1. Introduction
Topically applied eye drops are the most commonly used dosage forms in ocular therapy. They are well tolerated by patients but have low bioavailability. The low effective concentration can be explained by the remarkable precorneal loss of drugs, which is due to the elimination mechanisms (tears production and blinking) and ocular barriers. One possibility of overcoming the natural anatomical barrier of the eye is to utilize the surface layer of the mucous membrane as a site of adhesion. This can be done by introducing mucoadhesive agents into the delivery system and increasing the penetration across the mucous layer and membranes. Mucoadhesives can be integrated into various delivery systems, and can be combined with various concepts, such as penetration enhancement and increased solubility. Mucoadhesive drug delivery can be an effective means of delivering ocular drugs as well [
1]. Mucoadhesive delivery systems act in two main ways: (i) prolonging residence time at the site of drug absorption and (ii) increasing the epithelial transport of drugs such as peptides and proteins [
2].
In the case of topical ophthalmic formulations, a strategy to increase the ocular residence time of active compounds can also be the incorporation of mucoadhesive polymers into the formulations. Mucoadhesives contribute to the formation of a viscous, continuous layer on the surface of the eye that partially protects the drug from elimination by tearing, prolonging the retention time on the eye surface. Different polymers such as carboxymethylcellulose, hydroxypropyl methylcellulose (HPMC), hyaluronic acid or xanthan gum have been used for this purpose in ophthalmic drug deliveries [
3,
4,
5] due to their good tolerance on the eye both in vitro and in vivo [
6].
The mucoadhesive approach can be transferred to nanoparticulate systems as well, where the use of mucoadhesive polymers in liposomes and other nanosystem formulations can result in greater efficacy and thus a more successful treatment of ophthalmic diseases [
7,
8]. This approach can be executed in two main ways: (i) application of a nano-hydrogel hybrid system, where the nanosystem is dispersed in a hydrogel, or (ii) modification of the nanoparticle’s surface with mucoadhesive features (linkage of adhesives and/or modification of the surface charge).
In recent years, the combination of nanocomposites, such as nanoparticles [
9], nanoemulsions [
10], or niosomes [
11], with hydrogels to improve the ophthalmic bioavailability of drugs after topical instillation have been published. In addition, combinations of liposomes and hydrogels are being evaluated by many research teams [
7,
12]. Among the polymers used to create the mentioned nano-hydrogel hybrid systems, carbopols, chitosans, HPMC, and natural gums have been the most commonly applied. Yu et al., 2015 [
12] prepared liposomes filled with timolol maleate and inserted them into a gellan gum gel. This combination increased the duration of action and shortened the onset of action. Lux et al. [
13] developed a lyophilized polymer matrix from hydroxypropyl methylcellulose (HPMC), which is located on a flexible poly(tetrafluoroethylene) carrier strip. The bioavailability of fluorescein was measured after loading the lyophilized (or lyophilizator) system into a sachet. Upon contact with the conjunctiva, the lyophilizate was rapidly hydrated by the tear fluid. Compared to conventional eye drops, this new dosage form resulted in significantly higher corneal and aqueous concentrations for 7 h after application. Morsi et al., 2017 [
10] prepared an acetazolamide-based nanoemulsion formulation by the inclusion of the combination of several polymers, among them HPMC, in the external phase. The authors observed that HPMC acted as a viscosity enhancer and was able to prolong the intraocular pressure lowering effect in glaucomatous rabbits. This action was attributed to the increased retention time of the nanoemulsion on the ocular surface.
Nanostructured lipid carriers (NLCs), which were functionalized for a mucoadhesive purpose, can be found in the literature with surface modification as well. J. Shen et al. [
14] developed a thiolated mucoadhesive polymer coated NLC with cysteine–polyethylene glycol stearate (Cys-PEG-SA) conjugates, administered topically to rabbit eyes. It was found that the encapsulated cyclosporin remains on the ocular surface for up to 6 h, and the precorneal retention time and concentration in the anterior segment increased compared with the NLC without thiomers.
Liu et al. [
15] investigated curcumin containing surface modified NLC systems with thiolated chitosan. They synthesized an N-acetyl-l-cysteine functionalized chitosan copolymer and compared these modified polymer coated NLC systems with the simple chitosan coated NLCs. The modification of chitosan significantly improved transcorneal penetration compared to chitosan hydrochloride coated and noncoated NLCs [
15]. Chanburee et al. examined the effect of various polymers on the mucoadhesive properties of different NLC systems. Curcumin-filled NLCs were prepared and the surface of the particles was coated with mucoadhesive polymers: polyethylene glycol 400 (PEG 400), polyvinyl alcohol (PVA), and chitosan (CS). In vitro mucoadhesive assays were evaluated by a wash test, and both PEG-NLC and PVA-NLC showed a strong interaction with porcine mucosa; the mucosal adhesion observed was twice as strong as for uncoated NLCs [
16].
Dexamethasone (DXM) is a steroidal anti-inflammatory drug, which is often used after eye surgery to prevent severe injury and inflammatory processes. The water solubility of DXM is low, which is why only suspensions are available in the market. The DXM suspension has very low bioavailability in the anterior segment of the eye because of drainage, lachrymation, poor retention at the absorption surface, and low penetration across the hydrophilic layers [
9]. As DXM is a lipophilic drug, its dissolution in an NLC might increase the effectiveness of DXM containing eye drops [
17]. Furthermore, NLC formulations might provide better bioavailability with mucoadhesive polymers.
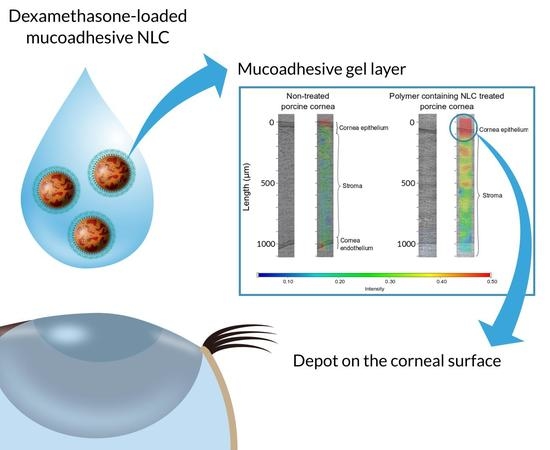
The aim of this study was to incorporate DXM into NLC systems that contain a mucoadhesive polymer (HPMC), where a mucoadhesive gel layer around the nanocarrier can ensure the adhesion of the nanoparticles to the mucosal surface. In our formulation, the mucoadhesive gel layer forms in situ because the amphiphilic characteristics of the polymer can result in its enrichment at the interface of the nanocarrier. A 23 factorial experimental design was made, in which the three factors were the polymer concentration, the DXM concentration, and the emulsifier concentration. The samples were then analyzed for particle size, zeta potential, polydispersity index, and Span value. The significant factors were identified. The biocompatibility of the formulations was evaluated with human corneal toxicity tests and immunoassay analysis. The possible increase in bioavailability was analyzed by means of mucoadhesivity, in vitro drug diffusion, and different penetration tests, such as in vitro cornea parallel artificial membrane permeability assay (PAMPA) model, human corneal cell penetration, and ex vivo porcine corneal penetration using Raman mapping.
2. Materials and Methods
2.1. Materials
Compritol 888ATO (glycerol dibehenate) was kindly supplied by Azelis Hungary Ltd. (Budapest, Hungary). Miglyol 812N (capric triglyceride) was provided by Sasol GmbH (Witten, Germany). Kolliphor RH40 (PEG-40 hydrogenated castor oil) was kindly supplied by BASF SE Chemtrade GmbH (Budapest, Hungary). Hydroxypropyl methylcellulose (Methocel F4M) was purchased from Colorcon (Dartford, Kent, England). DXM, DMSO, recombinant human insulin, recombinant human EGF, rat tail collagen, trypsin, ethylenediaminetetraacetic acid solution, collagen type I, Ringer buffer, Ringer-Hepes buffer, fluorescein, Evans blue labeled albumin, 3% paraformaldehyde solution, TX-100 solution, and bovine serum albumin were purchased from Sigma-Aldrich (St. Louis, MO, USA).
2.2. Sample Preparation
For the preparation of the NLC samples, an ultrasonication method was used. The lipids (Compritol 888 ATO and Miglyol 812N at 7:3 ratio) and surfactant (Cremophor RH40) were melted with a heating magnetic stirrer at 85 °C. The total lipid concentration was 10 w/w%. After that, DXM and the polymer (Methocel F4M) were added to the melted mixture and stirred at a temperature of 85 °C.
Pure water was heated at 85 °C and the two phases were mixed and ultrasonicated (one cycle, 70% amplitude, 10 min) with a Hielscher UP200S ultrasonic homogenizer (Hielscher Ultrasonics GmbH, Teltow, Germany). The NLC systems were cooled in an ice bath with continuous mixing using a magnetic stirrer.
Table 1 includes the compositions of the NLCs prepared.
2.3. X-ray Diffraction (XRD) Analysis of the Lyophilized NLCs
The solid state of DXM in the lyophilized lipid composition was analyzed with XRD. After the sample preparation, the formulations were freeze-dried.
In the case of NLC systems, freeze-drying was performed in Scanvac CoolSafe 100-9 Pro type equipment (LaboGene ApS, Lynge, Denmark). The liquid samples were transferred to 1.5 mL vials and freeze-dried at −40 °C for 24 h under 0.013 mbar pressure and then kept at 25 °C for 12 h as secondary drying to obtain lyophilized powders. The process was controlled by a computer program (Scanlaf CTS16a02); the temperature of the product and pressure values were monitored continuously.
The XRD measurements were performed with a Bruker D8 Advance diffractometer (Bruker AXS GmbH, Karlsruhe, Germany). The Cu K λI radiation (λ = 1.5406 Å) was used. The samples were scanned from 3° to 40° 2θ at 40 kV and 40 mA. The scanning speed was 0.1°/s, the step size was 0.010°.
2.4. Particle Size and Zeta Potential
The hydrodynamic diameter (Zave), zeta potential (ZP), and polydispersity index (PI) of NLCs 1-8 were investigated by the Zetasizer Nano ZS instrument (Malvern Instruments, Worcestershire, UK) with DTS 1070 folded capillary cell at 25 °C. The applied medium was purified water. The refractive index (RI) was 1.3553. Three parallel measurements were made and 6-fold dilution was used.
The NLCs (
Table 1) were also analyzed by particle size and particle size distribution measurements using laser diffraction, Mastersizer 2000 Hydro tool (Malvern Instruments, Worcestershire, UK). The d(0.1), d(0.5), and d(0.9) were assessed. The measuring medium was purified water with RI of 1.33. The RI of the samples was 1.36 and the imaginary RI was 0.01. The Span value can be calculated with the following Equation (1):
In order to evaluate the stability of NLCs, the particle size and ZP measurements were repeated after 1 week.
2.5. Entrapment Efficacy
The entrapment efficacy (EE%) of the NLCs was determined with this method. The clear aqueous phase of the NLCs was separated by centrifugation in Vivaspin 15R 5000 MWCO Hydrosart tubes (Sartorius, Stonehouse, UK) with Hermle Z323K, (HERMLE Labortechnik GmbH, Wehingen, Germany). Centrifugation was performed at 5000 rpm (9000 rcf) for 30 min at 4 °C.
The DXM content of the filtered solution was examined by HPLC (Shimadzu Nexera X2 UHPLC, Kyoto, Japan), which was equipped with a C18 reverse-phase column (Phenomenex Kinetex C18, Phenomenex, Torrance, CA, USA) with dimensions of 2.6 µm, 100 Å, 150 × 4.6 mm. The separation was evaluated with gradient elution with the following program: time (min)/% of acetonitrile: 0/35, 4.0/60, 4.01/35, 6.0/35, and the detection was made at 240 nm. The injection volume was 5 µL and the flow rate was 1 mL/min. The column temperature was 40 °C. The time of analysis was 6 min and the retention time for DXM was 3.6 min.
The following equation was used to calculate
EE% (2):
2.6. Mucoadhesion Study
The mucoadhesion of the formulations (
Table 1) and the polymer-free version of the compositions was investigated with a TA.XT plus Texture Analyzer (Stable Micro Systems Ltd., Vienna Court, Lammas Road, Godalming, Surrey, UK. GU7 1YL). A cylinder probe with a diameter of 1 cm [
18,
19] and a 1 kg load cell were used. Samples were placed in contact with a filter paper disc wetted with 50 µL of an 8%
w/
w mucin dispersion as in vitro mucosal surface [
19]. The mucin dispersion was made with PBS buffer (pH = 7.4). Five parallel measurements were made. Twenty mg of the sample was attached to the fixed filter paper of the cylinder probe and placed in contact with the artificial mucosal surface. A 2500 mN preload was applied for 3 min. The cylinder probe was moved upwards to separate the sample from the substrate at a prefixed speed of 2.5 mm min
−1. The work of adhesion (A, mN mm) was used to characterize the mucoadhesive behavior, which was calculated as the area (AUC) under the ‘‘force vs. distance’’ curve.
2.7. In Vitro Drug Release Study
To investigate in vitro drug release, the dialysis bag method was used. Firstly, 200 µL of the samples (NLC1-8) were filled in a Spectra/Por
® 4 dialysis membrane (Spectrum Laboratories, Inc., Rancho Dominguez, CA, USA), with Spectra/Por
® Closures (Spectrum Laboratories, Inc.). From each composition of NLCs, 3 replicates were used and placed into 20 mL of phosphate-buffered saline (PBS) (PBS of pH = 7.4 was prepared by dissolving 8 g dm
−3 NaCl, 0.2 g dm
−3 KCl, 1.44 g dm
−3 Na
2HPO
4·2H
2O and 0.12 g dm
−3 KH
2PO
4 in distilled water, the pH was adjusted with 0.1 M HCl). The sink condition was ensured during the experiments. The systems were held at 35 °C to mimic in vivo conditions and stirred at 370 rpm with a magnetic stirrer. During the diffusion study, seven sampling times were used (0.5, 1, 2, 3, 4, 5, 6 h) by removing 1 mL from the acceptor phase and replacing it with fresh thermostated PBS. As reference preparation, a DXM suspension (0.1 and 0.05
w/
w%) was formulated (d(0.5) = 7.8 µm measured by Mastersizer 2000) similarly to DXM suspensions in the market. The diffused amounts of DXM were analyzed by HPLC (the HPLC method is described in
Section 2.10).
2.8. Penetration Study on Corneal-PAMPA Model
For the in vitro transcorneal permeability measurement, the previously reported corneal-PAMPA method was applied [
20]. DXM and its formulations were used as a donor solution. In order to create the lipid membrane, phosphatidylcoline (PC, 16 mg) was dissolved in a solvent mixture (70% (
v/
v) hexane, 25% (
v/
v) dodecane, 5% (
v/
v) chloroform), and then each well of the donor plate (MultiscreenTM-IP, MAIPN4510, pore size 0.45 mm; Millipore) was coated with the lipid solution (5 μL each). Then hexane and chloroform were evaporated to form a PC lipid membrane with the concentration of 10.67
w/
v% in each well. The donor plate was then fit into the acceptor plate (Multiscreen Acceptor Plate, MSSACCEPTOR; Millipore) containing 300 μL of PBS solution (pH 7.4), and 150–150 μL of the PBS solutions were put on the membrane of the donor plate. The donor plate was covered with a sheet of wet tissue paper and a plate lid to avoid evaporation. The plates were incubated for 4 h at 35 °C (Heidolph Titramax 1000) followed by the separation of PAMPA sandwich plates and the determination of the concentrations of the APIs in the donor and acceptor solutions by HPLC method (
Section 2.5). Test solutions from PAMPA experiments were prepared in 96-well plates and sealed before injection. For each assay, 3 replicates per compound were measured. The effective permeability and membrane retention of drugs were calculated using Equation (3) [
20]:
where
Pe is the effective permeability coefficient (cm s
−1),
A is the filter area (0.24 cm
2),
VA is the volume of the acceptor phase (0.3 cm
3),
t is the incubation time (s),
τSS is the time to reach steady-state (s),
CA(
t) is the concentration of the compound in the acceptor phase at time point t (mol cm
−3), S is the free drug content of DXM in the donor phase.
2.9. Human Corneal Epithelial Cell (HCE-T) Line
Human corneal epithelial cells (HCE-T; RCB 2280; RIKEN BRC, Tsukuba, Japan) were immortalised by transfection with a recombinant SV40-adenovirus vector, established and characterized by Araki-Sasaki [
21]. The cells were grown in Dulbecco’s Modified Eagle’s Medium/F-12 (Gibco, Life Technologies, Carlsbad, CA, USA) supplemented with 10% fetal bovine serum (Gibco, Life Technologies, Carlsbad, CA, USA), 0.5% DMSO, 5 µg/mL recombinant human insulin and 10 ng/mL recombinant human EGF in a humidified incubator with 5% CO
2 at 37 °C. All plastic surfaces were coated with 0.05% rat tail collagen in sterile distilled water before cell seeding in culture dishes. The culture medium was changed every second day. When cells reached approximately 80–90% confluence in the dish, they were subcultured with 0.05% trypsin–ethylenediaminetetraacetic acid solution.
2.10. Cell Viability Measurements
Real-time cell electronic sensing was used to follow cell damage and/or protection in living barrier forming cells. The RTCA-SP instrument (ACEA Biosciences, San Diego, CA, USA) registered the impedance of cell layers every 10 min and at each time point the cell index was defined as (Rn − Rb)/15, where Rn is the cell-electrode impedance of the well when it contains cells and Rb is the background impedance of the well with the medium alone. The 96-well E-plates with built-in gold electrodes were coated with collagen type I (50 μg/mL for both) and dried for 20 min under sterile air-flow. Culture medium (60 μL) was added to each well for background readings, then 50 µL of HCE-T suspension was dispensed at the density of 5 × 103 cells/well. When cells reached a steady growth phase, they were treated.
For cell viability measurements, the originally prepared liquid formulations such as NLC1, NLC2, NLC3, and NLC4 (
Table 1) formulations and HPMC solution were prepared as 10×, 30× and 100× dilutions in cell culture media.
2.11. Immunohistochemistry
Morphological changes in HCE-T cells were investigated by immunostaining for junctional proteins zonula occludens protein-1 (ZO-1), occludin, β-catenin and E-cadherin. Cells were grown on culture inserts used for permeability experiments. After the treatment, the inserts were washed with PBS and the cells were fixed with 3% paraformaldehyde solution for 15 min at room temperature. The cells were permeabilized by 0.2% TX-100 solution for 10 min and the nonspecific binding sites were blocked with 3% bovine serum albumin in PBS. Primary antibodies rabbit anti-ZO-1 (AB_138452, 1:400; Life Technologies, Carlsbad, CA, USA), rabbit anti-β-catenin (AB_476831, 1:400), rabbit anti-occludin (AB_2533977, 1:100; Life Technologies, Carlsbad, CA, USA) and mouse anti-E-cadherin (AB_397580, 1:400; Life Technologies, Carlsbad, CA, USA) were applied as overnight treatment. Incubation with secondary antibodies Alexa Fluor-488-labeled anti-mouse (AB_2534088, 1:400; Life Technologies, Invitrogen, Carlsbad, CA, USA) and anti-rabbit IgG Cy3 conjugated (AB_258792, 1:400) lasted for 1 h. Hoechst dye 33342 was used to stain cell nuclei. After mounting the samples (Fluoromount-G; Southern Biotech, Birmingham, AL, USA), staining was visualized by a confocal laser scanning microscope (Olympus Fluoview FV1000, Olympus Life Science Europa GmbH, Hamburg, Germany).
2.12. Permeability Study on Cell Culture Model
Transepithelial electrical resistance (TEER) reflects the tightness of the intercellular junctions closing the paracellular cleft, therefore the overall tightness of cell layers of biological barriers. TEER was measured to check the barrier integrity by an EVOM volt-ohmmeter (World Precision Instruments, Sarasota, FL, USA) combined with STX-2 electrodes, and was expressed relative to the surface area of the monolayers as Ω × cm2. TEER of cell-free inserts was subtracted from the measured data. Cells were treated when the cell layer had reached steady TEER values.
HCE-T cells were seeded at a density of 105 cells onto Transwell inserts (polycarbonate membrane, 0.4 µm pore size, 1.12 cm2 surface area; 3401, Corning Life Sciences, Tewksbury, MA, USA) and cultured for 5–8 days at liquid-liquid and for 4–6 days at air-liquid interface. The culture medium was changed and TEER was checked every second day.
For the permeability experiments, the inserts were transferred to 12-well plates containing 1.5 mL Ringer buffer in the acceptor (lower/basal) compartments. In the donor (upper/apical) compartments, 0.5 mL buffer was pipetted containing different formulations of DXM (10-times dilution of NLCs). To avoid unstirred water layer effect, the plates were kept on a horizontal shaker (120 rpm) during the assay. The assay lasted for 60 min. At a 30-min timepoint, the inserts were transferred to a new well containing Ringer-Hepes buffer. Samples from both compartments were collected and the DXM concentration was detected by HPLC.
To determine the tightness of the cornea epithelial culture model, two passive permeability marker molecules were tested [
22]. In the donor compartments 0.5 mL buffer containing fluorescein (10 μg/mL; Mw: 376 Da) and Evans blue labeled albumin (167.5 μg/mL Evans blue dye and 10 mg/mL bovine serum albumin; MW: 67.5 kDa) was added. The inserts were kept in 12-well plates on a horizontal shaker (120 rpm) for 30 min. The concentrations of the marker molecules in the samples from the compartments were determined by a fluorescence multiwell plate reader (Fluostar Optima, BMG Labtechnologies, Germany; fluorescein: excitation wavelength: 485 nm, emission wavelength: 520 nm; Evans blue labeled albumin: excitation wavelength: 584 nm, emission wavelength: 680 nm).
The apparent permeability coefficients (P
app) were calculated as described previously [
22]. Briefly, cleared volume was calculated from the concentration difference of the tracer in the acceptor compartment (Δ[
C]
A) after 30 min and donor compartments at 0 h ([
C]
D), the volume of the acceptor compartment (
VA; 1.5 mL), and the surface area available for permeability (
A; 1.1 cm
2) using Equation (4):
For permeability measurements, NLC5, NLC6, NLC7, and NLC8 formulations were applied at 10 times dilution and DXM at 1 mg/mL concentration, all diluted in Ringer-Hepes buffer.
2.13. Experimental Design
In order to characterize the polymer containing NLC compositions, a 2
3 full factorial design was applied, which is suitable for generating a first-order polynomial model (Equation (5)) and for the investigation of the linear response surface. The model describes the principal effects and interaction among the identified variables.
where
a0 is the intercept,
a1,2,3 were the regression coefficients values.
x1, x2, and
x3 correspond to factors A, B and C, respectively.
The independent factors were A (polymer concentration), B (DXM concentration), and C (surfactant concentration). The optimization parameters were indicated in each measurement, when they were applicable. The chosen factors were examined at two levels (+1 and −1), which corresponds to the values in
Table 1.
2.14. Penetration Study on Porcine Cornea
The ex vivo penetration test was examined with Raman microscopy. The pig conjunctiva came from a slaughterhouse and was kept at −20 °C until measurement. The porcine cornea was placed on a sterile cotton wool bed moistened with physiological saline solution and the cornea was surrounded by a Teflon ring to prevent the flow of eye drops into the conjunctiva. The cornea was instilled with 250 µL of NLC sample (NLC6 and the polymer-free version of NLC6) every 30 min and the formulation was removed just before the next instillation. The duration of treatment was six hours. The system was thermostated at 35 °C. The treated cornea was frozen and divided into cross sections (20 μm thick) onto aluminum-coated slides using a Leica CM1950 cryostat (Leica Biosystems GmbH, Wetzlar, Germany). Untreated porcine cornea was used as a reference. Microscopic measurements of Raman were performed with a Thermo Scientific DXR Raman microscope (Thermo Fisher Scientific, Waltham, MA, USA). We used 780 nm laser light with a maximum power of 24 mW. The microscopic lenses used for the measurement were magnified 50× and the aperture was 25 mm. The chemical mapping area examined was 150 × 1200 μm; the size of the step was 50 μm vertically and horizontally. A total of 72 spectra were recorded, 16 images were collected for each spectrum, and the exposure time was 5 s. The operation of the instrument and evaluation of the measurements were performed by OMNIC for the Dispersive Raman 8.2 software package (Thermo Fisher Scientific). The characteristic peaks of the DXM spectrum coincided with the characteristic peaks of the corneal tissue; however, the profiled map showed a detectable NLC6 signal. Therefore, during the evaluation, profiling of the Raman map was performed using the entire NLC spectrum.
2.15. Statistical Analysis
All data presented are means ± SD. For the factorial design and mucoadhesive studies, statistical data analysis was performed using Statistica for Windows, version 10. In the case of cell penetration tests, the values were compared using one-way ANOVA followed by Dunnett’s test, 2-way ANOVA followed by the Bonferroni test with GraphPad Prism 5.0 software (GraphPad Software, Inc., San Diego, CA, USA). A level of p ≤ 0.05 was taken as significant, p ≤ 0.01 as very significant, and p ≤ 0.001 as highly significant.
4. Conclusions
In the present study, DXM-loaded NLCs were successfully combined with a mucoadhesive polymer. In our formulations, a mucoadhesive gel layer might be formed at the interface of the nanoparticle, thanks to the amphiphilic characteristics of HPMC.
Based on the results of the mucoadhesive studies, the incorporation of HPMC increased the mucoadhesive properties compared with the polymer-free formulations, even at very low polymer concentration.
The characterization of nanoparticles (Zave, PDI, d(0.5) and Span values) indicated that the preparation with the lowest absolute ZP values had the highest stability, which may suggest that our polymer-surfactant containing systems are mainly sterically stabilized.
The biocompatibility of the NLC systems was evaluated using toxicity tests on HCE-T cells with impedance measurement and immunoassay analyses. These measurements indicated no cell damage after treatment and the compositions did not have any harmful effects on cell junctions.
The drug release study of DXM showed increased drug diffusion from the NLC systems compared with conventional suspension forms, and it could also be concluded that the formulation with very high entrapment efficiency can hinder drug release from the nanoparticles. These results were in correlation with the cell permeability assays, where the optimized NLCs presented significantly better permeability across HCE-T cells.
The mucoadhesivity and penetration enhancing effects of our NLCs were presented in an ex vivo penetration-retention study through porcine cornea with Raman correlation mapping. The non-treated and treated (NLC with and without polymer) porcine corneas were compared. The results showed that the NLC systems with HPMC polymers could create a depot on the surface of the cornea. This might suggest a potential sustained release and increased residence time of DXM using this type of polymer-modified NLC systems.