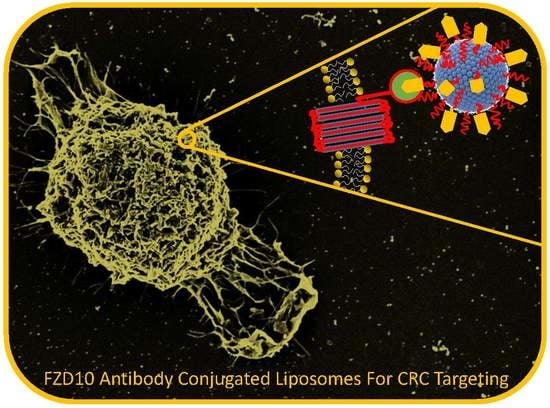
Effectiveness of a Controlled 5-FU Delivery Based on FZD10 Antibody-Conjugated Liposomes in Colorectal Cancer In vitro Models
Abstract
:1. Introduction
2. Material and Methods
2.1. Preparation of Liposomes
2.2. Evaluation of Encapsulation Efficiency (EE%)
2.3. In vitro Drug Release Study
2.4. Cell Culture
2.5. Cells Proliferation Assay
2.6. In vitro Investigation by Field Emission Scanning Electron Microscopy
2.7. In vitro Scratch Assay
2.8. Immunofluorescence Analysis
2.9. Dynamic Light Scattering Analysis and ζ-Potential Investigation
2.10. Morphological Characterization by Transmission Electron Microscopy (TEM)
2.11. Statistical Analysis
3. Results
3.1. Liposomes Formulation and Characterization
3.2. Effectiveness of Formulated Liposomes on Cell Viability
3.3. Effects of Formulated Liposomes on the Cell Morphology
3.4. Effectiveness of the Formulated Liposomes on Cell Migration
3.5. Effectiveness of Formulated LPs on Vimentin and Phospho-Paxillin Cytoskeletal Proteins
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Global Burden of Disease Cancer Collaboration; Fitzmaurice, C.; Allen, C.; Barber, R.M.; Barregard, L.; Bhutta, Z.A.; Brenner, H.; Dicker, D.J.; Chimed-Orchir, O.; Dandona, R.; et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability adjusted life-years for 32 cancer groups, 1990 to 2015. JAMA Oncol. 2017, 3, 524–548. [Google Scholar] [PubMed]
- Arias, J.L. Novel strategies to improve the anticancer action of 5-fluorouracil by using drug delivery systems. Molecules 2008, 13, 2340–2369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, N.; Yin, Y.; Xu, S.J.; Chen, W.S. 5-Fluorouracil: Mechanisms of resistance and reversal strategies. Molecules 2008, 13, 1551–1569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larsson, P.A.; Carlsson, G.; Gustavsson, B.; Graf, W.; Glimelius, B. Different intravenous administration techniques for 5-fluorouracil. Pharmacokinetics and pharmacodynamic effects. Acta. Oncol. 1996, 35, 207–212. [Google Scholar] [CrossRef]
- Davis, M.E.; Chen, Z.G.; Shin, D.M. Nanoparticle therapeutics: An emerging treatment modality for cancer. Nat. Rev. Drug Discov. 2008, 7, 771–782. [Google Scholar] [CrossRef]
- Gentile, E.; Cilurzo, F.; Di Marzio, L.; Carafa, M.; Ventura, C.A.; Wolfram, J.; Paolino, D.; Celia, C. Liposomal chemotherapeutics. Future Oncol. 2013, 9, 1849–1859. [Google Scholar] [CrossRef]
- Gupta, A.S.; Kshirsagar, S.J.; Bhalekar, M.R.; Saldanha, T. Design and development of liposomes for colon targeted drug delivery. J. Drug Target. 2013, 21, 146–160. [Google Scholar] [CrossRef] [PubMed]
- Barea, M.J.; Jenkins, M.J.; Gaber, M.H.; Bridson, R.H. Evaluation of liposomes coated with a pH responsive polymer. Int. J. Pharm. 2010, 402, 89–94. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Zhu, C. Mechanism of hepatic targeting via oral administration of DSPE-PEG-cholic acid-modified nanoliposomes. Int. J. Nanomedicine 2017, 12, 1673–1684. [Google Scholar] [CrossRef] [Green Version]
- Janeczek, A.A.; Scarpa, E.; Horrocks, M.H.; Tare, R.S.; Rowland, C.A.; Jenner, D.; Newman, T.A.; Oreffo, R.O.; Lee, S.F.; Evans, N.D. PEGylated liposomes associate with Wnt3A protein and expand putative stem cells in human bone marrow populations. Nanomedicine 2017, 12, 845–863. [Google Scholar] [CrossRef] [Green Version]
- Handali, S.; Moghimipour, E.; Rezaei, M.; Ramezani, Z.; Kouchak, M.; Amini, M.; Ahmadi, K.; Sadegh, A.; Farid, S.; Dorkoosh, A. A novel 5-Fluorouracil targeted delivery to colon cancer using folic acid conjugated liposomes. Biomed. Pharmacother. 2018, 108, 1259–1273. [Google Scholar] [CrossRef] [PubMed]
- Hua, S. Orally administered liposomal formulations for colon targeted drug delivered. Front. Pharmacol. 2014, 5, 138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, L.; Fan, Z.; Jun, N.; Benjia, L.; Zequn, L.; Xilong, W.; Zhongming, J.; Yong, H.; Xiaohong, W.; Kai, C.; et al. Tumor specific delivery and therapy mediate by integrin β6-target immunoliposomes for β6-siRNA in colon carcinoma. Oncotarget 2016, 7, 85163–85175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alavizadeh, S.H.; Soltani, F.; Ramezani, M. Recent advances in immunoliposome-based cancer therapy. Curr. Pharmacol. Rep. 2016, 2, 129–141. [Google Scholar] [CrossRef] [Green Version]
- Wong, S.C.C.; He, C.W.; Chan, C.M.L.; Chan, A.K.C.; Wong, H.T.; Cheung, M.T.; Luk, L.L.Y.; Au, T.C.C.; Chiu, M.K.; Ma, B.B.T.; et al. Clinical significance of frizzled homolog 3 protein in colorectal cancer patients. PLoS ONE 2013, 8, e79481. [Google Scholar] [CrossRef] [Green Version]
- Ueno, K.; Hiura, M.; Suehiro, Y.; Hazama, S.; Hirata, H.; Oka, M.; Imai, K.; Dahiya, R.; Hinoda, Y. Frizzled-7 as a potential therapeutic target in colorectal cancer. Neoplasia 2008, 10, 697–705. [Google Scholar] [CrossRef] [Green Version]
- Zeng, C.M.; Chen, Z.; Fu, L. Frizzled receptors as potential therapeutic targets in human cancers. Int. J. Mol. Sci. 2018, 19, 1543. [Google Scholar] [CrossRef] [Green Version]
- Scavo, M.P.; Depalo, N.; Rizzi, F.; Ingrosso, C.; Fanizza, E.; Chieti, A.; Messa, C.; Denora, N.; Laquintana, V.; Striccoli, M.; et al. FZD10 carried by exosomes sustains cancer cell proliferation. Cells 2019, 8, 777. [Google Scholar] [CrossRef] [Green Version]
- Scavo, M.P.; Cigliano, A.; Depalo, N.; Fanizza, E.; Bianco, M.G.; Denora, N.; Laquintana, V.; Curri, M.L.; Lorusso, D.; Lotesoriere, C.; et al. Frizzled-10 extracellular vesicles plasma concentration are associated with tumoral progression in patients with colorectal and gastric cancer. Int. J. Oncol. 2019. [Google Scholar] [CrossRef] [Green Version]
- Scavo, M.P.; Depalo, N.; Tutino, V.; De Nunzio, V.; Ingrosso, C.; Rizzi, F.; Notarnicola, M.; Curri, M.L.; Giannelli, G. Exosomes for diagnosis and therapy in gastrointestinal cancers. Int. J. Mol. Sci. 2020, 21, 367. [Google Scholar] [CrossRef] [Green Version]
- Nagayama, S.; Yamada, E.; Kohno, Y.; Aoyama, T.; Fukukawa, C.; Kubo, H.; Watanabe, G.; Katagiri, T.; Nakamura, Y.; Sakai, Y.; et al. Inverse correlation of the up-regulation of FZD10 expression and the activation of beta-catenin in synchronous colorectal tumors. Cancer Sci. 2009, 100, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Nagayama, S.; Fukukawa, C.; Katagiri, T.; Okamoto, T.; Aoyama, T.; Oyaizu, N.; Imamura, M.; Toguchida, J.; Nakamura, Y. Therapeutic potential of antibodies against FZD10, a cell-surface protein; for synovial sarcomas. Oncogene 2005, 24, 6201–6212. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scavo, M.P.; Fucci, L.; Caldarola, L.; Mangia, A.; Azzariti, A.; Simone, G.; Gasparini, G.; Krol, S. Frizzled-10 and cancer progression. Is it a new prognostic marker? Oncotarget 2017, 9, 824–830. [Google Scholar] [PubMed]
- Depalo, N.; Fanizza, E.; Vischio, F.; Denora, N.; Laquintana, V.; Cutrignelli, A.; Striccoli, M.; Giannelli, G.; Agostiano, A.; Curri, M.L.; et al. Imaging modification of colon carcinoma cells exposed to lipid based nanovectors for drug delivery: A scanning electron microscopy investigation. RSC Adv. 2019, 9, 21810. [Google Scholar] [CrossRef] [Green Version]
- Liang, C.C.; Park, A.Y.; Guan, J.L. In a vitro scratch assay: A convenient and inexpensive method for analysis of cell migration in vitro. Nature Protocols. 2007, 2, 329–333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tutino, V.; Gigante, I.; Scavo, M.P.; Refolo, M.G.; De Nunzio, V.; Milella, R.A.; Caruso, M.G.; Notarnicola, M. Stearoyl-CoA Desaturase-1 Enzyme inhibition by grape skin extracts affects membrane fluidity in human colon cancer cell lines. Nutrients 2020, 12, 683. [Google Scholar] [CrossRef] [Green Version]
- Ojima, E.; Inoue, Y.; Watanabe, H.; Hiro, J.; Toiyama, Y.; Miki, C.; Kusunoki, M. The optimal schedule for 5-fluorouracil radiosensitization in colon cancer cell lines. Oncolo. Rep. 2006, 16, 1085. [Google Scholar] [CrossRef]
- Dushinsky, R.; Pleven, E.; Heidelberger, C. The synthesis of 5-fluoropyrimidines. J. Am. Chem. Soc. 1957, 79, 4559–4560. [Google Scholar] [CrossRef]
- Durak, I.; Karaayvaz, M.; Kavutcu, M.; Cimen, M.Y.; Kaçmaz, M.; Büyükkoçak, S.; Oztürk, H.S.J. Reduced antioxidant defense capacity in myocardial tissue from guinea pigs treated with 5-fluorouracil. J. Toxicol. Environ. Health. 2000, 59, 585–589. [Google Scholar]
- Tsibiribi, P.; Bui-Xuan, C.; Bui-Xuan, B.; Lombard-Bohas, C.; Duperret, S.; Belkhiria, M.; Tabib, A.; Maujean, G.; Descotes, J.; Timour, Q. Cardiac lesions induced by 5-fluorouracil in the rabbit. Hum. Exp. Toxicol. 2006, 25, 305–309. [Google Scholar] [CrossRef]
- Brower, V. Cardiotoxicity debated for anthracyclines and trastuzumab in breast cancer. J. Natl. Cancer Inst. 2013, 105, 835–836. [Google Scholar] [CrossRef] [Green Version]
- Grover, S.; Leong, D.P.; Chakrabarty, A.; Joerg, L.; Kotasek, D.; Cheong, K.; Joshi, R.; Joseph, M.X.; De Pasquale, C.; Koczwara, B.; et al. Left and right ventricular effects of anthracycline and trastuzumab chemotherapy: A prospective study using novel cardiac imaging and biochemical markers. Int. J. Cardiol. 2013, 168, 5465–5467. [Google Scholar] [CrossRef]
- Cardinale, D.; Bacchiani, G.; Beggiato, M.; Colombo, A.; Cipolla, C.M. Strategies to prevent and treat cardiovascular risk in cancer patients. Semin. Oncol. 2013, 40, 186–198. [Google Scholar] [CrossRef]
- Lee, S.H.; Bajracharya, R.; Min, J.Y.; Han, J.W.; Park, B.J.; Han, H.K. Strategic approaches for colon targeted drug delivery: An overview of recent advancements. Pharmaceutics 2020, 12, 68. [Google Scholar] [CrossRef] [Green Version]
- Tiwari, A.; Saraf, S.; Jain, A.; Panda, P.K.; Verma, A.; Jain, S.K. Basics to Advances in Nanotherapy of colorectal cancer. Drug Deliv. Transl. Res. 2020, 10, 319–338. [Google Scholar] [CrossRef]
- Le, V.M.; Nho, T.D.T.; Ly, H.T.; Vo, T.S.; Nguyen, H.D.; Phung, T.T.H.; Zou, A.; Liu, J. Enhanced anticancer efficacy and tumor targeting through folate-PEG modified nanoliposome loaded with 5-fluorouracil. Adv. Nat. Sci. Nanosci. Nanotechnol. 2017, 8. [Google Scholar] [CrossRef]
- Liang, B.; Shahbaz, M.; Wang, Y.; Gao, H.; Fang, R.; Niu, Z.; Liu, S.; Wang, B.; Sun, Q.; Niu, W.; et al. Integrinβ6-targeted immunoliposomes mediate tumor-specific drug delivery and enhance therapeutic efficacy in colon carcinoma. Clin. Cancer Res. 2015, 21, 1183–1195. [Google Scholar] [CrossRef] [Green Version]
- Udofot, O.; Affram, K.; Israel, B.; Agyare, E. Cytotoxicity of 5-fluorouracil-loaded pH-sensitive liposomal nanoparticles in colorectal cancer cell lines. Integr. Cancer Sci. Ther. 2015, 2, 245–252. [Google Scholar] [CrossRef] [Green Version]
- Lopalco, A.; Cutrignelli, A.; Denora, N.; Lopedota, A.; Franco, M.; Laquintana, V. Transferrin functionalized liposomes loading dopamine HCl: Development and permeability studies across an in vitro model of human blood-brain barrier. Nanomaterials 2018, 8, 178. [Google Scholar] [CrossRef] [Green Version]
- Maruyama, K. Intracellular targeting delivery of liposomal drugs to solid tumors based on EPR effects. Adv. Drug Delivery Rev. 2011, 63, 161–169. [Google Scholar] [CrossRef]
- Kjellström, J.; Kjellén, E.; Johnsson, A. In vitro radiosensitization by oxaliplatin and 5-fluorouracil in a human colon cancer cell line. Acta Oncol. 2005, 44, 687–693. [Google Scholar] [CrossRef] [PubMed]
- Beumer, J.H.; Boisdron-Celle, M.; Clarke, W.; Courtney, J.B.; Egorin, M.J.; Gamelin, E.; Harney, R.L.; Hammett-Stabler, C.; Lepp, S.; Li, Y.; et al. Multicenter evaluation of a novel nanoparticle immunoassay for 5-fluorouracil on the olympus au400 analyzer. Ther. Drug Monit. 2009, 31, 688–694. [Google Scholar] [CrossRef] [PubMed]
- Gamelin, E.; Delva, R.; Jacob, J.; Merrouche, Y.; Raoul, J.L.; Pezet, D.; Dorval, E.; Piot, G.; Morel, A.; Boisdron-Celle, M. Individual fluorouracil dose adjustment based on pharmacokinetic follow-up compared with conventional dosage: Results of a multicenter randomized trial of patients with metastatic colorectal cancer. J. Clin. Oncol. 2008, 26, 2099–2105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- López-Colomé, A.M.; Lee-Rivera, I.; Benavides-Hidalgo, R. Paxillin: A crossroad in pathological cell migration. J. Hematol. Oncol. 2017, 10, 50. [Google Scholar] [CrossRef] [Green Version]
- Danielsson, F.; Peterson, M.K.; Araújo, H.C.; Lautenschläger, F.; Gad, A.K.B. Vimentin diversity in health and disease. Cells 2018, 7, 147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, D.W.; Huang, C.C.; Chang, S.W.; Chen, T.H.; Lee, H. Bcl-2 stabilization by paxillin confers 5-fluorouracil resistance in colorectal cancer. Cell Death Differ. 2015, 22, 779–789. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lazarova, D.L.; Bordonaro, M. Vimentin, colon cancer progression and resistance to butyrate and other HDACis. J. Cell. Mol. Med. 2016, 20, 989. [Google Scholar] [CrossRef]
- Huang, C.C.; Wu, D.W.; Lin, P.L.; Lee, H. Paxillin promotes colorectal tumor invasion and poor patient outcomes via ERK-mediated stabilization of Bcl-2 protein by phosphorylation at Serine 87. Oncotarget 2015, 6, 8698. [Google Scholar] [CrossRef]
- Zhao, C.J.; Du, S.; Dang, X.; Gong, M. Expression of paxillin is correlated with clinical prognosis in colorectal cancer patients. Med. Sci. Monit. 2015, 21, 1989. [Google Scholar] [PubMed] [Green Version]
- Nosova, A.S.; Koloskova, O.O.; Nikonova, A.A.; Simonova, S.A.; Smirnov, V.V.; Kudlay, D.; Khaito, M.R. Diversity of PEGylation methods of liposomes and their influence on RNA delivery. MedChemComm 2019, 10, 369–377. [Google Scholar] [CrossRef]
- Thomas, A.M.; Kapanen, A.I.; Hare, J.I.; Ramsay, E.; Edwards, K.; Karlsson, G.; Bally, M.B. Development of a liposomal nanoparticle formulation of 5-fluorouracil for parenteral administration: Formulation design, pharmacokinetics and efficacy. J. Control. Release. 2011, 150, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Satelli, A.; Li, S. Vimentin in cancer and its potential as a molecular target for cancer therapy. Cell Mol. Life Sci. 2011, 68, 3033–3046. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, C.Y.; Lin, H.H.; Tang, M.J.; Wang, Y.K. Vimentin contributes to epithelial-mesenchymal transition cancer cell mechanics by mediating cytoskeletal organization and focal adhesion maturation. Oncotarget 2015, 6, 15966–15983. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Downey, C.; Craig, D.H.; Basson, M.D. Pressure activates colon cancer cell adhesion via paxillin phosphorylation, Crk, Cas, and Rac1. Cell Mol. Life Sci. 2008, 65, 1446–1457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maki, K.C.; Lawless, A.L.; Reeves, M.S.; Kelley, K.M.; Dicklin, M.R.; Jenks, B.H.; Shneyvas, E.; Brooks, J.R. Lipid effects of a dietary supplement softgel capsule containing plant sterols/stanols in primary hypercholesterolemia. Nutrition 2013, 29, 96–100. [Google Scholar] [CrossRef] [Green Version]







| Samples | Dh (nm) | PDI | ζ-Potential (mV) | Drug EE (%) |
|---|---|---|---|---|
| 5-FU/LPs | 155 ± 47 | 0.32 ± 0.05 | −37.73 ± 5.38 | 65.9 ± 2.9 |
| Anti-FZD10/5FU/LPs | 193 ± 12 | 0.33 ± 0.15 | −43.43 ± 4.75 | 45.7 ± 5.9 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scavo, M.P.; Cutrignelli, A.; Depalo, N.; Fanizza, E.; Laquintana, V.; Gasparini, G.; Giannelli, G.; Denora, N. Effectiveness of a Controlled 5-FU Delivery Based on FZD10 Antibody-Conjugated Liposomes in Colorectal Cancer In vitro Models. Pharmaceutics 2020, 12, 650. https://doi.org/10.3390/pharmaceutics12070650
Scavo MP, Cutrignelli A, Depalo N, Fanizza E, Laquintana V, Gasparini G, Giannelli G, Denora N. Effectiveness of a Controlled 5-FU Delivery Based on FZD10 Antibody-Conjugated Liposomes in Colorectal Cancer In vitro Models. Pharmaceutics. 2020; 12(7):650. https://doi.org/10.3390/pharmaceutics12070650
Chicago/Turabian StyleScavo, Maria Principia, Annalisa Cutrignelli, Nicoletta Depalo, Elisabetta Fanizza, Valentino Laquintana, Giampietro Gasparini, Gianluigi Giannelli, and Nunzio Denora. 2020. "Effectiveness of a Controlled 5-FU Delivery Based on FZD10 Antibody-Conjugated Liposomes in Colorectal Cancer In vitro Models" Pharmaceutics 12, no. 7: 650. https://doi.org/10.3390/pharmaceutics12070650
APA StyleScavo, M. P., Cutrignelli, A., Depalo, N., Fanizza, E., Laquintana, V., Gasparini, G., Giannelli, G., & Denora, N. (2020). Effectiveness of a Controlled 5-FU Delivery Based on FZD10 Antibody-Conjugated Liposomes in Colorectal Cancer In vitro Models. Pharmaceutics, 12(7), 650. https://doi.org/10.3390/pharmaceutics12070650