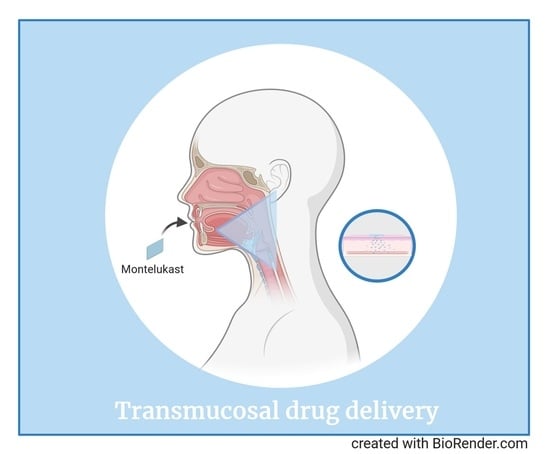
Improved Bioavailability of Montelukast through a Novel Oral Mucoadhesive Film in Humans and Mice
Abstract
:1. Introduction
2. Materials and Methods
2.1. Film Preparation
2.2. In Vitro Dissolution Test
2.3. Mechanical Properties
2.4. Clinical Study—Subjects and Study Design
2.5. Animals
2.6. Quantitative Assessment of MTK in Plasma and CSF Human Samples
2.7. Quantitative Assessment of MTK in Serum and CSF Mouse Samples (HPLC-MS/MS)
2.8. Statistical Analysis
3. Results
3.1. Composition, Preparation, Physical and Mechanical Properties of the MTK Mucoadhesive Film
3.2. Dissolution
3.3. Improved MTK Bioavailability in Human Plasma and CSF in MTK Mucoadhesive Film
3.4. Clinical Safety
3.5. Pharmacoexposure and Kinetics of MTK in WT and in 5xFAD Mice
3.6. Safety and General Health in Mice
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ciana, P.; Fumagalli, M.; Trincavelli, M.L.; Verderio, C.; Rosa, P.; Lecca, D.; Guerrini, U. The orphan receptor GPR17 identified as a new dual uracil nucleotides/cysteinyl-leukotrienes receptor. EMBO J. 2006, 25, 4615–4627. [Google Scholar] [CrossRef] [PubMed]
- Nayak, A. A review of montelukast in the treatment of asthma and allergic rhinitis. Expert Opin. Pharmacother. 2004, 5, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Reiss, T.F.; Chervinsky, P.; Dockhorn, R.J.; Shingo, S.; Seidenberg, B.; Edwards, T.B. Montelukast, a once-daily leukotriene receptor antagonist, in the treatment of chronic asthma: A multicenter, randomized, double-blind trial. Montelukast Clinical Research Study Group. Arch. Intern. Med. 1998, 158, 1213–1220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okumu, A.; Dimaso, M.; Löbenberg, R. Dynamic Dissolution Testing To Establish In Vitro/In Vivo Correlations for Montelukast Sodium, a Poorly Soluble Drug. Pharm. Res. 2008, 25, 2778–2785. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.D.; Capra, V.; Clunes, M.T.; Rovati, G.E.; Staňková, J.; Maj, M.; Duffy, D.L. Cysteinyl Leukotrienes Pathway Genes, Atopic Asthma and Drug Response: From Population Isolates to Large Genome-Wide Association Studies. Front. Pharm. 2016, 7, 299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noonan, M.J.; Chervinsky, P.; Brandon, M.; Zhang, J.; Kundu, S.; McBurney, J.; Reiss, T.F. Montelukast, a potent leukotriene receptor antagonist, causes dose-related improvements in chronic asthma. Montelukast Asthma Study Group. Eur. Respir. J. 1998, 11, 1232–1239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mougey, E.B.; Feng, H.; Castro, M.; Irvin, C.G.; Lima, J.J. Absorption of montelukast is transporter mediated: A common variant of OATP2B1 is associated with reduced plasma concentrations and poor response. Pharm. Genom. 2009, 19, 129–138. [Google Scholar] [CrossRef] [Green Version]
- Mougey, E.B.; Lang, J.E.; Wen, X.; Lima, J.J. Effect of Citrus Juice and SLCO2B1 Genotype on the Pharmacokinetics of Montelukast. J. Clin. Pharm. 2011, 51, 751–760. [Google Scholar] [CrossRef]
- Barbosa, J.S.; Paz, F.A.A.; Braga, S.S. Montelukast medicines of today and tomorrow: From molecular pharmaceutics to technological formulations. Drug Deliv. 2016, 23, 3257–3265. [Google Scholar] [CrossRef] [Green Version]
- Michael, J.; Marschallinger, J.; Aigner, L. The leukotriene signaling pathway: A druggable target in Alzheimer’s disease. Drug Discov. Today 2019, 24, 505–516. [Google Scholar] [CrossRef]
- Ikonomovic, M.D.; Abrahamson, E.E.; Uz, T.; Manev, H.; DeKosky, S.T. Increased 5-Lipoxygenase Immunoreactivity in the Hippocampus of Patients With Alzheimer’s Disease. J. Histochem. Cytochem. 2008, 56, 1065–1073. [Google Scholar] [CrossRef] [PubMed]
- Michael, J.; Unger, M.S.; Poupardin, R.; Schernthaner, P.; Mrowetz, H.; Attems, J.; Aigner, L. Microglia depletion diminishes key elements of the leukotriene pathway in the brain of Alzheimer’s Disease mice. Acta Neuropathol. Commun. 2020, 8, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Grinde, B.; Schirmer, H.; Eggen, A.E.; Aigner, L.; Engdahl, B. A possible effect of montelukast on neurological aging examined by the use of register data. Int. J. Clin. Pharm. 2020, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Grinde, B.; Engdahl, B. Prescription database analyses indicates that the asthma medicine montelukast might protect against dementia: A hypothesis to be verified. Immun. Ageing 2017, 14, 1–7. [Google Scholar] [CrossRef]
- Rozin, S.I. Case Series Using Montelukast in Patients with Memory Loss and Dementia. Open Neurol. J. 2017, 11, 7–10. [Google Scholar] [CrossRef]
- Shaikh, R.; Singh, T.R.R.; Garland, M.J.; Woolfson, A.D.; Donnelly, R.F. Mucoadhesive drug delivery systems. J. Pharm. Bioal. Sci. 2011, 3, 89. [Google Scholar]
- Shinkar, D.M.; Dhake, A.S.; Setty, C.M. Drug Delivery from the Oral Cavity: A Focus on Mucoadhesive Buccal Drug Delivery Systems. Pda J. Pharm. Sci. Technol. 2012, 66, 466–500. [Google Scholar] [CrossRef]
- Silva, B.M.; Borges, A.F.; Silva, C.; Coelho, J.F.; Simões, S. Mucoadhesive oral films: The potential for unmet needs. Int. J. Pharm. 2015, 494, 537–551. [Google Scholar] [CrossRef]
- Oakley, H.; Cole, S.L.; Logan, S.; Maus, E.; Shao, P.; Craft, J.; Guillozet-Bongaarts, A.; Ohno, M.; Disterhoft, J.; Van Eldik, L.; et al. Intraneuronal beta-Amyloid Aggregates, Neurodegeneration, and Neuron Loss in Transgenic Mice with Five Familial Alzheimer’s Disease Mutations: Potential Factors in Amyloid Plaque Formation. J. Neurosci. 2006, 26, 10129–10140. [Google Scholar] [CrossRef]
- Marschallinger, J.; Schäffner, I.; Klein, B.P.; Gelfert, R.; Rivera, F.J.; Illes, S.; Grassner, L.; Janssen, M.; Rotheneichner, P.; Schmuckermair, C.; et al. Structural and functional rejuvenation of the aged brain by an approved anti-asthmatic drug. Nat. Commun. 2015, 6, 8466. [Google Scholar] [CrossRef] [Green Version]
- Muppavarapu, R.; Guttikar, S.; Rajappan, M.; Kamarajan, K.; Mullangi, R. Sensitive LC-MS/MS-ESI method for simultaneous determination of montelukast and fexofenadine in human plasma: Application to a bioequivalence study. Biomed. Chromatogr. 2014, 28, 1048–1056. [Google Scholar] [CrossRef] [PubMed]
- Challa, B.; Awen, B.Z.; Chandu, B.R.; Khagga, M.; Kotthapalli, C.B. Method Development and Validation of Montelukast in Human Plasma by HPLC Coupled with ESI-MS/MS: Application to a Bioequivalence Study. Sci. Pharm. 2010, 78, 411–422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gelosa, P.; Colazzo, F.; Tremoli, E.; Sironi, L.; Castiglioni, L. Cysteinyl Leukotrienes as Potential Pharmacological Targets for Cerebral Diseases. Mediat. Inflamm. 2017, 2017, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, A.; Chen, F.; Thakur, A.; Hong, H. Cysteinyl Leukotrienes and Their Receptors: Emerging Therapeutic Targets in Central Nervous System Disorders. CNS Neurosci. 2016, 22, 943–951. [Google Scholar] [CrossRef] [PubMed]
- Lynch, K.R.; O’Neill, G.P.; Liu, Q.; Im, D.-S.; Sawyer, N.; Metters, K.M.; Coulombe, N.; Abramovitz, M.; Figueroa, D.J.; Zeng, Z.; et al. Characterization of the human cysteinyl leukotriene CysLT1 receptor. Nature 1999, 399, 789–793. [Google Scholar] [CrossRef] [PubMed]
- Storms, W.; Michele, T.M.; Knorr, B.; Noonan, G.; Shapiro, G.; Zhang, J.; Shingo, S.; Reiss, T.F. Clinical safety and tolerability of montelukast, a leukotriene receptor antagonist, in controlled clinical trials in patients aged > or = 6 years. Clin. Exp. Allergy 2001, 31, 77–87. [Google Scholar] [CrossRef]
- Calapai, G.; Casciaro, M.; Miroddi, M.; Calapai, F.; Navarra, M.; Gangemi, S. Montelukast-Induced Adverse Drug Reactions: A Review of Case Reports in the Literature. Pharmacology 2014, 94, 60–70. [Google Scholar] [CrossRef]
- Cereza, G.; Doladé, N.G.; Laporte, J.-R. Nightmares induced by montelukast in children and adults. Eur. Respir. J. 2012, 40, 1574–1575. [Google Scholar] [CrossRef] [Green Version]
- Haarman, M.G.; Van Hunsel, F.; De Vries, T.W. Adverse drug reactions of montelukast in children and adults. Pharm. Res. Perspect. 2017, 5, e00341. [Google Scholar] [CrossRef]
- Chu, J.; Li, J.G.; Praticò, D. Zileuton Improves Memory Deficits, Amyloid and Tau Pathology in a Mouse Model of Alzheimer’s Disease with Plaques and Tangles. PLoS ONE 2013, 8, e70991. [Google Scholar] [CrossRef] [Green Version]
- Chu, J.; Pratico, D. Pharmacologic blockade of 5-lipoxygenase improves the amyloidotic phenotype of an Alzheimer’s disease transgenic mouse model involvement of gamma-secretase. Am. J. Pathol. 2011, 178, 1762–1769. [Google Scholar] [CrossRef] [PubMed]
- Giannopoulos, P.F.; Chu, J.; Joshi, Y.B.; Sperow, M.; Li, J.G.; Kirby, L.G.; Praticò, D. 5-lipoxygenase activating protein reduction ameliorates cognitive deficit, synaptic dysfunction, and neuropathology in a mouse model of Alzheimer’s disease. Biol. Psychiatry 2013, 74, 348–356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Meco, A.; Lauretti, E.; Vagnozzi, A.N.; Praticò, D. Zileuton restores memory impairments and reverses amyloid and tau pathology in aged Alzheimer’s disease mice. Neurobiol. Aging 2014, 35, 2458–2464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giannopoulos, P.F.; Chiu, J.; Praticò, D. Learning Impairments, Memory Deficits, and Neuropathology in Aged Tau Transgenic Mice Are Dependent on Leukotrienes Biosynthesis: Role of the cdk5 Kinase Pathway. Mol. Neurobiol. 2018, 56, 1211–1220. [Google Scholar] [CrossRef]
- Gelosa, P.; Bonfanti, E.; Castiglioni, L.; Delgado-Garcia, J.M.; Gruart, A.; Fontana, L.; Gotti, M.; Tremoli, E.; Lecca, D.; Fumagalli, M.; et al. Improvement of fiber connectivity and functional recovery after stroke by montelukast, an available and safe anti-asthmatic drug. Pharm. Res. 2019, 142, 223–236. [Google Scholar] [CrossRef]
- Fleck, J.; Marafiga, J.R.; Jesse, A.C.; Ribeiro, L.R.; Rambo, L.M.; Mello, C.F. Montelukast potentiates the anticonvulsant effect of phenobarbital in mice: An isobolographic analysis. Pharm. Res. 2015, 94, 34–41. [Google Scholar] [CrossRef]
- Cevik, B.; Solmaz, V.; Aksoy, D.; Erbas, O. Montelukast Inhibits Pentylenetetrazol-Induced Seizures in Rats. Med. Sci. Monit. 2015, 21, 869–874. [Google Scholar] [CrossRef] [Green Version]
- Marschallinger, J.; Altendorfer, B.; Rockenstein, E.; Holztrattner, M.; Garnweidner-Raith, J.; Pillichshammer, N.; Leister, I.; Hutter-Paier, B.; Strempfl, K.; Unger, M.S.; et al. The Leukotriene Receptor Antagonist Montelukast Reduces Alpha-Synuclein Load and Restores Memory in an Animal Model of Dementia with Lewy Bodies. Neurotherapeutics 2020, 17, 1061–1074. [Google Scholar] [CrossRef] [Green Version]





| Excipient | Function | Composition (%w/w Wet) |
|---|---|---|
| Water | Solvent | 60.0–85.0 |
| Mucoadhesive Polymer | Film forming polymer | 5.0–15.0 |
| Gum | Viscosity modifier | 0.50–3.00 |
| Stabilizers | Degradation prevention | 0.01–0.05 |
| Colorant/Flavor | Patient compliance | 0.10–1.00 |
| Plasticizers | Tune mechanical properties | 0.10–4.00 |
| Permeation Enhancer | Increase oral absorption | 0.10–2.00 |
| API * | Therapeutic | 0–30.00 |
| Time | T0 | 15 Days | 30 Days |
|---|---|---|---|
| Folding endurance | >10 | >10 | >10 |
| Elongation at break (%) | 62 ± 6 | 69 ± 7 | 65 ± 9 |
| Tensile strength (kPa) | 128 ± 10 | 115 ± 15 | 123 ± 13 |
| Parameter | Age | Body Mass Index (BMI) |
|---|---|---|
| Mean | 44 ± 6 | 26 ± 3 |
| Median | 46 | 26.5 |
| Range | 31–50 | 22.4–29.4 |
| Parameter | Geometric Means | Ratio of Geometric Means (Test/Reference in (%)) | 90% Confidence Interval | Intra-Subject CV (%) | |
|---|---|---|---|---|---|
| Film | Singulair® | ||||
| AUCt (ng×h/mL) | 3673 | 2409 | 152.46 | 101.02–230.10 | 45.58 |
| AUCinf (ng×h/mL) | 3827 | 2499 | 153.15 | 99.77–235.1 | 45.88 |
| Cmax (ng/mL) | 554 | 338 | 163.89 | 99.12–270.99 | 57.05 |
| Tmax (h) | 2.63 | 3.63 | |||
| Descriptive Statistics | 3.0 h | 7.0 h |
|---|---|---|
| N | 8 | 8 |
| Max (ng/mL) | 4.2 | 4.7 |
| Min (ng/mL) | 3.2 | 3.8 |
| Median (ng/mL) | 3.4 | 4.2 |
| Mean (ng/mL) | 3.6 | 4.2 |
| Std Dev (ng/mL) | 0.36 | 0.31 |
| CV (%) | 10.2 | 7.19 |
| System Organ Classification/ Preferred Term (PT) | Reported Incidence by Treatment Group | |
|---|---|---|
| MTK Film (N = 8) | MTK Tablet (N = 8) | |
| Nervous System Disorders | ||
| Somnolence | 2 (25.0%)) | 0 (0.0%) |
| Headache | 1 (12.5%) | 0 (0.0%) |
| Skin and Subcutaneous Tissue Disorders | ||
| Pruritus | 1 (12.5%) | 0 (0.0%) |
| Mechanical urticaria | 1 (12.5%) | 0 (0.0%) |
| Musculoskeletal and Connective Tissue Disorders | ||
| Back pain | 1 (12.5%) | 0 (0.0%) |
| Total | 6 (75.0%) | 0 (0.0%) |
| Treatment Group | Severity | Relationship to Drug | Intervention | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | Unrelated | Unlikely | Possible | Probable | Pharmacologic | Other | None | |
| A | 6 | 0 | 0 | 3 | 1 | 2 | 0 | 2 * | 1 * | 4 |
| B | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 6 | 0 | 0 | 3 | 1 | 2 | 0 | 2 | 1 | 4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michael, J.; Bessa de Sousa, D.; Conway, J.; Gonzalez-Labrada, E.; Obeid, R.; Tevini, J.; Felder, T.; Hutter-Paier, B.; Zerbe, H.; Paiement, N.; et al. Improved Bioavailability of Montelukast through a Novel Oral Mucoadhesive Film in Humans and Mice. Pharmaceutics 2021, 13, 12. https://doi.org/10.3390/pharmaceutics13010012
Michael J, Bessa de Sousa D, Conway J, Gonzalez-Labrada E, Obeid R, Tevini J, Felder T, Hutter-Paier B, Zerbe H, Paiement N, et al. Improved Bioavailability of Montelukast through a Novel Oral Mucoadhesive Film in Humans and Mice. Pharmaceutics. 2021; 13(1):12. https://doi.org/10.3390/pharmaceutics13010012
Chicago/Turabian StyleMichael, Johanna, Diana Bessa de Sousa, Justin Conway, Erick Gonzalez-Labrada, Rodolphe Obeid, Julia Tevini, Thomas Felder, Birgit Hutter-Paier, Horst Zerbe, Nadine Paiement, and et al. 2021. "Improved Bioavailability of Montelukast through a Novel Oral Mucoadhesive Film in Humans and Mice" Pharmaceutics 13, no. 1: 12. https://doi.org/10.3390/pharmaceutics13010012
APA StyleMichael, J., Bessa de Sousa, D., Conway, J., Gonzalez-Labrada, E., Obeid, R., Tevini, J., Felder, T., Hutter-Paier, B., Zerbe, H., Paiement, N., & Aigner, L. (2021). Improved Bioavailability of Montelukast through a Novel Oral Mucoadhesive Film in Humans and Mice. Pharmaceutics, 13(1), 12. https://doi.org/10.3390/pharmaceutics13010012