Mosquito-Borne Viruses and Non-Human Vertebrates in Australia: A Review
Abstract
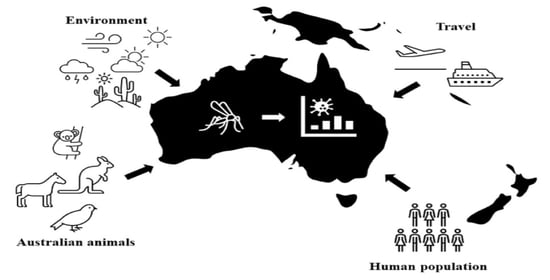
:1. Introduction
2. Mosquitoes: The Link between Vertebrate Host and Disease
3. Uniquely Australian Vertebrate Hosts
Marsupials
4. Ross River Virus
5. Barmah Forest Virus
6. Sindbis Virus
7. Murray Valley Encephalitis Virus
8. West Nile Virus
9. Japanese Encephalitis Virus
10. Kokobera and Related Viruses
11. Gan Gan and Trubanaman Viruses
12. A Changing Australia and Its Consequences
12.1. Climate and Its Significance to Australia’s Unique Vertebrate Communities
12.2. Climate and Its Significance to Mosquitoes
12.3. Urbanization and Habitat Fragmentation
13. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gubler, D.J. Human arbovirus infections worldwide. Ann. N. Y. Acad. Sci. 2001, 951, 13–24. [Google Scholar] [CrossRef]
- Russell, R.C. Mosquito-borne disease and climate change in Australia: Time for a reality check. Aust. J. Entomol. 2009, 48, 1–7. [Google Scholar] [CrossRef]
- Kraemer, M.U.; Sinka, M.E.; Duda, K.A.; Mylne, A.Q.; Shearer, F.M.; Barker, C.M.; Moore, C.G.; Carvalho, R.G.; Coelho, G.E.; Van Bortel, W. The global distribution of the arbovirus vectors Aedes aegypti and Ae. albopictus. eLife 2015, 4, e08347. [Google Scholar] [CrossRef]
- Canyon, D.; Speare, R.; Naumann, I.; Winkel, K. Environmental and economic costs of invertebrate invasions in Australia. In Biological Invasions: Economic and Environmental Cost of Alien Plant, Animal and Microbe Species; Pimental, D., Ed.; CRC Press: London, UK, 2002. [Google Scholar]
- Mwebaze, P.; Bennett, J.; Beebe, N.W.; Devine, G.J.; De Barro, P. Economic valuation of the threat posed by the establishment of the Asian Tiger Mosquito in Australia. Environ. Resour. Econ. 2018, 71, 357–379. [Google Scholar] [CrossRef]
- Mackenzie, J.S.; Poidinger, M.; Lindsay, M.D.; Hall, R.A.; Sammels, L.M. Molecular epidemiology and evolution of mosquito-borne flaviviruses and alphaviruses enzootic in Australia. In Molecular Evolution of Viruses—Past and Present; Becker, Y., Ed.; Springer: Boston, MA, USA, 1996; pp. 153–165. [Google Scholar]
- Webb, C.; Doggett, S.; Russell, R. A Guide to Mosquitoes of Australia; CSIRO Publishing: Canberra, Australia, 2016. [Google Scholar]
- Jansen, C.C.; Webb, C.E.; Graham, G.C.; Craig, S.B.; Zborowski, P.; Ritchie, S.A.; Russell, R.C.; Van den Hurk, A.F. Blood sources of mosquitoes collected from urban and peri-urban environments in eastern Australia with species-specific molecular analysis of avian blood meals. Am. J. Trop. Med. Hyg. 2009, 81, 849–857. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reiter, P. Climate change and mosquito-borne disease. Environ. Health Perspect. 2001, 109, 141. [Google Scholar] [PubMed] [Green Version]
- Stephenson, E.B.; Murphy, A.K.; Jansen, C.C.; Peel, A.J.; McCallum, H. Interpreting mosquito feeding patterns in Australia through an ecological lens: An analysis of blood meal studies. Parasit. Vectors 2019, 12, 156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takken, W.; Verhulst, N.O. Host preferences of blood-feeding mosquitoes. Annu. Rev. Entomol. 2013, 58, 433–453. [Google Scholar] [CrossRef] [Green Version]
- Gyawali, N.; Taylor-Robinson, A.W.; Bradbury, R.S.; Huggins, D.W.; Hugo, L.E.; Lowry, K.; Aaskov, J.G. Identification of the source of blood meals in mosquitoes collected from north-eastern Australia. Parasit. Vectors 2019, 12, 198. [Google Scholar] [CrossRef]
- Russell, R.C.; Dwyer, D.E. Arboviruses associated with human disease in Australia. Microbes Infect. 2000, 2, 1693–1704. [Google Scholar] [CrossRef]
- Flies, E.J.; Lau, C.L.; Carver, S.; Weinstein, P. Another Emerging Mosquito-Borne Disease? Endemic Ross River Virus Transmission in the Absence of Marsupial Reservoirs. Bioscience 2018, 68, 288–293. [Google Scholar] [CrossRef]
- Old, J.M.; Deane, E.M. Antibodies to the Ross River virus in captive marsupials in urban areas of eastern New South Wales, Australia. J. Wildl. Dis. 2005, 41, 611–614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boyd, A.M.; Hall, R.A.; Gemmell, R.T.; Kay, B.H. Experimental infection of Australian brushtail possums, Trichosurus vulpecula (Phalangeridae: Marsupialia), with Ross River and Barmah Forest viruses by use of a natural mosquito vector system. Am. J. Trop. Med. Hyg. 2001, 65, 777–782. [Google Scholar] [CrossRef] [Green Version]
- Doherty, R.; Standfast, H.; Domrow, R.; Wetters, E.; Whitehead, R.; Carley, J. Studies of the epidemiology of arthropod-borne virus infections at Mitchell River Mission, Cape York Peninsula, North Queensland IV. Arbovirus infections of mosquitoes and mammals, 1967–1969. Trans. R. Soc. Trop. Med. Hyg. 1971, 65, 504–513. [Google Scholar] [CrossRef]
- Potter, A.; Johansen, C.A.; Fenwick, S.; Reid, S.A.; Lindsay, M.D. The seroprevalence and factors associated with Ross River virus infection in western grey kangaroos (Macropus fuliginosus) in Western Australia. Vector Borne Zoonotic Dis. 2014, 14, 740–745. [Google Scholar] [CrossRef] [Green Version]
- Russell, R.C. Ross River virus: Ecology and distribution. Annu. Rev. Entomol. 2002, 47, 1–31. [Google Scholar] [CrossRef]
- Stephenson, E.B.; Peel, A.J.; Reid, S.A.; Jansen, C.C.; McCallum, H. The non-human reservoirs of Ross River virus: A systematic review of the evidence. Parasit. Vectors 2018, 11, 188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kay, B.H.; Boyd, A.M.; Ryan, P.A.; Hall, R.A. Mosquito feeding patterns and natural infection of vertebrates with Ross River and Barmah Forest viruses in Brisbane, Australia. Am. J. Trop. Med. Hyg. 2007, 76, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Roche, S.; Wicks, R.; Garner, M.; East, I.; Paskin, R.; Moloney, B.; Carr, M.; Kirkland, P. Descriptive overview of the 2011 epidemic of arboviral disease in horses in Australia. Aust. Vet. J. 2013, 91, 5–13. [Google Scholar] [CrossRef]
- National Notifiable Diseases Surveillance System. Available online: http://www9.health.gov.au/cda/source/cda-index.cfm (accessed on 30 January 2021).
- Kay, B.H.; Ryan, P.A. Vector Competence of Mosquitoes (Diptera: Culicidae) from Maroochy Shire, Australia, for Barmah Forest Virus. J. Med. Entomol. 1999, 36, 856–860. [Google Scholar]
- Aldred, J.; Campbell, J.; Mitchell, G.; Davis, G.; Elliott, J. Involvement of Wildlife in the Natural Cycle of Ross River and Barmah Forest Viruses. In Proceedings of the Wildlife Disease Association Meeting, Mallacoota, Melbourne, Australia, 12–16 March 1991. [Google Scholar]
- Vale, T.; Spratt, D.; Cloonan, M. Serological evidence of arbovirus infection in native and domesticated mammals on the south coast of New South Wales. Aust. J. Zool. 1991, 39, 1–7. [Google Scholar] [CrossRef]
- Boyd, A.; Kay, B. Assessment of the potential of dogs and cats as urban reservoirs of Ross River and Barmah Forest viruses. Aust. Vet. J. 2002, 80, 83–86. [Google Scholar] [CrossRef]
- Olson, K.; Trent, D. Genetic and antigenic variations among geographical isolates of Sindbis virus. J. Gen. Virol. 1985, 66, 797–810. [Google Scholar] [CrossRef] [PubMed]
- Dhileepan, K.; Azuolas, J.; Gibson, C. Evidence of vertical transmission of Ross River and Sindbis viruses (Togaviridae: Alphavirus) by mosquitoes (Diptera: Culicidae) in southeastern Australia. J. Med. Entomol. 1996, 33, 180–182. [Google Scholar] [CrossRef] [PubMed]
- Sammels, L.M.; Lindsay, M.D.; Poidinger, M.; Coelen, R.J.; Mackenzie, J.S. Geographic distribution and evolution of Sindbis virus in Australia. J. Gen. Virol. 1999, 80, 739–748. [Google Scholar] [CrossRef] [Green Version]
- Johansen, C.; Power, S.; Broom, A. Determination of mosquito (Diptera: Culicidae) bloodmeal sources in Western Australia: Implications for arbovirus transmission. J. Med. Entomol. 2009, 46, 1167–1175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cordova, S.; Smith, D.; Broom, A.; Lindsay, M.; Dowse, G.; Beers, M. Murray Valley encephalitis in Western Australia in 2000, with evidence of southerly spread. Commun. Dis. Intell. 2000, 24, 368–372. [Google Scholar]
- Hobson-Peters, J.; Yam, A.W.Y.; Lu, J.W.F.; Setoh, Y.X.; May, F.J.; Kurucz, N.; Walsh, S.; Prow, N.A.; Davis, S.S.; Weir, R. A new insect-specific flavivirus from northern Australia suppresses replication of West Nile virus and Murray Valley encephalitis virus in co-infected mosquito cells. PLoS ONE 2013, 8, e56534. [Google Scholar] [CrossRef]
- Marshall, I.D.; Brown, B.K.; Keith, K.; Gard, G.P.; Thibos, E. Variation in arbovirus infection rates in species of birds sampled in a serological survey during an encephalitis epidemic in the Murray Valley of south-eastern Australia, February 1974. Immunol. Cell Biol. 1982, 60, 471. [Google Scholar] [CrossRef]
- Kay, B.; Fanning, I.; Carley, J. The vector competence of Australian Culex annulirostris with Murray Valley encephalitis and Kunjin viruses. Aust. J. Exp. Biol. Med. Sci. 1984, 62, 641–650. [Google Scholar] [CrossRef]
- Johansen, C.A.; Susai, V.; Hall, R.A.; Mackenzie, J.S.; Clark, D.C.; May, F.J.; Hemmerter, S.; Smith, D.W.; Broom, A.K. Genetic and phenotypic differences between isolates of Murray Valley encephalitis virus in Western Australia, 1972–2003. Virus Genes 2007, 35, 147–154. [Google Scholar] [CrossRef]
- Kay, B.; Young, P.; Hall, R.; Fanning, I. Experimental infection with Murray Valley encephalitis virus. Pigs, cattle, sheep, dogs, rabbits, macropods and chickens. Aust. J. Exp. Biol. Med. Sci. 1985, 63, 109–126. [Google Scholar] [CrossRef] [PubMed]
- Kay, B.; Hall, R.; Fanning, I.; Young, P. Experimental infection with Murray Valley Encephalitis virus: Galahs, sulphur-crested cockatoos, corellas, black ducks and wild mice. Aust. J. Exp. Biol. Med. Sci. 1985, 63, 599–606. [Google Scholar] [CrossRef]
- Carver, S.; Bestall, A.; Jardine, A.; Ostfeld, R.S. Influence of hosts on the ecology of arboviral transmission: Potential mechanisms influencing dengue, Murray Valley encephalitis, and Ross River virus in Australia. Vector Borne Zoonotic Dis. 2009, 9, 51–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gordon, A.N.; Marbach, C.R.; Oakey, J.; Edmunds, G.; Condon, K.; Diviney, S.M.; Williams, D.T.; Bingham, J. Confirmed case of encephalitis caused by Murray Valley encephalitis virus infection in a horse. J. Vet. Diagn. Investig. 2012, 24, 431–436. [Google Scholar] [CrossRef] [Green Version]
- Holmes, J.; Gilkerson, J.; El Hage, C.; Slocombe, R.; Muurlink, M. Murray Valley encephalomyelitis in a horse. Aust. Vet. J. 2012, 90, 252–254. [Google Scholar] [CrossRef]
- Frost, M.J.; Zhang, J.; Edmonds, J.H.; Prow, N.A.; Gu, X.; Davis, R.; Hornitzky, C.; Arzey, K.E.; Finlaison, D.; Hick, P. Characterization of virulent West Nile virus Kunjin strain, Australia, 2011. Emerg. Infect. Dis. 2012, 18, 792. [Google Scholar] [CrossRef]
- Jansen, C.C.; Ritchie, S.A.; van den Hurk, A.F. The Role of Australian Mosquito Species in the Transmission of Endemic and Exotic West Nile Virus Strains. Int. J. Environ. Res. Public Health 2013, 10, 3735–3752. [Google Scholar] [CrossRef]
- Scherret, J.H.; Poidinger, M.; Mackenzie, J.S.; Broom, A.K.; Deubel, V.; Lipkin, W.I.; Briese, T.; Gould, E.A.; Hall, R.A. The Relationships between West Nile and Kunjin Viruses. Emerg. Infect. Dis. 2001, 7, 697–705. [Google Scholar] [CrossRef]
- Prow, N.A. The Changing Epidemiology of Kunjin Virus in Australia. Int. J. Environ. Res. Public Health 2013, 10, 6255–6272. [Google Scholar] [CrossRef] [PubMed]
- Jansen, C.C.; Webb, C.E.; Northill, J.A.; Ritchie, S.A.; Russell, R.C.; Hurk, A.F.V.D. Vector Competence of Australian Mosquito Species for a North American Strain of West Nile Virus. Vector Borne Zoonotic Dis. 2008, 8, 805–812. [Google Scholar] [CrossRef]
- Maute, K.; Webb, C.; Phalen, D.; Martin, J.; Hobson-Peters, J.; Major, R.E.; French, K. Clean bill of health? Towards an understanding of health risks posed by urban ibis. J. Urban Ecol. 2019, 5, juz006. [Google Scholar] [CrossRef]
- van den Hurk, A.F.; Hall-Mendelin, S.; Webb, C.E.; Tan, C.S.E.; Frentiu, F.D.; Prow, N.A.; Hall, R.A. Role of enhanced vector transmission of a new West Nile virus strain in an outbreak of equine disease in Australia in 2011. Parasit. Vectors 2014, 7, 586. [Google Scholar] [CrossRef]
- Langevin, S.A.; Brault, A.C.; Panella, N.A.; Bowen, R.A.; Komar, N. Variation in virulence of West Nile virus strains for house sparrows (Passer domesticus). Am. J. Trop. Med. Hyg. 2005, 72, 99–102. [Google Scholar] [CrossRef] [Green Version]
- Tiawsirisup, S.; Platt, K.B.; Tucker, B.J.; Rowley, W.A. Eastern cottontail rabbits (Sylvilagus floridanus) develop West Nile virus viremias sufficient for infecting select mosquito species. Vector Borne Zoonotic Dis. 2005, 5, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Suen, W.; Prow, N.; Wang, W.; Broad, N.; Hall, R.; Kirkland, P.; Bielefeldt-Ohmann, H. The establishment of a rabbit model to elucidate the mechanism of neuroinvasion by an emergent Australian West Nile virus, In Proceedings of the 7th Australasian Virology Society Meeting, Queenstown, New Zealand, 8–11 December 2013.
- Austgen, L.E.; Bowen, R.A.; Bunning, M.L.; Davis, B.S.; Mitchell, C.J.; Chang, G.-J.J. Experimental infection of cats and dogs with West Nile virus. Emerg. Infect. Dis. 2004, 10, 82. [Google Scholar] [CrossRef] [PubMed]
- Hanna, J.N.; Ritchie, S.A.; Phillips, D.A.; Shield, J.; Bailey, M.C.; Mackenzie, J.S.; Poidinger, M.; McCall, B.J.; Mills, P.J. An outbreak of Japanese encephalitis in the Torres Strait, Australia, 1995. Med. J. Aust. 1996, 165, 256–260. [Google Scholar] [CrossRef] [PubMed]
- Hanna, J.N.; Ritchie, S.A.; Hills, S.L.; van den Hurk, A.F.; Phillips, D.A.; Pyke, A.T.; Lee, J.M.; Johansen, C.A.; Mackenzie, J.S. Japanese encephalitis in north Queensland, Australia, 1998. Med. J. Aust. 1999, 170, 533–536. [Google Scholar] [CrossRef]
- Burke, D.; Leake, C. Japanese encephalitis. In Arboviruses: Epidemiology and Ecology; Monath, T., Ed.; CRC Press: Boca Raton, FL, USA, 1988. [Google Scholar]
- Ompusunggu, S.; Hills, S.L.; Maha, M.S.; Moniaga, V.A.; Susilarini, N.K.; Widjaya, A.; Sasmito, A.; Suwandono, A.; Sedyaningsih, E.R.; Jacobson, J.A. Confirmation of Japanese encephalitis as an endemic human disease through sentinel surveillance in Indonesia. Am. J. Trop. Med. Hyg. 2008, 79, 963–970. [Google Scholar] [CrossRef]
- Halstead, S.B.; Jacobson, J. Japanese encephalitis. Adv. Virus Res. 2003, 61, 103–138. [Google Scholar]
- van den Hurk, A.F.; Ritchie, S.A.; Johansen, C.A.; Mackenzie, J.S.; Smith, G.A. Domestic pigs and Japanese encephalitis virus infection, Australia. Emerg. Infect. Dis. 2008, 14, 1736. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.I.; Kweon, C.H.; Tark, D.S.; Kim, S.H.; Yang, D.K. Sero-survey on Aino, Akabane, Chuzan, bovine ephemeral fever and Japanese encephalitis virus of cattle and swine in Korea. J. Vet. Sci. 2007, 8, 45–49. [Google Scholar] [CrossRef] [Green Version]
- van den Hurk, A.F.; Smith, C.S.; Field, H.E.; Smith, I.L.; Northill, J.A.; Taylor, C.T.; Jansen, C.C.; Smith, G.A.; Mackenzie, J.S. Transmission of Japanese encephalitis virus from the black flying fox, Pteropus alecto, to Culex annulirostris mosquitoes, despite the absence of detectable viremia. Am. J. Trop. Med. Hyg. 2009, 81, 457–462. [Google Scholar] [CrossRef] [Green Version]
- Russell, R. Arboviruses and their vectors in Australia: An update on the ecology and epidemiology of some mosquito-borne arboviruses. Rev. Med. Vet. Entomol. 1995, 83, 141–158. [Google Scholar]
- Mackenzie, J.; Lindsay, M.; Coelen, R.; Broom, A.; Hall, R.; Smith, D. Arboviruses causing human disease in the Australasian zoogeographic region. Arch. Virol. 1994, 136, 447–467. [Google Scholar] [CrossRef] [PubMed]
- Toi, C.S.; Webb, C.E.; Haniotis, J.; Clancy, J.; Doggett, S.L. Seasonal activity, vector relationships and genetic analysis of mosquito-borne Stratford virus. PLoS ONE 2017, 12, e0173105. [Google Scholar] [CrossRef] [Green Version]
- Doherty, R.L.; Carley, J.; Gorman, B.M.; Buchanan, P.; Welch, J.; Whitehead, R. Studies of arthropod-borne virus infections in Queensland: IV. Further serological investigations of antibodies to group B arboviruses in man and animals. Aust. J. Exp. Biol. Med. Sci. 1964, 42, 149–164. [Google Scholar] [CrossRef]
- May, F.J.; Clark, D.C.; Pham, K.; Diviney, S.M.; Williams, D.T.; Field, E.J.; Kuno, G.; Chang, G.-J.; Cheah, W.Y.; Setoh, Y.X.; et al. Genetic divergence among members of the Kokobera group of flaviviruses supports their separation into distinct species. J. Gen. Virol. 2013, 94, 1462–1467. [Google Scholar] [CrossRef]
- Briese, T.; Williams, D.T.; Kapoor, V.; Diviney, S.M.; Certoma, A.; Wang, J.; Johansen, C.A.; Chowdhary, R.; Mackenzie, J.S.; Lipkin, W.I. Analysis of arbovirus isolates from Australia identifies novel bunyaviruses including a Mapputta group virus from Western Australia that links Gan Gan and Maprik viruses. PLoS ONE 2016, 11, e0164868. [Google Scholar] [CrossRef]
- Gard, G.; Marshall, I.D.; Woodroofe, G.M. Annually recurrent epidemic polyarthritis and Ross River virus activity in a coastal area of New South Wales: II. Mosquitoes, viruses, and wildlife. Am. J. Trop. Med. Hyg. 1973, 22, 551–560. [Google Scholar] [CrossRef] [PubMed]
- Doherty, R.; Whitehead, R.; Wetters, E.J.; Gorman, B. Studies of the epidemiology of arthropod-borne virus infections at Mitchell River Mission, Cape York Peninsula, North Queensland: II. Arbovirus infections of mosquitoes, man and domestic fowls, 1963–1966. Trans. R. Soc. Trop. Med. Hyg. 1968, 62, 430–438. [Google Scholar] [CrossRef]
- Weir, R.P. Classification and Identification of Viruses Isolated from Mosquitoes in the Northern Territory, 1982–1992, Using a Range of Techniques. Ph.D. Thesis, University of Sydney, Sydney, Australia, 2002. [Google Scholar]
- Johansen, C.A.; Mackenzie, J.S.; Smith, D.W.; Lindsay, M.D.A. Prevalence of neutralising antibodies to Barmah Forest, Sindbis and Trubanaman viruses in animals and humans in the south-west of Western Australia. Aust. J. Zool. 2005, 53, 51–58. [Google Scholar] [CrossRef]
- Johnson, C.N.; Isaac, J.L.; Fisher, D.O. Rarity of a top predator triggers continent-wide collapse of mammal prey: Dingoes and marsupials in Australia. Proc. R. Soc. Lond. B Biol. Sci. 2006, 274, 341–346. [Google Scholar] [CrossRef]
- Old, J.M.; Deane, E.M. The detection of mature T-and B-cells during development of the lymphoid tissues of the tammar wallaby (Macropus eugenii). J. Anat. 2003, 203, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Old, J.M.; Selwood, L.; Deane, E.M. The appearance and distribution of mature T and B cells in the developing immune tissues of the stripe-faced dunnart (Sminthopsis macroura). J. Anat. 2004, 205, 25–33. [Google Scholar] [CrossRef]
- Wilson, D.; Fox, D.; Rowlands, D., Jr. Proliferative reactivity of opossum peripheral blood leukocytes to allogeneic cells, mitogens, and specific antigens. Transplantation 1976, 21, 164–167. [Google Scholar] [CrossRef]
- Stone, W.H.; Bruun, D.A.; Foster, E.B.; Manis, G.S.; Hoffman, E.S.; Saphire, D.G.; VandeBerg, J.L.; Infante, A.J. Absence of a significant mixed lymphocyte reaction in a marsupial (Monodelphis domestica). Comp. Med. 1998, 48, 184–189. [Google Scholar]
- Belov, K.; Miller, R.D.; Old, J.M.; Young, L.J. Marsupial immunology bounding ahead. Aust. J. Zool. 2013, 61, 24–40. [Google Scholar] [CrossRef]
- Mackenzie, J.S.; Gubler, D.J.; Petersen, L.R. Emerging flaviviruses: The spread and resurgence of Japanese encephalitis, West Nile and dengue viruses. Nat. Med. 2004, 10, S98. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, J.S.; van den Hurk, A.F. The risks to Australia from emerging and exotic arboviruses. Microbiol. Aust. 2018, 63, 24–27. [Google Scholar] [CrossRef]
- Lindsay, M.; Oliveira, N.; Jasinska, E.; Johansen, C.; Harrington, S.; Wright, A.; Smith, D. An outbreak of Ross River virus disease in Southwestern Australia. Emerg. Infect. Dis. 1996, 2, 117. [Google Scholar] [CrossRef] [Green Version]
- Kelly-Hope, L.A.; Purdie, D.M.; Kay, B.H. Ross River virus disease in Australia, 1886–1998, with analysis of risk factors associated with outbreaks. J. Med. Entomol. 2004, 41, 133–150. [Google Scholar] [CrossRef] [PubMed]
- Contigiani, M.S.; Diaz, L.A. Togaviridae. In Arthropod Borne Diseases; Marcondes, C., Ed.; Springer: Berlin/Heidelberg, Germany, 2017; pp. 115–135. [Google Scholar]
- Suhrbier, A.; La Linn, M. Clinical and pathologic aspects of arthritis due to Ross River virus and other alphaviruses. Curr. Opin. Rheumatol. 2004, 16, 374–379. [Google Scholar] [CrossRef]
- Togami, E.; Gyawali, N.; Ong, O.; Kam, M.; Cao-Lormeaud, V.-M.; Aubry, M.; Ko, A.I.; Nilles, E.J.; Collins-Emerson, J.M.; Devine, G.J.; et al. First evidence of concurrent enzootic and endemic transmission of Ross River virus in the absence of marsupial reservoirs in Fiji. Int. J. Infect. Dis. 2020, 96, 94–96. [Google Scholar] [CrossRef] [PubMed]
- Sammels, L.M.; Coelen, R.J.; Lindsay, M.D.; Mackenzie, J.S. Geographic distribution and evolution of Ross River virus in Australia and the Pacific Islands. Virology 1995, 212, 20–29. [Google Scholar] [CrossRef] [Green Version]
- Rosen, L.; Gubler, D.J.; Bennett, P.H. Epidemic polyarthritis (Ross River) virus infection in the Cook Islands. Am. J. Trop. Med. Hyg. 1981, 30, 294–1302. [Google Scholar] [CrossRef]
- Aubry, M.; Finke, J.; Teissier, A.; Roche, C.; Broult, J.; Paulous, S.; Desprès, P.; Cao-Lormeau, V.-M.; Musso, D. Silent circulation of ross river virus in French Polynesia. Int. J. Infect. Dis. 2015, 37, 19–24. [Google Scholar] [CrossRef] [Green Version]
- Harley, D.; Sleigh, A.; Ritchie, S. Ross River virus transmission, infection, and disease: A cross-disciplinary review. Clin. Microbiol. Rev. 2001, 14, 909–932. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Claflin, S.B.; Webb, C.E. Ross River virus: Many vectors and unusual hosts make for an unpredictable pathogen. PLoS Pathog. 2015, 11, e1005070. [Google Scholar] [CrossRef] [Green Version]
- Johnson, B.J.; Robbins, A.; Gyawali, N.; Ong, O.; Loader, J.; Murphy, A.K.; Hanger, J.; Devine, G.J. The environmental and ecological determinants of elevated Ross River Virus exposure in koalas residing in urban coastal landscapes. Sci. Rep. 2021. under review. [Google Scholar]
- Kay, B.; Hall, R.; Fanning, I.; Mottram, P.; Young, P.; Pollitt, C. Experimental infection of vertebrates with Murray Valley encephalitis and Ross River viruses. Arbovirus Res. Aust. 1986, 4, 71–75. [Google Scholar]
- Carver, S.; Sakalidis, V.; Weinstein, P. House mouse abundance and Ross River virus notifications in Victoria, Australia. Int. J. Infect. Dis. 2008, 12, 528–533. [Google Scholar] [CrossRef] [Green Version]
- El-Hage, C.M.; Bamford, N.J.; Gilkerson, J.R.; Lynch, S.E. Ross River Virus Infection of Horses: Appraisal of Ecological and Clinical Consequences. J. Equine Vet. Sci. 2020, 93, 103143. [Google Scholar] [CrossRef]
- Gummow, B.; Tan, R.; Joice, R.; Burgess, G.; Picard, J. Seroprevalence and associated risk factors of mosquito-borne alphaviruses in horses in northern Queensland. Aust. Vet. J. 2018, 96, 243–251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gordon, J. The Horse Industry; Rural Industries Research and Development Corporation: Kingston, Australia, 2001; pp. 1–7. [Google Scholar]
- Skinner, E.B.; Murphy, A.; Jansen, C.C.; Shivas, M.A.; McCallum, H.; Onn, M.B.; Reid, S.A.; Peel, A.J. Associations Between Ross River Virus Infection in Humans and Vector-Vertebrate Community Ecology in Brisbane, Australia. Vector Borne Zoonotic Dis. 2020, 20, 680–691. [Google Scholar] [CrossRef] [PubMed]
- Skinner, E.B.; Rudd, P.A.; Peel, A.J.; McCallum, H.; Reid, S.A.; Herrero, L.J. Species Traits and Hotspots Associated with Ross River Virus Infection in Nonhuman Vertebrates in South East Queensland. Vector Borne Zoonotic Dis. 2020, 21, 50–58. [Google Scholar] [CrossRef]
- Walsh, M.G.; Webb, C. Hydrological features and the ecological niches of mammalian hosts delineate elevated risk for Ross River virus epidemics in anthropogenic landscapes in Australia. Parasit. Vectors 2018, 11, 192. [Google Scholar] [CrossRef]
- Walsh, M.G. Ecological and life history traits are associated with Ross River virus infection among sylvatic mammals in Australia. BMC Ecol. 2019, 19, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flaxman, J.P.; Smith, D.W.; Mackenzie, J.S.; Fraser, J.; Bass, S.P.; Hueston, L.; Lindsay, M.D.; Cunningham, A.L. A comparison of the diseases caused by Ross River virus and Barmah Forest virus. Med. J. Aust. 1998, 169, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Marshall, I.D.; Woodroofe, G.M.; Hirsch, S. Viruses recovered from mosquitoes and wildlife serum collected in the Murray Valley of south-eastern Australia, February 1974, during an epidemic of encephalitis. Aust. J. Exp. Biol. Med. Sci. 1982, 60, 457–470. [Google Scholar] [CrossRef] [PubMed]
- Kizu, J.; Neuman, C.; Le Grand, L.; Liu, W. Discovery of Cocirculating Ross River Virus and Barmah Forest Virus At Wide Bay Military Training Area, Northeastern Australia. J. Am. Mosq. Control Assoc. 2019, 35, 220–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lindsay, M.D.; Johansen, C.A.; Wallace, M.J.; Mackenzie, J.S.; Smith, D.W. An outbreak of Barmah Forest virus disease in the south-west of Western Australia. Med. J. Aust. 1995, 162, 291–294. [Google Scholar] [CrossRef]
- Doggett, S.L.; Russell, R.C.; Clancy, J.; Haniotis, J.; Cloonan, M.J. Barmah Forest virus epidemic on the south coast of New South Wales, Australia, 1994–1995: Viruses, vectors, human cases, and environmental factors. J. Med. Entomol. 1999, 36, 861–868. [Google Scholar] [CrossRef]
- Ryan, P.; Do, K.-A.; Kay, B. Definition of Ross River virus vectors at Maroochy shire, Australia. J. Med. Entomol. 2000, 37, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Hawkes, R.A.; Nairn, H.M.; Myrick, B.M.; Ramsay, L.G. Barmah Forest virus infections in humans in New South Wales. Med. J. Aust. 1987, 146, 569–573. [Google Scholar] [CrossRef]
- Merianos, A.; Farland, A.; Patel, M.; Currie, B.; Whelan, P.; Dentith, H.; Smith, D. A concurrent outbreak of Barmah Forest and Ross River virus disease in Nhulunbuy, Northern Territory. Commun. Dis. Intell. 1992, 16, 110–111. [Google Scholar]
- Whelan, P.; Weir, R. The isolation of alpha and flavi viruses from mosquitoes in the Northern Territory 1982–1992. Arbovirus Res. Aust. 1993, 6, 270–278. [Google Scholar]
- Kay, B.H.; Watson, T.M. Vector Competence of Aedes notoscriptus (Diptera: Culicidae) for Barmah Forest Virus and of Aedes aegypti (Diptera: Culicidae) for Dengue 1–4 Viruses in Queensland, Australia. J. Med. Entomol. 1999, 36, 508–514. [Google Scholar]
- Boyd, A.M.; Kay, B.H. Vector Competence of Aedes aegypti, Culex sitiens, Culex annulirostris, and Culex quinquefasciatus (Diptera: Culicidae) for Barmah Forest Virus. J. Med. Entomol. 2000, 37, 660–663. [Google Scholar] [CrossRef] [Green Version]
- Van Buynder, P.; Sam, G.; Russel, R. Barmah Forest virus epidemic on the south coast of New South Wales. Commun. Dis. Intell. 1995, 19, 188–191. [Google Scholar]
- Boyd, A.; Kay, B. Solving the urban puzzle of Ross River and Barmah Forest viruses. Arbrovirus Res. Aust. 2001, 8, 14–22. [Google Scholar]
- Muturi, E.J.; Alto, B.W. Larval environmental temperature and insecticide exposure alter Aedes aegypti competence for arboviruses. Vector Borne Zoonotic Dis. 2011, 11, 1157–1163. [Google Scholar] [CrossRef]
- Buckley, A.; Dawson, A.; Moss, S.R.; Hinsley, S.A.; Bellamy, P.E.; Gould, E.A. Serological evidence of West Nile virus, Usutu virus and Sindbis virus infection of birds in the UK. J. Gen. Virol. 2003, 84, 2807–2817. [Google Scholar] [CrossRef]
- Kurkela, S.; Rätti, O.; Huhtamo, E.; Uzcátegui, N.Y.; Nuorti, J.P.; Laakkonen, J.; Manni, T.; Helle, P.; Vaheri, A.; Vapalahti, O. Sindbis virus infection in resident birds, migratory birds, and humans, Finland. Emerg. Infect. Dis. 2008, 14, 41. [Google Scholar] [CrossRef]
- McIntosh, B.; Madsen, W.; Dickinson, D. Ecological studies on Sindbis and West Nile viruses in South Africa. VI. The antibody response of wild birds. S. Afr. J. Med. Sci. 1969, 34, 83–91. [Google Scholar]
- Hesson, J.C.; Lundström, J.O.; Tok, A.; Östman, Ö.; Lundkvist, Å. Temporal variation in Sindbis virus antibody prevalence in bird hosts in an endemic area in Sweden. PLoS ONE 2016, 11, e0162005. [Google Scholar]
- Knox, J.; Cowan, R.; Doyle, J.; Ligtermoet, M.; Archer, J.; Burrow, J.; Tong, S.; Currie, B.; Mackenzie, J.; Smith, D. Murray Valley encephalitis: A review of clinical features, diagnosis and treatment. Med. J. Aust. 2012, 196, 322–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Selvey, L.A.; Dailey, L.; Lindsay, M.; Armstrong, P.; Tobin, S.; Koehler, A.P.; Markey, P.G.; Smith, D.W. The Changing Epidemiology of Murray Valley Encephalitis in Australia: The 2011 Outbreak and a Review of the Literature. PLoS Negl. Trop. Dis. 2014, 8, e2656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- French, E.; Anderson, S.; Price, A.; Rhodes, F. Murray Valley Encephalitis in New Guinea. Am. J. Trop. Med. Hyg. 1957, 6, 827–834. [Google Scholar] [CrossRef] [PubMed]
- Essed, W.; Van Tongeren, H. Arthropod-Borne Virus Infections in Western New Guinea. I. Report of a Case of Murray Valley Encephalitis in a Papuan Woman. Trop. Geogr. Med. 1965, 17, 52–55. [Google Scholar]
- Kay, B.H.; Fanning, I.D.; Mottram, P. The vector competence of Culex annulirostris, Aedes sagax and Aedes alboannulatus for Murray Valley encephalitis virus at different temperatures. Med. Vet. Entomol. 1989, 3, 107–112. [Google Scholar] [CrossRef]
- Kay, B.; Fanning, I.; Carley, J. Vector competence of Culex pipiens quinquefasciatus for Murray Valley encephalitis, Kunjin, and Ross River viruses from Australia. Am. J. Trop. Med. Hyg. 1982, 31, 844–848. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S. Murray Valley encephalitis: A survey of avian sera, 1951–1952. J. Med. 1953, 1, 573–576. [Google Scholar] [CrossRef]
- Miles, J.; Howes, D. Observations on virus encaphalitis in South Australia. Med. J. Aust. 1953, 1, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Cella, E.; Gabrielli, I.; Zehender, G.; Giovanetti, M.; Presti, A.L.; Lai, A.; Dicuonzo, G.; Angeletti, S.; Salemi, M.; Ciccozzi, M. Phylogeny of Murray Valley encephalitis virus in Australia and Papua New Guinea. Asian Pac. J. Trop. Med. 2016, 9, 385–389. [Google Scholar] [CrossRef] [Green Version]
- Hayes, C.G. West Nile Virus: Uganda, 1937, to New York City, 1999. Ann. N. Y. Acad. Sci. 2001, 951, 25–37. [Google Scholar] [CrossRef]
- May, F.J.; Davis, C.T.; Tesh, R.B.; Barrett, A.D. Phylogeography of West Nile virus: From the cradle of evolution in Africa to Eurasia, Australia, and the Americas. J. Virol. 2011, 85, 2964–2974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doherty, R.L.; Carley, J.; Mackerras, M.J.; Marks, E.N. Studies of arthropod-borne virus infections in Queensland: III. Isolation and characterization of virus strains from wild-caught mosquitoes in Northern Queensland. Aust. J. Exp. Biol. Med. Sci. 1963, 41, 17–39. [Google Scholar] [CrossRef] [PubMed]
- Blitvich, B.J. Transmission dynamics and changing epidemiology of West Nile virus. Anim. Health Res. Rev. 2008, 9, 71–86. [Google Scholar] [CrossRef]
- Root, J.J. West Nile virus associations in wild mammals: A synthesis. Arch. Virol. 2013, 158, 735–752. [Google Scholar] [CrossRef]
- Gómez, A.; Kilpatrick, A.M.; Kramer, L.D.; Dupuis, A.P. Land use and West Nile virus seroprevalence in wild mammals. Emerg. Infect. Dis. 2008, 14, 962. [Google Scholar] [CrossRef]
- Goodman, H.; Egizi, A.; Fonseca, D.M.; Leisnham, P.T.; LaDeau, S.L. Primary blood-hosts of mosquitoes are influenced by social and ecological conditions in a complex urban landscape. Parasit. Vectors 2018, 11, 218. [Google Scholar] [CrossRef]
- Root, J.J.; Hall, J.S.; Mclean, R.G.; Marlenee, N.L.; Beaty, B.J.; Gansowski, J.; Clark, L. Serologic evidence of exposure of wild mammals to flaviviruses in the central and eastern United States. Am. J. Trop. Hyg. Med. 2005, 72, 622–630. [Google Scholar] [CrossRef] [Green Version]
- Docherty, D.E.; Samuel, M.D.; Nolden, C.A.; Egstad, K.F.; Griffin, K.M. West Nile virus antibody prevalence in wild mammals, Southern Wisconsin. Emerg. Infect. Dis. 2006, 12, 1982. [Google Scholar] [CrossRef] [Green Version]
- Bentler, K.T.; Hall, J.S.; Root, J.J.; Klenk, K.; Schmit, B.; Blackwell, B.F.; Ramey, P.C.; Clark, L. Serologic evidence of West Nile virus exposure in North American mesopredators. Am. J. Trop. Hyg. Med. 2007, 76, 173–179. [Google Scholar] [CrossRef] [Green Version]
- Lamglait, B.; Lair, S. Fatal West Nile virus infection in a Virginia opossum (Didelphis virginiana) with pulmonary lepidic-predominant adenocarcinoma. J. Wildl. Dis. 2019, 55, 990–994. [Google Scholar] [CrossRef]
- Russell, R. Transport of insects of public health importance on international aircraft. Travel Med. Int. 1989, 7, 26–31. [Google Scholar]
- Ritchie, S.A.; Rochester, W. Wind-blown mosquitoes and introduction of Japanese encephalitis into Australia. Emerg. Infect. Dis. 2001, 7, 900. [Google Scholar] [CrossRef] [PubMed]
- Fischer, M.; Hills, S.; Staples, E.; Johnson, B.; Yaich, M.; Solomon, T. Japanese encephalitis prevention and control: Advances, challenges, and new initiatives. In Emerging Infections 8; Scheld, W., Hammer, S., Hughes, J.M., Eds.; American Society of Microbiology: Washington, DC, USA, 2008; pp. 93–124. [Google Scholar]
- Cui, J.; Counor, D.; Shen, D.; Sun, G.; He, H.; Deubel, V.; Zhang, S. Detection of Japanese encephalitis virus antibodies in bats in Southern China. Am. J. Trop. Med. Hyg. 2008, 78, 1007–1011. [Google Scholar] [CrossRef] [PubMed]
- Webb, N.; Tidemann, C. Mobility of Australian flying-foxes, Pteropus spp.(Megachiroptera): Evidence from genetic variation. Proc. R. Soc. Lond. B Biol. Sci. 1996, 263, 497–502. [Google Scholar]
- Calisher, C.H.; Childs, J.E.; Field, H.E.; Holmes, K.V.; Schountz, T. Bats: Important reservoir hosts of emerging viruses. Clin. Microbiol. Rev. 2006, 19, 531–545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, S.; Lau, S.; Woo, P.; Yuen, K.Y. Bats as a continuing source of emerging infections in humans. Rev. Med. Virol. 2007, 17, 67–91. [Google Scholar] [CrossRef]
- Field, H.; de Jong, C.; Melville, D.F.; Smith, C.; Smith, I.; Broos, A.; Kung, N.Y.; McLaughlin, A.; Zeddeman, A. Hendra virus infection dynamics in Australian fruit bats. PLoS ONE 2011, 6, e28678. [Google Scholar] [CrossRef] [PubMed]
- McMichael, L.; Eson, D.; Smith, C.; Mayer, D.; Smith, I.; Kopp, S.; Meers, J.; Field, H. Physiological stress and Hendra virus in flying foxes (Pteropus spp.), Australia. PLoS ONE 2017, 12, e182171. [Google Scholar]
- Nisbet, D.J.; Lee, K.J.; van den Hurk, A.F.; Johansen, C.A.; Kuno, G.; Chang, G.-J.J.; Mackenzie, J.S.; Ritchie, S.A.; Hall, R.A. Identification of new flaviviruses in the Kokobera virus complex. J. Gen. Virol. 2005, 86, 121–124. [Google Scholar] [CrossRef] [PubMed]
- Hall, R.A.; Burgess, G.W.; Kay, B.H.; Clancy, P. Monoclonal antibodies to Kunjin and Kokobera viruses. Immunol. Cell Biol. 1991, 69, 47–49. [Google Scholar] [CrossRef]
- Poidinger, M.; Hall, R.A.; Mackenzie, J.S. Molecular characterization of the Japanese encephalitis serocomplex of the flavivirus genus. Virology 1996, 218, 17–421. [Google Scholar] [CrossRef]
- Johansen, C.A.; Nisbet, D.J.; Foley, P.N.; Van Den Hurk, A.F.; Hall, R.A.; Mackenzie, J.S.; Ritchie, S.A. Flavivirus isolations from mosquitoes collected from Saibai Island in the Torres Strait, Australia, during an incursion of Japanese encephalitis virus. Med. Vet. Entomol. 2004, 18, 281–287. [Google Scholar] [CrossRef]
- Miura, Y.; Inaba, Y.; Tsuda, T.; Tokuhisa, S.; Sato, K.; Akashi, H.; Matumoto, M. A Survey of Antibodies to Arthropod-Borne Viruses in Indonesian Cattle. Jpn. J. Vet. Res. 1982, 44, 857–863. [Google Scholar] [CrossRef] [Green Version]
- Mackenzie, J.; Williams, D. The zoonotic flaviviruses of Southern, South-Eastern and Eastern Asia, and Australasia: The potential for emergent viruses. Zoonoses Public Health 2009, 56, 338–356. [Google Scholar] [CrossRef]
- Blasi, A.; Presti, A.L.; Cella, E.; Angeletti, S.; Ciccozzi, M. The phylogenetic and evolutionary history of Kokobera virus. Asian Pac. J. Trop. Med. 2016, 9, 968–972. [Google Scholar] [CrossRef] [Green Version]
- Warrilow, D.; Hall-Mendelin, S.; Hobson-Peters, J.; Prow, N.A.; Allcock, R.; Hall, R.A. Complete coding sequences of three members of the Kokobera group of flaviviruses. Genome Announc. 2014, 2, e00890–e14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gauci, P.J.; McAllister, J.; Mitchell, I.R.; Weir, R.P.; Melville, L.F.; Gubala, A.J. Genomic characterisation of Trubanaman and Gan Gan viruses, two bunyaviruses with potential significance to public health in Australia. Virol. Rep. 2016, 6, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Boughton, C.; Hawkes, R.; Naim, H. Arbovirus infection in humans in NSW: Seroprevalence and pathogenicity of certain Australian bunyaviruses. Aust. N. Z. J. Med. 1990, 20, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Walter, C.T.; Barr, J.N. Recent advances in the molecular and cellular biology of bunyaviruses. J. Gen. Virol. 2011, 92, 2467–2484. [Google Scholar] [CrossRef]
- Bartlow, A.W.; Manore, C.; Xu, C.; Kaufeld, K.A.; Del Valle, S.; Ziemann, A.; Fairchild, G.; Fair, J.M. Forecasting zoonotic infectious disease response to climate change: Mosquito vectors and a changing environment. Vet. Sci. 2019, 6, 40. [Google Scholar] [CrossRef] [Green Version]
- Yu, W.; Dale, P.; Turner, L.; Tong, S. Projecting the impact of climate change on the transmission of Ross River virus: Methodological challenges and research needs. Epidemiol. Infect. 2014, 142, 2013–2023. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patz, J.A.; Graczyk, T.K.; Geller, N.; Vittor, A.Y. Effects of environmental change on emerging parasitic diseases. Int. J. Parasitol. 2000, 30, 1395–1405. [Google Scholar] [CrossRef] [Green Version]
- Scott, T.W.; Clark, G.G.; Lorenz, L.H.; Amerasinghe, P.H.; Reiter, P.; Edman, J.D. Detection of multiple blood feeding in Aedes aegypti (Diptera: Culicidae) during a single gonotrophic cycle using a histologic technique. J. Med. Entomol. 1993, 30, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Loehle, C.; Eschenbach, W. Historical bird and terrestrial mammal extinction rates and causes. Divers. Distrib. 2012, 18, 84–91. [Google Scholar] [CrossRef]
- Urban, M.C. Accelerating extinction risk from climate change. Science 2015, 348, 571–573. [Google Scholar] [CrossRef] [Green Version]
- Schmidt, K.A.; Ostfeld, R.S. Biodiversity and the dilution effect in disease ecology. Ecology 2001, 82, 609–619. [Google Scholar] [CrossRef]
- Bradley, C.A.; Altizer, S. Urbanization and the ecology of wildlife diseases. Trends Ecol. Evol. 2007, 22, 95–102. [Google Scholar] [CrossRef] [PubMed]
- LoGiudice, K.; Ostfeld, R.S.; Schmidt, K.A.; Keesing, F. The ecology of infectious disease: Effects of host diversity and community composition on Lyme disease risk. Proc. Natl. Acad. Sci. USA 2003, 100, 567–571. [Google Scholar] [CrossRef] [Green Version]
- Russell, R. Survival of insects in the wheel bays of a Boeing 747B aircraft on flights between tropical and temperate airports. Bull. World Health Organ. 1987, 65, 659. [Google Scholar]
- Gratz, N.G.; Steffen, R.; Cocksedge, W. Why aircraft disinsection? Bull. World Health Organ. 2000, 78, 995–1004. [Google Scholar]
- Baldwin, C.; Ross, H. Our warming climate and fire’s role in the Australian landscape. Australas. J. Environ. Manag. 2019, 26, 305–310. [Google Scholar] [CrossRef]
- Biondi, M.; Zannino, L.-G. Psychological stress, neuroimmunomodulation, and susceptibility to infectious diseases in animals and man: A review. Psychother. Psychosom. 1997, 66, 3–26. [Google Scholar] [CrossRef]
- Pickrell, J. Australian blazes will ‘reframe our understanding of bushfire’. Science 2019, 366, 937. [Google Scholar] [CrossRef] [PubMed]
- Behera, S.; Sahu, S.; Pradhan, B. Bushfire Study: Causes, effects and risks to the ecosystem due to changes in climate. Int. J. Mod. Agric. 2020, 9, 579–589. [Google Scholar]
- Wallis, R.L. Koalas Phascolarctos cinereus in Framlingham Forest, south-west Victoria: Introduction, translocation and the effects of a bushfire. Vic. Nat. 2013, 130, 37. [Google Scholar]
- Bain, K.; Halley, M.; Barton, B.; Wayne, A.; McGilvray, A.; Wilson, I.; Wayne, J. Survival of Quokkas in the 2015 Northcliffe Bush Fire: Understanding the Impact of Intense and Broadscale Fire on an Important Population of Quokkas in the Southern Forest of Western Australia; WWF Australia: Wembley, Australia, 2016; p. 34. [Google Scholar]
- Russell, B.; Smith, B.; Augee, M. Changes to a population of common ringtail possums (Pseudocheirus peregrinus) after bushfire. Wildl. Res. 2003, 30, 389–396. [Google Scholar] [CrossRef]
- Kiem, A.S.; Johnson, F.; Westra, S.; van Dijk, A.; Evans, J.P.; O’Donnell, A.; Rouillard, A.; Barr, C.; Tyler, J.; Thyer, M. Natural hazards in Australia: Droughts. Clim. Chang. 2016, 139, 37–54. [Google Scholar] [CrossRef]
- Johnson, B.J.; Fonseca, D.M. The effects of forced-egg retention on the blood-feeding behavior and reproductive potential of Culex pipiens (Diptera: Culicidae). J. Insect Physiol. 2014, 66, 53–58. [Google Scholar] [CrossRef]
- Smartt, C.T.; Richards, S.L.; Anderson, S.L.; Vitek, C.J. Effects of forced egg retention on the temporal progression of West Nile virus infection in Culex pipiens quinquefasciatus (Diptera: Culicidae). Environ. Entomol. 2010, 39, 190–194. [Google Scholar] [CrossRef]
- Townroe, S.; Callaghan, A. British container breeding mosquitoes: The impact of urbanisation and climate change on community composition and phenology. PLoS ONE 2014, 9, e95325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beebe, N.W.; Cooper, R.D.; Mottram, P.; Sweeney, A.W. Australia’s dengue risk driven by human adaptation to climate change. Plos Negl. Trop. Dis. 2009, 3, e429. [Google Scholar] [CrossRef]
- Epstein, P. The ecology of climate change and infectious diseases: Comment. Ecology 2010, 91, 925–928. [Google Scholar] [CrossRef] [PubMed]
- Parrott, M.L.; Ward, S.J.; Temple-Smith, P.D.; Selwood, L. Effects of drought on weight, survival and breeding success of agile antechinus (Antechinus agilis), dusky antechinus (A. swainsonii) and bush rats (Rattus fuscipes). Wildl. Res. 2007, 34, 437–442. [Google Scholar] [CrossRef]
- Rhind, S. Reproductive demographics among brush-tailed phascogales (Phascogale tapoatafa) in south-western Australia. Wildl. Res. 2002, 29, 247–257. [Google Scholar] [CrossRef]
- Pople, A.R.; Phinn, S.R.; Menke, N.; Grigg, G.C.; Possingham, H.P.; McAlpine, C. Spatial patterns of kangaroo density across the South Australian pastoral zone over 26 years: Aggregation during drought and suggestions of long distance movement. J. Appl. Ecol. 2007, 44, 1068–1079. [Google Scholar] [CrossRef]
- Taylor-Brown, A.; Booth, R.; Gillett, A.; Mealy, E.; Ogbourne, S.M.; Polkinghorne, A.; Conroy, G.C. The impact of human activities on Australian wildlife. PLoS ONE 2019, 14, e0206958. [Google Scholar] [CrossRef] [Green Version]
- McKechnie, A.E.; Wolf, B.O. The physiology of heat tolerance in small endotherms. Physiology 2019, 34, 302–313. [Google Scholar] [CrossRef] [PubMed]
- Cleugh, H.; Cleugh, H.; Smith, M.S.; Battaglia, M.; Graham, P. Climate Change: Science and Solutions for Australia; CSIRO Publishing: Collinwood, Australia, 2011. [Google Scholar]
- Mackenzie, J.; Lindsay, M.; Broom, A. Climate changes and vector-borne diseases: Potential consequences for human health. In Health in the Greenhouse: The Medical and Environmental Health Effects of Global Climate Change; Ewan, C.E., Bryant, E.A., Calvert, C.D., Carrick, J.A., Eds.; Australian Government Publishing Service: Canberra, Australia, 1993; pp. 229–234. [Google Scholar]
- Hanna, J.N.; Ritchie, S.A. Outbreaks of dengue in north Queensland, 1990–2008. Commun. Dis. Intell. 2009, 33, 32. [Google Scholar]
- Williams, C.R.; Mincham, G.; Ritchie, S.A.; Viennet, E.; Harley, D. Bionomic response of Aedes aegypti to two future climate change scenarios in far north Queensland, Australia: Implications for dengue outbreaks. Parasit. Vectors 2014, 7, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Samy, A.M.; Elaagip, A.H.; Kenawy, M.A.; Ayres, C.F.; Peterson, A.T.; Soliman, D.E. Climate change influences on the global potential distribution of the mosquito Culex quinquefasciatus, vector of West Nile virus and lymphatic filariasis. PLoS ONE 2016, 11, e0163863. [Google Scholar] [CrossRef]
- Ren, Z.; Wang, D.; Ma, A.; Hwang, J.; Bennett, A.; Sturrock, H.J.; Fan, J.; Zhang, W.; Yang, D.; Feng, X. Predicting malaria vector distribution under climate change scenarios in China: Challenges for malaria elimination. Sci. Rep. 2016, 6, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brady, O.J.; Golding, N.; Pigott, D.M.; Kraemer, M.U.; Messina, J.P.; Reiner, R.C., Jr.; Scott, T.W.; Smith, D.L.; Gething, P.W.; Hay, S.I. Global temperature constraints on Aedes aegypti and Ae. albopictus persistence and competence for dengue virus transmission. Parasit. Vectors 2014, 7, 338. [Google Scholar] [CrossRef] [Green Version]
- Faull, K.J.; Williams, C.R. Intraspecific variation in desiccation survival time of Aedes aegypti (L.) mosquito eggs of Australian origin. J. Vector Ecol. 2015, 40, 292–300. [Google Scholar] [CrossRef] [Green Version]
- Costa, E.A.P.A.; Santos, E.M.M.; Correia, J.C.; Albuquerque, C.M.R. Impact of small variations in temperature and humidity on the reproductive activity and survival of Aedes aegypti (Diptera, Culicidae). Rev. Bras. Entomol. 2010, 54, 488–493. [Google Scholar] [CrossRef] [Green Version]
- Parker, V.T.; Boyer, K.E. Sea-level rise and climate change impacts on an urbanized Pacific Coast estuary. Wetlands 2019, 39, 1219–1232. [Google Scholar] [CrossRef]
- Ramasamy, R.; Surendran, S.N. Possible impact of rising sea levels on vector-borne infectious diseases. BMC Infect. Dis. 2011, 11, 18. [Google Scholar] [CrossRef] [Green Version]
- Van Schie, C.; Spafford, H.; Carver, S.; Weinstein, P. Salinity tolerance of Aedes camptorhynchus (Diptera: Culicidae) from two regions in southwestern Australia. Austral. Entomol. 2009, 48, 293–299. [Google Scholar] [CrossRef]
- Ryan, P.; Alsemgeest, D.; Gatton, M.; Kay, B. Ross River virus disease clusters and spatial relationship with mosquito biting exposure in Redland Shire, southern Queensland, Australia. J. Med. Entomol. 2006, 43, 1042–1059. [Google Scholar] [CrossRef]
- Johnson, B.J.; Manby, R.; Devine, G.J. What happens on islands, doesn’t stay on islands: Patterns of synchronicity in mosquito nuisance and host-seeking activity between a mangrove island and adjacent coastal development. Urban Ecosyst. 2020, 23, 1321–1333. [Google Scholar] [CrossRef]
- Taylor, L.H.; Latham, S.M.; Woolhouse, M.E. Risk factors for human disease emergence. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2001, 356, 983–989. [Google Scholar] [CrossRef]
- McFarlane, R.; Sleigh, A.; McMichael, A. Land-use change and emerging infectious disease on an island continent. Int. J. Environ. Res. Public Health 2013, 10, 2699–2719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brunton, E.A.; Srivastava, S.K.; Schoeman, D.S.; Burnett, S. Quantifying trends and predictors of decline in eastern grey kangaroo (Macropus giganteus) populations in a rapidly urbanising landscape. Pac. Conserv. Biol. 2018, 24, 63–73. [Google Scholar] [CrossRef]
- Isaac, B.; White, J.; Ierodiaconou, D.; Cooke, R. Simplification of arboreal marsupial assemblages in response to increasing urbanization. PLoS ONE 2014, 9, e91049. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, B.D.; Wallis, I.R.; Wood, J.T.; Foley, W.J. Foliar nutrition, site quality, and temperature influence foliar chemistry of tallowwood (Eucalyptus microcorys). Ecol. Monogr. 2004, 74, 553–568. [Google Scholar] [CrossRef]
- Lunney, D.; Crowther, M.S.; Wallis, I.; Foley, W.J.; Lemon, J.; Wheeler, R.; Madani, G.; Orscheg, C.; Griffith, J.E.; Krockenberger, M. Koalas and climate change: A case study on the Liverpool Plains, north-west New South Wales. In Wildlife and Climate Change: Towards Robust Conservation Strategies for Australian Fauna; Lunney, D., Hutchings, P., Eds.; Royal Zoological Society of New South Wales: Mosman, Australia, 2012; pp. 150–168. [Google Scholar]
- Adams-Hosking, C.; McBride, M.F.; Baxter, G.; Burgman, M.; De Villiers, D.; Kavanagh, R.; Lawler, I.; Lunney, D.; Melzer, A.; Menkhorst, P. Use of expert knowledge to elicit population trends for the koala (Phascolarctos cinereus). Divers. Distrib. 2016, 22, 249–262. [Google Scholar] [CrossRef] [Green Version]
- De Oliveira, S.; Murray, P.; De Villiers, D.; Baxter, G. Ecology and movement of urban koalas adjacent to linear infrastructure in coastal south-east Queensland. Aust. Mammal. 2014, 36, 45–54. [Google Scholar] [CrossRef] [Green Version]
- Tarlinton, R.; Meers, J.; Hanger, J.; Young, P. Real-time reverse transcriptase PCR for the endogenous koala retrovirus reveals an association between plasma viral load and neoplastic disease in koalas. J. Gen. Virol. 2005, 86, 783–787. [Google Scholar] [CrossRef]
- Williamson, K.; Doherty, H.; Di Stefano, J. Changes in the relative density of swamp wallabies (Wallabia bicolor) and Eastern grey kangaroos (Macropus giganteus) in response to timber harvesting and wildfire. In New Advances and Contributions to Forestry Research; Oteng-Amoako, A.A., Ed.; InTech: Rijeka, Croatia, 2012; pp. 101–116. [Google Scholar]
- Hillman, A.E.; Lymbery, A.J.; Elliot, A.D.; Ash, A.L.; Thompson, R.A. Parasitic infections of brushtail possums Trichosurus vulpecula in urbanised environments and bushland in the greater Perth region, Western Australia. Wildl. Biol. 2018, 1. [Google Scholar] [CrossRef] [Green Version]
- Soulsbury, C.D.; White, P.C. Human-wildlife interactions in urban areas: A review of conflicts, benefits and opportunities. Wildl. Res. 2016, 42, 541–553. [Google Scholar] [CrossRef] [Green Version]
- Lindsay, M.; Mackenzie, J. Vector-borne viral diseases and climate change in the Australia region: Major concerns and public health response. In Climate Change and Human Health in the Asia-Pacific Region; Curson, P., Guest, C., Jackson, E., Eds.; Australian Medical Association and Greenpeace International: Canberra, Australia, 1996; pp. 47–62. [Google Scholar]
- Kay, B.; Jennings, C. Enhancement or modulation of the vector competence of Ochlerotatus vigilax (Diptera: Culicidae) for Ross River virus by temperature. J. Med. Entomol. 2002, 39, 99–105. [Google Scholar] [CrossRef] [PubMed]

| Pathogen | Pathogen Distribution in Australia | Mosquito Vectors | Asymptomatic Hosts of Pathogen in Australia | Symptomatic Hosts of Pathogen in Australia |
|---|---|---|---|---|
| Ross River virus (RRV) | All of Australia [13] | Aedes and Culex mosquitoes, particularly Aedes vigilax, Aedes camptohynchus, and Culex annulirostris [14] | Marsupials: wallabies, wallaroos [15], common brushtail possums [16], eastern grey kangaroos [17], western grey kangaroos [18] Australian birds: little corella, magpie larks, Australian brown flycatcher, masked finch [19,20] Wild eutherian mammals: rodents, Pteropus spp. [20] Domestic mammals: cattle, dogs [20], cats [21] | Domestic mammals: horses [20,22] |
| Barmah Forest virus (BFV) | All of Australia [23] | Culex annuliristris, Aedes normanensis, Aedes vigilax and Aedes procax [24] | Marsupials: eastern grey kangaroo [25], koalas [25] and brushtail possums [21]. Wild eutherian mammals: Australian bush rats and swamp rats [26] Domestic mammals: cats, dogs, horses [27] | |
| Sindbis virus (SINV) | Most of Australia (excluding Tasmania) [28] | Culex annulirostris, Aedes normanensis, Aedes camptorhynchus [29], Aedes pseudonormanensis [30] | Marsupials: chudditch [31] Wild eutherian mammals: European rabbits [31] Domestic mammals: horses [31] Birds: Emus [31] | |
| Murray Valley encephalitis virus (MVEV) | Western Australia [32], Northern Territory [33], New South Wales, and Victoria [34] | Culex annulirostris [35], Culex sitiens and other Culicine mosquitoes [36] | Marsupials: eastern grey kangaroos [37], western grey kangaroos, agile wallabies [38] Australian birds: galahs, sulphur-crested cockatoos [38], chickens [39] Wild eutherian mammals: rabbits [37], wild mice [38] Domestic mammals: dogs, sheep, pigs, cattle [37] Water birds: rufous night herons [34], Pacific black ducks [38] | Domestic mammals: horses [22,40,41] |
| West Nile virus (WNV) | All of Australia [42,43] | Mainly isolated from Culex annulirostris [44]. Other Culex species, Aedes species and Anopheles amictus can also transmit the virus [45,46] | Marsupials: western grey kangaroos, agile wallabies [37] Australian bird: Australian white ibis [47] Ardeid birds: herons, egrets [48] Introduced bird: house sparrow [49]. | Wild eutherian mammals: rabbits [50,51] Domestic mammals: horses [22,42], cats (mild) [52] |
| Japanese encephalitis virus (JEV) | Torres Strait (incursion) [53], North Peninsula Area and mainland [54] | Culex annulirostris [53]. | Ardeid birds: herons, egrets [55,56,57] Domestic mammals: pigs [58], horses [59] | Wild eutherian mammals: Frugivorous bats i.e., black flying fox [60] Other birds: pigeons, sparrows, ducks, chickens [60] |
| Kokobera (KOKV) and related viruses | Queensland, New South Wales, Northern Territory, Western Australia, and Papua New Guinea [61,62] | Aedes species including Aedes aculeatus, Aedes alternas, Aedes notoscriptus, Aedes procax, Aedes vigilax and Anopheles annulipes [63] | Marsupials: mainly kangaroos and wallabies [17,64]. Domestic mammals: cattle [26] | Domestic mammals: horses [64,65] It is unknown whether horses are affected by Kokobera and related viruses, as it could be associated with a known equine disease. |
| Gan Gan (GGV) and Trubanaman viruses (TRUV) | Queensland, New South Wales, and Western Australia [66] | Aedes vigilax (GGV) [67], Culex annulirostris (GGV and TRUV) [62,68], Anopheles annulipes (TRUV) [66] and Anopheles meraukensis [69] | Marsupials: eastern grey kangaroos (GGV, TRUV), red-necked wallaby (GGV, TRUV) [26], western grey kangaroos (TRUV) [70] Wild eutherian mammals: Australian bush rat (GGV) [26], feral pigs (TRUV), rabbits (TRUV), foxes (TRUV), quokkas (TRUV) [70] Domestic mammals: sheep (GGV), horses (GGV, TRUV), cattle (GGV) [26,70] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ong, O.T.W.; Skinner, E.B.; Johnson, B.J.; Old, J.M. Mosquito-Borne Viruses and Non-Human Vertebrates in Australia: A Review. Viruses 2021, 13, 265. https://doi.org/10.3390/v13020265
Ong OTW, Skinner EB, Johnson BJ, Old JM. Mosquito-Borne Viruses and Non-Human Vertebrates in Australia: A Review. Viruses. 2021; 13(2):265. https://doi.org/10.3390/v13020265
Chicago/Turabian StyleOng, Oselyne T. W., Eloise B. Skinner, Brian J. Johnson, and Julie M. Old. 2021. "Mosquito-Borne Viruses and Non-Human Vertebrates in Australia: A Review" Viruses 13, no. 2: 265. https://doi.org/10.3390/v13020265
APA StyleOng, O. T. W., Skinner, E. B., Johnson, B. J., & Old, J. M. (2021). Mosquito-Borne Viruses and Non-Human Vertebrates in Australia: A Review. Viruses, 13(2), 265. https://doi.org/10.3390/v13020265