1. Introduction
The design and production of appropriate drug delivery systems, in particular, nanosized ones, offer an advanced approach to optimised bioavailability and/or the stability of drugs, to control drug delivery and to maintain drug stability during transport to the site of action. A successful drug carrier system should possess a long shelf life, optimal drug loading and release properties, and exert a much higher therapeutic efficacy as well as have low side effects [
1,
2].
Phospholipids are the main amphiphilic components of the cell membrane and currently represent the main constituents of nanovectors because they can self-assembly in aqueous milieu, generating different supramolecular structures such as micelles and vesicles [
1,
3]. Typically, their variation in head groups, aliphatic chains and alcohols leads to a wide variety of phospholipids, generally classified as glycerophospholipids and sphingomyelins. The most common natural glycerophospholipids are phosphatidylcholine (PC), phosphatidylinositol, phosphatidylserine (PS), phosphatidylglycerol and phosphatidic acid, having diverse acyl moieties, principally myristoyl, palmitoyl, oleoyl and stearoyl.
In particular, glycerophospholipids are the specific constituents of liposomes, which are widely used as drug vectors because of their high biocompatibility, non-toxicity, complete biodegradability, and non-immunogenic effects after both systemic and non-systemic routes of administration [
4]. Conversely, the therapeutic use of vesicles has some limitations, principally poor stability and availability under the harsh conditions typically presented in the gastrointestinal tract [
1,
2,
5,
6]. A very limited number of studies report on the use of cochleates as an alternative platform to vesicles in order to overcome these limitations. Cochleates were first observed by Verkleij et al. [
7] using phosphatidylglycerol liposomes and later by Papahadjopoulos et al. [
8], using phosphatidylserine liposomes in the presence of divalent metal cations (Me
2+), i.e., Ca
2+, Ba
2+, Fe
2+, Mg
2+ and Zn
2+. Cochleates can be produced as nano- and microstructures and they are extremely biocompatible, with excellent stability due to their unique compact structure. They present an elongated shape and a carpet roll-like morphology always accompanied by narrowly packed bilayers, through the interaction with Me
2+ as bridging agents between the bilayers (
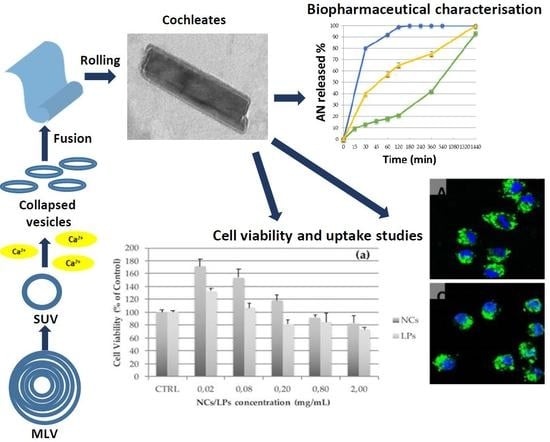
Figure 1). During this arrangement, the close approach of bilayers is dependent on dehydration of the head group of the phospholipid. They roll-up in order to minimise their interaction with water and, consequently, cochleates possess little or no aqueous phase. The relevant differences between cochleates and different liposomes, i.e., small unilamellar vesicle (SUV), large unilamellar vesicle (LUV), multilamellar vesicle (MLV) and multivesicle vesicle (MVV), are reported in
Figure 1.
The bilayers in a cochleate are organised very precisely at a very close repeating distance of 54 Angstrom [
9] with a water-free interior, which is a rigid, stable, rod-shaped structure. Due to this unique structure, cochleates can be easily lyophilised to a free-flowing powder that can be incorporated in capsules for oral administration or re-dispersed in water for parental administration. Yet what remains very unclear is their mechanism of permeation throughout the biological membranes. It is reported that after oral administration, cochleates cross the epithelium, delivering the loaded drug into the blood vessel [
10]. There are two current hypotheses to explain the mechanism of permeation. According to the first assumption, the contact of the calcium-rich membrane of the cochleate with a cell can cause a perturbation and the reordering of the cell membrane. Subsequently, there is fusion between the outer layer of the cochleate and the cell membrane [
10]. An alternative hypothesis for the delivery mechanism of cochleates is phagocytosis. In both cases, once within the interior of a cell, a low calcium concentration results in the opening of the cochleate crystal and the release of the entrapped drug [
11,
12,
13].
Currently, cochleates represent difficult drug delivery systems for clinical use, principally due to the numerous difficulties in producing monodisperse systems because of a tendency to form stable and huge aggregates, which represent a serious drawback at the industrial level. Diverse patents and publications have reported different strategies to overcome these limitations [
11], in particular, the use of methylcellulose, casein, or albumin, but proteins may decrease stability and safety due to the change of pharmacokinetic parameters. Methylcellulose is able only in part to disrupt the formed aggregates. Other natural polysaccharides (including celluloses, gums, and starches) have been recommended as inhibitors of the aggregation processes, but their efficiency still remains ambiguous [
11,
12]. In recent times, the ability of citric acid to remove Ca
2+ ions from the external surface of cochleates, leading to the dispersion of the aggregates, has been investigated [
13]. Furthermore, a recent approach compared a novel microfluidics-based strategy with the conventional cochleate production methods; however, the formation of aggregates was still present in the samples [
14].
The aim of this study was the production of monodisperse and stable nanocochleates (NCs) using two different phospholipids, PC and PS, loaded with a typical small hydrophobic natural product, andrographolide (AN) from the Asiatic medicinal plant
Andrographis paniculata. Besides the numerous potential activities ranging from anti-inflammatory to neuroprotection, antidiabetic to anti-obesity properties, and antitumor activity to hepatoprotective activity [
15], AN has poor water solubility (3.29 ± 0.73 µg at 25 °C) [
16], which deeply limits its biodistribution and localisation, resulting in low bioavailability [
17]. Additionally, AN is unstable in gastrointestinal media and has a very short biological half-life (
t½ = 1.33 h) after a single oral dose [
18]. The stability of developed nanocochleates after lyophilisation and in simulated gastrointestinal fluids was investigated. In addition, the possible hazards and the cellular effects of NCs were determined using J774a.1 murine macrophages and 3T3 fibroblasts. Lastly, studies on uptake using a confocal microscope were carried out in the macrophages cell line.
2. Materials and Methods
2.1. Materials
The phospholipon 90G (soy phosphatidylcholine, PC) was sourced from the Italian agent AVG srl (Milan, Italy) of Lipoid AG (Cologne, Germany). The dioleoyl phosphatidylserine (PS) was a kind gift from Lipoid AG (Cologne, Germany). The following reagents were from Sigma-Aldrich (Milan, Italy): pepsin from porcine gastric mucosa, bile salts, andrographolide (AN), fluorescein isothiocyanate (FITC, purity ≥ 90%, HPLC), lipase from porcin pancreas, sodium hydroxide (NaOH), calcium chloride (CaCl2), cholesterol, phosphate buffered saline (PBS) bioperformance certified, paraformaldehyde (PFA), Dulbecco’s Modified Eagle Medium (DMEM), fetal bovine serum (FBS), l-glutamine, penicillin–streptomycin solution, WST-8 kit, acetonitrile (HPLC grade), methanol (HPLC grade), formic acid (analytical grade), hydrochloric acid (HCl) (analytical grade) and dichloromethane (CH2Cl2). The water used was from the Milli-Qplus system from Millipore (Milford, CT, USA). The phosphotungstic acid (PTA) was from Electron Microscopy Sciences (Hatfield, PA, USA). The dialysis kit was from Spectrum Laboratories, Inc. (Breda, The Netherlands). The J774a.1 murine macrophages and the 3T3 fibroblasts were purchased from the American Type Culture Collection (ATCC® TIB-67™, Manassas, VA, USA). A LT-4000 reader from Labtech was used to read the absorbance (Bergamo, Italy).
2.2. Preparation of PC- and PS-based Liposomes and NCs
The NCs were obtained from nano-sized liposomes (LPs), which were prepared according to the film hydration method [
19]. The liposomes were formulated as follows: the required amounts of phospholipids (60 mg) and cholesterol (20 mg) were dissolved in a dichloromethane/methanol mixture (20 mL of a mixture, 3:2
v/
v). The obtained organic solution was evaporated under vacuum and the lipid film was hydrated by the addition of PBS (10 mL) using a mechanical stirrer (RW20 digital, IKA, Staufen im Breisgau, Germany) for 30 min in a water bath at a constant temperature of 37 °C for PC and 60 °C for PS. The resulting formulations were optimised by ultrasonication (3 min, two cycles of 90 s) in an ice bath to prevent lipid degradation. Subsequently, a gentle centrifugation (1205×
g, 1 min) was performed to remove possible metallic particles released during the ultrasonication. The NCs were prepared from the nanoliposomes according to the trapping method, described by Asprea et al. [
20]. Briefly, a 0.1 M solution of CaCl
2 was added drop-by-drop to the liposomal suspension under magnetic stirring (150 rpm, room temperature) until the formulation appeared cloudy, indicating the formation of NCs. The molar ratio between PC and CaCl
2 was 1:1, while the molar ratio between PS and CaCl
2 was 1:4.
2.3. Characterisation of Nanocarriers: Size, Polydispersity Index and ζ-Potential
The Zsizer Nano series ZS90 (Malvern Instruments, Malvern, UK) outfitted with a JDS Uniphase 22 mW He-Ne laser operating at 632.8 nm, an optical fiber-based detector, a digital LV/LSE-5003 correlator and a temperature controller (Julabo water-bath) set at 25 °C was used for Dynamic Light Scattering (DLS) measurements, including for the particle size, polydispersity index (PdI) and ζ-potential. The cumulant method was used to analyse time correlation functions, obtaining the mean diameter of the nanocarriers (Z-average) and the size distribution using the ALV-60X0 software V.3.X provided by Malvern. The size characterisation technique for the nanoparticles in suspension, based on the measurement of their translational diffusion coefficient, related to the length, L, of their major axis is as
where
η represents the viscosity of the solvent,
kB represents the Boltzmann constant and
T represents the sample temperature.
FD is a geometrical coefficient depending on the shape, but not the size, of the particles [
21,
22]. In particular, for NCs, the expressions of
FD corresponding to these particle shapes are
ζ-potential values were obtained from the electrophoretic mobility, using the Henry correction to Smoluchowski’s equation. The samples were diluted in distilled water and an average of three measurements at the stationary level were taken. A Haake temperature controller kept the temperature constant at 25 °C.
2.4. Morphological and Size Characterisation by Transmission Electron Microscopy (TEM)
A transmission electron microscope (TEM, Jeol Jem 1010, Tokyo, Japan) was used to evaluate the morphology, shape and dimensions of NCs. The NCs dispersion was diluted 10-fold and placed on a carbon film-covered copper grid and stained with a phosphotungstic acid solution 1 g/100 mL in sterile water, before the TEM analysis. The samples were dried for 1 min and then examined under TEM and photographed at an accelerating voltage of 64 kV.
2.5. Stability Study of NCs after Lyophilisation
The lyophilisation process of NCs provides an extended storage period at room temperature and can be carried out without the use of lyoprotectants because of the very low water content. The samples were frozen by a freezer (−23 °C) overnight before lyophilisation. Then, the samples were moved to a freeze-drier. The temperature was set to −23 °C and the pressure was −1.0 bar. The drying time was 24 h. The pressure and the temperature remained unchanged during the process.
The stability of the lyophilised NCs was evaluated after reconstitution of the colloidal system to the original volume with distilled water, using a vortex mixer at room temperature. The samples were stored in sealed glass containers after being placed into a desiccator containing silica gel to absorb water vapor. The samples were also protected from light. The stability of the lyophilised NCs was assessed by checking the size, ζ-potential, polydispersity and morphology every week for 2 months.
2.6. Stability Study of NCs in Gastrointestinal Media
NCs could be used to protect the entrapped compound from the effects of the gastrointestinal fluids. Accordingly, NC formulations were tested for their stability using simulated gastrointestinal conditions. Simulated gastric fluid (SGF) was used to investigate the gastric stability of NCs, as previously reported [
23,
24]. Briefly, 5 mL of NCs was suspended in 5 mL of SGF (0.32%
w/
v pepsin, 2 g of sodium chloride and 7 mL HCl dissolved in 1 L water and pH adjusted to 1.8 using 1 M HCl) and incubated at 37 °C under shaking at a speed of 100 strokes/min. After 2 h, the sample was collected. The size and PdI were analysed by DLS, while the morphology of the colloidal systems was analysed by TEM.
The stability of the samples was also investigated in simulated intestinal fluid (SIF) containing an intestinal enzyme complex (lipase 0.4 mg/mL, bile salts 0.7 mg/mL and pancreatin 0.5 mg/mL) and 750 mM calcium chloride solution at 37 °C, under shaking, with a speed of 100 strokes/min. The pH of the mixture was adjusted to a value of 7.0 with NaOH 0.1 N. After 2 h, the sample was collected and its physical and morphological properties were assessed by size and PDI analysis by DLS and TEM.
2.7. Preparation of Nanocarriers Based on AN and FITC
NCs were obtained from nanoliposomes (SUVs), which were prepared using the film hydration method. The nanoliposomes were formulated as follows: phospholipids (60 mg), cholesterol (20 mg) and AN (20 mg) or FITC (5 mg) were dissolved in dichloromethane/methanol mixture (20 mL of a mixture 3:2
v/
v). The obtained organic solution was evaporated under vacuum to obtain a lipid film, which was hydrated by the addition of PBS (10 mL) using a mechanical stirrer (RW20 digital, IKA, Staufen im Breisgau, Germany) for 30 min in a water bath at a constant temperature of 37 °C for PC and 60 °C for PS. The resulting formulations were reduced in size using an ultrasonication probe for 3 min (two cycles of 90 s). During the sonication, the samples were kept in an ice bath to prevent lipid degradation. After that, a gentle centrifugation (1205×
g, 1 min) was performed to remove possible metallic particles released during the ultrasonication. The NCs were prepared by the trapping method, according to Asprea et al. [
20]. A 0.1 M solution of CaCl
2 was added drop-by-drop to the liposomal suspension under magnetic stirring (150 rpm, at room temperature) until the formulation became cloudy, indicating the formation of NCs. The molar ratio between PC and CaCl
2 was 1:1, while the molar ratio between PS and CaCl
2 was 1:4.
2.8. Determination of Encapsulation Efficiency of AN–NCs by HPLC
After preparation of the NCs, free AN was removed by dialysis using bags with a pore size of 3.5–5 kD, and according to previous studies [
25]. The dialysis bag was placed in 1 L of distilled water at room temperature for 1 h under stirring. The physical mixture was used as a control to validate the procedure. The AN-loaded content was quantified by HPLC–DAD analysis using a standard sample of AN, after the treatment of NCs with methanol to destroy the cochleates. HPLC–DAD analyses were performed with a HP 1200 Liquid Chromatograph (Agilent Technologies, Palo Alto, CA, USA), equipped with a Diode Array Detector (DAD), managed by a HP 9000 workstation (Agilent Technologies). The column was a Varian Polaris RP18 (250 mm × 4.6 mm i.d., particle size 5 μm) (Agilent Technologies) maintained at 27 °C. The chromatograms were acquired at 223 nm. The eluents were acetonitrile (A) and formic acid/water at pH 3.2 (B) at a flow rate of 1 mL/min. The following gradient profile was applied: 0–3 min, 10% A, and 90% B; 3–11 min, 10–38% A, and 90–62% B; 11–25 min, 38% A, and 62% B; 25–30 min, 38–50% A, and 62–50% B; and 30–34 min, 50–10% A, and 50–90% B. The post time was 10 min. The injected volume of the samples was 10–20 µL.
The calibration curve was obtained from a dilution series of the AN reference standard solubilised in MeOH, in the range between 56 and 0.56 ng/mL. Linear regression was used to establish the calibration curve. AN was quantified using the peak areas acquired at 223 nm. The correlation coefficient (R2) was 0.9995. The data are expressed as the mean ± SD of the three experiments.
The encapsulation efficiency (EE%) for each preparation was calculated using the following equation:
where
Wt is the total amount of the loaded AN and
Wi is the total quantity of AN added initially during the preparation. The encapsulation efficiency was determined in triplicate.
2.9. Determination of Encapsulation Efficiency of FITC–NCs by HPLC
Free FITC was removed by means of dialysis, as previously described. The contents of FITC were determined by the same HPLC instrument used for AN quantification. The column was a Lichrosorb RP18 (4.6 mm × 100 mm i.d., 5 µm) (Agilent Technologies) maintained at 27 °C. The mobile phases were (A) acetonitrile and (B) formic acid/water pH 3.2, at a flow rate of 0.8 mL/min and an injection volume of 10 μL. The following gradient profile was used: 0–5 min, 10–40% A, and 90–60% B; 5–10 min, 40–50% A, and 60–50% B; 10–12 min 50–55% A, and 50–45% B; 12–15 min, 55% A, and 45% B; 15–18 min, 55–90% A, and 45–10% B; and 18–20 min, 10% A, and 90% B. The post time was 5 min. The chromatograms were acquired at 224 nm. The linearity range of responses of FITC dissolved in CH
3OH was determined on five concentration levels from 6.40 ng/mL to 520 ng/mL and the correlation coefficient (
R2) was 0.9994 [
26].
The encapsulation efficiency was calculated using the equation described in the previous paragraph. In this case, Wt is the total amount of the loaded FITC and Wi is the total quantity of FITC added initially during the preparation.
2.10. In Vitro Release Study
The in vitro release of AN from the NCs was investigated using the dialysis bag method. In order to simulate the physiological conditions, PBS (pH 7.4) and enzyme-free SGF and SIF were used as dissolution media. A total of 2 mL of AN–NCs suspension was deposited into the dialysis membrane (pore size 3.5 kD) and placed in 200 mL of the release medium. The temperature was set at 37 °C and the system was stirred at 150 rpm. Release into the PBS was monitored for 24 h while in SGF and for 2 h while in SIF, corresponding to the theoretical transit through the gastrointestinal tract; aliquots of one millilitre were withdrawn in duplicate and replaced with fresh dissolution medium. The samples were analysed by HPLC for the quantification of released AN. The percentage of AN released was calculated as follows:
where AN
r is the amount of AN detected by HPLC analyses and AN
tot is the total quantity of AN deposited into the dialysis membrane.
Furthermore, to evaluate the kinetics of drug release from the NCs, different mathematical models were used, i.e., zero order and first order kinetics model, the Higuchi model, the Korsmeyer–Peppas model and the Hixson–Crowell model. The best fitting model was selected according to the best regression coefficient (R2) value for the release data.
2.11. Cell Viability and Uptake Studies
The albino mouse embryonic 3T3 fibroblast cell line and the murine monocyte/macrophage cell line J774a.1 were used for cell viability and uptake studies [
27,
28]. The cell lines were maintained in Dulbecco’s Modified Eagle’s Medium (DMEM, Sigma-Aldrich) supplemented with foetal bovine serum, 100 units/mL penicillin, and 100 μg/mL streptomycin; for the 3T3 cell line, an additional glucose concentration (4.5 g/L) was used. The cells were maintained under standard culture conditions (37 °C, 5% CO
2, 95% air and 100% relative humidity).
The cells were inoculated into 96-well microplates and maintained under standard culture conditions for 24 h to test the cell viability. Thereafter, the medium was replaced with fresh medium containing different concentrations of NCs or LPs. After 24 h, a WST-8 test was performed following the kit protocol as indicated by the manufacturer and as described in [
28]. Briefly, 100 µL of DMEM supplemented with 10% WST-8 reagent was incubated in each well for 2 h at 37 °C. The formazan concentration was quantified by an optical absorbance at 450 nm, with a reference wavelength of 630 nm and by subtracting blank values. The data were expressed as a percentage of the optical absorbance with respect to the controls.
The cells were inoculated into a 33-mm petri dish and maintained under standard culture conditions for 24 h for uptake experiments. Subsequently, the medium was replaced with fresh medium containing different concentrations of FITC loaded in NCs or SUVs. After 1 h, the medium was removed and the cells were fixed in 3.6% PFA in PBS for 10 min at room temperature, stained with DAPI and analysed by confocal imaging. Images were acquired by a Leica SP7 confocal microscope and underwent no subsequent manipulation. A minimum of five different fields was acquired from each sample and all samples were performed in triplicate.
4. Discussion
In the present study, the potential of NCs is explored for the delivery of AN, a very promising active natural constituent with various potential therapeutic benefits, but due to the low bioavailability and instability in gastrointestinal media when administered with conventional dosage forms, it has never reached a milestone therapeutic potential. Accordingly, the development of suitable delivery systems for AN represents an urgent issue to formulate effective therapeutic approaches. Lipid-based delivery systems, especially vesicles, have attracted huge efforts as high bio-compatible and biodegradable nanocarriers crossing membrane delivery systems because of their resemblance to the cell membrane. One of the main drawbacks of conventional liposomes for oral administration is their poor stability in the gastrointestinal environment. By contrast, NCs can easily be lyophilised to obtain solid, stable, biocompatible and biodegradable nanovectors [
1,
2,
5,
6].
The NCs were simply developed from nanoliposomes (
Figure 2), selecting both PS and PC and cholesterol as lipid phases due to their close resemblance to natural membranes and their high compatibility for human use. Ca
2+ was selected among the diverse divalent cations to generate NCs because it can enhance membrane fusion and phagocytosis. It is well documented that calcium ions induce perturbations of the contact region and thereby promote the membrane fusion [
11,
31]. Astonishingly, in our studies, only PC and cholesterol generated monodisperse NCs with a tightly packed structure after the addition of Ca
2+. As previously reported, PS-based NCs are not stable, producing systems with elevated polydispersity because of a tendency to form stable and huge aggregates, which represents a serious drawback at the industrial level [
15]. By contrast, developed PC-based NCs were stable after lyophilisation and re-suspension in distilled water, and after incubation in simulated gastric and intestinal media. In vitro dissolution studies explained an extended release, making AN available over a prolonged period after administration. The PC-based NCs were biocompatible. Even at high concentrations, the cell morphology and vitality were not affected by internalisation. Moreover, high cellular uptake of PC-based NCs was found in macrophages using fluorescent nanovectors. After treatment of the cells with NCs, a bright fluorescent color of the cytoplasm arose due to the FITC and it was clearly distinguished from the nucleus stained with DAPI. Due to the similar uptake performances of SUVs and NCs, it is plausible that the developed NCs fuse with the cell membrane due to the interaction of calcium ions with the membrane containing negatively charged lipids, entering into the cells as nanovesicles [
11]. A distinctive geometry, together with peculiar internal interactions, makes NCs ideal as pharmaceutical carriers, which may provide unparalleled protection for the molecular species in order to be carried harmlessly toward its destination. Developed NCs are inexpensive, stable, monodisperse, highly safe, biocompatible, and cell-permeating delivery systems. Moreover, they have high EE%, and suitable drug release properties for oral delivery, but with possible uses in other routes of administration. NCs are characterised by a series of solid-lipid bilayers; the components within the interior of this structure remain intact, even though the outer layers of NCs may be exposed to harsh external environmental conditions or enzymes. This interior structure of NCs is essentially free of water and resistant to penetration by oxygen, which leads to an increased shelf-life of the formulation. NCs can be stored at room temperature or 4 °C, and can be lyophilised to a powder form. Thus, NCs can be used to formulate capsules, pills, tablets, granules, suspensions or emulsions. Due to the ease of the internalisation process, this system could be exploited by employing future in vivo experiments and could be of interest in various therapeutic options.