Cumulative Effects of Particulate Matter Pollution and Meteorological Variables on the Risk of Influenza-Like Illness
Abstract
:1. Introduction
2. Materials and Methods
2.1. Influenza-Like Illness Data
2.2. Meteorological and Air Pollution Data
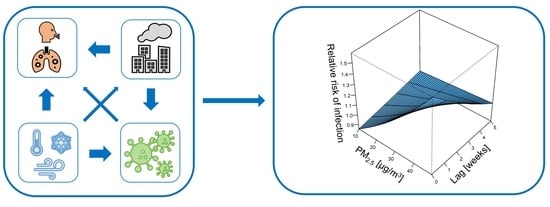
2.3. Statistical Analysis
3. Results
3.1. Influenza-Like Illness Activity in 2013–2019
3.2. Air Pollution and Meteorological Data
3.3. Correlations between Influenza-Like Illness Cases and Meteorological Data
3.4. Non-Linear Univariable Models
3.5. Non-Linear Multivariable Models
3.6. The Effect of Wind Speed
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Air Quality Guidelines: Global Update 2005: Particulate Matter, Ozone, Nitrogen Dioxide, and Sulfur Dioxide; World Health Organization: Geneva, Switzerland, 2006; ISBN 978-92-890-2192-0. [Google Scholar]
- Kim, K.-H.; Kabir, E.; Kabir, S. A review on the human health impact of airborne particulate matter. Environ. Int. 2015, 74, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Sun, Q.; Hong, X.; Wold, L.E. Cardiovascular Effects of Ambient Particulate Air Pollution Exposure. Circulation 2010, 121, 2755–2765. [Google Scholar] [CrossRef]
- Huang, L.; Zhou, L.; Chen, J.; Chen, K.; Liu, Y.; Chen, X.; Tang, F. Acute effects of air pollution on influenza-like illness in Nanjing, China: A population-based study. Chemosphere 2016, 147, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Silva, D.R.; Viana, V.P.; Müller, A.M.; Livi, F.P.; Dalcin, P.D.T.R. Respiratory viral infections and effects of meteorological parameters and air pollution in adults with respiratory symptoms admitted to the emergency room. Influ. Other Respir. Viruses 2014, 8, 42–52. [Google Scholar] [CrossRef] [PubMed]
- Su, W.; Wu, X.; Geng, X.; Zhao, X.; Liu, Q.; Liu, T. The short-term effects of air pollutants on influenza-like illness in Jinan, China. BMC Public Heal. 2019, 19, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, Y.; Wu, X.-J.; Guan, Y.-J. Effect of ambient air pollutants and meteorological variables on COVID-19 incidence. Infect. Control. Hosp. Epidemiol. 2020, 41, 1011–1015. [Google Scholar] [CrossRef]
- Fukuda, K.; WHO (Eds.) Pandemic Influenza Preparedness and Response: A WHO Guidance Document; World Health Organization: Geneva, Switzerland, 2009; ISBN 978-92-4-154768-0. [Google Scholar]
- Feng, L.; Feng, S.; Chen, T.; Yang, J.; Lau, Y.C.; Peng, Z.; Li, L.; Wang, X.; Wong, J.Y.T.; Qin, Y.; et al. Burden of influenza-associated outpatient influenza-like illness consultations in China, 2006-2015: A population-based study. Influ. Other Respir. Viruses 2019, 14, 162–172. [Google Scholar] [CrossRef] [Green Version]
- Tsai, Y.; Zhou, F.; Kim, I.K. The burden of influenza-like illness in the US workforce. Occup. Med. 2014, 64, 341–347. [Google Scholar] [CrossRef] [Green Version]
- Air Quality Statistics—European Environment Agency. Available online: https://www.eea.europa.eu/data-and-maps/dashboards/air-quality-statistics (accessed on 19 August 2020).
- Juda-Rezler, K.; Reizer, M.; Maciejewska, K.; Błaszczak, B.; Klejnowski, K. Characterization of atmospheric PM2.5 sources at a Central European urban background site. Sci. Total. Environ. 2020, 713, 136729. [Google Scholar] [CrossRef]
- Slama, A.; Śliwczyński, A.; Woźnica, J.; Zdrolik, M.; Wiśnicki, B.; Kubajek, J.; Turżańska-Wieczorek, O.; Gozdowski, D.; Wierzba, W.; Franek, E. Impact of air pollution on hospital admissions with a focus on respiratory diseases: A time-series multi-city analysis. Environ. Sci. Pollut. Res. 2019, 26, 16998–17009. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.-X.; Li, Y.; Qin, G.; Zhu, Y.; Li, X.; Zhang, J.; Zhao, K.; Hu, M.; Wang, X.-L.; Zheng, X. Effects of air pollutants on occurrences of influenza-like illness and laboratory-confirmed influenza in Hefei, China. Int. J. Biometeorol. 2018, 63, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Hu, W.; Williams, G.; Clements, A.C.; Kan, H.; Tong, S. Air pollution, temperature and pediatric influenza in Brisbane, Australia. Environ. Int. 2013, 59, 384–388. [Google Scholar] [CrossRef]
- Boëlle, P.-Y.; Souty, C.; Launay, T.; Guerrisi, C.; Turbelin, C.; Behillil, S.; Enouf, V.; Poletto, C.; Lina, B.; Van Der Werf, S.; et al. Excess cases of influenza-like illnesses synchronous with coronavirus disease (COVID-19) epidemic, France, March 2020. Eurosurveillance 2020, 25, 2000326. [Google Scholar] [CrossRef] [Green Version]
- Kong, W.-H.; Li, Y.; Peng, M.-W.; Kong, D.-G.; Yang, X.-B.; Wang, L.; Liu, M.-Q. SARS-CoV-2 detection in patients with influenza-like illness. Nat. Microbiol. 2020, 5, 675–678. [Google Scholar] [CrossRef] [Green Version]
- Yu, X.; Wei, D.; Chen, Y.; Zhang, D.; Zhang, X. Retrospective detection of SARS-CoV-2 in hospitalized patients with influenza-like illness. Emerg. Microbes Infect. 2020, 9, 1470–1473. [Google Scholar] [CrossRef]
- Conticini, E.; Frediani, B.; Caro, D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020, 261, 114465. [Google Scholar] [CrossRef]
- Poland State Inspection for Environmental Protection; Chief Inspectorate of Environmental Protection. Fine Particles in the Atmosphere: A Compendium of Knowledge about Particulate Matter Air Pollution in Poland; Degórska, A., Juda-Rezler, K., Toczko, B., Eds.; Chief Inspectorate of Environmental Protection: Warsaw, Poland, 2016; ISBN 978-83-61227-73-1.
- Statistics Poland—Local Data Bank. Available online: https://bdl.stat.gov.pl (accessed on 4 August 2020).
- Merkel, A. Climate-Data.Org. Available online: https://en.climate-data.org/europe/poland/podlaskie-voivodeship/bia%C5%82ystok-1031/ (accessed on 9 January 2020).
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Distributed lag non-linear models. Stat. Med. 2010, 29, 2224–2234. [Google Scholar] [CrossRef] [Green Version]
- Burnham, K.P.; Anderson, D.R. Model Selection and Inference: A Practical Information-Theoretic Approach; Springer: New York, NY, USA, 1998; ISBN 978-1-4757-2917-7. [Google Scholar]
- Liang, Y.; Fang, L.; Pan, H.; Zhang, K.; Kan, H.; Brook, J.R.; Sun, Q. PM2.5 in Beijing—temporal pattern and its association with influenza. Environ. Health 2014, 13, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Feng, C.; Li, J.; Sun, W.; Zhang, Y.; Wang, Q. Impact of ambient fine particulate matter (PM2.5) exposure on the risk of influenza-like-illness: A time-series analysis in Beijing, China. Environ. Health 2016, 15, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vandini, S.; Corvaglia, L.; Alessandroni, R.; Aquilano, G.; Marsico, C.; Spinelli, M.; Lanari, M.; Faldella, G. Respiratory syncytial virus infection in infants and correlation with meteorological factors and air pollutants. Ital. J. Pediatr. 2013, 39, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brunekreef, B.; Holgate, S.T. Air pollution and health. Lancet 2002, 360, 1233–1242. [Google Scholar] [CrossRef]
- Laden, F.; Neas, L.M.; Dockery, D.W.; Schwartz, J. Association of fine particulate matter from different sources with daily mortality in six U.S. cities. Environ. Health Perspect. 2000, 108, 941–947. [Google Scholar] [CrossRef]
- Polichetti, G.; Cocco, S.; Spinali, A.; Trimarco, V.; Nunziata, A. Effects of particulate matter (PM10, PM2.5 and PM1) on the cardiovascular system. Toxicology 2009, 261, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Raaschou-Nielsen, O.; Andersen, Z.J.; Beelen, R.; Samoli, E.; Stafoggia, M.; Weinmayr, G.; Hoffmann, B.; Fischer, P.; Nieuwenhuijsen, M.J.; Brunekreef, B.; et al. Air pollution and lung cancer incidence in 17 European cohorts: Prospective analyses from the European Study of Cohorts for Air Pollution Effects (ESCAPE). Lancet Oncol. 2013, 14, 813–822. [Google Scholar] [CrossRef]
- Domingo, J.L.; Rovira, J. Effects of air pollutants on the transmission and severity of respiratory viral infections. Environ. Res. 2020, 187, 109650. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.-S.; Tsai, F.T.; Lin, C.K.; Yang, C.-Y.; Chan, C.-C.; Young, C.-Y.; Lee, C.-H. Ambient Influenza and Avian Influenza Virus during Dust Storm Days and Background Days. Environ. Health Perspect. 2010, 118, 1211–1216. [Google Scholar] [CrossRef] [Green Version]
- Lindner-Cendrowska, K.; Bröde, P. Impact of biometeorological conditions and air pollution on influenza-like illnesses incidence in Warsaw. Int. J. Biometeorol. 2021, 1–16. [Google Scholar] [CrossRef]
- Stellrecht, K.A. Chapter 11—Molecular Testing for Respiratory Viruses. In Diagnostic Molecular Pathology; Coleman, W.B., Tsongalis, G.J., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 123–137. ISBN 978-0-12-800886-7. [Google Scholar]
- Cowling, B.J.; Ip, D.K.M.; Fang, V.J.; Suntarattiwong, P.; Olsen, S.J.; Levy, J.; Uyeki, T.M.; Leung, G.M.; Peiris, J.S.M.; Chotpitayasunondh, T.; et al. Aerosol transmission is an important mode of influenza A virus spread. Nat. Commun. 2013, 4, 1–6. [Google Scholar] [CrossRef]
- Tellier, R.; Li, Y.; Cowling, B.J.; Tang, J.W. Recognition of aerosol transmission of infectious agents: A commentary. BMC Infect. Dis. 2019, 19, 1–9. [Google Scholar] [CrossRef]
- Tellier, R. Aerosol transmission of influenza A virus: A review of new studies. J. R. Soc. Interface 2009, 6, S783–S790. [Google Scholar] [CrossRef] [Green Version]
- Hammond, G.W.; Raddatz, R.L.; Gelskey, D.E. Impact of Atmospheric Dispersion and Transport of Viral Aerosols on the Epidemiology of Influenza. Clin. Infect. Dis. 1989, 11, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.E. Is influenza-like illness a useful concept and an appropriate test of influenza vaccine effectiveness? Vaccine 2014, 32, 2143–2149. [Google Scholar] [CrossRef] [PubMed]
- Burke, C.W.; Bridges, O.; Brown, S.; Rahija, R.; Russell, C.J. Mode of Parainfluenza Virus Transmission Determines the Dynamics of Primary Infection and Protection from Reinfection. PLoS Pathog. 2013, 9, e1003786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kulkarni, H.; Smith, C.; Hirst, R.; Baker, N.; Easton, A.; O’Callaghan, C. Airborne Transmission of Respiratory Syncytial Virus (RSV) Infection. Eur. Respir. J. 2011, 38, 1722. [Google Scholar]
- Aintablian, N.; Walpita, P.; Sawyer, M.H. Detection of Bordetella pertussis and Respiratory Syncytial Virus in Air Samples from Hospital Rooms. Infect. Control. Hosp. Epidemiol. 1998, 19, 918–923. [Google Scholar] [CrossRef]
- Dick, E.C.; Jennings, L.C.; Mink, K.A.; Wartgow, C.D.; Inborn, S.L. Aerosol Transmission of Rhinovirus Colds. J. Infect. Dis. 1987, 156, 442–448. [Google Scholar] [CrossRef] [PubMed]
- Myatt, T.A.; Johnston, S.L.; Zuo, Z.; Wand, M.; Kebadze, T.; Rudnick, S.; Milton, D.K. Detection of Airborne Rhinovirus and Its Relation to Outdoor Air Supply in Office Environments. Am. J. Respir. Crit. Care Med. 2004, 169, 1187–1190. [Google Scholar] [CrossRef]
- Couch, R.B.; Cate, T.R.; Fleet, W.F.; Gerone, P.J.; Knight, V. Aerosol-induced adenoviral illness resembling the naturally occurring illness in military recruits. Am. Rev. Respir. Dis. 1966, 93, 529–535. [Google Scholar]
- Echavarria, M.; Kolavic, S.A.; Cersovsky, S.; Mitchell, F.; Sanchez, J.L.; Polyak, C.; Innis, B.L.; Binn, L.N. Detection of Adenoviruses (AdV) in Culture-Negative Environmental Samples by PCR during an AdV-Associated Respiratory Disease Outbreak. J. Clin. Microbiol. 2000, 38, 2982–2984. [Google Scholar] [CrossRef] [Green Version]
- Da Silva, P.G.; Nascimento, M.S.J.; Soares, R.R.; Sousa, S.I.; Mesquita, J.R. Airborne spread of infectious SARS-CoV-2: Moving forward using lessons from SARS-CoV and MERS-CoV. Sci. Total. Environ. 2021, 764, 142802. [Google Scholar] [CrossRef]
- Yu, I.T.; Li, Y.; Wong, T.W.; Tam, W.; Chan, A.T.; Lee, J.H.; Leung, D.Y.; Ho, T. Evidence of Airborne Transmission of the Severe Acute Respiratory Syndrome Virus. New Engl. J. Med. 2004, 350, 1731–1739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morawska, L.; Cao, J. Airborne transmission of SARS-CoV-2: The world should face the reality. Environ. Int. 2020, 139, 105730. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; Li, Y.; Eames, I.; Chan, P.; Ridgway, G. Factors involved in the aerosol transmission of infection and control of ventilation in healthcare premises. J. Hosp. Infect. 2006, 64, 100–114. [Google Scholar] [CrossRef] [PubMed]
- Griffin, D.W.; Garrison, V.H.; Herman, J.R.; Shinn, E.A. African desert dust in the Caribbean atmosphere: Microbiology and public health. Aerobiology 2001, 17, 203–213. [Google Scholar] [CrossRef]
- Sooryanarain, H.; Elankumaran, S. Environmental Role in Influenza Virus Outbreaks. Annu. Rev. Anim. Biosci. 2015, 3, 347–373. [Google Scholar] [CrossRef]
- Lowen, A.C.; Steel, J. Roles of Humidity and Temperature in Shaping Influenza Seasonality. J. Virol. 2014, 88, 7692–7695. [Google Scholar] [CrossRef] [Green Version]
- Ianevski, A.; Zusinaite, E.; Shtaida, N.; Kallio-Kokko, H.; Valkonen, M.; Kantele, A.; Telling, K.; Lutsar, I.; Letjuka, P.; Metelitsa, N.; et al. Low Temperature and Low UV Indexes Correlated with Peaks of Influenza Virus Activity in Northern Europe during 2010–2018. Viruses 2019, 11, 207. [Google Scholar] [CrossRef] [Green Version]
- Lowen, A.C.; Mubareka, S.; Steel, J.; Palese, P. Influenza Virus Transmission Is Dependent on Relative Humidity and Temperature. PLOS Pathog. 2007, 3, e151. [Google Scholar] [CrossRef]
- Schaffer, F.L.; Soergel, M.E.; Straube, D.C. Survival of airborne influenza virus: Effects of propagating host, relative humidity, and composition of spray fluids. Arch. Virol. 1976, 51, 263–273. [Google Scholar] [CrossRef]
- Tamerius, J.D.; Shaman, J.; Alonso, W.J.; Bloom-Feshbach, K.; Uejio, C.K.; Comrie, A.; Viboud, C. Environmental Predictors of Seasonal Influenza Epidemics across Temperate and Tropical Climates. PLOS Pathog. 2013, 9, e1003194. [Google Scholar] [CrossRef]
- Shoji, M.; Katayama, K.; Sano, K. Absolute Humidity as a Deterministic Factor Affecting Seasonal Influenza Epidemics in Japan. Tohoku J. Exp. Med. 2011, 224, 251–256. [Google Scholar] [CrossRef] [Green Version]
- Sundell, N.; Andersson, L.-M.; Brittain-Long, R.; Lindh, M.; Westin, J. A four year seasonal survey of the relationship between outdoor climate and epidemiology of viral respiratory tract infections in a temperate climate. J. Clin. Virol. 2016, 84, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Ypma, R.J.; Jonges, M.; Bataille, A.; Stegeman, A.; Koch, G.; Van Boven, M.; Koopmans, M.; Van Ballegooijen, W.M.; Wallinga, J. Genetic Data Provide Evidence for Wind-Mediated Transmission of Highly Pathogenic Avian Influenza. J. Infect. Dis. 2012, 207, 730–735. [Google Scholar] [CrossRef] [Green Version]
- Tai, A.P.K.; Mickley, L.J.; Jacob, D.J. Correlations between fine particulate matter (PM2.5) and meteorological variables in the United States: Implications for the sensitivity of PM2.5 to climate change. Atmos. Environ. 2010, 44, 3976–3984. [Google Scholar] [CrossRef]
- Ouyang, W.; Guo, B.; Cai, G.; Li, Q.; Han, S.; Liu, B.; Liu, X. The washing effect of precipitation on particulate matter and the pollution dynamics of rainwater in downtown Beijing. Sci. Total. Environ. 2015, 505, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Song, M.; Zhao, T.; Gunthe, S.S.; Ham, S.; He, Y.; Qin, Y.M.; Gong, Z.; Amorim, J.C.; Bertram, A.K.; et al. Resolving the mechanisms of hygroscopic growth and cloud condensation nuclei activity for organic particulate matter. Nat. Commun. 2018, 9, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Ciencewicki, J.; Jaspers, I. Air Pollution and Respiratory Viral Infection. Inhal. Toxicol. 2007, 19, 1135–1146. [Google Scholar] [CrossRef] [PubMed]
- Saravia, J.; You, D.; Thevenot, P.; Lee, G.I.; Shrestha, B.; Lomnicki, S.; Cormier, S.A. Early-life exposure to combustion-derived particulate matter causes pulmonary immunosuppression. Mucosal Immunol. 2014, 7, 694–704. [Google Scholar] [CrossRef] [PubMed]
- I Lee, G.; Saravia, J.; You, D.; Shrestha, B.; Jaligama, S.; Hebert, V.Y.; Dugas, T.R.; A Cormier, S. Exposure to combustion generated environmentally persistent free radicals enhances severity of influenza virus infection. Part. Fibre Toxicol. 2014, 11, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Jaspers, I.; Ciencewicki, J.M.; Zhang, W.; Brighton, L.E.; Carson, J.L.; Beck, M.A.; Madden, M.C. Diesel Exhaust Enhances Influenza Virus Infections in Respiratory Epithelial Cells. Toxicol. Sci. 2005, 85, 990–1002. [Google Scholar] [CrossRef] [Green Version]
- Li, N.; Harkema, J.R.; Lewandowski, R.P.; Wang, M.; Bramble, L.A.; Gookin, G.R.; Ning, Z.; Kleinman, M.T.; Sioutas, C.; Nel, A.E. Ambient ultrafine particles provide a strong adjuvant effect in the secondary immune response: Implication for traffic-related asthma flares. Am. J. Physiol. Cell. Mol. Physiol. 2010, 299, L374–L383. [Google Scholar] [CrossRef]
- Yang, J.; Chen, Y.; Yu, Z.; Ding, H.; Ma, Z. The influence of PM2.5 on lung injury and cytokines in mice. Exp. Ther. Med. 2019, 18, 2503–2511. [Google Scholar] [CrossRef] [Green Version]
- E Pinkerton, K.; Green, F.H.; Saiki, C.; Vallyathan, V.; Plopper, C.G.; Gopal, V.; Hung, D.; Bahne, E.B.; Lin, S.S.; Ménache, M.G.; et al. Distribution of particulate matter and tissue remodeling in the human lung. Environ. Health Perspect. 2000, 108, 1063–1069. [Google Scholar] [CrossRef]
- Sancini, G.; Farina, F.; Battaglia, C.; Cifola, I.; Mangano, E.; Mantecca, P.; Camatini, M.; Palestini, P. Health Risk Assessment for Air Pollutants: Alterations in Lung and Cardiac Gene Expression in Mice Exposed to Milano Winter Fine Particulate Matter (PM2.5). PLoS ONE 2014, 9, e109685. [Google Scholar] [CrossRef] [PubMed]
- Comunian, S.; Dongo, D.; Milani, C.; Palestini, P. Air Pollution and COVID-19: The Role of Particulate Matter in the Spread and Increase of COVID-19′s Morbidity and Mortality. Int. J. Environ. Res. Public Heal. 2020, 17, 4487. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Nigmatulina, K.; Eckhoff, P. The scaling of contact rates with population density for the infectious disease models. Math. Biosci. 2013, 244, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Williams, E.; Kirk, M. Risk Factors for Acute Respiratory Infection in the Australian Community. PLoS ONE 2014, 9, e101440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Filonchyk, M.; Hurynovich, V.; Yan, H. Impact of Covid-19 lockdown on air quality in the Poland, Eastern Europe. Environ. Res. 2020, 110454. [Google Scholar] [CrossRef]
- Shi, Z.; Song, C.; Liu, B.; Lu, G.; Xu, J.; Van Vu, T.; Elliott, R.J.R.; Li, W.; Bloss, W.J.; Harrison, R.M. Abrupt but smaller than expected changes in surface air quality attributable to COVID-19 lockdowns. Sci. Adv. 2021, 7, eabd6696. [Google Scholar] [CrossRef]




| Mean | SD | Min | P5 | P25 | Median | P75 | P95 | Max | |
|---|---|---|---|---|---|---|---|---|---|
| Number of cases of ILI | 1029.72 | 1034.50 | 0.00 | 108.0 | 313.75 | 700.00 | 1280.50 | 3227.0 | 6309.00 |
| Temperature (°C) | 8.28 | 8.03 | −12.90 | −5.51 | 2.02 | 7.99 | 15.83 | 21.00 | 23.11 |
| Relative humidity (%) | 79.30 | 9.81 | 45.46 | 57.50 | 72.28 | 80.51 | 87.52 | 96.40 | 97.30 |
| Absolute humidity (g/m3) | 7.30 | 3.18 | 1.34 | 2.97 | 4.65 | 6.92 | 10.00 | 12.79 | 15.91 |
| Wind speed (m/s) | 2.40 | 0.57 | 1.05 | 1.00 | 2.01 | 2.33 | 2.71 | 4.10 | 4.66 |
| Precipitation (mm) | 1.79 | 2.09 | 0.00 | 0.00 | 0.29 | 1.06 | 2.46 | 9.82 | 13.29 |
| Precipitation duration (hours) | 3.09 | 2.75 | 0.00 | 0.00 | 1.00 | 2.35 | 4.46 | 13.40 | 13.85 |
| Sunshine duration (hours) | 4.99 | 3.75 | 0.00 | 0.20 | 1.42 | 4.88 | 7.93 | 13.16 | 14.59 |
| PM2.5 (µg/m3) | 22.34 | 7.96 | 6.56 | 7.50 | 15.26 | 19.60 | 26.86 | 44.70 | 49.77 |
| PM10 (µg/m3) | 22.41 | 9.93 | 9.04 | 8.60 | 16.83 | 20.39 | 26.90 | 50.42 | 55.99 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toczylowski, K.; Wietlicka-Piszcz, M.; Grabowska, M.; Sulik, A. Cumulative Effects of Particulate Matter Pollution and Meteorological Variables on the Risk of Influenza-Like Illness. Viruses 2021, 13, 556. https://doi.org/10.3390/v13040556
Toczylowski K, Wietlicka-Piszcz M, Grabowska M, Sulik A. Cumulative Effects of Particulate Matter Pollution and Meteorological Variables on the Risk of Influenza-Like Illness. Viruses. 2021; 13(4):556. https://doi.org/10.3390/v13040556
Chicago/Turabian StyleToczylowski, Kacper, Magdalena Wietlicka-Piszcz, Magdalena Grabowska, and Artur Sulik. 2021. "Cumulative Effects of Particulate Matter Pollution and Meteorological Variables on the Risk of Influenza-Like Illness" Viruses 13, no. 4: 556. https://doi.org/10.3390/v13040556
APA StyleToczylowski, K., Wietlicka-Piszcz, M., Grabowska, M., & Sulik, A. (2021). Cumulative Effects of Particulate Matter Pollution and Meteorological Variables on the Risk of Influenza-Like Illness. Viruses, 13(4), 556. https://doi.org/10.3390/v13040556