Vector Competence of Culicoides sonorensis (Diptera: Ceratopogonidae) for Epizootic Hemorrhagic Disease Virus Serotype 2 Strains from Canada and Florida
Abstract
:1. Introduction
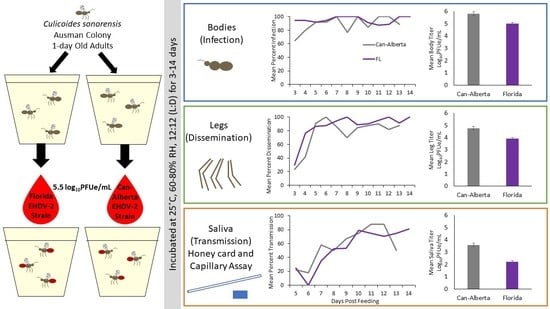
2. Materials and Methods
2.1. Culicoides Sonorensis Colony
2.2. Viral Strains
2.3. Viral Infection
2.4. Insect Tissue/Saliva Collection for Viral RNA Detection
2.4.1. Capillary Tube Bioassays
2.4.2. Honey Card Bioassays
2.5. Sample Processing and Viral RNA Detection
2.6. Statistical Analysis
3. Results
3.1. Infection, Dissemination, and Transmission Rates
3.2. Viral Titer Analysis
3.3. Honey Card Versus Capillary Tube Assay Comparison
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kedmi, M.; Van Straten, M.; Ezra, E.; Galon, N.; Klement, E. Assessment of the productivity effects associated with epizootic hemorrhagic disease in dairy herds. J. Dairy Sci. 2010, 93, 2486–2495. [Google Scholar] [CrossRef]
- Stevens, G.; McCluskey, B.; King, A.; O’Hearn, E.; Mayr, G. Review of the 2012 epizootic hemorrhagic disease outbreak in domestic ruminants in the United States. PLoS ONE 2015, 10, 1–12. [Google Scholar] [CrossRef]
- Fox, K.A.; Diamond, B.; Sun, F.; Clavijo, A.; Sneed, L.; Kitchen, D.N.; Wolfe, L.L. Testicular lesions and antler abnormalities in Colorado, USA mule deer (Odocoileus hemionus): A possible role for epizootic hemorrhagic disease virus. J. Wildl. Dis. 2015, 51, 166–176. [Google Scholar] [CrossRef]
- Dubay, S.A.; deVos, J.C.; Noon, T.H.; Boe, S. Epizootiology of hemorrhagic disease in mule deer in central Arizona. J. Wildl. Dis. 2004, 40, 119–124. [Google Scholar] [CrossRef]
- Davidson, W.R.; Fischer, J.R.; Little, S.E.; Lockhart, J.M.; Luttrell, M.P.; Mead, D.G.; Nettles, V.F.; Quist, C.F.; Smith, K.E.; Stallknecht, D.E.; et al. White-tailed Deer (Odocoileus virginianus). In Field Manual of Wildlife Diseases in the Southeastern United States, 3rd ed.; Davidson, W.R., Ed.; Southeastern Cooperative Wildlife Disease Study: Athens, GA, USA, 2006; pp. 26–37. [Google Scholar]
- Allison, A.B.; Goekjian, V.H.; Potgieter, A.C.; Wilson, W.C.; Johnson, D.J.; Mertens, P.P.C.; Stallknecht, D.E. Detection of a novel reassortant epizootic hemorrhagic disease virus (EHDV) in the USA containing RNA segments derived from both exotic (EHDV-6) and endemic (EHDV-2) serotypes. J. Gen. Virol. 2010, 91, 430–439. [Google Scholar] [CrossRef]
- Chalmers, G.A.; Vance, H.N.; Mitchell, G.J. An outbreak of epizootic hemorrhagic disease in wild ungulates in Alberta. J. Wildl. Dis. 1964, 42, 15–20. [Google Scholar]
- Shope, R.; MacNamara, L.; Mangold, R. Report on the deer mortality, epizootic hemorrhagic disease of deer. NJ Outdoors 1955, 6, 17–21. [Google Scholar]
- Anthony, S.J.; Maan, S.; Maan, N.; Kgosana, L.; Bachanek-Bankowska, K.; Batten, C.; Darpel, K.E.; Sutton, G.; Attoui, H.; Mertens, P.P.C. Genetic and phylogenetic analysis of the outer-coat proteins VP2 and VP5 of epizootic hemorrhagic disease virus (EHDV): Comparison of genetic and serological data to characterize the EHDV serogroup. Virus Res. 2009, 145, 200–210. [Google Scholar] [CrossRef]
- Holmes, E.C.; Burch, S.S. The causes and consequences of genetic variation in dengue virus. Trends Microbiol. 2000, 8, 74–77. [Google Scholar] [CrossRef]
- Brault, A.C.; Powers, A.M.; Ortiz, D.; Estrada-franco, J.G.; Navarro-Lopez, R.; Weaver, S.C.; Beaty, B.J. Venezuelan equine encephalitis emergence: Enhanced vector infection from a single amino acid substitution in the envelope glycoprotein. Proc. Natl. Acad. Sci. USA 2004, 101, 11344–11349. [Google Scholar] [CrossRef] [Green Version]
- Tsetsarkin, K.A.; Vanlandingham, D.L.; McGee, C.E.; Higgs, S. A single mutation in Chikungunya virus affects vector specificity and epidemic potential. PLoS Pathog. 2007, 3, 1895–1906. [Google Scholar] [CrossRef]
- Tsetsarkin, K.A.; Weaver, S.C. Sequential adaptive mutations enhance efficient vector switching by Chikungunya virus and its epidemic emergence. PLoS Pathog. 2011, 7, e1002412. [Google Scholar] [CrossRef]
- Brault, A.C.; Powers, A.M.; Holmes, E.C.; Woelk, C.H.; Weaver, S.C. Positively charged amino acid substitutions in the E2 envelope glycoprotein are associated with the emergence of Venezuelan equine encephalitis virus. J. Virol. 2002, 76, 1718–1730. [Google Scholar] [CrossRef]
- Anischenko, M.; Bowen, R.A.; Paessler, S.; Austgen, L.; Greene, I.P.; Weaver, S.C. Venezuelan encephalitis emergence mediated by a phylogenetically predicted viral mutation. Proc. Natl. Acad. Sci. USA 2006, 103, 4994–4999. [Google Scholar] [CrossRef] [Green Version]
- Weaver, S.C.; Reisen, W.K. Present and future arboviral threats. Antivir. Res. 2010, 85, 328–345. [Google Scholar] [CrossRef] [Green Version]
- Venter, G.J.; Wright, I.M.; Van der Linde, T.C.; Paweska, J.T. The oral susceptibility of South African field populations of Culicoides to African horse sickness virus. Med. Vet. Entomol. 2009, 23, 367–378. [Google Scholar] [CrossRef]
- Campbell, C.H.; Barber, T.L.; Jochim, M.M. Antigenic relationship of Ibaraki, bluetongue, and epizootic hemorrhagic disease viruses. Vet. Microbiol. 1978, 3, 15–22. [Google Scholar] [CrossRef]
- Omori, T.; Inaba, Y.; Morimoto, T.; Tanaka, Y.; Ishitani, R.; Kurogi, H.; Munakata, K.; Matsuda, K.; Matumoto, M. Ibaraki virus, an agent of epizootic disease of cattle resembling bluetongue: IV. Physicochemical and serological properties of the virus. Jpn. J. Microbiol. 1970, 14, 351–360. [Google Scholar]
- Ohashi, S.; Yoshida, K.; Watanabe, Y.; Tsuda, T. Identification and PCR-restriction fragment length polymorphism analysis of a variant of the Ibaraki virus from naturally infected cattle and aborted fetuses in Japan. J. Clin. Microbiol. 1999, 37, 3800–3803. [Google Scholar]
- Ohashi, S.; Yoshida, K.; Yanase, T.; Tsuda, T. Analysis of intratypic variation evident in an Ibaraki virus strain and its epizootic hemorrhagic disease virus serogroup. J. Clin. Microbiol. 2002, 40, 3684–3688. [Google Scholar] [CrossRef]
- Jones, R.H.; Roughton, R.D.; Foster, N.M.; Bando, B.M. Culicoides, the vector of epizootic hemorrhagic disease in white-tailed deer in Kentucky in 1971. J. Wildl. Dis. 1977, 13, 2–8. [Google Scholar] [CrossRef]
- Foster, N.M.; Breckon, R.D.; Luedke, A.J.; Jones, R.H. Transmission of two strains of epizootic hemorrhagic disease virus in deer by Culicoides variipennis. J. Wildl. Dis. 1977, 13, 9–16. [Google Scholar] [CrossRef]
- Pfannenstiel, R.S.; Mullens, B.A.; Ruder, M.G.; Zurek, L.; Cohnstaedt, L.W.; Nayduch, D. Management of North American Culicoides biting midges: Current knowledge and research needs. Vector Borne Zoonotic Dis. 2015, 15, 374–384. [Google Scholar] [CrossRef]
- Savini, G.; Afonso, A.; Mellor, P.; Aradaib, I.; Yadin, H.; Sanaa, M.; Wilson, W.; Monaco, F.; Domingo, M. Epizootic heamorragic disease. Res. Vet. Sci. 2011, 91, 1–17. [Google Scholar] [CrossRef]
- Anderson, D.P.; Outlaw, J.L.; Earle, M.L.; Richardson, J.W. Economic impact of U.S. deer breeding and hunting operations. Texas A&M Univ. Ag. Food Pol. Cent. Res. Rep. 2017, 17, 1–20. [Google Scholar]
- Roughton, R.D. An outbreak of a hemorrhagic disease in white-tailed deer in Kentucky. J. Wildl. Dis. 1975, 11, 177–186. [Google Scholar] [CrossRef]
- Lee, J.; English, A. Economic impact of the deer and elk farming industry in Indiana. Indiana Deer Elk Farm. Assoc. 2011, 1, 1–25. [Google Scholar]
- Hall-Mendelin, S.; Ritchie, S.A.; Johansen, C.A.; Zborowski, P.; Cortis, G.; Dandridge, S.; Hall, R.A.; van den Hurk, A.F. Exploiting mosquito sugar feeding to detect mosquito-borne pathogens. Proc. Natl. Acad. Sci. USA 2010, 107, 11255–11259. [Google Scholar] [CrossRef] [Green Version]
- Alto, B.W.; Wiggins, K.; Eastmond, B.; Velez, D.; Lounibos, L.P.; Lord, C.C. Transmission risk of two chikungunya lineages by invasive mosquito vectors from Florida and the Dominican Republic. PLoS Negl. Trop. Dis. 2017, 11, 1–23. [Google Scholar] [CrossRef]
- Veronesi, E.; Henstock, M.R.; Gubbins, S.; Batten, C.; Manley, R.; Barber, J.; Hoffmann, B.; Beer, M.; Attoui, H.; Mertens, P.P.C.; et al. Implicating Culicoides biting midges as vectors of Schmallenberg virus using semi-quantitative RT-PCR. PLoS ONE 2013, 8, e57747. [Google Scholar] [CrossRef]
- Hunt, G.J. A Procedural Manual for the Large-Scale Rearing of the Biting Midges, Culicoides Variipennis (Diptera: Ceratopogonidae); U.S. Department of Agriculture-Agricultural Research Service, ARS 1–1; National Technical Information Service: Springfield, VA, USA, 1994; pp. 1–68.
- Zhao, L.; Alto, B.W.; Shin, D.; Yu, F. The effect of permethrin resistance on Aedes aegypti transcriptome following ingestion of Zika virus. Viruses 2018, 10, 470. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S.L.; Richards, S.L.; Smartt, C.T. A simple method for determining arbovirus transmission in mosquitoes. J. Am. Mosq. Control. Assoc. 2010, 26, 108–111. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.R.; Carrara, A.; Aguilar, P.V.; Weaver, S.C. Evaluation of methods to assess transmission potential of Venezuelan equine encephalitis virus by mosquitoes and estimation of mosquito saliva titers. Am. J. Trop. Med. Hyg. 2005, 73, 33–39. [Google Scholar] [CrossRef]
- Boorman, J. Induction of salivation in biting midges and mosquitoes, and demonstration of virus in the saliva of infected insects. Med. Vet. Entomol. 1987, 1, 211–214. [Google Scholar] [CrossRef]
- Wiggins, K.; Eastmond, B.; Alto, B.W. Transmission potential of Mayaro virus in Florida Aedes aegypti and Aedes albopictus mosquitoes. Med. Vet. Entomol. 2018, 32, 436–442. [Google Scholar] [CrossRef]
- Honorio, N.A.; Wiggins, K.; Camara, D.C.; Eastmond, B.; Alto, B.W. Chikungunya virus vector competency of Brazilian and Florida mosquito vectors. PLoS Negl. Trop. Dis. 2018, 12, 1–17. [Google Scholar] [CrossRef]
- Wernike, K.; Hoffmann, B.; Beer, M. Simultaneous detection of five notifiable viral diseases of cattle by single-tube multiplex real-time RT-PCR. J. Virol. Methods 2015, 217, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Wilson, W.C.; O’Hearn, E.S.; Tellgren-Roth, C.; Stallknecht, D.E.; Mead, D.G.; Mecham, J.O. Detection of all eight serotypes of epizootic hemorrhagic disease virus by real-time reverse transcription polymerase chain reaction. J. Vet. Diagn. Investig. 2009, 101, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Bustin, S.A. Absolute quantification of mRNA using real-time reverse transcription polymerase chain reaction assays. J. Mol. Endocrin. 2000, 25, 169–193. [Google Scholar] [CrossRef] [Green Version]
- Mills, M.K.; Ruder, M.G.; Nayduch, D.; Michel, K.; Drolet, B.S. Dynamics of epizootic hemorrhagic disease virus infection within the vector, Culicoides sonorensis (Diptera: Ceratopogonidae). PLoS ONE 2017, 12, 1–16. [Google Scholar] [CrossRef]
- Ruder, M.G.; Howerth, E.W.; Stallknecht, D.E.; Allison, A.B.; Carter, D.L.; Drolet, B.S.; Klement, E.; Mead, D.G. Vector competence of Culicoides sonorensis (Diptera: Ceratopogonidae) to epizootic hemorrhagic disease virus serotype 7. Parasites Vectors 2012, 5, 236. [Google Scholar] [CrossRef]
- Ruder, M.G.; Stallknecht, D.E.; Allison, A.B.; Mead, D.G.; Carter, D.L.; Howerth, E.W. Host and potential vector susceptibility to an emerging Orbivirus in the United States: Epizootic hemorrhagic disease virus serotype 6. Vet. Pathol. 2015, 53, 574–584. [Google Scholar] [CrossRef]
- Mills, M.K.; Michel, K.; Pfannenstiel, R.S.; Ruder, M.G.; Veronesi, E.; Nayduch, D. Culicoides-virus interactions: Infection barriers and possible factors underlying vector competence. Curr. Opin. Insect Sci. 2017, 22, 7–15. [Google Scholar] [CrossRef]
- Veronesi, E.; Paslaru, A.; Silaghi, C.; Tobler, K.; Glavinic, U.; Torgerson, P.; Mathis, A. Experimental evaluation of infection, dissemination, and transmission rates for two West Nile virus strains in European Aedes japonicus under a fluctuating temperature regime. Parasitol. Res. 2018, 117, 1925–1932. [Google Scholar] [CrossRef]
- Richards, S.L.; Anderson, S.L.; Lord, C.C. Vector competence of Culex pipiens quinquefasciatus (Diptera: Culicidae) for West Nile virus isolates from Florida. Trop. Med. Int. Health 2014, 19, 610–617. [Google Scholar] [CrossRef]
- Ruder, M.G.; Stallknecht, D.E.; Howerth, E.W.; Carter, D.L.; Pfannenstiel, R.S.; Allison, A.B.; Mead, D.G. Effect of temperature on replication of epizootic hemorrhagic disease viruses in Culicoides sonorensis (Diptera: Ceratopogonidae). J. Med. Entomol. 2015, 52, 1050–1059. [Google Scholar] [CrossRef]
- Bowne, J.G.; Jones, R.H. Observations on bluetongue virus in the salivary glands of an insect vector, Culicoides variipennis. Virology 1966, 30, 127–133. [Google Scholar] [CrossRef]
- Fu, H.; Leake, C.J.; Mertens, P.P.C.; Mellor, P.S. The barriers to bluetongue virus infection, dissemination, and transmission in the vector, Culicoides variipennis (Diptera: Ceratopogonidae). Arch. Virol. 1999, 144, 747–761. [Google Scholar] [CrossRef]
- McMeniman, C.J.; Lane, R.V.; Cass, B.N.; Fong, A.W.C.; Sidhu, M.; Wang, Y.F.; O’Neill, S.L. Stable introduction of a life-shortening Wolbachia infection into the mosquito Aedes aegypti. Nature 2009, 323, 141–144. [Google Scholar] [CrossRef]
- Jennings, D.M.; Mellor, P.S. Variation in the responses of Culicoides variipennis (Diptera: Ceratopogonidae) to oral infection with bluetongue virus. Arch. Virol. 1987, 95, 177–182. [Google Scholar] [CrossRef]
- Baylis, M.; O’Connell, L.; Mellor, P.S. Rates of bluetongue virus transmission between Culicoides sonorensis and sheep. Med. Vet. Entomol. 2008, 22, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Borkent, A.; Grogan, W.L. Catalog of the new world biting midges north of Mexico (Diptera: Ceratopogonidae). Zootaxa 2009, 48, 1–48. [Google Scholar]
- Vigil, S.L.; Wlodskowski, J.C.; Parris, J. New records of biting midges of the genus Culicoides Latreille from the southeastern United States (Diptera: Ceratopogonidae). Insecta Mundi 2014, 0394, 1–14. [Google Scholar]
- Smith, K.; Stallknecht, D.; Sewell, C.; Rollor, E.; Mullen, G.; Anderson, R. Monitoring of Culicoides spp. at a site enzootic for hemorrhagic disease in white-tailed deer in Georgia, USA. J. Wildl. Dis. 1996, 32, 627–642. [Google Scholar] [CrossRef] [PubMed]
- Sloyer, K.E.; Wisely, S.M.; Burkett-Cadena, N.D. Effects of ultraviolet LED versus incandescent bulb and carbon dioxide for sampling abundance and diversity of Culicoides in Florida. J. Med. Entomol. 2019, 56, 353–361. [Google Scholar] [CrossRef]
- Smith, K.E.; Stallknecht, D.E. Culicoides (Diptera: Ceratopogonidae) collected during epizootics of hemorrhagic disease among captive white-tailed deer. J. Med. Entomol. 1996, 33, 507–510. [Google Scholar] [CrossRef] [PubMed]
- Colton, L.; Biggerstaff, B.J.; Johnson, A.; Nasci, R.S. Quantification of West Nile virus in vector mosquito saliva. J. Am. Mosq. Control. Assoc. 2005, 21, 49–53. [Google Scholar] [CrossRef]
- Alto, B.W.; Wiggins, K.; Eastmond, B.; Ortiz, S.; Zirbel, K.; Lounibos, L.P. Diurnal temperature range and Chikungunya virus infection in invasive mosquito vectors. J. Med. Entomol. 2018, 55, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Guedes, D.R.D.; Paiva, M.H.S.; Donato, M.M.A.; Barbosa, P.P.; Krokovsky, L.; Rocha, S.W.S.; Saraiva, K.L.A.; Crespo, M.M.; Rezende, T.M.T.; Wallau, G.L.; et al. Zika virus replication in the mosquito Culex quinquefasciatus in Brazil. Emerg. Microbes Infect. 2017, 6, e69. [Google Scholar] [CrossRef] [PubMed]
- Brustolin, M.; Talavera, S.; Nuñez, A.; Santamaría, C.; Rivas, R.; Pujol, N.; Valle, M.; Verdún, M.; Brun, A.; Pagés, N.; et al. Rift Valley fever virus and European mosquitoes: Vector competence of Culex pipiens and Stegomyia albopicta (=Aedes albopictus). Med. Vet. Entomol. 2017, 31, 365–372. [Google Scholar] [CrossRef]




| Can-Alberta Strain | Florida Strain | |||||
|---|---|---|---|---|---|---|
| Day | Infection a | Dissemination a | Transmission a | Infection a | Dissemination a | Transmission a |
| 3 | 65.0 (13/20) | 23.1 (3/13) | nd | 94.4 (17/18) | 29.4 (5/17) | nd |
| 4 | 80.0 (12/15) | 41.7 (5/12) | nd | 94.4 (17/18) | 76.5 (13/17) | nd |
| 5 | 91.7 (11/12) | 90.9 (10/11) | 22.2 (2/9) | 91.1 (22/24) | 86.4 (19/22) | 25.0 (1/4) |
| 6 | 91.7 (11/12) | 100.0 (11/11) | 18.2 (2/11) | 94.1 (16/17) | 87.5 (14/16) | 0.0 (0/14) |
| 7 | 100.0 (14/14) | 85.7 (12/14) | 58.3 (7/12) | 100.0 (18/18) | 94.4 (17/18) | 35.3 (6/17) |
| 8 | 76.9 (20/26) | 70.0 (14/20) | 50.0 (5/10) | 100.0 (19/19) | 100.0 (19/19) | 52.6 (10/19) |
| 9 | 100.0 (19/19) | 84.2 (16/19) | 66.7 (8/12) | 100.0 (18/18) | 88.9 (16/18) | 53.3 (8/15) |
| 10 | 84.2 (16/19) | 87.5 (14/16) | 75.0 (6/8) | 91.3 (21/23) | 90.5 (19/21) | 79.0 (15/19) |
| 11 | 100.0 (10/10) | 90.0 (9/10) | 87.5 (7/8) | 87.5 (21/24) | 95.2 (20/21) | 75.0 (12/16) |
| 12 | 100.0 (11/11) | 81.8 (9/11) | 87.5 (7/8) | 88.9 (24/27) | 100.0 (24/24) | 70.6 (12/17) |
| 13 | 88.9 (8/9) | 87.5 (7/8) | 50.0 (3/6) | 100.0 (23/23) | 91.3 (21/23) | 75.0 (15/20) |
| 14 b | nd | nd | nd | 100.0 (21/21) | 100.0 (21/21) | 81.3 (13/16) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
McGregor, B.L.; Erram, D.; Acevedo, C.; Alto, B.W.; Burkett-Cadena, N.D. Vector Competence of Culicoides sonorensis (Diptera: Ceratopogonidae) for Epizootic Hemorrhagic Disease Virus Serotype 2 Strains from Canada and Florida. Viruses 2019, 11, 367. https://doi.org/10.3390/v11040367
McGregor BL, Erram D, Acevedo C, Alto BW, Burkett-Cadena ND. Vector Competence of Culicoides sonorensis (Diptera: Ceratopogonidae) for Epizootic Hemorrhagic Disease Virus Serotype 2 Strains from Canada and Florida. Viruses. 2019; 11(4):367. https://doi.org/10.3390/v11040367
Chicago/Turabian StyleMcGregor, Bethany L., Dinesh Erram, Carolina Acevedo, Barry W. Alto, and Nathan D. Burkett-Cadena. 2019. "Vector Competence of Culicoides sonorensis (Diptera: Ceratopogonidae) for Epizootic Hemorrhagic Disease Virus Serotype 2 Strains from Canada and Florida" Viruses 11, no. 4: 367. https://doi.org/10.3390/v11040367
APA StyleMcGregor, B. L., Erram, D., Acevedo, C., Alto, B. W., & Burkett-Cadena, N. D. (2019). Vector Competence of Culicoides sonorensis (Diptera: Ceratopogonidae) for Epizootic Hemorrhagic Disease Virus Serotype 2 Strains from Canada and Florida. Viruses, 11(4), 367. https://doi.org/10.3390/v11040367