Dental Sealant Composition-Retention Assessment in Young Permanent Molars
Abstract
:1. Introduction
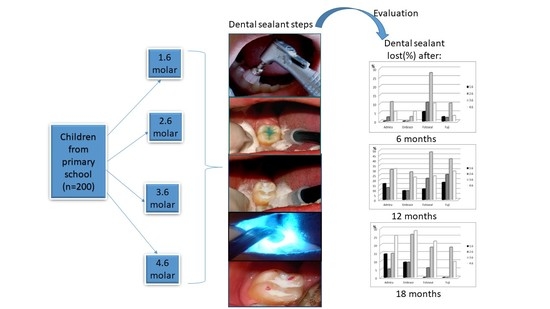
2. Materials and Methods
- Normal, healthy children;
- Availability for the duration of the study;
- Satisfactory dental care performed at home;
- The willingness of the patient to accept the treatment.
- Enamel dysplasia, MIH;
- A child with compromised health;
- Long-term medication affecting the salivary flow;
- Adverse reaction reported to any dental material;
- Uncooperative child.
2.1. Sealing Procedures.
- Group I–III: the occlusal mesio-distal grooves were etched with 37% phosphoric acid gel for 20 s (Vococid©, Voco Corporation, Cuxhaven, Germany), rinsed with water spray for 20 s and dried with a gentle air stream for 10 s. One layer of resin-based sealant was applied using a special applicator with a light brushing motion, and then light cured for 20 s using LED Elipar Deep Cure-L© (3M, St. Paul, MN, USA)
- Group IV: the occlusal mesio-distal grooves were conditioned with GC Cavity Conditioner©, GC America INC, Alsip, IL, USA (20% polyacrylic acid and 3% aluminum chloride hexahydrate) for 10s, then washed for 20 s and dried but not desiccated with a gentle air stream for 3 s, in order to obtain a moist surface. The resin-modified glass ionomer sealant (RMGI) (GC Fuji Triage®, GC America INC, Alsip, IL, USA) was prepared according to the manufacturer’s recommendations and one layer was applied with an explorer, and then light cured for 20s using LED Elipar DeepCure-L© (3M, St. Paul, MN, USA).
- Sealant completely preserved;
- Incomplete or complete missing material, without caries;
- Incomplete or complete missing material, with caries.
2.2. Data Analysis
3. Results
3.1. Sealant Retention in Relation to Dental Material Characteristics.
3.2. Sealant Retention, Dependent on the Topography of the Tooth and Patient Age (When the Tooth Was Sealed for the First Time).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Manton, D.J. Child dental caries-A global problem of inequality. EClinicalMedicine 2018, 1, 3–4. [Google Scholar] [CrossRef] [Green Version]
- Kassebaum, N.J.; Bernabe, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.; Marcenes, W. Global burden of untreated caries: A systematic review and metaregression. J. Dent. Res. 2015, 94, 650–658. [Google Scholar] [CrossRef]
- Papageorgiou, S.N.; Dimitraki, D.; Kotsanos, N.; Bekes, K.; van Waes, H. Performance of pit and fissure sealants according to tooth characteristics: A systematic review and meta-analysis. J. Dent. 2017, 66, 8–17. [Google Scholar] [CrossRef] [Green Version]
- Kantovitz, K.R.; Pascon, F.N.; Nociti Jr., F.H.; Tabchoury, C.P.; Puppin-Rontani, R.M. Inhibition of enamel mineral loss by fissure sealant: An in-situ study. J. Dent. 2013, 41, 42–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cocco, A.R.; Cuevas-Suarez, C.E.; Liu, Y.; Lund, R.G.; Piva, E.; Hwang, G. Anti-biofilm activity of a novel pit and fissure self-adhesive sealant modified with metallic monomers. Biofouling 2020, 36, 245–255. [Google Scholar] [CrossRef]
- Garcia, I.M.; Rodrigues, S.B.; de Souza Balbinot, G.; Visioli, F.; Leitune, V.C.B.; Collares, F.M. Quaternary ammonium compound as antimicrobial agent in resin-based sealants. Clin. Oral Investig. 2020, 24, 777–784. [Google Scholar] [CrossRef]
- Nupur, N.; Ullal, N.A.; Khandelwal, V. A 1-year clinical evaluation of fissure sealants on permanent first molars. Contemp. Clin. Dent. 2012, 3, 54–59. [Google Scholar]
- Feigal, R.J. The use of pit and fissure sealants. Pediatr. Dent. 2002, 24, 415–422. [Google Scholar]
- Bagheri, M.; Pilecki, P.; Sauro, S.; Sherriff, M.; Watson, T.F.; Hosey, M.T. An in vitro investigation of pre-treatment effects before fissure sealing. Int. J. Paediatr. Dent. 2017, 27, 514–522. [Google Scholar] [CrossRef]
- Tudoroniu, C.; Popa, M.; Iacob, S.M.; Pop, A.L.; Nasui, B.A. Correlation of caries prevalenca oral health behavior and sweets nutritional habits among 10 to 19-year-old Cluj-Napoca Romania adolescents. Int. J. Environ. Res. Public Health 2020, 17, 6923. [Google Scholar] [CrossRef] [PubMed]
- Lucaciu, P.O.; Mester, A.; Constantin, I.; Orban, N.; Cosma, L.; Candrea, S.; Mesaros, A.S. A WHO Pathfinder survey of dental caries in 6- and 12-Year-Old Transylvanian children and the possible correlation with their family background, oral-health behavior, and the intake of sweets. Int. J. Environ. Res. Public Health 2020, 17, 4180. [Google Scholar] [CrossRef]
- Fontana, M.; Gonzalez-Cabezas, C. Evidence-based dentistry caries risk assessment and disease management. Dent. Clin. N. Am. 2019, 63, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Preetha, V.; Shashikiran, N.; Reddy, V. Comparison of antibacterial properties of two fluoride-releasing and a nonfluoride-releasing pit and fissure sealants. J. Indian Soc. Pedod. Prev. Dent. 2007, 25, 133–136. [Google Scholar]
- Naorungroj, S.; Wei, H.H.; Arnold, R.R.; Swift, E.J., Jr.; Walter, R. Antibacterial surface properties of fluoride-containing resin-based sealants. J. Dent. 2010, 38, 387–391. [Google Scholar] [CrossRef]
- Pagano, S.; Coniglio, M.; Valenti, C.; Negri, P.; Lombardo, G.; Costanzi, E.; Cianetti, S.; Montaseri, A.; Marinucci, L. Biological effects of resin monomers on oral cell populations: Descriptive analysis of literature. Eur. J. Paediatr. Dent. 2019, 20, 224–232. [Google Scholar] [PubMed]
- Alves, L.S.; Giongo, F.C.M.D.S.; Mua, B.; Martins, V.B.; Barbachan e Silva, B.; Qvist, V.; Maltz, M. A randomized clinical trial on the sealing of occlusal carious lesions: 3–4-year results. Braz. Oral Res. 2017, 31, e44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poulsen, S.; Laurberg, L.; Vaeth, M.; Jensen, U.; Haubek, D. A field trial of resin-based and glass ionomer fissure sealants: Clinical and radiographic assessment of caries. Community Dent. Oral Epidemiol. 2006, 34, 36–40. [Google Scholar] [CrossRef]
- Eramo, S.; Baldi, M.; Marci, M.C.; Monaco, A. Histopathological and therapeutical aspects of cervical lesions. Minerva Stomatol. 2003, 52, 69–74. [Google Scholar]
- Fontana, M.; Platt, J.A.; Eckert, G.J.; Gonzalez-Cabezas, C.; Yoder, K.; Zero, D.T.; Ando, M.; Soto-Rojas, A.E.; Peters, M.C. Monitoring of sound and carious surfaces under sealants over 44 months. J. Dent. Res. 2014, 93, 1070–1075. [Google Scholar] [CrossRef] [Green Version]
- Karaman, E.; Yazici, A.R.; Baseren, M.; Gorucu, J. Comparison of acid versus laser etching on the clinical performance of a fissure sealant: 24-month results. Oper. Dent. 2013, 38, 151–158. [Google Scholar] [CrossRef] [Green Version]
- Ahovuo-Saloranta, A.; Forss, A.; Hiiri, A.; Nordblad, A.; Makela, M. Pit and fissure sealants versus fluoride varnishes for preventing dental decay in the permanent teeth of children and adolescents. Cochrane Database Syst. Rev. 2016, CD003067. [Google Scholar] [CrossRef]
- Furtos, G.; Cosma, V.; Prejmerean, C.; Moldovan, M.; Brie, M.; Colceriu, A.; Vezsenyi, L.; Silaghi-Dumitrescu, L.; Sarbu, C. Fluoride release from dental resin composites. Mater. Sci. Eng. C 2005, 25, 231–236. [Google Scholar] [CrossRef]
- Muntean, A.; Mesaros, A.; Festila, D.; Moldovan, M.; Mesaros, M. In vitro microleakage evaluation around three types of dental sealants. Mater. Plast. 2016, 53, 166–169. [Google Scholar]
- Oulis, C.; Berdouses, E.; Mamai-Homata, E.; Polychronopoulou, A. Prevalence of sealants in relation to dental caries on the permanent molars of 12 and 15-year-old Greek adolescents. A national pathfinder surveys. BMC Public Health 2011, 11, 100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delbem, A.C.B.; Brighenti, F.L.; Vieira, A.E.d.M.; Cury, J.A. In vitro comparison of the cariostatic effect between topical application of fluoride gels and fluoride toothpaste. J. Appl. Oral Sci. 2004, 12, 121–126. [Google Scholar] [CrossRef]
- Habib, E.; Wang, R.; Zhu, X. Correlation of resin viscosity and monomer conversion to filler particle size in dental composite. Dent Mater. 2018, 34, 1501–1508. [Google Scholar] [CrossRef] [PubMed]
- Khosravani, M.R. Mechanical behavior of restorative dental composites under various loading conditions. J. Mech. Behav. Biomed. Mater. 2019, 93, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Cury, J.A.; de Oliveira, B.H.; dos Santos, A.P.; Tenuta, L.M. Are fluoride releasing dental materials clinically effective on caries control? Dent. Mater. 2016, 32, 323–333. [Google Scholar] [CrossRef] [PubMed]
- Kucukyilmaz, E.; Savas, S. Evaluation of different fissure sealant materials and flowable composites used as pitand-fissure sealants: A 24-month clinical trial. Pediatr. Dent. 2015, 37, 468–473. [Google Scholar]
- Cvikl, B.; Moritz, A.; Bekes, K. Pit and fissure sealants-A comprehensive review. Dent. J. 2018, 6, 18. [Google Scholar] [CrossRef] [Green Version]
- Locker, D.; Jokovic, A.; Kay, E.J. Prevention. Part 8: The use of pit and fissure sealants in preventing caries in the permanent dentition of children. Br. Dent. J. 2003, 195, 375–378. [Google Scholar] [CrossRef]
- Wright, J.T.; Crall, J.J.; Fontana, M.; Gillette, E.J.; Novy, B.B.; Dhar, V.; Donly, K.; Hewlett, E.R.; Quinonez, R.B.; Chaffin, J.; et al. Evidence-based clinical practice guideline for the use of pit-and-fissure sealants: A report of the American dental association and the American academy of pediatric dentistry. J. Am. Dent. Assoc. 2016, 147, 672–682. [Google Scholar] [CrossRef] [Green Version]
- Naaman, R.; El-Housseiny, A.; Alamoudi, N. The use of pit and fissure sealants-A literature review. Dent J. 2017, 5, 34. [Google Scholar] [CrossRef] [Green Version]
- Ahovuo-Saloranta, A.; Forss, H.; Walsh, T.; Nordblad, A.; Makela, M.; Worthington, H.V. Pit and fissure sealants for preventing dental decay in permanent teeth. Cochrane Database Syst. Rev. 2017, 7, Cd001830. [Google Scholar] [CrossRef] [Green Version]
- Beiruti, N.; Frencken, J.E.; Van’t Hof, M.A.; Taifour, D.; van Palenstein, H.W.H. Caries-preventive effect of a one-time application of composite resin and glass ionomer sealants after 5 years. Caries Res 2006, 40, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Jodkowska, E. Efficacy of pit and fissure sealing: Long-term clinical observations. Quintessence Int. 2008, 39, 593–602. [Google Scholar] [PubMed]
- Chen, X.; Du, M.; Fan, M.; Mulder, J.; Huysmans, M.C.; Frencken, J.E. Effectiveness of two new types of sealants: Retention after 2 years. Clin. Oral Investig. 2012, 16, 1443–1450. [Google Scholar] [CrossRef] [Green Version]
- AlShahrani, S.S.; AlAbbas, M.S.; Garcia, I.M.; AlGhannam, M.I.; AlRuwaili, M.A.; Collares, F.M.; Ibrahim, M.S. The antibacterial effects of resin-based dental sealants: A systematic review of In vitro studies. Materials 2021, 14, 413. [Google Scholar] [CrossRef] [PubMed]
- Par, M.; Spanovic, N.; Mohn, D.; Attin, T.; Tauböck, T.T.; Tarle, Z. Curing potential of experimental resin composites filled with bioactive glass: A comparison between Bis-EMA and UDMA based resin systems. Dent. Mater. 2020, 36, 711–723. [Google Scholar] [CrossRef]
- Imataki, R.; Shinonaga, Y.; Nishimura, T.; Abe, Y.; Arita, K. Mechanical and functional properties of a novel apatite-ionomer cement for prevention and remineralization of dental caries. Materials 2019, 12, 3998. [Google Scholar] [CrossRef] [Green Version]
- Hasanuddin, S.; Reddy, E.R.; Manjula, M.; Srilaxmi, N.; Rani, S.T.; Rajesh, A. Retention of fissure sealants in young permanent molars affected by dental fluorosis: A 12-month clinical study. Eur. Arch. Paediatr. Dent. 2014, 15, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, J.C. Caries process on occlusal surfaces: Evolving evidence and understanding. Caries Res. 2014, 48, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Muller-Bolla, M.; Courson, F.; Droz, D.; Lupi-Pegurier, L.; Velly, A.M. Definition of at-risk occlusal surfaces of permanent molars—A descriptive study. J. Clin. Pediatr. Dent. 2009, 34, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Salem Ibrahim, M.; AlQarni, F.D.; Al-Dulaijan, Y.A.; Weir, D.M.; Oates, T.W.; Xu, H.H.; Melo, M.A.S. Tuning nano-amorphous calcium phosphate content in novel rechargeable antibacterial dental sealant. Materials 2018, 11, 1544. [Google Scholar] [CrossRef] [PubMed] [Green Version]






| Age (Average ± SD) | Median (IQR) | Range |
|---|---|---|
| 7.11 ± 0.614 years | 7 (7–7.75) years | 6–8 years |
| Group | Material | Producer | Composition |
|---|---|---|---|
| I | Admira seal | Voco, Cuxhaven, Germany | Ormocer dimethacrylates, inorganic microparticles, silicate fillers, fumed silica and different additives |
| II | Embrace Wet Bond | 150320 Pulpdent Corporation, Watertown, MA, USA | Aliphatic urethane dimethacrylate, bis-methacryloyl phosphate, HEMA, trimethylolpropane trimethacrylate, water, 3% NaF, 36.6% silicon dioxide (SiO2) |
| III | Fotoseal | Remed Prodimpex SRL, Bucharest, Romania | 60% dimethacrylate monomer mixture, 40% hybrid inorganic filler (colloidal silica, titanium dioxide, eutectic fluoride) |
| IV | Fuji GC Triage (white shade) | GC Corporation, Tokyo, Japan | Fluoroaluminium silicate glass, polyacrylic acid, polybasic carboxylic acid |
| Status—6 Months | Average ± SD | Median (IQR) | Average Rank | p* |
| Sealant intact (p < 0.001 **) | 7.14 ± 0.613 | 7 (7–8) | 77.78 | 0.617 |
| Lost sealant (p < 0.001 **) | 7.33 ± 0.577 | 7 | 89.17 | |
| Status—12 Months | Average ± SD | Median (IQR) | Average Rank | p* |
| Sealant intact (p < 0.001 **) | 7.14 ± 0.625 | 7 (7–8) | 77.60 | 0.742 |
| Lost sealant (p < 0.001 **) | 7.2 ± 0.523 | 7 (7–7.75) | 80.67 | |
| Status—18 Months | Average ± SD | Median (IQR) | Average Rank | p* |
| Sealant intact (p < 0.001 **) | 7.18 ± 0.629 | 7 (7–8) | 68.17 | 0.655 |
| Lost sealant (p < 0.001 **) | 7.11 ± 0.333 | 7 (7–7) | 73.85 |
| Status—6 Months | Average ± SD | Median (IQR) | Average Rank | p* |
| Sealant intact (p < 0.001 **) | 7.08 ± 0.589 | 7 (7–7) | 82.00 | 0.015 |
| Lost sealant (p = 0.001 **) | 7.67 ± 0.516 | 8 (7–8) | 123.50 | |
| Status—12 Months | Average ± SD | Median (IQR) | Average Rank | p* |
| Sealant intact (p < 0.001 **) | 7.07 ± 0.612 | 7 (7–7) | 81.93 | 0.274 |
| Lost sealant (p < 0.001 **) | 7.21 ± 0.499 | 7 (7–7.75) | 91.21 | |
| Status—18 Months | Average ± SD | Median (IQR) | Average Rank | p* |
| Sealant intact (p < 0.001 **) | 7.1 ± 0.599 | 7 (7–7) | 78.05 | 0.157 |
| Lost sealant (p = 0.001 **) | 7.43 ± 0.535 | 7 (7–8) | 99.36 |
| Status—6 Months | Average ± SD | Median (IQR) | Average Rank | p* |
| Sealant intact (p < 0.001 **) | 7.07 ± 0.576 | 7 (7–7) | 66.32 | 0.437 |
| Lost sealant (p = 0.005 **) | 6.94 ± 0.772 | 7 (6–7.75) | 59.66 | |
| Status—12 Months | Average ± SD | Median (IQR) | Average Rank | p* |
| Sealant intact (p < 0.001 **) | 7.04 ± 0.614 | 7 (7–7) | 64.58 | 0.664 |
| Lost sealant (p < 0.001 **) | 7.09 ± 0.583 | 7 (7–7) | 67.13 | |
| Status—18 Months | Average ± SD | Median (IQR) | Average Rank | p* |
| Sealant intact (p < 0.001 **) | 7.13 ± 0.565 | 7 (7–7) | 64.85 | 0.035 |
| Lost sealant (p < 0.001 **) | 6.83 ± 0.702 | 7 (6–7) | 50.25 |
| Status—6 Months | Average ± SD | Median (IQR) | Average Rank | p* |
| Sealant intact (p < 0.001 **) | 7.15 ± 0.545 | 7 (7–7) | 63.92 | 0.899 |
| Lost sealant (p = 0.005 **) | 7.14 ± 0.900 | 7 (6–8) | 65.43 | |
| Status—12 Months | Average ± SD | Median (IQR) | Average Rank | p* |
| Sealant intact (p < 0.001 **) | 7.13 ± 0.494 | 7.13 ± 0.494 | 7.13 ± 0.494 | 0.373 |
| Lost sealant (p < 0.001 **) | 7.21 ± 0.729 | 7.21 ± 0.729 | 7.21 ± 0.729 | |
| Status—18 Months | Average ± SD | Median (IQR) | Average Rank | p* |
| Sealant intact (p < 0.001 **) | 7.09 ± 0.478 | 7 (7–7) | 58.95 | 0.004 |
| Lost sealant (p < 0.001 **) | 7.41 ± 0.747 | 8 (7–8) | 77.70 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muntean, A.; Sarosi, C.; Sava, S.; Moldovan, M.; Condurache, A.I.; Delean, A.G. Dental Sealant Composition-Retention Assessment in Young Permanent Molars. Materials 2021, 14, 1646. https://doi.org/10.3390/ma14071646
Muntean A, Sarosi C, Sava S, Moldovan M, Condurache AI, Delean AG. Dental Sealant Composition-Retention Assessment in Young Permanent Molars. Materials. 2021; 14(7):1646. https://doi.org/10.3390/ma14071646
Chicago/Turabian StyleMuntean, Alexandrina, Codruta Sarosi, Sorina Sava, Marioara Moldovan, Andrei Ilie Condurache, and Ada Gabriela Delean. 2021. "Dental Sealant Composition-Retention Assessment in Young Permanent Molars" Materials 14, no. 7: 1646. https://doi.org/10.3390/ma14071646
APA StyleMuntean, A., Sarosi, C., Sava, S., Moldovan, M., Condurache, A. I., & Delean, A. G. (2021). Dental Sealant Composition-Retention Assessment in Young Permanent Molars. Materials, 14(7), 1646. https://doi.org/10.3390/ma14071646