Mesenchymal Stem Cell Derived Biocompatible Membrane Vesicles Demonstrate Immunomodulatory Activity Inhibiting Activation and Proliferation of Human Mononuclear Cells
Abstract
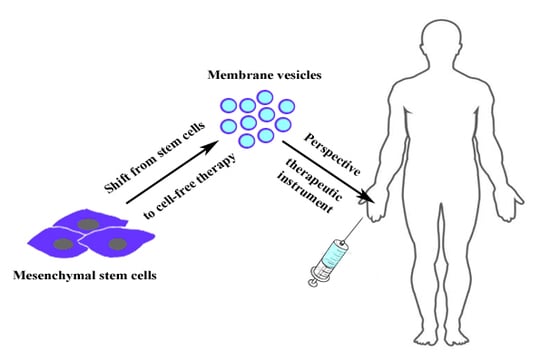
:1. Introduction
2. Materials and Methods
2.1. PBMC Isolation
2.2. FACS-Based Sorting of PBMCs
2.3. CFDA SE Staining of PBMC
2.4. CIMVs Production
2.5. Staining with Calcein AM
2.6. Flow Cytometry Analysis with Calibration Particles
2.7. Scanning Electron Microscopy (SEM)
2.8. Staining of CIMVS with DiD
2.9. Phytohemagglutinin (PHA) Activation
2.10. Multiplex Analysis
2.11. Animals
2.12. Immunostaining of Murine PBMCs
2.13. Statistical Analysis
3. Results
3.1. CIMVs Isolation Procedure
3.2. CIMVs Uptake by Leukocytes
3.3. CIMVs-MCSs Inhibition of PHA-Induced Proliferation of PBMCs
3.4. Immunosuppressive Activity of CIMVs
3.5. Multiplex Analysis
3.6. Transplantation of Allogeneic and Xenogeneic CIMVs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Data Availability
References
- Gomzikova, M.O.; James, V.; Rizvanov, A.A. Therapeutic Application of Mesenchymal Stem Cells Derived Extracellular Vesicles for Immunomodulation. Front. Immunol. 2019, 10. [Google Scholar] [CrossRef]
- Gomzikova, M.O.; Rizvanov, A.A. Current Trends in Regenerative Medicine: From Cell to Cell-Free Therapy. Bionanoscience 2017, 7, 240–245. [Google Scholar] [CrossRef]
- Zhou, Y.; Yamamoto, Y.; Xiao, Z.; Ochiya, T. The Immunomodulatory Functions of Mesenchymal Stromal/Stem Cells Mediated via Paracrine Activity. J. Clin. Med. 2019, 8, 1025. [Google Scholar] [CrossRef] [Green Version]
- Tatsumi, K.; Ohashi, K.; Matsubara, Y.; Kohori, A.; Ohno, T.; Kakidachi, H.; Horii, A.; Kanegae, K.; Utoh, R.; Iwata, T.; et al. Tissue factor triggers procoagulation in transplanted mesenchymal stem cells leading to thromboembolism. Biochem. Biophys. Res. Commun. 2013, 431, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Di Trapani, M.; Bassi, G.; Midolo, M.; Gatti, A.; Kamga, P.T.; Cassaro, A.; Carusone, R.; Adamo, A.; Krampera, M. Differential and transferable modulatory effects of mesenchymal stromal cell-derived extracellular vesicles on T, B and NK cell functions. Sci. Rep. 2016, 6, 24120. [Google Scholar] [CrossRef]
- Seo, Y.; Kim, H.S.; Hong, I.S. Stem Cell-Derived Extracellular Vesicles as Immunomodulatory Therapeutics. Stem. Cells Int. 2019. [Google Scholar] [CrossRef]
- Kordelas, L.; Rebmann, V.; Ludwig, A.K.; Radtke, S.; Ruesing, J.; Doeppner, T.R.; Epple, M.; Horn, P.A.; Beelen, D.W.; Giebel, B. MSC-derived exosomes: A novel tool to treat therapy-refractory graft-versus-host disease. Leukemia 2014, 28, 970–973. [Google Scholar] [CrossRef] [PubMed]
- Nassar, W.; El-Ansary, M.; Sabry, D.; Mostafa, M.A.; Fayad, T.; Kotb, E.; Temraz, M.; Saad, A.N.; Essa, W.; Adel, H. Umbilical cord mesenchymal stem cells derived extracellular vesicles can safely ameliorate the progression of chronic kidney diseases. Biomater. Res. 2016, 20, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phan, J.; Kumar, P.; Hao, D.; Gao, K.; Farmer, D.; Wang, A.J. Engineering mesenchymal stem cells to improve their exosome efficacy and yield for cell-free therapy. J. Extracell Vesicles 2018, 7. [Google Scholar] [CrossRef]
- Pick, H.; Schmid, E.L.; Tairi, A.P.; Ilegems, E.; Hovius, R.; Vogel, H. Investigating cellular signaling reactions in single attoliter vesicles. J. Am. Chem. Soc. 2005, 127, 2908–2912. [Google Scholar] [CrossRef]
- Mao, Z.; Cartier, R.; Hohl, A.; Farinacci, M.; Dorhoi, A.; Nguyen, T.L.; Mulvaney, P.; Ralston, J.; Kaufmann, S.H.; Mohwald, H.; et al. Cells as factories for humanized encapsulation. Nano Lett. 2011, 11, 2152–2156. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.H.; Park, J.; Oh, E.H.; Ko, H.J.; Hong, S.; Park, T.H. Nanovesicle-based bioelectronic nose for the diagnosis of lung cancer from human blood. Adv. Healthc. Mater. 2014, 3, 360–366. [Google Scholar] [CrossRef] [PubMed]
- Eyer, K.; Herger, M.; Kramer, S.D.; Dittrich, P.S. Cell-free microfluidic determination of P-glycoprotein interactions with substrates and inhibitors. Pharm. Res. 2014, 31, 3415–3425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomzikova, M.O.; Zhuravleva, M.N.; Miftakhova, R.R.; Arkhipova, S.S.; Evtugin, V.G.; Khaiboullina, S.F.; Kiyasov, A.P.; Persson, J.L.; Mongan, N.P.; Pestell, R.G.; et al. Cytochalasin B-induced membrane vesicles convey angiogenic activity of parental cells. Oncotarget 2017, 8, 70496–70507. [Google Scholar] [CrossRef]
- Gomzikova, M.; Kletukhina, S.; Kurbangaleeva, S.; Rizvanov, A. Evaluation of Cytochalasin B-Induced Membrane Vesicles Fusion Specificity with Target Cells. Biomed. Res. Int. 2018, 2018, 7053623. [Google Scholar] [CrossRef] [Green Version]
- Gomzikova, M.O.; Zhuravleva, M.N.; Vorobev, V.V.; Salafutdinov, I.I.; Laikov, A.V.; Kletukhina, S.K.; Martynova, E.V.; Tazetdinova, L.G.; Ntekim, A.I.; Khaiboullina, S.F.; et al. Angiogenic Activity of Cytochalasin B-Induced Membrane Vesicles of Human Mesenchymal Stem Cells. Cells 2019, 9, 95. [Google Scholar] [CrossRef] [Green Version]
- Peng, L.H.; Zhang, Y.H.; Han, L.J.; Zhang, C.Z.; Wu, J.H.; Wang, X.R.; Gao, J.Q.; Mao, Z.W. Cell Membrane Capsules for Encapsulation of Chemotherapeutic and Cancer Cell Targeting in Vivo. ACS Appl. Mater. Inter. 2015, 7, 18628–18637. [Google Scholar] [CrossRef]
- Gomzikova, M.O.; Aimaletdinov, A.M.; Bondar, O.V.; Starostina, I.G.; Gorshkova, N.V.; Neustroeva, O.A.; Kletukhina, S.K.; Kurbangaleeva, S.V.; Vorobev, V.V.; Garanina, E.E.; et al. Immunosuppressive properties of cytochalasin B-induced membrane vesicles of mesenchymal stem cells: Comparing with extracellular vesicles derived from mesenchymal stem cells. Sci. Rep. 2020. [Google Scholar] [CrossRef]
- Wise, G.E.; Prescott, D.M. Ultrastructure of enucleated mammalian cells in culture. Exp. Cell Res. 1973, 81, 63–72. [Google Scholar] [CrossRef]
- Chao, K.H.; Wu, M.Y.; Yang, J.H.; Chen, S.U.; Yang, Y.S.; Ho, H.N. Expression of the interleukin-2 receptor alpha (CD25) is selectively decreased on decidual CD4+ and CD8+ T lymphocytes in normal pregnancies. Mol. Hum. Reprod. 2002, 8, 667–673. [Google Scholar] [CrossRef] [Green Version]
- Shatrova, A.N.; Mityushova, E.V.; Vassilieva, I.O.; Aksenov, N.D.; Zenin, V.V.; Nikolsky, N.N.; Marakhova, I.I. Time-Dependent Regulation of IL-2R alpha-Chain (CD25) Expression by TCR Signal Strength and IL-2-Induced STAT5 Signaling in Activated Human Blood T Lymphocytes. PLoS ONE 2016, 11, e0167215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amu, S.; Gjertsson, I.; Brisslert, M. Functional characterization of murine CD25 expressing B cells. Scand. J. Immunol. 2010, 71, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Regmi, S.; Pathak, S.; Kim, J.O.; Yong, C.S.; Jeong, J.H. Mesenchymal stem cell therapy for the treatment of inflammatory diseases: Challenges, opportunities, and future perspectives. Eur. J. Cell Biol. 2019, 98, 151041. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Riano, A.; Bovolenta, E.R.; Mendoza, P.; Oeste, C.L.; Martin-Bermejo, M.J.; Bovolenta, P.; Turner, M.; Martinez-Martin, N.; Alarcon, B. Antigen phagocytosis by B cells is required for a potent humoral response. EMBO Rep. 2018, 19. [Google Scholar] [CrossRef]
- Khare, D.; Or, R.; Resnick, I.; Barkatz, C.; Almogi-Hazan, O.; Avni, B. Mesenchymal Stromal Cell-Derived Exosomes Affect mRNA Expression and Function of B-Lymphocytes. Front. Immunol. 2018, 9, 3053. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, S.; Horwood, N.; Cope, A.; Dazzi, F. The antiproliferative effect of mesenchymal stem cells is a fundamental property shared by all stromal cells. J. Immunol. 2007, 179, 2824–2831. [Google Scholar] [CrossRef]
- Yang, H.; Sun, J.; Li, Y.; Duan, W.M.; Bi, J.; Qu, T. Human umbilical cord-derived mesenchymal stem cells suppress proliferation of PHA-activated lymphocytes in vitro by inducing CD4(+)CD25(high)CD45RA(+) regulatory T cell production and modulating cytokine secretion. Cell Immunol. 2016, 302, 26–31. [Google Scholar] [CrossRef] [Green Version]
- Yoo, H.S.; Lee, K.; Na, K.; Zhang, Y.X.; Lim, H.J.; Yi, T.; Song, S.U.; Jeon, M.S. Mesenchymal stromal cells inhibit CD25 expression via the mTOR pathway to potentiate T-cell suppression. Cell Death Dis. 2017, 8, e2632. [Google Scholar] [CrossRef]
- Le Blanc, K.; Rasmusson, I.; Gotherstrom, C.; Seidel, C.; Sundberg, B.; Sundin, M.; Rosendahl, K.; Tammik, C.; Ringden, O. Mesenchymal stem cells inhibit the expression of CD25 (interleukin-2 receptor) and CD38 on phytohaemagglutinin-activated lymphocytes. Scand. J. Immunol. 2004, 60, 307–315. [Google Scholar] [CrossRef]
- Bertolo, A.; Pavlicek, D.; Gemperli, A.; Baur, M.; Potzel, T.; Stoyanov, J. Increased motility of mesenchymal stem cells is correlated with inhibition of stimulated peripheral blood mononuclear cells in vitro. J. Stem Cells Regen. Med. 2017, 13, 62–74. [Google Scholar]
- English, K. Mechanisms of mesenchymal stromal cell immunomodulation. Immunol. Cell Biol. 2013, 91, 19–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DelaRosa, O.; Lombardo, E.; Beraza, A.; Mancheno-Corvo, P.; Ramirez, C.; Menta, R.; Rico, L.; Camarillo, E.; Garcia, L.; Abad, J.L.; et al. Requirement of IFN-gamma-mediated indoleamine 2,3-dioxygenase expression in the modulation of lymphocyte proliferation by human adipose-derived stem cells. Tissue Eng. Part. A 2009, 15, 2795–2806. [Google Scholar] [CrossRef] [PubMed]
- Ren, K.; Torres, R. Role of interleukin-1beta during pain and inflammation. Brain Res. Rev. 2009, 60, 57–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kouro, T.; Takatsu, K. IL-5- and eosinophil-mediated inflammation: From discovery to therapy. Int. Immunol. 2009, 21, 1303–1309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rozenberg, A.; Rezk, A.; Boivin, M.N.; Darlington, P.J.; Nyirenda, M.; Li, R.; Jalili, F.; Winer, R.; Artsy, E.A.; Uccelli, A.; et al. Human Mesenchymal Stem Cells Impact Th17 and Th1 Responses Through a Prostaglandin E2 and Myeloid-Dependent Mechanism. Stem Cells Transl. Med. 2016, 5, 1506–1514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rasmusson, I.; Le Blanc, K.; Sundberg, B.; Ringdén, O. Mesenchymal Stem Cells Stimulate Antibody Secretion in Human B Cells. Scand. J. Immunol. 2007, 65, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Le Blanc, K.; Tammik, C.; Rosendahl, K.; Zetterberg, E.; Ringden, O. HLA expression and immunologic properties of differentiated and undifferentiated mesenchymal stem cells. Exp. Hematol. 2003, 31, 890–896. [Google Scholar] [CrossRef]







| Cytokine | PBMCs | PBMCs+CIMVs-MSCs | CD4+ Cells | CD4+cells+ CIMVs-MSCs | CD8+ Cells | CD8+cells+ CIMVs-MSCs |
|---|---|---|---|---|---|---|
| EGF | 89.01 ± 17.96 | 60.31 ± 4.15 | 9.91 ± 2.12 | 9.51 ± 1.15 | 10.56 ± 2.73 | 11.13 ± 0.66 |
| FGF-2 | 9.81 ± 2.02 | 2204.22 ± 108.62 | <5.94 | 2656.99 ± 141.89 | <5.94 | 2576.9 ± 229.82 |
| Eotaxin (CCL11) | 10.85 ± 1.9 | 11.34 ± 1.39 | 1.38 | 3.03 ± 0.37 | <0.72 | 2.1 ± 1.02 |
| TGF-a | 7.07 ± 0.83 | 8.36 ± 0.51 | <0.81 | <0.81 | <0.81 | <0.81 |
| G-CSF | 2434.68 ± 313.12 | 4823.67 ± 1358.55 | 3.29 ± 2.79 | 28.53 ± 5.31 | <1.82 | 73.76 ± 15.37 |
| GM-CSF | 66.63 ± 10.38 | 109.33 ± 14.5 | 1.13 ± 0.93 | 1.07 ± 0.05 | 2.51 | 3.57 ± 0.14 |
| Fractalkine (CX3CL1) | 43.73 ± 15.99 | 16.79 ± 3.85 | <3.2 | <3.2 | <3.2 | <3.2 |
| IFN-a2 | 53.9 ± 24.33 | 84.06 ± 47.18 | <1.27 | <1.27 | <1.27 | <1.27 |
| IL-10 | 3086.13 ± 112.82 | 3429.61 ± 576.28 | <0.4 | <0.4 | <0.4 | <0.4 |
| MCP-3 (CCL7) | 179.34 ± 22.65 | 272.61 ± 30.47 | <3.41 | <3.41 | <3.41 | <3.41 |
| IL-12p40 | 35.76 ± 6.05 | 41.58 ± 7.09 | <1.39 | <1.39 | <1.39 | <1.39 |
| MDC (CCL22) | 391.78 ± 70.17 | 558.93 ± 70.78 | <13.47 | <13.47 | <13.47 | <13.47 |
| IL-12p70 | 2.33 ± 0.74 | 5.73 ± 2.34 | <0.17 | 0.24 ± 0.16 | <0.17 | 0.31 ± 0.15 |
| PDGF-AA | 144.38 ± 25.07 | 133.34 ± 20.2 | 10.68 ± 0.54 | 11 ± 1.15 | 8.53 ± 0.8 | 10.36 ± 1.56 |
| IL-15 | <1.03 | 1.44 ± 0.39 | <1.03 | <1.03 | <1.03 | <1.03 |
| sCD40L | 8.5 ± 3.82 | 6.21 ± 2.03 | 0.25 ± 0.19 | 0.57 ± 0.3 | <LLOQ * | <LLOQ * |
| IL-1Ra | 212.07 ± 56.48 | 228.47 ± 29.57 | <0.85 | <0.85 | <0.85 | <0.85 |
| IL-1a | 3541.85 ± 426.81 | 3755.48 ± 437.57 | <3.2 | <3.2 | <3.2 | <3.2 |
| IL-9 | 1.07 ± 0.22 | 1.93 ± 1.37 | <0.05 | <0.05 | <0.05 | <0.05 |
| IL-1b | 2510.15 ± 254.06 | 2913.38 ± 120.82 | 4.09 ± 0.71 | 4.9 ± 2.1 | 11 ± 1.36 | 8.33 ± 1.15 |
| IL-4 | 124.01 ± 8.04 | 124.97 ± 5.77 | <3.2 | 9.05 ± 2.13 | <3.2 | 6.7 ± 3.34 |
| IL-5 | 0.18 ± 0.06 | 0.45 ± 0.58 | <LLOQ* | 0.06 ± 0.01 | 0.02 ± 0.01 | 0.04 ± 0.02 |
| IL-6 | >7819.31 | >7819.31 | 6.68 ± 3.3 | 237.66 ± 36.78 | 9.32 ± 3.63 | 359.11 ± 0.39 |
| IL-7 | 55.8 ± 5.61 | 45.04 ± 17.6 | <2.1 | 4.91 ± 1.1 | <2.1 | 8.19 ± 0.43 |
| IL-8 | 21222.36 ± 9057.91 | >30603.7 | 25.82 ± 7.25 | 440.74 ± 86.82 | 47.28 ± 26.46 | 601.86 ± 23.44 |
| IP10 (CXCL10) | 51.66 ± 4.82 | 65.36 ± 10.39 | 4.08 ± 2.52 | 9.9 ± 1.2 | 2.67 ± 1.52 | 35.78 ± 7.56 |
| MCP-1 (CCL2) | 5640.54 ± 109.79 | 6263.61 ± 418.96 | 6.83 ± 2.55 | 52.27 ± 4.74 | <LLOQ* | 148.64 ± 13.17 |
| MIP-1a (CCL3) | >9996.8 | >9996.8 | 60.3 ± 12.85 | 60.72 ± 8.41 | 95.97 ± 20.97 | 81.65 ± 25.96 |
| MIP-1b (CCL4) | 7617.27 ± 1114.36 | 8438.14 ± 935.11 | 12.54 ± 3.65 | 12.07 ± 2.93 | 69.52 ± 0.22 | 61.76 ± 29.48 |
| RANTES (CCL5) | >12068.63 | >12068.63 | 152.43 ± 17.56 | 166.12 ± 18.63 | 131.65 ± 54.86 | 130.21 ± 27.08 |
| TNFa | 1825.11 ± 231.14 | 2237.44 ± 324.68 | 10.3 ± 3.97 | 11.12 ± 0.66 | 63.69 ± 10.27 | 55.52 ± 17.18 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gomzikova, M.O.; Kletukhina, S.K.; Kurbangaleeva, S.V.; Neustroeva, O.A.; Vasileva, O.S.; Garanina, E.E.; Khaiboullina, S.F.; Rizvanov, A.A. Mesenchymal Stem Cell Derived Biocompatible Membrane Vesicles Demonstrate Immunomodulatory Activity Inhibiting Activation and Proliferation of Human Mononuclear Cells. Pharmaceutics 2020, 12, 577. https://doi.org/10.3390/pharmaceutics12060577
Gomzikova MO, Kletukhina SK, Kurbangaleeva SV, Neustroeva OA, Vasileva OS, Garanina EE, Khaiboullina SF, Rizvanov AA. Mesenchymal Stem Cell Derived Biocompatible Membrane Vesicles Demonstrate Immunomodulatory Activity Inhibiting Activation and Proliferation of Human Mononuclear Cells. Pharmaceutics. 2020; 12(6):577. https://doi.org/10.3390/pharmaceutics12060577
Chicago/Turabian StyleGomzikova, Marina O., Sevindzh K. Kletukhina, Sirina V. Kurbangaleeva, Olga A. Neustroeva, Olga S. Vasileva, Ekaterina E. Garanina, Svetlana F. Khaiboullina, and Albert A. Rizvanov. 2020. "Mesenchymal Stem Cell Derived Biocompatible Membrane Vesicles Demonstrate Immunomodulatory Activity Inhibiting Activation and Proliferation of Human Mononuclear Cells" Pharmaceutics 12, no. 6: 577. https://doi.org/10.3390/pharmaceutics12060577
APA StyleGomzikova, M. O., Kletukhina, S. K., Kurbangaleeva, S. V., Neustroeva, O. A., Vasileva, O. S., Garanina, E. E., Khaiboullina, S. F., & Rizvanov, A. A. (2020). Mesenchymal Stem Cell Derived Biocompatible Membrane Vesicles Demonstrate Immunomodulatory Activity Inhibiting Activation and Proliferation of Human Mononuclear Cells. Pharmaceutics, 12(6), 577. https://doi.org/10.3390/pharmaceutics12060577