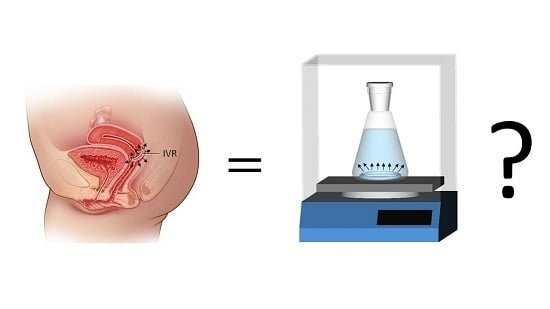
In Vitro Methods for Evaluating Drug Release of Vaginal Ring Formulations—A Critical Review
Abstract
:1. Introduction
2. Current In Vitro Methods for Evaluating Drug Release of Intravaginal Rings
2.1. Compendial Methods
2.2. Methods Described in Regulatory Guidances
2.3. Methods Described in the Relevant Literature
2.4. Methodological Approaches
2.5. Release Media
2.6. Entire Rings vs. Segments and Their Materials
2.7. Temperature
2.8. Presentation of Data
3. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hussain, A.; Ahsan, F. The vagina as a route for systemic drug delivery. J. Control. Release 2005, 103, 301–313. [Google Scholar] [CrossRef] [PubMed]
- Duncan, G.W. Medicated Devices and Methods. U.S. Patent 3,545,439, 8 December 1970. [Google Scholar]
- Friend, D.R. Development of controlled release systems over the past 50 years in the area of contraception. J. Control. Release 2016, 240, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Brache, V.; Payan, L.J.; Faundes, A. Current status of contraceptive vaginal rings. Contraception 2013, 87, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Sivin, I.; Mishell, D.R.; Alvarez, F.; Brache, V.; Elomaa, K.; Lähteenmäki, P.; Massai, R.; Miranda, P.; Croxatto, H.; Dean, C.; et al. Contraceptive vaginal rings releasing Nestorone and ethinylestradiol: A 1-year dose-finding trial. Contraception 2005, 71, 122–129. [Google Scholar] [CrossRef]
- FDA Approves New Vaginal Ring for One Year of Birth Control. Available online: http://www.fda.gov/news-events/press-announcements/fda-approves-new-vaginal-ring-one-year-birth-control (accessed on 5 June 2019).
- Vermani, K.; Garg, S.; Zaneveld, L.J.D. Assemblies for in vitro measurement of bioadhesive strength and retention characteristics in simulated vaginal environment. Drug Dev. Ind. Pharm. 2002, 28, 1133–1146. [Google Scholar] [CrossRef]
- Ferguson, L.M.; Rohan, L.C. The importance of the vaginal delivery route for antiretrovirals in HIV prevention. Ther. Deliv. 2011, 2, 1535–1550. [Google Scholar] [CrossRef] [Green Version]
- Friend, D.R.; Doncel, G.F. Combining prevention of HIV-1, other sexually transmitted infections and unintended pregnancies: Development of dual-protection technologies. Antivir. Res. 2010, 88, 47–54. [Google Scholar] [CrossRef]
- Ugaonkar, S.R.; Wesenberg, A.; Wilk, J.; Seidor, S.; Mizenina, O.; Kizima, L.; Rodriguez, A.; Zhang, S.; Levendosky, K.; Kenney, J.; et al. A novel intravaginal ring to prevent HIV-1, HSV-2, HPV, and unintended pregnancy. J. Control. Release 2015, 213, 57–68. [Google Scholar] [CrossRef] [Green Version]
- Friend, D.R. Drug delivery in multiple indication (multipurpose) prevention technologies: Systems to prevent HIV-1 transmission and unintended pregnancies or HSV-2 transmission. Expert Opin. Drug Deliv. 2012, 9, 417–427. [Google Scholar] [CrossRef]
- Friend, D.R. An update on multipurpose prevention technologies for the prevention of HIV transmission and pregnancy. Expert Opin. Drug Deliv. 2016, 13, 533–545. [Google Scholar] [CrossRef]
- Ramjee, G.; Daniels, B. Women and HIV in Sub-Saharan Africa. AIDS Res. Ther. 2013, 10, 30. [Google Scholar] [CrossRef] [PubMed]
- Dapivirine Vaginal Ring. Available online: https://www.prepwatch.org/nextgen-prep/dapivirine-vaginal-ring/ (accessed on 2 May 2019).
- Malcolm, R.K.; Boyd, P.J.; McCoy, C.F.; Murphy, D.J. Microbicide vaginal rings: Technological challenges and clinical development. Adv. Drug Deliv. Rev. 2016, 103, 33–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malcolm, R.K.; Edwards, K.-L.; Kiser, P.; Romano, J.; Smith, T.J. Advances in microbicide vaginal rings. Antivir. Res. 2010, 88, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Moss, J.A.; Malone, A.M.; Smith, T.J.; Kennedy, S.; Kopin, E.; Nguyen, C.; Gilman, J.; Butkyavichene, I.; Vincent, K.L.; Motamedi, M.; et al. Simultaneous delivery of tenofovir and acyclovir via an intravaginal ring. Antimicrob. Agents Chemother. 2012, 56, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Crowley, M.M.; Zhang, F.; Repka, M.A.; Thumma, S.; Upadhye, S.B.; Battu, S.K.; McGinity, J.W.; Martin, C. Pharmaceutical applications of hot-melt extrusion: Part I. Drug Dev. Ind. Pharm. 2007, 33, 909–926. [Google Scholar] [CrossRef]
- Repka, M.A.; Battu, S.K.; Upadhye, S.B.; Thumma, S.; Crowley, M.M.; Zhang, F.; Martin, C.; McGinity, J.W. Pharmaceutical applications of hot-melt extrusion: Part II. Drug Dev. Ind. Pharm. 2007, 33, 1043–1057. [Google Scholar] [CrossRef]
- Repka, M.A.; Majumdar, S.; Kumar Battu, S.; Srirangam, R.; Upadhye, S.B. Applications of hot-melt extrusion for drug delivery. Expert Opin. Drug Deliv. 2008, 5, 1357–1376. [Google Scholar] [CrossRef]
- Asvadi, N.H.; Dang, N.T.T.; Davis-Poynter, N.; Coombes, A.G.A. Evaluation of microporous polycaprolactone matrices for controlled delivery of antiviral microbicides to the female genital tract. J. Mater. Sci. Mater. Med. 2013, 24, 2719–2727. [Google Scholar] [CrossRef]
- Pathak, M.; Turner, M.; Palmer, C.; Coombes, A.G.A. Evaluation of polycaprolactone matrices for the intravaginal delivery of metronidazole in the treatment of bacterial vaginosis. J. Biomater. Appl. 2014, 29, 354–363. [Google Scholar] [CrossRef] [Green Version]
- Fernando, H.V.; Chan, L.L.; Dang, N.; Santhanes, D.; Banneheke, H.; Nalliah, S.; Coombes, A.G.A. Controlled delivery of the antiprotozoal agent (tinidazole) from intravaginal polymer matrices for treatment of the sexually transmitted infection, trichomoniasis. Pharm. Dev. Technol. 2019, 24, 348–356. [Google Scholar] [CrossRef]
- Moss, J.A.; Malone, A.M.; Smith, T.J.; Butkyavichene, I.; Cortez, C.; Gilman, J.; Kennedy, S.; Kopin, E.; Nguyen, C.; Sinha, P.; et al. Safety and pharmacokinetics of intravaginal rings delivering tenofovir in pig-tailed macaques. Antimicrob. Agents Chemother. 2012, 56, 5952–5960. [Google Scholar] [CrossRef] [PubMed]
- USP. United States Pharmacopoeia and National Formulary; USP42-NF37; United States Pharmacopoeia Convention, Inc.: Rockville, MD, USA, 2018. [Google Scholar]
- European Pharmacopoeia. European Pharmacopoeia, 9th ed.; Council of Europe: Strasbourg, France, 2018. [Google Scholar]
- Japanese Pharmacopoeia. Japanese Pharmacopoeia, 17th ed.; Pharmaceuticals and Medical Devices Agency: Tokyo, Japan, 2018.
- WHO. The International Pharmacopoeia; WHO Department of Essential Medicines and Health Products: Geneva, Switzerland, 2006. [Google Scholar]
- Roumen, F.J.M.E. Review of the combined contraceptive vaginal ring, NuvaRing®. Ther. Clin. Risk Manag. 2008, 4, 441–451. [Google Scholar] [CrossRef] [PubMed]
- Timmer, C.J.; Mulders, T.M. Pharmacokinetics of etonogestrel and ethinylestradiol released from a combined contraceptive vaginal ring. Clin. Pharm. 2000, 39, 233–242. [Google Scholar] [CrossRef] [PubMed]
- Malcolm, K.; Woolfson, D.; Russell, J.; Tallon, P.; McAuley, L.; Craig, D. Influence of silicone elastomer solubility and diffusivity on the in vitro release of drugs from intravaginal rings. J. Control. Release 2003, 90, 217–225. [Google Scholar] [CrossRef]
- Drugs@FDA: FDA Approved Drug Products. Available online: https://www.accessdata.fda.gov/scripts/cder/dissolution/dsp_getallData.cfm (accessed on 11 February 2019).
- Kraft, R. Method for Dissolution Testing of a Pharmaceutical Delivery Device. U.S. Patent No. 7,357,046, 15 April 2008. [Google Scholar]
- Externbrink, A.; Eggenreich, K.; Eder, S.; Mohr, S.; Nickisch, K.; Klein, S. Development and evaluation of accelerated drug release testing methods for a matrix-type intravaginal ring. Eur. J. Pharm. Biopharm. 2017, 110, 1–12. [Google Scholar] [CrossRef]
- Wang, Y.; Boyd, P.; Hunter, A.; Malcolm, R.K. Intravaginal rings for continuous low-dose administration of cervical ripening agents. Int. J. Pharm. 2018, 549, 124–132. [Google Scholar] [CrossRef] [Green Version]
- McConville, C.; Major, I.; Friend, D.R.; Clark, M.R.; Woolfson, A.D.; Malcolm, R.K. Development of polylactide and polyethylene vinyl acetate blends for the manufacture of vaginal rings. J. Biomed. Mater. Res. Part B Appl. Biomater. 2012, 100, 891–895. [Google Scholar] [CrossRef]
- Murphy, D.J.; Desjardins, D.; Dereuddre-Bosquet, N.; Brochard, P.; Perrot, L.; Pruvost, A.; Le Grand, R.; Lagatie, O.; Vanhooren, L.; Feyaerts, M.; et al. Pre-clinical development of a combination microbicide vaginal ring containing dapivirine and darunavir. J. Antimicrob. Chemother. 2014, 69, 2477–2488. [Google Scholar] [CrossRef] [Green Version]
- McConville, C.; Smith, J.M.; McCoy, C.F.; Srinivasan, P.; Mitchell, J.; Holder, A.; Otten, R.A.; Butera, S.; Doncel, G.F.; Friend, D.R.; et al. Lack of in vitro-in vivo correlation for a UC781-releasing vaginal ring in macaques. Drug Deliv. Transl. Res. 2015, 5, 27–37. [Google Scholar] [CrossRef]
- Moss, J.A.; Srinivasan, P.; Smith, T.J.; Butkyavichene, I.; Lopez, G.; Brooks, A.A.; Martin, A.; Dinh, C.T.; Smith, J.M.; Baum, M.M. Pharmacokinetics and preliminary safety study of pod-intravaginal rings delivering antiretroviral combinations for HIV prophylaxis in a macaque model. Antimicrob. Agents Chemother. 2014, 58, 5125–5135. [Google Scholar] [CrossRef]
- Fetherston, S.M.; Geer, L.; Veazey, R.S.; Goldman, L.; Murphy, D.J.; Ketas, T.J.; Klasse, P.J.; Blois, S.; La Colla, P.; Moore, J.P.; et al. Partial protection against multiple RT-SHIV162P3 vaginal challenge of rhesus macaques by a silicone elastomer vaginal ring releasing the NNRTI MC1220. J. Antimicrob. Chemother. 2013, 68, 394–403. [Google Scholar] [CrossRef] [PubMed]
- Baum, M.M.; Butkyavichene, I.; Gilman, J.; Kennedy, S.; Kopin, E.; Malone, A.M.; Nguyen, C.; Smith, T.J.; Friend, D.R.; Clark, M.R.; et al. An intravaginal ring for the simultaneous delivery of multiple drugs. J. Pharm. Sci. 2012, 101, 2833–2843. [Google Scholar] [CrossRef] [PubMed]
- Morrow, R.J.; Woolfson, A.D.; Donnelly, L.; Curran, R.; Andrews, G.; Katinger, D.; Malcolm, R.K. Sustained release of proteins from a modified vaginal ring device. Eur. J. Pharm. Biopharm. 2011, 77, 3–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loxley, A.; Mitchnick, M.; Okoh, O.; McConnell, J.; Goldman, L.; Morgan, C.; Clark, M.; Friend, D.R. Ethylene vinyl acetate intravaginal rings for the simultaneous delivery of the antiretroviral UC781 and contraceptive levonorgestrel. Drug Deliv. Transl. Res. 2011, 1, 247–255. [Google Scholar] [CrossRef]
- Boyd, P.; Fetherston, S.M.; McCoy, C.F.; Major, I.; Murphy, D.J.; Kumar, S.; Holt, J.; Brimer, A.; Blanda, W.; Devlin, B.; et al. Matrix and reservoir-type multipurpose vaginal rings for controlled release of dapivirine and levonorgestrel. Int. J. Pharm. 2016, 511, 619–629. [Google Scholar] [CrossRef] [Green Version]
- Srinivasan, P.; Moss, J.A.; Gunawardana, M.; Churchman, S.A.; Yang, F.; Dinh, C.T.; Mitchell, J.M.; Zhang, J.; Fanter, R.; Miller, C.S.; et al. Topical Delivery of Tenofovir Disoproxil Fumarate and Emtricitabine from Pod-Intravaginal Rings Protects Macaques from Multiple SHIV Exposures. PLoS ONE 2016, 11, e0157061. [Google Scholar] [CrossRef]
- Boyd, P.; Major, I.; Wang, W.; McConville, C. Development of disulfiram-loaded vaginal rings for the localised treatment of cervical cancer. Eur. J. Pharm. Biopharm. 2014, 88, 945–953. [Google Scholar] [CrossRef]
- Malcolm, R.K.; Woolfson, A.D.; Toner, C.F.; Morrow, R.J.; McCullagh, S.D. Long-term, controlled release of the HIV microbicide TMC120 from silicone elastomer vaginal rings. J. Antimicrob. Chemother. 2005, 56, 954–956. [Google Scholar] [CrossRef] [Green Version]
- McBride, J.W.; Boyd, P.; Dias, N.; Cameron, D.; Offord, R.E.; Hartley, O.; Kett, V.L.; Malcolm, R.K. Vaginal rings with exposed cores for sustained delivery of the HIV CCR5 inhibitor 5P12-RANTES. J. Control. Release 2019, 298, 1–11. [Google Scholar] [CrossRef]
- Externbrink, A.; Clark, M.R.; Friend, D.R.; Klein, S. Investigating the feasibility of temperature-controlled accelerated drug release testing for an intravaginal ring. Eur. J. Pharm. Biopharm. 2013, 85, 966–973. [Google Scholar] [CrossRef]
- Eder, S.; Beretta, M.; Witschnigg, A.; Koutsamanis, I.; Eggenreich, K.; Khinast, J.G.; Koscher, G.; Paudel, A.; Nickisch, K.; Friedrich, M.; et al. Establishment of a Molding Procedure to Facilitate Formulation Development for Co-extrudates. AAPS Pharm. Sci. Tech. 2017, 18, 2971–2976. [Google Scholar] [CrossRef] [PubMed]
- Clark, J.T.; Johnson, T.J.; Clark, M.R.; Nebeker, J.S.; Fabian, J.; Tuitupou, A.L.; Ponnapalli, S.; Smith, E.M.; Friend, D.R.; Kiser, P.F. Quantitative evaluation of a hydrophilic matrix intravaginal ring for the sustained delivery of tenofovir. J. Control. Release 2012, 163, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Johnson, T.J.; Clark, M.R.; Albright, T.H.; Nebeker, J.S.; Tuitupou, A.L.; Clark, J.T.; Fabian, J.; McCabe, R.T.; Chandra, N.; Doncel, G.F.; et al. A 90-day tenofovir reservoir intravaginal ring for mucosal HIV prophylaxis. Antimicrob. Agents Chemother. 2012, 56, 6272–6283. [Google Scholar] [CrossRef] [PubMed]
- Clark, M.R.; Johnson, T.J.; McCabe, R.T.; Clark, J.T.; Tuitupou, A.; Elgendy, H.; Friend, D.R.; Kiser, P.F. A hot-melt extruded intravaginal ring for the sustained delivery of the antiretroviral microbicide UC781. J. Pharm. Sci. 2012, 101, 576–587. [Google Scholar] [CrossRef] [PubMed]
- Mesquita, P.M.M.; Rastogi, R.; Segarra, T.J.; Teller, R.S.; Torres, N.M.; Huber, A.M.; Kiser, P.F.; Herold, B.C. Intravaginal ring delivery of tenofovir disoproxil fumarate for prevention of HIV and herpes simplex virus infection. J. Antimicrob. Chemother. 2012, 67, 1730–1738. [Google Scholar] [CrossRef] [PubMed]
- Teller, R.S.; Malaspina, D.C.; Rastogi, R.; Clark, J.T.; Szleifer, I.; Kiser, P.F. Controlling the hydration rate of a hydrophilic matrix in the core of an intravaginal ring determines antiretroviral release. J. Control. Release 2016, 224, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Traore, Y.L.; Chen, Y.; Bernier, A.-M.; Ho, E.A. Impact of Hydroxychloroquine-Loaded Polyurethane Intravaginal Rings on Lactobacilli. Antimicrob. Agents Chemother. 2015, 59, 7680–7686. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.; Traore, Y.L.; Li, A.; Fowke, K.R.; Ho, E.A. Development of polyether urethane intravaginal rings for the sustained delivery of hydroxychloroquine. Drug Des. Dev. Ther. 2014, 8, 1801–1815. [Google Scholar] [CrossRef]
- Woolfson, A.D.; Malcolm, R.K.; Gallagher, R.J. Design of a silicone reservoir intravaginal ring for the delivery of oxybutynin. J. Control. Release 2003, 91, 465–476. [Google Scholar] [CrossRef]
- Gupta, K.M.; Pearce, S.M.; Poursaid, A.E.; Aliyar, H.A.; Tresco, P.A.; Mitchnik, M.A.; Kiser, P.F. Polyurethane intravaginal ring for controlled delivery of dapivirine, a nonnucleoside reverse transcriptase inhibitor of HIV-1. J. Pharm. Sci. 2008, 97, 4228–4239. [Google Scholar] [CrossRef]
- Van Laarhoven, H.; Veurink, J.; Kruft, M.-A.; Vromans, H. Influence of Spinline Stress on Release Properties of a Coaxial Controlled Release Device Based on EVA Polymers. Pharm. Res. 2004, 21, 1811–1817. [Google Scholar] [CrossRef] [PubMed]
- Van Laarhoven, J.A.H.; Kruft, M.A.B.; Vromans, H. Effect of supersaturation and crystallization phenomena on the release properties of a controlled release device based on EVA copolymer. J. Control. Release 2002, 82, 309–317. [Google Scholar] [CrossRef]
- Van Laarhoven, J.A.H.; Kruft, M.A.B.; Vromans, H. In vitro release properties of etonogestrel and ethinyl estradiol from a contraceptive vaginal ring. Int. J. Pharm. 2002, 232, 163–173. [Google Scholar] [CrossRef]
- Helbling, I.M.; Ibarra, J.C.D.; Luna, J.A. The optimization of an intravaginal ring releasing progesterone using a mathematical model. Pharm. Res. 2014, 31, 795–808. [Google Scholar] [CrossRef] [PubMed]
- Helbling, I.M.; Ibarra, J.C.D.; Luna, J.A. Evaluation and optimization of progesterone release from intravaginal rings using response surface methodology. J. Drug Deliv. Sci. Technol. 2015, 29, 218–225. [Google Scholar] [CrossRef]
- Helbling, I.M.; Ibarra, J.C.D.; Luna, J.A. The Use of Cellulose Membrane to Eliminate Burst Release from Intravaginal Rings. AAPS J. 2016, 18, 960–971. [Google Scholar] [CrossRef] [PubMed]
- Verstraelen, H.; Vervaet, C.; Remon, J.-P. Rationale and Safety Assessment of a Novel Intravaginal Drug-Delivery System with Sustained DL-Lactic Acid Release, Intended for Long-Term Protection of the Vaginal Microbiome. PLoS ONE 2016, 11, e0153441. [Google Scholar] [CrossRef]
- Xia, L.; Qiu, S.; Liu, Z.; Ning, M. Preparation and in vitro/in vivo evaluation of anastrozole reservoir-type intravaginal ring. Biomed. Chromatogr. 2019, 33, e4459. [Google Scholar] [CrossRef]
- Pathak, M.; Coombes, A.G.A.; Turner, M.S.; Palmer, C.; Wang, D.; Steadman, K.J. Investigation of Polycaprolactone Matrices for Intravaginal Delivery of Doxycycline. J. Pharm. Sci. 2015, 104, 4217–4222. [Google Scholar] [CrossRef]
- Dang, N.T.T.; Turner, M.S.; Coombes, A.G.A. Development of intra-vaginal matrices from polycaprolactone for sustained release of antimicrobial agents. J. Biomater. Appl. 2013, 28, 74–83. [Google Scholar] [CrossRef]
- Moss, J.A.; Butkyavichene, I.; Churchman, S.A.; Gunawardana, M.; Fanter, R.; Miller, C.S.; Yang, F.; Easley, J.T.; Marzinke, M.A.; Hendrix, C.W.; et al. Combination Pod-Intravaginal Ring Delivers Antiretroviral Agents for HIV Prophylaxis: Pharmacokinetic Evaluation in an Ovine Model. Antimicrob. Agents Chemother. 2016, 60, 3759–3766. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rotgeri, A.; Korolainen, H.; Sundholm, O.; Schmitz, H.; Fuhrmann, U.; Prelle, K.; Sacher, F. Characterization of anastrozole effects, delivered by an intravaginal ring in cynomolgus monkeys. Hum. Reprod. 2015, 30, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Reinecke, I.; Schultze-Mosgau, M.-H.; Nave, R.; Schmitz, H.; Ploeger, B.A. Model-Based Dose Selection for Intravaginal Ring Formulations Releasing Anastrozole and Levonorgestrel Intended for the Treatment of Endometriosis Symptoms. J. Clin. Pharmacol. 2017, 57, 640–651. [Google Scholar] [CrossRef] [PubMed]
- Clark, J.T.; Clark, M.R.; Shelke, N.B.; Johnson, T.J.; Smith, E.M.; Andreasen, A.K.; Nebeker, J.S.; Fabian, J.; Friend, D.R.; Kiser, P.F. Engineering a segmented dual-reservoir polyurethane intravaginal ring for simultaneous prevention of HIV transmission and unwanted pregnancy. PLoS ONE 2014, 9, e88509. [Google Scholar] [CrossRef] [PubMed]
- Johnson, T.J.; Srinivasan, P.; Albright, T.H.; Watson-Buckheit, K.; Rabe, L.; Martin, A.; Pau, C.-P.; Hendry, R.M.; Otten, R.; McNicholl, J.; et al. Safe and sustained vaginal delivery of pyrimidinedione HIV-1 inhibitors from polyurethane intravaginal rings. Antimicrob. Agents Chemother. 2012, 56, 1291–1299. [Google Scholar] [CrossRef] [PubMed]
- Murphy, D.J.; Boyd, P.; McCoy, C.F.; Kumar, S.; Holt, J.D.S.; Blanda, W.; Brimer, A.N.; Malcolm, R.K. Controlling levonorgestrel binding and release in a multi-purpose prevention technology vaginal ring device. J. Control. Release 2016, 226, 138–147. [Google Scholar] [CrossRef] [Green Version]
- Johnson, T.J.; Gupta, K.M.; Fabian, J.; Albright, T.H.; Kiser, P.F. Segmented polyurethane intravaginal rings for the sustained combined delivery of antiretroviral agents dapivirine and tenofovir. Eur. J. Pharm. Sci. 2010, 39, 203–212. [Google Scholar] [CrossRef]
- Kaur, M.; Gupta, K.M.; Poursaid, A.E.; Karra, P.; Mahalingam, A.; Aliyar, H.A.; Kiser, P.F. Engineering a degradable polyurethane intravaginal ring for sustained delivery of dapivirine. Drug Deliv. Transl. Res. 2011, 1, 223–237. [Google Scholar] [CrossRef]
- Fetherston, S.M.; Boyd, P.; McCoy, C.F.; McBride, M.C.; Edwards, K.-L.; Ampofo, S.; Malcolm, R.K. A silicone elastomer vaginal ring for HIV prevention containing two microbicides with different mechanisms of action. Eur. J. Pharm. Sci. 2013, 48, 406–415. [Google Scholar] [CrossRef] [Green Version]
- Murphy, D.J.; Desjardins, D.; Boyd, P.; Dereuddre-Bosquet, N.; Stimmer, L.; Caldwell, A.; Le Grand, R.; Kelly, C.; van Roey, J.; Malcolm, R.K. Impact of ring size and drug loading on the pharmacokinetics of a combination dapivirine-darunavir vaginal ring in cynomolgus macaques. Int. J. Pharm. 2018, 550, 300–308. [Google Scholar] [CrossRef] [Green Version]
- McCoy, C.F.; Murphy, D.J.; Boyd, P.; Derrick, T.; Spence, P.; Devlin, B.; Malcolm, R.K. Packing Polymorphism of Dapivirine and Its Impact on the Performance of a Dapivirine-Releasing Silicone Elastomer Vaginal Ring. J. Pharm. Sci. 2017, 106, 2015–2025. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weiss, H.; Martell, B.; Constantine, G.D.; Davis, S.M.; Vidal, J.D.; Mayer, P.R.; Doorbar, M.; Friend, D.R. Pharmacokinetics and tolerability of a novel progesterone intravaginal ring in sheep. Drug Deliv. Transl. Res. 2019, 9, 1008–1016. [Google Scholar] [CrossRef] [PubMed]
- Weiss, H.; Martell, B.; Constantine, G.D.; Davis, S.M.; Vidal, J.D.; Mayer, P.R.; Doorbar, M.; Friend, D.R. Pharmacokinetics and Tolerability of a Novel 17β-Estradiol and Progesterone Intravaginal Ring in Sheep. J. Pharm. Sci. 2019, 108, 2677–2684. [Google Scholar] [CrossRef] [PubMed]
- Nave, R.; Jalkanen, T.; Talling, C.; Kaneko, M.; Matsuki, S.; Höchel, J. The Effect of Drug Content Reduction on the in Vitro and in Vivo Properties of Levonorgestrel-Releasing Intravaginal Rings. J. Pharm. Sci. 2018, 107, 1020–1027. [Google Scholar] [CrossRef]
- Owen, D.H.; Katz, D.F. A vaginal fluid simulant. Contraception 1999, 59, 91–95. [Google Scholar] [CrossRef]
- Tietz, K.; Klein, S. Simulated Genital Tract Fluids and Their Applicability in Drug Release/Dissolution Testing of Vaginal Dosage Forms. Dissolut. Technol. 2018, 25, 40–51. [Google Scholar] [CrossRef]
- Owen, D.H.; Katz, D.F. A review of the physical and chemical properties of human semen and the formulation of a semen simulant. J. Androl. 2005, 26, 459–469. [Google Scholar] [CrossRef]
- Raffi, R.O.; Moghissi, K.S.; Sacco, A.G. Proteins of human vaginal fluid. Fertil. Steril. 1977, 28, 1345–1348. [Google Scholar] [CrossRef]
- Tomas, M.S.J.; Nader-Macias, M.E. Effect of a medium simulating vaginal fluid on the growth and expression of beneficial characteristics of potentially probiotic lactobacilli. Commun. Curr. Res. Educ. Top. Trends Appl. Microbiol. 2007, 2, 732–739. [Google Scholar]
- Dorr, R.T.; Surwit, E.A.; Droegemueller, W.; Alberts, D.S.; Meyskens, F.L.; Chvapil, M. In vitro retinoid binding and release from a collagen sponge material in a simulated intravaginal environment. J. Biomed. Mater. Res. 1982, 16, 839–850. [Google Scholar] [CrossRef] [Green Version]
- Timmer, C.J.; Apter, D.; Voortman, G. Pharmacokinetics of 3-keto-desogestrel and ethinylestradiol released from different types of contraceptive vaginal rings. Contraception 1990, 42, 629–642. [Google Scholar] [CrossRef]
- Shanbhag, V.P.; Södergård, R. The temperature dependence of the binding of 5α-dihydrotestosterone, testosterone and estradiol to the sex hormone globulin (SHBG) of human plasma. J. Steroid Biochem. 1986, 24, 549–555. [Google Scholar] [CrossRef]
- Kuhnz, W.; Pfeffer, M.; Al-Yacoub, G. Protein binding of the contraceptive steroids gestodene, 3-keto-desogestrel and ethinylestradiol in human serum. J. Steroid Biochem. 1990, 35, 313–318. [Google Scholar] [CrossRef]
- Hammond, G.L.; Bocchinfuso, W.P.; Orava, M.; Smith, C.L.; van den Ende, A.; van Enk, A. Serum distribution of two contraceptive progestins: 3-ketodesogestrel and gestodene. Contraception 1994, 50, 301–318. [Google Scholar] [CrossRef]
- Clark, M.R.; Kiser, P.F.; Loxley, A.; McConville, C.; Malcolm, R.K.; Friend, D.R. Pharmacokinetics of UC781-loaded intravaginal ring segments in rabbits: A comparison of polymer matrices. Drug Deliv. Transl. Res. 2011, 1, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Murphy, D.J.; McCoy, C.F.; Boyd, P.; Derrick, T.; Spence, P.; Devlin, B.; Malcolm, R.K. Drug stability and product performance characteristics of a dapivirine-releasing vaginal ring under simulated real-world conditions. Int. J. Pharm. 2019, 565, 351–357. [Google Scholar] [CrossRef] [PubMed]


| IVR | Indication | API | Status | Reference(s) |
|---|---|---|---|---|
| Estring® | hormone replacement | 17β-Estradiol | marketed worldwide | [3] |
| Femring® | hormone replacement | 17β-Estradiol-3-acetate | marketed worldwide | [3] |
| NuvaRing® & generics | contraception | Ethinyl estradiol & etonogestrel | marketed worldwide | [3,4] |
| Progering®/Fertiring® | contraception | Progesterone | Peru and Chile | [3,4] |
| Annovera® | contraception | Ethinyl estradiol & segesterone acetate | FDA-approved | [5,6] |
| Drug | Apparatus | Speed | Medium | Volume | Sampling |
|---|---|---|---|---|---|
| Estradiol | Incubator shaker | 130 rpm | 0.9% saline | 250 mL | 1, 9, 16, 17, 18, 19, 45 d |
| Ethinyl estradiol & etonogestrel | Develop a method to characterize in vitro release | ||||
| Author(s) | API | Ring Material | Test Method | Formulation Tested | Test Medium | Agitation and Temperature |
|---|---|---|---|---|---|---|
| Asvadi et al. [21] | Acyclovir | PCL matrices as inserts for an IVR | Matrices were immersed in release medium in PP tubes | S | 10 mL of VFS | Not specified |
| Externbrink et al. [34] | Ethinyl estradiol and etonogestrel | PEVA | Incubator shaker, USP apparatus 7 (400-DS) | E, S | AB and different hydro-organic media, 100 mL/10 mL (400-DS) | 130 rpm/40 dpm, 37 and 45 °C |
| Wang et al. [35] | Isosorbide mononitrate, misoprostol | Silicone elastomer | Incubator shaker | E | 50 mL VFS | 60 rpm, 37 °C |
| Mc Conville et al. [36] | Tenofovir | PLA, PEVA | Incubator shaker | R | 5 mL of VFS | 60 rpm, 37 °C |
| Murphy et al. [37] | Dapivirine and darunavir | Silicone elastomer | Incubator shaker | MSR | 100 mL of IPA:H2O (1:1) or VFS | 60 rpm, 37 °C |
| McConville et al. [38] | UC781 | Silicone elastomer | Incubator shaker | R, MSR | 100 mL of EtOH:H2O (1:1) or 1% aqueous BAC solution; 50 or 100 mL of IPA:H2O (1:1) | 60 rpm, 37 °C |
| Moss et al. [39] | Tenofovir disoproxil fumarate, emtricitabine, maraviroc | PDMS | Incubator shaker | MSR | 100 mL VFS | 60 rpm, 25 °C |
| Fetherston et al. [40] | MC1220 | Silicone elastomer | Incubator shaker | MSR | 50 mL VFS or 200 mL IPA:H2O (1:1) | 60 rpm, 37 °C |
| Baum et al. [41] | Tenofovir and acyclovir | Silicone elastomer with PLA pods | Incubator shaker | E, S | 100 mL VFS | 60 rpm, 25 °C |
| Morrow et al. [42] | BSA and monoclonal antibody 2F5 | Silicone elastomer | Incubator shaker | E | 30 mL ammonium acetate buffer | 60 rpm, 37 °C |
| Loxley et al. [43] | UC781 | PEVA | Incubator shaker | E | 100 mL IPA:H2O (1:1) | 60 rpm, 37 °C |
| Boyd et al. [44] | Dapivirine and levonorgestrel | Silicone elastomer | Incubator shaker | E | 50/200 mL IPA:H2O (1:1) (reservoir vs. matrix) | 60 rpm, 37 °C |
| Srinivasan et al. [45] | Tenofovir disoproxil fumarate, emtricitabine and maraviroc | PDMS | Incubator shaker | MSR | 100 mL VFS | 60 rpm, 37 °C |
| Boyd et al. [46] | Disulfiram | PEVA | Incubator shaker | E | 100 mL 2% SDS solution or 20 mL water | 60 rpm, 37 °C |
| Boyd et al. [46] | Disulfiram | PEVA | Dual chambered release method, in an incubator shaker | E | Latex balloon with 20 mL of water, balloons were submerged in 100 mL of 2% SDS solution | 60 rpm, 37 °C |
| Malcolm et al. [47] | TMC120 | Silicone elastomer | Incubator shaker | E | 200 mL IPA:H2O (1:1) | 60 rpm, 37 °C |
| Malcolm et al. [31] | 17β-Estradiol, 17β-Estradiol-3-acetate, metronidazole, norethisterone, norethisterone acetate, clindamycin, oxybutynin | Silicone elastomer | Incubator shaker | E | 100 mL 1% aqueous BAC solution/ phosphate buffer | 60 rpm, 37 °C |
| Mc Bride et al. [48] | 5P12-RANTES | Silicone elastomer | Incubator shaker | E | 15 mL Type 1 water | 60 rpm, 37 °C |
| Externbrink et al. [49] | Ethinyl estradiol and etonogestrel | PEVA | USP apparatus 7 (400-DS) | S | 10 mL VFS or water | 37, 44, 50 and 55 °C, 40 dpm |
| Eder et al. [50] | Ethinyl estradiol and etonogestrel | PEVA | Incubator shaker | S | 30 mL MilliQ water | 130 rpm, 37 °C |
| Clark, J. et al. [51] | Tenofovir | PU | Incubator shaker | E | AB, volume not specified | 80 rpm, 37 °C |
| Johnson et al. [52] | Tenofovir | PU | Incubator shaker | E | 50 mL AB | 80 rpm, 37 °C |
| Clark, M. et al. [53] | UC781 | PU | Incubator shaker | S | 100 mL AB or PPB containing 2% Solutol HS-15 | 80 rpm, 37 °C |
| Mesquita et al. [54] | Nonoxynol-9, acyclovir, tenofovir and tenofovir disoproxil fumarate | PU, PEVA, silicone elastomer | Incubator shaker | S | VFS, volume not specified | 80 rpm, 37 °C |
| Teller et al. [55] | Dapivirine, maraviroc, tenofovir and tenofovir disoproxil fumarate, rhodamine B dextrane | PU with flux controlled pumps | Incubator shaker | FCPs | 20 mL AB | 80 rpm, 37 °C |
| Traore et al. [56] | Hydroxychloroquine | PU | Incubator shaker | MSR S | 5 mL AB or 5 mL MRS broth | 100 rpm, 37 °C |
| Chen et al. [57] | Hydroxychloroquine | PU | Incubator shaker | S | AB, volume not specified | 100 rpm, 37 °C |
| Woolfson et al. [58] | Oxybutynin | Silicone elastomer | Incubator shaker | E | 100 mL AB | 100 rpm, 37 °C |
| Moss et al. [17] | Tenofovir and acyclovir | Silicone elastomer | Incubator shaker | SSR and S | 100 mL VFS | 110 rpm, 25 °C |
| Gupta et al. [59] | Dapivirine | PU ring with rods | Water bath shaker | S and E | 5 mL 25:75 IPA:H2O, 50 mL 25:75 IPA:H2O | 64 rpm, 37 °C |
| van Laarhoven et al. [60,61,62] | Ethinyl estradiol and etonogestrel | PEVA | Automated release control system | E | 200 mL water | 750 rpm, 37 °C |
| Helbling et al. [63,64,65] | Progesterone | PEVA | USP apparatus 1 | E | 1000 mL 20: 80 EtOH:H2O | 25 rpm or 100 rpm, 37 °C |
| Verstraelen et al. [66] | Lactic acid | PEVA, Eudragit L 100 | Incubation | S | 5 mL demineralized water | 37 °C, agitation not specified |
| Xia et al. [67] | Anastrozole | Silicone elastomer | USP apparatus 2 | E | 250 mL water | 50 rpm, 37 °C |
| Pathak et al. [68] | Doxycycline | PCL matrices as inserts for an IVR | Incubation | S | 10 mL VFS | 37 °C, agitation not specified |
| Ugaonkar et al. [10] | MIV-150, levonorgestel, carrageenan, zinc acetate | PEVA | Incubator shaker | MSR | 10 mL AB | 37 °C, 100 rpm |
| Pathak et al. [22] | Metronidazole | PCL matrices as inserts for an IVR | Incubation | S | 10 mL VFS | 37 °C, agitation not specified |
| Dang et al. [69] | Tenofovir | PCL matrices as inserts for an IVR | Incubation | S | 10 mL VFS | 37 °C, agitation not specified |
| Moss et al. [70] | Tenofovir disoproxil fumarate and maraviroc | PDMS | Incubator shaker | SSR | 100 mL VFS | 60 rpm, 25 °C |
| Rotgeri et al. [71] | Anastrozole | PDMS | Incubator shaker | MSR | 75 mL 1% aqueous hydroxy-propyl-β-cyclodextrin solution | 100 rpm, 37 °C |
| Reinecke et al. [72] | Anastrozole and levonorgestrel | Not specified | Incubator shaker | Not specified | 1% aqueous hydroxy-propyl-β-cyclodextrin solution, volume not specified | 37 °C, agitation not specified |
| Clark, J. et al. [73] | Tenofovir and levonorgestrel | PU | Incubator shaker | E, S | 2% Solutol in AB, volume not specified | 80 rpm, 37 °C |
| Johnson et al. [74] | Pyrimidinedione | PU | Not specified | MSR | 2% Solutol in AB or 0.05% Solutol in AB, volume not specified | Not specified |
| Murphy et al. [75] | Dapivirine and levonorgestrel | Silicone elastomer | Incubator shaker | E | 200 mL IPA:H2O (1:1) | 60 rpm, 37 °C |
| Johnson et al. [76] | Dapivirine and tenofovir | PU | Water bath shaker | S | 5 mL 25:75 IPA:AB | 64 rpm, 37 °C |
| Kaur et al. [77] | Dapivirine | PU | Water bath shaker | S | 5 mL IPA:AB (25:75) | 60 rpm, 37 °C |
| Fetherston et al. [78] | Dapivirine and maraviroc | Silicone elastomer | Incubator shaker | E | 200 mL IPA:H2O (1:1) | 60 rpm, 37 °C |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tietz, K.; Klein, S. In Vitro Methods for Evaluating Drug Release of Vaginal Ring Formulations—A Critical Review. Pharmaceutics 2019, 11, 538. https://doi.org/10.3390/pharmaceutics11100538
Tietz K, Klein S. In Vitro Methods for Evaluating Drug Release of Vaginal Ring Formulations—A Critical Review. Pharmaceutics. 2019; 11(10):538. https://doi.org/10.3390/pharmaceutics11100538
Chicago/Turabian StyleTietz, Katharina, and Sandra Klein. 2019. "In Vitro Methods for Evaluating Drug Release of Vaginal Ring Formulations—A Critical Review" Pharmaceutics 11, no. 10: 538. https://doi.org/10.3390/pharmaceutics11100538
APA StyleTietz, K., & Klein, S. (2019). In Vitro Methods for Evaluating Drug Release of Vaginal Ring Formulations—A Critical Review. Pharmaceutics, 11(10), 538. https://doi.org/10.3390/pharmaceutics11100538