher influence on copings retentiveness than the luting agent.
- (3)
- The best compromise for stability and retrievability consists of a long, slightly tapered abutment, cemented with a temporary cement.
Author Contributions
Funding
Conflicts of Interest
References
- Zanetti, E.M.; Pascoletti, G.; Cali, M.; Bignardi, C.; Franceschini, G. Clinical assessment of dental implant stability during follow-up: What is actually measured, and perspectives. Biosensors 2018, 8, 68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wittneben, J.G.; Joda, T.; Weber, H.P.; Brägger, U. Screw retained vs. cement retained implant-supported fixed dental prosthesis. Periodontol. 2000 2017, 73, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Vigolo, P.; Givani, A.; Majzoub, Z.; Cordioli, G. Cemented versus screw-retained implant-supported single-tooth crowns: A 4-year prospective clinical study. Int. J. Oral Maxillofac. Implant. 2004, 19, 260–265. [Google Scholar]
- Manzella, C.; Bignardi, C.; Burello, V.; Carossa, S.; Schierano, G. Method to improve passive fit of frameworks on implant-supported prostheses: An in vitro study. J. Prosthet. Dent. 2016, 116, 52–58. [Google Scholar] [CrossRef]
- Assenza, B.; Scarano, A.; Leghissa, G.; Carusi, G.; Thams, U.; Roman, F.S.; Piattelli, A. Screw- vs cement-implant-retained restorations: An experimental study in the beagle. Part 1. screw and abutment loosening. J. Oral Implantol. 2005, 31, 242–246. [Google Scholar] [CrossRef]
- Manzella, C.; Burello, V.; Bignardi, C.; Carossa, S.; Schierano, G. A method to improve passive fit of frameworks on implant-supported prostheses: An in vivo study. Int. J. Prosthodont. 2013, 26, 577–579. [Google Scholar] [CrossRef] [Green Version]
- Shadid, R.; Sadaqa, N. A comparison between screw-and cement-retained implant prostheses. A literature review. J. Oral Implantol. 2012, 38, 298–307. [Google Scholar] [CrossRef] [Green Version]
- Menini, M.; Piccardo, P.; Baldi, D.; Dellepiane, E.; Pera, P. Morphological and chemical characteristics of different titanium surfaces treated by bicarbonate and glycine powder air abrasive systems. Implant Dent. 2015, 24, 47–56. [Google Scholar] [CrossRef] [Green Version]
- Breeding, L.C.; Dixon, D.L.; Bogacki, M.T.; Tietge, J.D. Use of luting agents with an implant system: Part I. J. Prosthet. Dent. 1992, 68, 737–741. [Google Scholar] [CrossRef]
- Addy, L.; Bartley, A.; Hayes, S. Crown and bridge disassembly—When, why and how. Dent. Update 2007, 34, 140–150. [Google Scholar] [CrossRef]
- Mansour, A.; Ercoli, C.; Graser, G.; Tallents, R.; Moss, M. Comparative evaluation of casting retention using the ITI solid abutment with six cements. Clin. Oral Implant. Res. 2002, 13, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Al Hamad, K.Q.; Al Rashdan, B.A.; Abu-Sitta, E.H. The effects of height and surface roughness of abutments and the type of cement on bond strength of cement-retained implant restorations. Clin. Oral Implant. Res. 2011, 22, 638–644. [Google Scholar] [CrossRef] [PubMed]
- Mehl, C.; Harder, S.; Schwarz, D.; Steiner, M.; Vollrath, O.; Kern, M. In vitro influence of ultrasonic stress, removal force preload and thermocycling on the retrievability of implant-retained crowns. Clin. Oral Implant. Res. 2012, 23, 930–937. [Google Scholar] [CrossRef]
- Mehl, C.; Harder, S.; Wolfart, M.; Kern, M.; Wolfart, S. Retrievability of implant-retained crowns following cementation. Clin. Oral Implants Res. 2008, 19, 1304–1311. [Google Scholar] [CrossRef]
- Akça, K.; Iplikçioğlu, H.; Cehreli, M.C. Comparison of uniaxial resistance forces of cements used with implant-supported crowns. Int. J. Oral Maxillofac. Implant. 2002, 17, 536–542. [Google Scholar]
- Schwarz, S.; Schröder, C.; Corcodel, N.; Hassel, A.J.; Rammelsberg, P. Retrospective comparison of semipermanent and permanent cementation of implant-supported single crowns and FDPs with regard to the incidence of survival and complications. Clin. Implant Dent. Relat. Res. 2012, 14, 151–158. [Google Scholar] [CrossRef]
- Naik, S.; Tredwin, C.J.; Nesbit, M.; Setchell, D.J.; Moles, D.R. The effect of engaging the screw access channel of an implant abutment with a cement-retained restoration. J. Prosthodont. 2009, 18, 245–248. [Google Scholar] [CrossRef]
- Ayad, M.F.; Johnston, W.M.; Rosenstiel, S.F. Influence of tooth preparation taper and cement type on recementation strength of complete metal crowns. J. Prosthet. Dent. 2009, 102, 354–361. [Google Scholar] [CrossRef]
- Bresciano, M.; Schierano, G.; Manzella, C.; Screti, A.; Bignardi, C.; Preti, G. Retention of luting agents on implant abutments of different height and taper. Clin. Oral Implants Res. 2005, 16, 594–598. [Google Scholar] [CrossRef]
- Gultekin, P.; Gultekin, B.A.; Aydin, M.; Yalcin, S. Cement selection for implant-supported crowns fabricated with different luting space settings. J. Prosthodont. 2013, 22, 112–119. [Google Scholar] [CrossRef]
- Dudley, J.E.; Richards, L.C.; Abbottf, J.R. Retention of cast crown copings cemented to implant abutments. Aust. Dent. J. 2008, 53, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Lugas, A.T.; Terzini, M.; Zanetti, E.M.; Schierano, G.; Manzella, C.; Baldi, D.; Bignardi, C.; Audenino, A.L. In vitro impact testing to simulate implant-supported prosthesis retrievability in clinical practice: Influence of cement and abutment geometry. Materials 2020, 13, 1749. [Google Scholar] [CrossRef] [Green Version]
- Schiessl, C.; Schaefer, L.; Winter, C.; Fuerst, J.; Rosentritt, M.; Zeman, F.; Behr, M. Factors determining the retentiveness of luting agents used with metal- and ceramic-based implant components. Clin. Oral Investig. 2013, 17, 1179–1190. [Google Scholar] [CrossRef] [PubMed]
- Schierano, G.; Manzella, C.; Menicucci, G.; Parrotta, A.; Zanetti, E.M.; Audenino, A.L. In vitro standardization of two different removal devices in cemented implant prosthesis. Clin. Oral Implants Res. 2016, 27, 1026–1030. [Google Scholar] [CrossRef] [PubMed]
- Bignardi, C.; Terzini, M.; Ciccola, A.R.; Audenino, A.L.; Zanetti, E.M.; Schierano, G. Reliability, learnability and efficiency of two tools for cement crowns retrieval in dentistry. Open Biomed. Eng. J. 2018, 12, 27–35. [Google Scholar] [CrossRef]
- Bernal, G.; Okamura, M.; Muñoz, C.A. The effects of abutment taper, length and cement type on resistance to dislodgement of cement-retained, implant-supported restorations. J. Prosthodont. 2003, 12, 111–115. [Google Scholar] [CrossRef]
- Heinemann, F.; Mundt, T.; Biffar, R. Retrospective evaluation of temporary cemented, tooth and implant supported fixed partial dentures. J. Cranio-Maxillofac. Surg. 2006, 34, 86–90. [Google Scholar] [CrossRef]
- Mehl, C.; Harder, S.; Steiner, M.; Vollrath, O.; Kern, M. Influence of cement film thickness on the retention of implant-retained crowns. J. Prosthodont. 2013, 22, 618–625. [Google Scholar] [CrossRef]
- Worni, A.; Gholami, H.; Marchand, L.; Katsoulis, J.; Mericske-Stern, R.; Enkling, N. Retrievability of implant-supported crowns when using three different cements: A controlled clinical trial. Int. J. Prosthodont. 2015, 28, 22–29. [Google Scholar] [CrossRef] [Green Version]
- Choi, K.H.; Da Son, K.B.; Lee, D.H.; Lee, K.B. Influence of abutment height and convergence angle on the retrievability of cement-retained implant prostheses with a lingual slot. J. Adv. Prosthodont. 2018, 10, 381–387. [Google Scholar] [CrossRef]
- Saleh, M.; Faruk, S.T. Enhancing retrievability of cement retained implant supported restorations. EC Dent. Sci. 2019, 3, 508–512. [Google Scholar]
- Emms, M.; Tredwin, C.J.; Setchell, D.J.; Moles, D.R. The effects of abutment wall height, platform size, and screw access channel filling method on resistance to dislodgement of cement-retained, implant-supported restorations. J. Prosthodont. 2007, 16, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Hill, E.E.; Lott, J. A Clinically focused discussion of luting materials. Aust. Dent. J. 2011, 56, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Donovan, T.E.; Cho, G.C. Contemporary evaluation of dental cements. Compend. Contin. Educ. Dent. 1999, 20, 197–199. [Google Scholar]
- Burbano, M.; Wilson, T.; Valderrama, P.; Blansett, J.; Wadhwani, C.; Choudhary, P.; Rodriguez, L.; Rodrigues, D. Characterization of cement particles found in peri-implantitis–affected human biopsy specimens. Int. J. Oral Maxillofac. Implants 2015, 30, 1168–1173. [Google Scholar] [CrossRef] [Green Version]
- Mehl, C.; Ali, S.; El Bahra, S.; Harder, S.; Vollrath, O.; Kern, M. Is there a correlation between tensile strength and retrievability of cemented implant-retained crowns using artificial aging? Int. J. Prosthodont. 2016, 29, 83–90. [Google Scholar] [CrossRef]
- Lennartz, A.; Dohmen, A.; Bishti, S.; Fischer, H.; Wolfart, S. Retrievability of implant-supported zirconia restorations cemented on zirconia abutments. J. Prosthet. Dent. 2018, 120, 740–746. [Google Scholar] [CrossRef]








| Bridge | Abutment 1 Geometry | Abutment 2 Geometry |
|---|---|---|
| 1 | 5 mm-0° | 5 mm-0° |
| 2 | 7 mm-0° | 7 mm-0° |
| 3 | 7 mm-2° | 7 mm-2° |
| 4 | 5 mm-2° | 5 mm-4° |
| 5 | 5 mm-0° | 5 mm-4° |
| 6 | 7 mm-2° | 7 mm-4° |
| 7 | 7 mm-0° | 7 mm-4° |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lugas, A.T.; Terzini, M.; Zanetti, E.M.; Schierano, G.; Manzella, C.; Baldi, D.; Bignardi, C.; Audenino, A.L. In Vitro Simulation of Dental Implant Bridges Removal: Influence of Luting Agent and Abutments Geometry on Retrievability. Materials 2020, 13, 2797. https://doi.org/10.3390/ma13122797
Lugas AT, Terzini M, Zanetti EM, Schierano G, Manzella C, Baldi D, Bignardi C, Audenino AL. In Vitro Simulation of Dental Implant Bridges Removal: Influence of Luting Agent and Abutments Geometry on Retrievability. Materials. 2020; 13(12):2797. https://doi.org/10.3390/ma13122797
Chicago/Turabian StyleLugas, Andrea T., Mara Terzini, Elisabetta M. Zanetti, Gianmario Schierano, Carlo Manzella, Domenico Baldi, Cristina Bignardi, and Alberto L. Audenino. 2020. "In Vitro Simulation of Dental Implant Bridges Removal: Influence of Luting Agent and Abutments Geometry on Retrievability" Materials 13, no. 12: 2797. https://doi.org/10.3390/ma13122797
APA StyleLugas, A. T., Terzini, M., Zanetti, E. M., Schierano, G., Manzella, C., Baldi, D., Bignardi, C., & Audenino, A. L. (2020). In Vitro Simulation of Dental Implant Bridges Removal: Influence of Luting Agent and Abutments Geometry on Retrievability. Materials, 13(12), 2797. https://doi.org/10.3390/ma13122797