Effect of UV and Gamma Irradiation Sterilization Processes in the Properties of Different Polymeric Nanoparticles for Biomedical Applications
Abstract
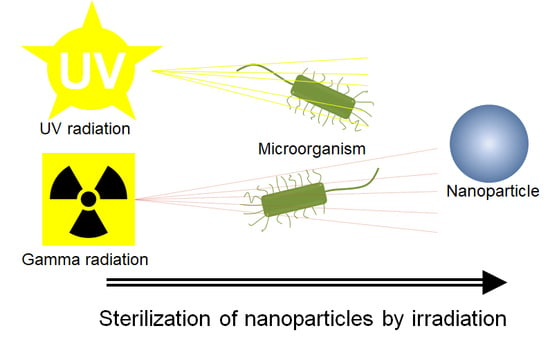
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Nanoparticle Systems
2.3. Sterilization Methods
2.4. Microbiological Evaluation
2.5. Physicochemical Characterization
2.5.1. Particle Size and Zeta-Potential Measurement
2.5.2. Scanning Electron Microscopy (SEM)
2.5.3. Fourier Transform-InfraRed (FTIR) Spectroscopy
2.5.4. Thermogravimetric Analysis (TGA)
2.5.5. Differential Scanning Calorimetry (DSC)
2.6. Biological Characterization
2.6.1. Cell culture
2.6.2. Cell Viability Assay
2.6.3. Immunofluorescence and Confocal Microscopy Analysis
3. Results and Discussion
3.1. NP Manufacture and Physicochemical Characteristics
3.2. Microbiological Evaluation Before and After Sterilization
3.3. Influence of Sterilization on the Physical Characteristics of Nanoparticles
3.4. Influence of Sterilization on the Chemical Characteristics of NP
3.4.1. Fourier-Transform Infrared Spectroscopy (FTIR)
3.4.2. Thermogravimetric Analysis (TGA)
3.4.3. Differential Scanning Calorimetry (DSC)
3.5. Biological Characterization
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bathia, S. Nanoparticles Types, Classification, Characterization, Fabrication Methods. In Natural Polymer Drug Delivery Systems; Springer: Cham, Switzerland, 2016; ISBN 9783319411293. [Google Scholar]
- Grabrucker, A.M.; Ruozi, B.; Belletti, D.; Pederzoli, F.; Forni, F.; Vandelli, M.A.; Tosi, G. Nanoparticle transport across the blood brain barrier. Tissue Barriers 2016, 4, e1153568. [Google Scholar] [CrossRef] [Green Version]
- Saraiva, C.; Praça, C.; Ferreira, R.; Santos, T.; Ferreira, L.; Bernardino, L. Nanoparticle-mediated brain drug delivery: Overcoming blood—Brain barrier to treat neurodegenerative diseases. J. Control. Release 2016, 235, 34–47. [Google Scholar] [CrossRef] [Green Version]
- Patra, J.K.; Das, G.; Fraceto, L.F.; Campos, E.V.; del Pilar Rodriguez-Torres, M.; Acosta-Torres, L.S.; Diaz-Torres, L.A.; Grillo, R.; Swamy, M.K.; Sharma, S.; et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018, 16, 71. [Google Scholar] [CrossRef] [Green Version]
- Re, F.; Gregori, M.; Masserini, M. Nanotechnology for neurodegenerative disorders. Maturitas 2012, 73, 45–51. [Google Scholar] [CrossRef]
- Escalona-Rayo, O.; Fuentes-Vázquez, P.; Leyva-Gómez, G.; Cisneros, B.; Villalobos, R.; Magaña, J.J.; Quintanar-Guerrero, D. Nanoparticulate strategies for the treatment of polyglutamine diseases by halting the protein aggregation process†. Drug Dev. Ind. Pharm. 2017, 43, 871–888. [Google Scholar] [CrossRef] [PubMed]
- Ulery, B.D.; Nair, L.S.; Laurencin, C.T. Biomedical applications of biodegradable polymers. J. Polym. Sci. Part B Polym. Phys. 2011, 49, 832–864. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mundargi, R.C.; Babu, V.R.; Rangaswamy, V.; Patel, P.; Aminabhavi, T.M. Nano/micro technologies for delivering macromolecular therapeutics using poly(d,l-lactide-co-glycolide) and its derivatives. J. Control. Release 2008, 125, 193–209. [Google Scholar] [CrossRef]
- Nazila, K.; Yameen, B.; Wu, J.; Farokhzad, O.C. Nanoparticles: Mechanisms of Controlling Drug Release Nazila. Chem. Rev. 2016, 116, 2602–2663. [Google Scholar]
- Vetten, M.A.; Yah, C.S.; Singh, T.; Gulumian, M. Challenges facing sterilization and depyrogenation of nanoparticles: Effects on structural stability and biomedical applications. Nanomed. Nanotechnol. Biol. Med. 2014, 10, 1391–1399. [Google Scholar] [CrossRef] [PubMed]
- Memisoglu-Bilensoy, E.; Hincal, A.A. Sterile, injectable cyclodextrin nanoparticles: Effects of gamma irradiation and autoclaving. Int. J. Pharm. 2006, 311, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Masson, V.; Maurin, F.; Fessi, H.; Devissaguet, J.P. Influence of sterilization processes on poly (& -caprolactone ) nanospheres. Biomaterials 1997, 18, 327–335. [Google Scholar] [PubMed]
- Bozdag, S.; Dillen, K.; Vandervoort, J.; Ludwig, A. The effect of freeze-drying with different cryoprotectants and gamma-irradiation sterilization on the characteristics of ciprofloxacin HCl-loaded poly(d,l-lactide-glycolide) nanoparticles. J. Pharm. Pharmacol. 2005, 57, 699–707. [Google Scholar] [CrossRef] [PubMed]
- Shahabi, S.; Najafi, F.; Majdabadi, A.; Hooshmand, T.; Haghbin Nazarpak, M.; Karimi, B.; Fatemi, S.M. Effect of gamma irradiation on structural and biological properties of a PLGA-PEG-hydroxyapatite composite. Sci. World J. 2014, 2014, 420616. [Google Scholar] [CrossRef] [PubMed]
- Kroll, C.; Borchert, H.; Kissel, T. Tetracycline-HCl-loaded poly (dl-lactide-co-glycolide) microspheres prepared by a spray drying technique: Influence of g-irradiation on radical formation and polymer degradation. J. Control. Release 1999, 59, 23–32. [Google Scholar]
- Mohr, D.; Wolff, M.; Kissel, T. Gamma irradiation for terminal sterilization of 17 b-estradiol loaded poly-(d,l-lactide-co-glycolide) microparticles. J. Mod. Food Pharm. 1999, 61, 203–217. [Google Scholar]
- Montanari, L.; Cilurzo, F.; Valvo, L.; Faucitano, A.; Buttafava, A.; Groppo, A. Gamma irradiation effects on stability of containing clonazepam. J. Control Release 2001, 75, 317–330. [Google Scholar] [CrossRef]
- Zhao, L.; Mei, S.; Wang, W.; Chu, P.K.; Wu, Z.; Zhang, Y. The role of sterilization in the cytocompatibility of titania nanotubes. Biomaterials 2010, 31, 2055–2063. [Google Scholar] [CrossRef]
- Dutz, S.; Wojahn, S.; Gräfe, C.; Weidner, A.; Clement, J. Influence of Sterilization and Preservation Procedures on the Integrity of Serum Protein-Coated Magnetic Nanoparticles. Nanomaterials 2017, 7, 453. [Google Scholar] [CrossRef] [Green Version]
- Galante, R.; Rediguieri, C.F.; Kikuchi, I.S.; Vasquez, P.A.S.; Colaço, R.; Serro, A.P.; Pinto, T.J.A. About the sterilization of chitosan hydrogel nanoparticles. PLoS ONE 2016, 11, e0168862. [Google Scholar] [CrossRef]
- Abdelwahed, W.; Degobert, G.; Fessi, H. A pilot study of freeze drying of poly(epsilon-caprolactone) nanocapsules stabilized by poly(vinyl alcohol): Formulation and process optimization. Int. J. Pharm. 2006, 309, 178–188. [Google Scholar] [CrossRef]
- Voigt, N.; Henrich-Noack, P.; Kockentiedt, S.; Hintz, W.; Tomas, J.; Sabel, B.A. Surfactants, not size or zeta-potential influence blood-brain barrier passage of polymeric nanoparticles. Eur. J. Pharm. Biopharm. 2014, 87, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Shilo, M.; Sharon, A.; Baranes, K.; Motiei, M.; Lellouche, J.M.; Popovtzer, R. The effect of nanoparticle size on the probability to cross the blood—Brain barrier: An in-vitro endothelial cell model. J. Nanobiotechnol. 2015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, V.R.; Agrawal, Y.K. Nanosuspension: An approach to enhance solubility of drugs. J. Adv. Pharm. Technol. Res. 2011, 2, 81–87. [Google Scholar] [PubMed]
- Petros, R.A.; Desimone, J.M. Strategies in the design of nanoparticles for therapeutic applications. Nat. Rev. Drug Discov. 2010, 9, 615–627. [Google Scholar] [CrossRef]
- Jallouk, A.P.; Palekar, R.U.; Pan, H.; Schlesinger, P.H.; Wickline, S.A. Modifications of Natural Peptides for Nanoparticle and Drug Design. In Advances in Protein Chemistry and Structural Biology; Academic Press Inc.: Cambridge, MA, USA, 2015; Volume 98, pp. 57–91. [Google Scholar]
- Konan, Y.N.; Gurny, R.; Alle, E. Preparation and characterization of sterile and freeze-dried sub-200 nm nanoparticles. Int. J. Pharm. 2002, 233, 239–252. [Google Scholar] [CrossRef]
- Tsukada, Y.; Hara, K.; Bando, Y.; Huang, C.C.; Kousaka, Y.; Kawashima, Y.; Morishita, R.; Tsujimoto, H. Particle size control of poly (dl-lactide-co-glycolide ) nanospheres for sterile applications. Int. J. Pharm. 2009, 370, 196–201. [Google Scholar] [CrossRef]
- Meunier, S.M.; Sasges, M.R.; Aucoin, M.G. Evaluating ultraviolet sensitivity of adventitious agents in biopharmaceutical manufacturing. J. Ind. Microbiol. Biotechnol. 2017, 44, 893–909. [Google Scholar] [CrossRef]
- Rastogi, R.P.; Kumar, A.; Tyagi, M.B. Molecular mechanisms of ultraviolet radiation-induced DNA damage and repair. J. Nucleic Acids 2010, 2010. [Google Scholar] [CrossRef] [Green Version]
- Hasanain, F.; Guenther, K.; Mullett, W.M.; Craven, E. Gamma Sterilization of Pharmaceuticals—A Review of the Irradiation of Excipients, Active Pharmaceutical Ingredients, and Final Drug Product Formulations. PDA J. Pharm. Sci. Technol. 2014, 68, 113–137. [Google Scholar] [CrossRef]
- Zhang, S.; Yu, H. Radiation-induced degradation of polyvinyl alcohol in aqueous solutions. Water Res. 2004, 38, 309–316. [Google Scholar] [CrossRef]
- González-Torres, M.; Leyva-Gómez, G.; Rivera, M.; Krötzsch, E.; Rodríguez-Talavera, R.; Rivera, A.L.; Cabrera-Wrooman, A. Biological activity of radiation-induced collagen–polyvinylpyrrolidone–PEG hydrogels. Mater. Lett. 2018, 214, 224–227. [Google Scholar] [CrossRef]
- Leyva-Gómez, G.; Santillan-Reyes, E.; Lima, E.; Madrid-Martínez, A.; Krötzsch, E.; Quintanar-Guerrero, D.; Garciadiego-Cázares, D.; Martínez-Jiménez, A.; Hernández Morales, M.; Ortega-Peña, S.; et al. A novel hydrogel of poloxamer 407 and chitosan obtained by gamma irradiation exhibits physicochemical properties for wound management. Mater. Sci. Eng. C 2017, 74, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.; Punshon, G.; Darbyshire, A.; Seifalian, A.M. Effects of sterilization treatments on bulk and surface properties of nanocomposite biomaterials. J. Biomed. Mater. Res.—Part B Appl. Biomater. 2013, 101, 1182–1190. [Google Scholar] [CrossRef]
- Dai, Z.; Ronholm, J.; Tian, Y.; Sethi, B.; Cao, X. Sterilization techniques for biodegradable scaffolds in tissue engineering applications. J. Tissue Eng. 2016, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elzein, T.; Nasser-Eddine, M.; Delaite, C.; Bistac, S.; Dumas, P. FTIR study of polycaprolactone chain organization at interfaces. J. Colloid Interface Sci. 2004, 273, 381–387. [Google Scholar] [CrossRef] [PubMed]
- El-Hefian, E.A.; Nasef, M.M.; Yahaya, A.H. The preparation and characterization of Chitosan/Poly (Vinyl Alcohol) blended films. E-J. Chem. 2010, 7, 1212–1219. [Google Scholar] [CrossRef]
- Malferrari, M.; Nalepa, A.; Venturoli, G.; Francia, F.; Lubitz, W.; Möbius, K.; Savitsky, A. Structural and dynamical characteristics of trehalose and sucrose matrices at different hydration levels as probed by FTIR and high-field EPR. Phys. Chem. Chem. Phys. 2014, 16, 9831–9848. [Google Scholar] [CrossRef] [Green Version]
- Márquez, M.J.; Romani, D.; Díaz, S.B.; Brandán, S.A. Structural and vibrational characterization of anhydrous and dihydrated species of trehalose based on the FTIR and FTRaman spectra and DFT calculations. J. King Saud Univ.—Sci. 2018, 30, 229–249. [Google Scholar] [CrossRef]
- Tan, H.; Ye, J. Surface morphology and in vitro release performance of double-walled PLLA/PLGA microspheres entrapping a highly water-soluble drug. Appl. Surf. Sci. 2008, 255, 353–356. [Google Scholar] [CrossRef]
- Wang, Y.; Li, P.; Kong, L. Chitosan-Modified PLGA Nanoparticles with Versatile Surface for Improved Drug Delivery. AAPS PharmSciTech 2013, 14, 585–592. [Google Scholar] [CrossRef] [Green Version]
- Burger, A.; Henck, J.O.; Hetz, S.; Rollinger, J.M.; Weissnicht, A.A.; Stöttner, H. Energy/temperature diagram and compression behavior of the polymorphs of D-mannitol. J. Pharm. Sci. 2000, 89, 457–468. [Google Scholar] [CrossRef]
- Mohamed, A.; Finkenstadt, V.L.; Gordon, S.H.; Biresaw, G.; Palmquist Debra, E.; Rayas-Duarte, P. Thermal properties of PCL/gluten bioblends characterized by TGA, DSC, SEM, and infrared-PAS. J. Appl. Polym. Sci. 2008, 110, 3256–3266. [Google Scholar] [CrossRef]
- Persenaire, O.; Alexandre, M.; Degée, P.; Dubois, P. Mechanisms and kinetics of thermal degradation of poly(ε-caprolactone). Biomacromolecules 2001, 2, 288–294. [Google Scholar] [CrossRef] [PubMed]
- Jeong Kim, S.; Jun Park, S.; Young Kim, I.; Hee Lee, Y.; Kim, S.I. Thermal characteristics of poly(vinyl alcohol) and poly(vinylpyrrolidone) IPNs. J. Appl. Polym. Sci. 2002, 86, 1844–1847. [Google Scholar] [CrossRef]
- Guirguis, O.W.; Moselhey, M.T.H. Thermal and structural studies of poly (vinyl alcohol) and hydroxypropyl cellulose blends. Nat. Sci. 2012, 4, 57–67. [Google Scholar] [CrossRef] [Green Version]
- Yang, H.; Xu, S.; Jiang, L.; Dan, Y. Thermal decomposition behavior of poly (vinyl alcohol) with different hydroxyl content. J. Macromol. Sci. Part B Phys. 2012, 51, 464–480. [Google Scholar] [CrossRef]
- Lin, S.-Y.; Chien, J.-L. In vitro simulation of solid-solid dehydration, rehydration, and solidification of trehalose dihydrate using thermal and vibrational spectroscopic techniques. Pharm. Res. 2003, 20, 1926–1931. [Google Scholar] [CrossRef]
- D’Avila Carvalho Erbetta, C. Synthesis and Characterization of Poly(d,l-Lactide-co-Glycolide) Copolymer. J. Biomater. Nanobiotechnol. 2012, 3, 208–225. [Google Scholar] [CrossRef]
- Palacios, J.; Albano, C.; González, G.; Castillo, R.V.; Karam, A.; Covis, M. Characterization and thermal degradation of poly(d, l-lactide-co-glycolide) composites with nanofillers. Polym. Eng. Sci. 2013, 53, 1414–1429. [Google Scholar] [CrossRef]
- Lawrence, J.M.; Singhal, S.; Bhatia, B.; Keegan, D.J.; Reh, T.A.; Luthert, P.J.; Khaw, P.T.; Limb, G.A. MIO-M1 Cells and Similar Müller Glial Cell Lines Derived from Adult Human Retina Exhibit Neural Stem Cell Characteristics. Stem Cells 2007, 25, 2033–2043. [Google Scholar] [CrossRef]
- Karakirova, Y.; Yordanov, N. Mannitol as a radiation sensitive material for electron paramagnetic resonance dosimetry. Bulg. Chem. Commun. 2015, 47, 144–148. [Google Scholar]
- Yoshinaga, K.; Yoshioka, H.; Kurosaki, H.; Hirasawa, M.; Uritani, M.; Hasegawa, K. Protection by trehalose of DNA from Radiation Damage. Biosci. Biotechnol. Biochem. 1997, 61, 160–161. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, M.R.; Foroughizadeh, M.M.; Mozdarani, H. Evaluation of the role of mannitol in radaioprotection of amifostine TT-. Int.-J.-Radiat.-Res. 2003, 1, 151–155. [Google Scholar]
- Maksimenko, O.; Pavlov, E.; Toushov, E.; Molin, A.; Stukalov, Y.; Prudskova, T.; Feldman, V.; Kreuter, J.; Gelperina, S. Radiation sterilisation of doxorubicin bound to poly(butyl cyanoacrylate) nanoparticles. Int. J. Pharm. 2008, 356, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-segura, A.; Nehme, J.; Demaria, M. Hallmarks of Cellular Senescence. Trends Cell Biol. 2018, 28, 436–453. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.; Li, H.; Wu, D.; Li, B.; Liu, C.; Guo, W.; Min, J.; Hu, M.; Zhao, Y.; Yang, Q. Oxidative damage to human parametrial ligament fibroblasts induced by mechanical stress. Mol. Med. Rep. 2015, 12, 5342–5348. [Google Scholar] [CrossRef] [PubMed]






| Sample | Size (nm) | PDI | Zeta Potential (mV) |
|---|---|---|---|
| PCL/PVA NP | 228.8 ± 11.60 | 0.050 ± 0.10 | −14.47 ± 1.76 |
| PCL/PVA NP UV | 232.5 ± 5.70 | 0.040 ± 0.06 | −14.07 ± 0.25 |
| PCL/PVA NP 5 kGy | 213.6 ± 2.21 * | 0.080 ± 0.03 | −18.53 ± 0.78 * |
| PCL/PVA NP 10 kGy | 208.8 ± 1.37 ** | 0.110 ± 0.05 ** | −22.90 ± 0.66 ** |
| PLGA/PVA NP | 243.1 ± 3.06 | 0.064 ± 0.02 | −17.00 ± 0.17 |
| PLGA/PVA NP UV | 240.0 ± 1.55 | 0.070 ± 0.05 | −18.16 ± 0.58 |
| PLGA/PVA NP 5 kGy | 209.6 ± 1.95 *** | 0.046 ± 0.02 | −17.00 ± 0.50 |
| PLGA/PVA NP 10 kGy | 217.0 ± 1.96 *** | 0.028 ± 0.03 ** | −17.50 ± 0.40 |
| Sample | T1 (°C) | T2 (°C) | T3 (°C) | T4 (°C) |
|---|---|---|---|---|
| PCL | 67.5 | - | - | - |
| PVA | 195.5 | - | - | - |
| D-(+)-trehalose dehydrate | 100.0 | 212.0 | - | - |
| PCL/PVA NP | 56.0 | 99.5 | 211.0 | - |
| PCL/PVA NP UV | 56.7 | 99.7 | 212.0 | - |
| PCL/PVA NP 5 kGy | 54.8 | 97.8 | 130.0 | 212.0 |
| PCL/PVA NP 10 kGy | 55.8 | 98.5 | 130.0 | 212.0 |
| PLGA | 50.4 | 241.4 | - | - |
| Mannitol | 167.0 | - | - | - |
| PLGA/PVA NP | 165.3 | - | - | - |
| PLGA/PVA NP UV | 165.5 | - | - | - |
| PLGA/PVA NP 5 kGy | 165.1 | - | - | - |
| PLGA/PVA NP 10 kGy | 163.6 | - | - | - |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tapia-Guerrero, Y.S.; Del Prado-Audelo, M.L.; Borbolla-Jiménez, F.V.; Giraldo Gomez, D.M.; García-Aguirre, I.; Colín-Castro, C.A.; Morales-González, J.A.; Leyva-Gómez, G.; Magaña, J.J. Effect of UV and Gamma Irradiation Sterilization Processes in the Properties of Different Polymeric Nanoparticles for Biomedical Applications. Materials 2020, 13, 1090. https://doi.org/10.3390/ma13051090
Tapia-Guerrero YS, Del Prado-Audelo ML, Borbolla-Jiménez FV, Giraldo Gomez DM, García-Aguirre I, Colín-Castro CA, Morales-González JA, Leyva-Gómez G, Magaña JJ. Effect of UV and Gamma Irradiation Sterilization Processes in the Properties of Different Polymeric Nanoparticles for Biomedical Applications. Materials. 2020; 13(5):1090. https://doi.org/10.3390/ma13051090
Chicago/Turabian StyleTapia-Guerrero, Y. S., M. L. Del Prado-Audelo, F. V. Borbolla-Jiménez, D. M. Giraldo Gomez, I. García-Aguirre, C. A. Colín-Castro, J. A. Morales-González, G. Leyva-Gómez, and J. J. Magaña. 2020. "Effect of UV and Gamma Irradiation Sterilization Processes in the Properties of Different Polymeric Nanoparticles for Biomedical Applications" Materials 13, no. 5: 1090. https://doi.org/10.3390/ma13051090
APA StyleTapia-Guerrero, Y. S., Del Prado-Audelo, M. L., Borbolla-Jiménez, F. V., Giraldo Gomez, D. M., García-Aguirre, I., Colín-Castro, C. A., Morales-González, J. A., Leyva-Gómez, G., & Magaña, J. J. (2020). Effect of UV and Gamma Irradiation Sterilization Processes in the Properties of Different Polymeric Nanoparticles for Biomedical Applications. Materials, 13(5), 1090. https://doi.org/10.3390/ma13051090