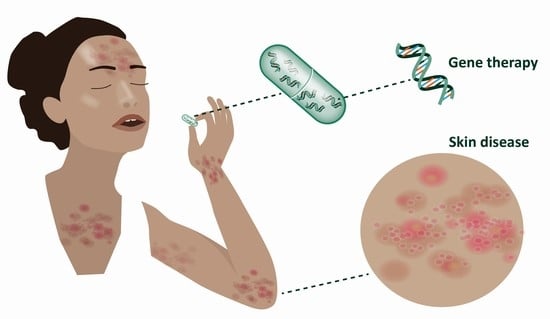
Future Perspectives of Oral Delivery of Next Generation Therapies for Treatment of Skin Diseases
Abstract
:1. An Introduction to the Next Generation of Treatments
1.1. Oligonucleotides
1.2. DNA Editors
2. Gene Therapy in Dermatology
2.1. Gene Therapy and Gene Editing
2.2. Oligonucleotide Therapies in Dermatology
2.3. Gene Delivery Challenges
3. Evolution of Macromolecule Delivery
3.1. From Injections to Oral Delivery of Macromolecules
3.2. Oral Oligonucleotides
3.3. Oral Delivery of Macromolecules
3.4. Drug Device Combinations for Oral Delivery
4. Forward Looking
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fakhr, E.; Zare, F.; Teimoori-Toolabi, L. Precise and efficient siRNA design: A key point in competent gene silencing. Cancer Gene Ther. 2016, 23, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Roberts, T.C.; Langer, R.; Wood, M.J.A. Advances in oligonucleotide drug delivery. Nat. Rev. Drug Discov. 2020, 19, 673–694. [Google Scholar] [CrossRef] [PubMed]
- Hu, B.; Zhong, L.; Weng, Y.; Peng, L.; Huang, Y.; Zhao, Y.; Liang, X.J. Therapeutic siRNA: State of the art. Signal Transduct. Target. Ther. 2020, 5, 101. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, J.A.; Witzigmann, D.; Thomson, S.B.; Chen, S.; Leavitt, B.R.; Cullis, P.R.; van der Meel, R. The current landscape of nucleic acid therapeutics. Nat. Nanotechnol. 2021, 16, 630–643. [Google Scholar] [CrossRef] [PubMed]
- Chery, J. RNA therapeutics: RNAi and antisense mechanisms and clinical applications. Postdoc. J. 2016, 4, 35–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Svoboda, P. Key Mechanistic Principles and Considerations Concerning RNA Interference. Front. Plant Sci. 2020, 11, 1237. [Google Scholar] [CrossRef]
- Zhang, J. RNA-Cleaving DNAzymes: Old Catalysts with New Tricks for Intracellular and In Vivo Applications. Catalysts 2018, 8, 550. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Nguyen, K.; Spitale, R.C.; Chaput, J.C. A biologically stable DNAzyme that efficiently silences gene expression in cells. Nat. Chem. 2021, 13, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, R.; Purath, U.; Turowska, A.; Homburg, U.; Runkel, F.; Schmidts, T.; Dobler, D.; Renz, H.; Garn, H.; Mueller, A. Effects of interference with GATA-3 expression by target-specific DNAzyme treatment on disease progression in a subacute oxazolone-induced mouse model of atopic dermatitis. Clin. Transl. Allergy 2015, 5, O21. [Google Scholar] [CrossRef] [Green Version]
- Allemailem, K.S.; Almatroudi, A.; Alsahli, M.A.; Basfar, G.T.; Alrumaihi, F.; Rahmani, A.H.; Khan, A.A. Recent advances in understanding oligonucleotide aptamers and their applications as therapeutic agents. 3 Biotech 2020, 10, 551. [Google Scholar] [CrossRef] [PubMed]
- Giudice, V.; Mensitieri, F.; Izzo, V.; Filippelli, A.; Selleri, C. Aptamers and Antisense Oligonucleotides for Diagnosis and Treatment of Hematological Diseases. Int. J. Mol. Sci. 2020, 21, 3252. [Google Scholar] [CrossRef]
- Stanton, R.; Sciabola, S.; Salatto, C.; Weng, Y.; Moshinsky, D.; Little, J.; Walters, E.; Kreeger, J.; DiMattia, D.; Chen, T.; et al. Chemical modification study of antisense gapmers. Nucleic Acid Ther. 2012, 22, 344–359. [Google Scholar] [CrossRef]
- Layzer, J.M.; McCaffrey, A.P.; Tanner, A.K.; Huang, Z.; Kay, M.A.; Sullenger, B.A. In vivo activity of nuclease-resistant siRNAs. RNA 2004, 10, 766–771. [Google Scholar] [CrossRef] [Green Version]
- Wan, W.B.; Seth, P.P. The Medicinal Chemistry of Therapeutic Oligonucleotides. J. Med. Chem. 2016, 59, 9645–9667. [Google Scholar] [CrossRef]
- Chernikov, I.V.; Vlassov, V.V.; Chernolovskaya, E.L. Current Development of siRNA Bioconjugates: From Research to the Clinic. Front. Pharmacol. 2019, 10, 444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sajid, M.I.; Moazzam, M.; Kato, S.; Yeseom Cho, K.; Tiwari, R.K. Overcoming Barriers for siRNA Therapeutics: From Bench to Bedside. Pharmaceuticals 2020, 13, 294. [Google Scholar] [CrossRef] [PubMed]
- Springer, A.D.; Dowdy, S.F. GalNAc-siRNA Conjugates: Leading the Way for Delivery of RNAi Therapeutics. Nucleic Acid Ther. 2018, 28, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S.; Simon, A.R.; Goel, V.; Habtemariam, B.A.; Clausen, V.A.; Kim, J.B.; Robbie, G.J. Pharmacokinetics and Pharmacodynamics of the Small Interfering Ribonucleic Acid, Givosiran, in Patients with Acute Hepatic Porphyria. Clin. Pharmacol. Ther. 2020, 108, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Doudna, J.A. The promise and challenge of therapeutic genome editing. Nature 2020, 578, 229–236. [Google Scholar] [CrossRef]
- Komor, A.C.; Kim, Y.B.; Packer, M.S.; Zuris, J.A.; Liu, D.R. Programmable editing of a target base in genomic DNA without double-stranded DNA cleavage. Nature 2016, 533, 420–424. [Google Scholar] [CrossRef] [Green Version]
- Kantor, A.; McClements, M.E.; MacLaren, R.E. CRISPR-Cas9 DNA Base-Editing and Prime-Editing. Int. J. Mol. Sci. 2020, 21, 6240. [Google Scholar] [CrossRef]
- Knott, G.J.; Doudna, J.A. CRISPR-Cas guides the future of genetic engineering. Science 2018, 361, 866–869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Porto, E.M.; Komor, A.C.; Slaymaker, I.M.; Yeo, G.W. Base editing: Advances and therapeutic opportunities. Nat. Rev. Drug Discov. 2020, 19, 839–859. [Google Scholar] [CrossRef] [PubMed]
- Komor, A.C.; Badran, A.H.; Liu, D.R. CRISPR-Based Technologies for the Manipulation of Eukaryotic Genomes. Cell 2017, 168, 20–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rees, H.A.; Minella, A.C.; Burnett, C.A.; Komor, A.C.; Gaudelli, N.M. CRISPR-derived genome editing therapies: Progress from bench to bedside. Mol Ther. 2021. [Google Scholar] [CrossRef]
- Anzalone, A.V.; Randolph, P.B.; Davis, J.R.; Sousa, A.A.; Koblan, L.W.; Levy, J.M.; Chen, P.J.; Wilson, C.; Newby, G.A.; Raguram, A.; et al. Search-and-replace genome editing without double-strand breaks or donor DNA. Nature 2019, 576, 149–157. [Google Scholar] [CrossRef]
- Lino, C.A.; Harper, J.C.; Carney, J.P.; Timlin, J.A. Delivering CRISPR: A review of the challenges and approaches. Drug Deliv. 2018, 25, 1234–1257. [Google Scholar] [CrossRef] [Green Version]
- Mehta, A.; Merkel, O.M. Immunogenicity of Cas9 Protein. J. Pharm. Sci. 2020, 109, 62–67. [Google Scholar] [CrossRef] [Green Version]
- Gillmore, J.D.; Gane, E.; Taubel, J.; Kao, J.; Fontana, M.; Maitland, M.L.; Seitzer, J.; O’Connell, D.; Walsh, K.R.; Wood, K.; et al. CRISPR-Cas9 In Vivo Gene Editing for Transthyretin Amyloidosis. N. Engl. J. Med. 2021, 385, 493–502. [Google Scholar] [CrossRef]
- Urits, I.; Swanson, D.; Swett, M.C.; Patel, A.; Berardino, K.; Amgalan, A.; Berger, A.A.; Kassem, H.; Kaye, A.D.; Viswanath, O. A Review of Patisiran (ONPATTRO®) for the Treatment of Polyneuropathy in People with Hereditary Transthyretin Amyloidosis. Neurol. Ther. 2020, 9, 301–315. [Google Scholar] [CrossRef]
- McKinsey & Company. Gene Therapy Coming of Age: Opportunities and Challenges to Getting Ahead. 2019. Available online: https://www.mckinsey.com/industries/pharmaceuticals-and-medical-products/our-insights/gene-therapy-coming-of-age-opportunities-and-challenges-to-getting-ahead (accessed on 18 July 2021).
- Zhang, W.W.; Li, L.; Li, D.; Liu, J.; Li, X.; Li, W.; Xu, X.; Zhang, M.J.; Chandler, L.A.; Lin, H.; et al. The First Approved Gene Therapy Product for Cancer Ad-p53 (Gendicine): 12 Years in the Clinic. Hum. Gene Ther. 2018, 29, 160–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moran, N. First gene therapy approved. Nat. Biotechnol. 2012, 30, 1153. [Google Scholar] [CrossRef]
- US Food and Drug Administration. FDA Approval Brings First Gene Therapy to the United States. 2017. Available online: https://www.fda.gov/news-events/press-announcements/fda-approval-brings-first-gene-therapy-united-states (accessed on 31 May 2021).
- Gene Therapy Net. Gene Therapy Products on the Market. 2021. Available online: https://www.genetherapynet.com/gene-therapy-products-on-the-market/624-gene-therapy-products-on-the-market.html (accessed on 14 July 2021).
- Bardhan, A.; Bruckner-Tuderman, L.; Chapple, I.L.C.; Fine, J.D.; Harper, N.; Has, C.; Magin, T.M.; Marinkovich, M.P.; Marshall, J.F.; McGrath, J.A.; et al. Epidermolysis bullosa. Nat. Rev. Dis. Primers 2020, 6, 78. [Google Scholar] [CrossRef] [PubMed]
- Bonafont, J.; Mencía, A.; Chacón-Solano, E.; Srifa, W.; Vaidyanathan, S.; Romano, R.; Garcia, M.; Hervás-Salcedo, R.; Ugalde, L.; Duarte, B.; et al. Correction of recessive dystrophic epidermolysis bullosa by homology-directed repair-mediated genome editing. Mol. Ther. 2021, 29, 2008–2018. [Google Scholar] [CrossRef]
- Jacków, J.; Guo, Z.; Hansen, C.; Abaci, H.E.; Doucet, Y.S.; Shin, J.U.; Hayashi, R.; DeLorenzo, D.; Kabata, Y.; Shinkuma, S.; et al. CRISPR/Cas9-based targeted genome editing for correction of recessive dystrophic epidermolysis bullosa using iPS cells. Proc. Natl. Acad. Sci. USA 2019, 116, 26846–26852. [Google Scholar] [CrossRef]
- Hainzl, S.; Peking, P.; Kocher, T.; Murauer, E.M.; Larcher, F.; Rio, M.D.; Duarte, B.; Steiner, M.; Klausegger, A.; Bauer, J.W.; et al. COL7A1 Editing via CRISPR/Cas9 in Recessive Dystrophic Epidermolysis Bullosa. Mol. Ther. 2017, 25, 2573–2584. [Google Scholar] [CrossRef] [Green Version]
- Pulkkinen, L.; Uitto, J. Mutation analysis and molecular genetics of epidermolysis bullosa. Matrix Biol. 1999, 18, 29–42. [Google Scholar] [CrossRef]
- Marinkovich, M.P.; Tang, J.Y. Gene Therapy for Epidermolysis Bullosa. J. Investig. Dermatol. 2019, 139, 1221–1226. [Google Scholar] [CrossRef] [Green Version]
- Christiano, A.M.; Greenspan, D.S.; Lee, S.; Uitto, J. Cloning of human type VII collagen. Complete primary sequence of the alpha 1(VII) chain and identification of intragenic polymorphisms. J. Biol. Chem. 1994, 269, 20256–20262. [Google Scholar] [CrossRef]
- Woodley, D.T.; Keene, D.R.; Atha, T.; Huang, Y.; Ram, R.; Kasahara, N.; Chen, M. Intradermal injection of lentiviral vectors corrects regenerated human dystrophic epidermolysis bullosa skin tissue in vivo. Mol. Ther. 2004, 10, 318–326. [Google Scholar] [CrossRef]
- Kerstin, B.; Kaufmann, H.B.; Galy, A.; Schambach, A.; Grez, M. Gene therapy on the move. EMBO Mol. Med. 2013, 5, 1642–1661. [Google Scholar]
- Robbins, P.B.; Sheu, S.M.; Goodnough, J.B.; Khavari, P.A. Impact of laminin 5 beta3 gene versus protein replacement on gene expression patterns in junctional epidermolysis bullosa. Hum. Gene Ther. 2001, 12, 1443–1448. [Google Scholar] [CrossRef]
- Seitz, C.S.; Giudice, G.J.; Balding, S.D.; Marinkovich, M.P.; Khavari, P.A. BP180 gene delivery in junctional epidermolysis bullosa. Gene Ther. 1999, 6, 42–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Medicines Agency. EU Clinical Trial Register. 2021. Available online: https://www.clinicaltrialsregister.eu/ (accessed on 11 May 2021).
- National Institutes of Health—US National Library of Medicine. 2021. Available online: www.clinicaltrials.gov (accessed on 11 June 2021).
- Hirsch, T.; Rothoeft, T.; Teig, N.; Bauer, J.W.; Pellegrini, G.; De Rosa, L.; Scaglione, D.; Reichelt, J.; Klausegger, A.; Kneisz, D.; et al. Regeneration of the entire human epidermis using transgenic stem cells. Nature 2017, 551, 327–332. [Google Scholar] [CrossRef]
- De Rosa, L.; Carulli, S.; Cocchiarella, F.; Quaglino, D.; Enzo, E.; Franchini, E.; Giannetti, A.; De Santis, G.; Recchia, A.; Pellegrini, G.; et al. Long-term stability and safety of transgenic cultured epidermal stem cells in gene therapy of junctional epidermolysis bullosa. Stem Cell Rep. 2014, 2, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Community College Bioscience. Castle Creek Bioscience. Available online: https://castlecreekbio.com/autologous-fibroblast-pipeline/gene-therapy-dystrophic-epidermolysis-bullosa/ (accessed on 28 July 2021).
- Abeona Therapeutics. Abeona Therapeutics Announces Updated EB-101 Phase 1/2a Clinical Results in Recessive Dystrophic Epidermolysis Bullosa at the Society for Pediatric Dermatology 46th Annual Meeting. 2021. Available online: https://www.abeonatherapeutics.com/ (accessed on 22 August 2021).
- Eichstadt, S.; Barriga, M.; Ponakala, A.; Teng, C.; Nguyen, N.T.; Siprashvili, Z.; Nazaroff, J.; Gorell, E.S.; Chiou, A.S.; Taylor, L.; et al. Phase 1/2a clinical trial of gene-corrected autologous cell therapy for recessive dystrophic epidermolysis bullosa. JCI Insight 2019, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Supp, D.M.; Hahn, J.M.; Combs, K.A.; McFarland, K.L.; Schwentker, A.; Boissy, R.E.; Boyce, S.T.; Powell, H.M.; Lucky, A.W. Collagen VII Expression Is Required in Both Keratinocytes and Fibroblasts for Anchoring Fibril Formation in Bilayer Engineered Skin Substitutes. Cell Transpl. 2019, 28, 1242–1256. [Google Scholar] [CrossRef] [Green Version]
- Chavanas, S.; Bodemer, C.; Rochat, A.; Hamel-Teillac, D.; Ali, M.; Irvine, A.D.; Bonafé, J.-L.; Wilkinson, J.; Taïeb, A.; Barrandon, Y.; et al. Mutations in SPINK5, encoding a serine protease inhibitor, cause Netherton syndrome. Nat. Genet. 2000, 25, 141–142. [Google Scholar] [CrossRef]
- Di, W.L.; Larcher, F.; Semenova, E.; Talbot, G.E.; Harper, J.I.; Del Rio, M.; Thrasher, A.J.; Qasim, W. Ex-vivo gene therapy restores LEKTI activity and corrects the architecture of Netherton syndrome-derived skin grafts. Mol. Ther. 2011, 19, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Di, W.L.; Lwin, S.M.; Petrova, A.; Bernadis, C.; Syed, F.; Farzaneh, F.; Moulding, D.; Martinez, A.E.; Sebire, N.J.; Rampling, D.; et al. Generation and Clinical Application of Gene-Modified Autologous Epidermal Sheets in Netherton Syndrome: Lessons Learned from a Phase 1 Trial. Hum. Gene Ther. 2019, 30, 1067–1078. [Google Scholar] [CrossRef]
- Krishnan, S.; Agarwal, P.; Freedman, J.C.; O’Malley, M.E.; Regula, L.K.; Krystal Biotech Inc. Compositions and Methods for the Treatment of Autosomal Recessive Congenital Ichthyosis. U.S. Patent 10,525,090, 1 July 2020. [Google Scholar]
- Krystal Biotech. Krystal Biotech Announces Completion of Patient Enrollment in the GEM-3 Pivotal Trial of B-VEC for the Treatment of Dystrophic Epidermolysis Bullosa. 2021. Available online: https://ir.krystalbio.com/news-releases/news-release-details/krystal-biotech-announces-completion-patient-enrollment-gem-3 (accessed on 7 July 2021).
- Amryt Pharma. Amryt Pharma Corporate Overview March 2021. Available online: https://www.amrytpharma.com/wp-content/uploads/2021/03/AMRYT-Corporate-Overview-Presentation-March-2021-FINAL.pdf (accessed on 13 July 2021).
- Intrado. Amryt Receives Positive Opinion From EMA on Orphan Drug Designation for AP103. 2020. Available online: https://www.globenewswire.com/fr/news-release/2020/09/15/2093560/0/en/AMRYT-RECEIVES-POSITIVE-OPINION-FROM-EMA-ON-ORPHAN-DRUG-DESIGNATION-FOR-AP103.html (accessed on 26 June 2021).
- Jackow, J.; Guo, Z.; Abaci, E.; Doucet, Y.; Hansen, C.; Salas-Alanis, J.; Christiano, A. Biallelic correction of recessive dystrophic epidermolysis bullosa mutations in iPSCs using CRISPR/Cas9- based genome editing. J. Investig. Dermatol. 2017, 137, S225. [Google Scholar] [CrossRef]
- Webber, B.R.; Osborn, M.J.; McElroy, A.N.; Twaroski, K.; Lonetree, C.-l.; DeFeo, A.P.; Xia, L.; Eide, C.; Lees, C.J.; McElmurry, R.T.; et al. CRISPR/Cas9-based genetic correction for recessive dystrophic epidermolysis bullosa. NPJ Regen. Med. 2016, 1, 16014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonafont, J.; Mencía, Á.; García, M.; Torres, R.; Rodríguez, S.; Carretero, M.; Chacón-Solano, E.; Modamio-Høybjør, S.; Marinas, L.; León, C.; et al. Clinically Relevant Correction of Recessive Dystrophic Epidermolysis Bullosa by Dual sgRNA CRISPR/Cas9-Mediated Gene Editing. Mol. Ther. 2019, 27, 986–998. [Google Scholar] [CrossRef] [PubMed]
- Wan, T.; Pan, Q.; Ping, Y. Microneedle-assisted genome editing: A transdermal strategy of targeting NLRP3 by CRISPR-Cas9 for synergistic therapy of inflammatory skin disorders. Sci. Adv. 2021, 7, eabe2888. [Google Scholar] [CrossRef]
- Koller, U.; Bauer, J.W. Gene Replacement Therapies for Genodermatoses: A Status Quo. Front. Genet. 2021, 12, 658295. [Google Scholar] [CrossRef]
- Baker, C.; Hayden, M.S. Gene editing in dermatology: Harnessing CRISPR for the treatment of cutaneous disease. F1000Research 2020, 9, 281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rashidghamat, E.; Kadiyirire, T.; Ayis, S.; Petrof, G.; Liu, L.; Pullabhatla, V.; Ainali, C.; Guy, A.; Aristodemou, S.; McMillan, J.R.; et al. Phase I/II open-label trial of intravenous allogeneic mesenchymal stromal cell therapy in adults with recessive dystrophic epidermolysis bullosa. J. Am. Acad. Dermatol. 2020, 83, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Petrof, G.; Lwin, S.M.; Martinez-Queipo, M.; Abdul-Wahab, A.; Tso, S.; Mellerio, J.E.; Slaper-Cortenbach, I.; Boelens, J.J.; Tolar, J.; Veys, P.; et al. Potential of Systemic Allogeneic Mesenchymal Stromal Cell Therapy for Children with Recessive Dystrophic Epidermolysis Bullosa. J. Investig. Dermatol. 2015, 135, 2319–2321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Darouti, M.; Fawzy, M.; Amin, I.; Abdel Hay, R.; Hegazy, R.; Gabr, H.; El Maadawi, Z. Treatment of dystrophic epidermolysis bullosa with bone marrow non-hematopoeitic stem cells: A randomized controlled trial. Dermatol. Ther. 2016, 29, 96–100. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials.gov. A Study of PTR-01 in Recessive Dystrophic Epidermolysis Bullosa. 2020. Available online: https://clinicaltrials.gov/ct2/show/NCT04599881 (accessed on 18 June 2021).
- Sarkar, T.; Sarkar, S.; Gangopadhyay, D.N. Gene Therapy and its Application in Dermatology. Indian J. Dermatol. 2020, 65, 341–350. [Google Scholar] [CrossRef] [PubMed]
- Prodinger, C.M.; Reichelt, J.; Bauer, J.W.; Laimer, M. Current and Future Perspectives of Stem Cell Therapy in Dermatology. Ann. Dermatol. 2017, 29, 667–687. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Busch, K.H.; Bender, R.; Walezko, N.; Aziz, H.; Altintas, M.A.; Aust, M.C. Combination of medical needling and non-cultured autologous skin cell transplantation (ReNovaCell) for repigmentation of hypopigmented burn scars. Burns 2016, 42, 1556–1566. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cooper-Jones, B.; Visintini, S. A Noncultured Autologous Skin Cell Spray Graft for the Treatment of Burns. In CADTH Issues in Emerging Health Technologies; Canadian Agency for Drugs and Technologies in Health: Ottawa, ON, Canada, 2016; pp. 1–11. [Google Scholar]
- Shin, T.H.; Kim, H.S.; Choi, S.W.; Kang, K.S. Mesenchymal Stem Cell Therapy for Inflammatory Skin Diseases: Clinical Potential and Mode of Action. Int. J. Mol. Sci. 2017, 18, 244. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orr, R.M. Technology evaluation: Fomivirsen, Isis Pharmaceuticals Inc/CIBA vision. Curr. Opin. Mol. Ther. 2001, 3, 288–294. [Google Scholar] [PubMed]
- Hoy, S.M. Patisiran: First Global Approval. Drugs 2018, 78, 1625–1631. [Google Scholar] [CrossRef]
- Akinc, A.; Maier, M.A.; Manoharan, M.; Fitzgerald, K.; Jayaraman, M.; Barros, S.; Ansell, S.; Du, X.; Hope, M.J.; Madden, T.D.; et al. The Onpattro story and the clinical translation of nanomedicines containing nucleic acid-based drugs. Nat. Nanotechnol. 2019, 14, 1084–1087. [Google Scholar] [CrossRef] [PubMed]
- Xiong, H.; Veedu, R.N.; Diermeier, S.D. Recent advances in oligonucleotide therapeutics in oncology. Int. J. Mol. Sci. 2021, 22, 3295. [Google Scholar] [CrossRef] [PubMed]
- Leachman, S.A.; Hickerson, R.P.; Schwartz, M.E.; Bullough, E.E.; Hutcherson, S.L.; Boucher, K.M.; Hansen, C.D.; Eliason, M.J.; Srivatsa, G.S.; Kornbrust, D.J.; et al. First-in-human mutation-targeted siRNA phase Ib trial of an inherited skin disorder. Mol. Ther. 2010, 18, 442–446. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Kim, J.; Ahn, M.; Kim, J.; Heo, M.G.; Min, D.H.; Won, C. RNAi nanotherapy for fibrosis: Highly durable knockdown of CTGF/CCN-2 using siRNA-DegradaBALL (LEM-S401) to treat skin fibrotic diseases. Nanoscale 2020, 12, 6385–6393. [Google Scholar] [CrossRef] [PubMed]
- Gale, J.D.; Jensen, J.; Berman, G.; Freimuth, W.; Li, G.; Pleil, A.; Kutty, M.; Rosenthal, A.; Boswell, C.B.; Noah, V.; et al. A Placebo-controlled Study of PF-06473871 (Anti-Connective Tissue Growth Factor Antisense Oligonucleotide) in Reducing Hypertrophic Skin Scarring. Plast. Reconstr. Surg. Glob. Open 2018, 6, e1861. [Google Scholar] [CrossRef] [PubMed]
- Han-soo, L. Hugel Completes P1 Clinical Trial on Hypertrophic Scar Treatment. 2018. Available online: http://www.koreabiomed.com/news/articleView.html?idxno=3298 (accessed on 25 June 2021).
- Sirnaomics. Science. 2021. Available online: https://sirnaomics.com/science/ (accessed on 15 May 2021).
- Zuidam, J.V. Delving into RXi’s RNAi Delivery Platform. 2017. Available online: https://www.drugdiscoverytrends.com/delving-into-rxis-rnai-delivery-platform/#.Wg3exJa_LPE.twitter (accessed on 15 May 2021).
- National Institutes of Health—US National Library of Medicine. A Study to Evaluate the Effectiveness and Safety of RXI 109 on the Outcome of Revised Hypertrophic Scars. 2021. Available online: https://clinicaltrials.gov/ct2/show/NCT02246465 (accessed on 15 May 2021).
- Bae, C.J.; Lee, J.W.; Shim, S.B.; Jee, S.W.; Lee, S.H.; Woo, J.M.; Lee, C.K.; Hwang, D.Y. GATA binding protein 3 overexpression and suppression significantly contribute to the regulation of allergic skin inflammation. Int. J. Mol. Med. 2011, 28, 171–179. [Google Scholar]
- Zeitvogel, J.; Jokmin, N.; Rieker, S.; Klug, I.; Brandenberger, C.; Werfel, T. GATA3 regulates FLG and FLG2 expression in human primary keratinocytes. Sci. Rep. 2017, 7, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Sterna Biologicals. Pipeline Sterna Biologicals. 2021. Available online: https://www.sterna-biologicals.com/pipeline (accessed on 26 July 2021).
- Bremer, J.; Bornert, O.; Nyström, A.; Gostynski, A.; Jonkman, M.F.; Aartsma-Rus, A.; van den Akker, P.C.; Pasmooij, A.M. Antisense Oligonucleotide-mediated Exon Skipping as a Systemic Therapeutic Approach for Recessive Dystrophic Epidermolysis Bullosa. Mol. Ther. Nucleic Acids 2016, 5, e379. [Google Scholar] [CrossRef] [PubMed]
- Bornert, O.; Kühl, T.; Bremer, J.; Van Den Akker, P.C.; Pasmooij, A.M.G.; Nyström, A. Analysis of the functional consequences of targeted exon deletion in COL7A1 reveals prospects for dystrophic epidermolysis bullosa therapy. Mol. Ther. 2016, 24, 1302–1311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turczynski, S.; Titeux, M.; Tonasso, L.; Décha, A.; Ishida-Yamamoto, A.; Hovnanian, A. Targeted Exon Skipping Restores Type VII Collagen Expression and Anchoring Fibril Formation in an In Vivo RDEB Model. J. Investig. Dermatol. 2016, 136, 2387–2395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bornert, O.; Hogervorst, M.; Nauroy, P.; Bischof, J.; Swildens, J.; Athanasiou, I.; Tufa, S.F.; Keene, D.R.; Kiritsi, D.; Hainzl, S.; et al. QR-313, an Antisense Oligonucleotide, Shows Therapeutic Efficacy for Treatment of Dominant and Recessive Dystrophic Epidermolysis Bullosa: A Preclinical Study. J. Investig. Dermatol. 2021, 141, 883–893.e6. [Google Scholar] [CrossRef]
- Kim, S.T.; Lee, K.-M.; Park, H.-J.; Jin, S.-E.; Ahn, W.S.; Kim, C.-K. Topical delivery of interleukin-13 antisense oligonucleotides with cationic elastic liposome for the treatment of atopic dermatitis. J. Gene Med. 2009, 11, 26–37. [Google Scholar] [CrossRef] [PubMed]
- Exicure Inc. Annual Report on Form K-10; United States Securities and Exchange Commission: Washington, DC, USA, 2019. Available online: www.annualreports.com (accessed on 2 August 2021).
- Kapadia, C.H.; Melamed, J.R.; Day, E.S. Spherical Nucleic Acid Nanoparticles: Therapeutic Potential. BioDrugs 2018, 32, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Allergan Pays Exicure $25M to Discover Nucleic Acid Hair Loss Drugs. 2019. Available online: https://www.fiercebiotech.com/biotech/allergan-pays-exicure-25m-to-discover-nucleic-acid-hair-loss-drugs (accessed on 12 August 2021).
- ClinicalTrials.gov. Oblimersen and Dacarbazine in Treating Patients with Advanced Malignant Melanoma That Has Responded to Treatment on Clinical Trial GENTA-GM301. 2003. Available online: https://clinicaltrials.gov/ct2/show/NCT00070343 (accessed on 2 August 2021).
- Hong, C.A.; Nam, Y.S. Functional nanostructures for effective delivery of small interfering RNA therapeutics. Theranostics 2014, 4, 1211–1232. [Google Scholar] [CrossRef]
- Wang, D.; Tai, P.W.L.; Gao, G. Adeno-associated virus vector as a platform for gene therapy delivery. Nat. Rev. Drug Discov. 2019, 18, 358–378. [Google Scholar] [CrossRef] [PubMed]
- Sung, Y.K.; Kim, S.W. Recent advances in the development of gene delivery systems. Biomater. Res. 2019, 23, 8. [Google Scholar] [CrossRef] [PubMed]
- Lundstrom, K. Viral Vectors in Gene Therapy. Diseases 2018, 6, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chamorro, C.; Mencía, A.; Almarza, D.; Duarte, B.; Büning, H.; Sallach, J.; Hausser, I.; Del Río, M.; Larcher, F.; Murillas, R. Gene Editing for the Efficient Correction of a Recurrent COL7A1 Mutation in Recessive Dystrophic Epidermolysis Bullosa Keratinocytes. Mol. Ther. Nucleic Acids 2016, 5, e307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colella, P.; Ronzitti, G.; Mingozzi, F. Emerging Issues in AAV-Mediated In Vivo Gene Therapy. Mol. Ther. Methods Clin. Dev. 2018, 8, 87–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verdera, H.C.; Kuranda, K.; Mingozzi, F. AAV Vector Immunogenicity in Humans: A Long Journey to Successful Gene Transfer. Mol. Ther. 2020, 28, 723–746. [Google Scholar] [CrossRef] [PubMed]
- Mandal, A.; Kumbhojkar, N.; Reilly, C.; Dharamdasani, V.; Ukidve, A.; Ingber, D.E.; Mitragotri, S. Treatment of psoriasis with NFKBIZ siRNA using topical ionic liquid formulations. Sci. Adv. 2020, 6. [Google Scholar] [CrossRef]
- Ball, R.L.; Bajaj, P.; Whitehead, K.A. Oral delivery of siRNA lipid nanoparticles: Fate in the GI tract. Sci. Rep. 2018, 8, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Lin, P.Y.; Chiu, Y.L.; Huang, J.H.; Chuang, E.Y.; Mi, F.L.; Lin, K.J.; Juang, J.H.; Sung, H.W.; Leong, K.W. Oral Nonviral Gene Delivery for Chronic Protein Replacement Therapy. Adv. Sci. 2018, 5, 1701079. [Google Scholar] [CrossRef]
- Forbes, D.C.; Peppas, N.A. Oral delivery of small RNA and DNA. J. Control. Release 2012, 162, 438–445. [Google Scholar] [CrossRef]
- enGene. Pioneering Oral Delivery for Gene Therapy; Nature Research Custom Media: London, UK, 2021. [Google Scholar]
- Gennemark, P.; Walter, K.; Clemmensen, N.; Rekić, D.; Nilsson, C.A.M.; Knöchel, J.; Hölttä, M.; Wernevik, L.; Rosengren, B.; Kakol-Palm, D.; et al. An oral antisense oligonucleotide for PCSK9 inhibition. Sci. Transl. Med. 2021, 13, eabe9117. [Google Scholar] [CrossRef]
- Bhavsar, M.D.; Amiji, M.M. Gastrointestinal distribution and in vivo gene transfection studies with nanoparticles-in-microsphere oral system (NiMOS). J. Control. Release 2007, 119, 339–348. [Google Scholar] [CrossRef]
- Zakrewsky, M.; Kumar, S.; Mitragotri, S. Nucleic acid delivery into skin for the treatment of skin disease: Proofs-of-concept, potential impact, and remaining challenges. J. Control. Release 2015, 219, 445–456. [Google Scholar] [CrossRef] [Green Version]
- Dokka, S.; Cooper, S.R.; Kelly, S.; Hardee, G.E.; Karras, J.G. Dermal delivery of topically applied oligonucleotides via follicular transport in mouse skin. J. Investig. Dermatol. 2005, 124, 971–975. [Google Scholar] [CrossRef] [Green Version]
- Zheng, D.; Giljohann, D.A.; Chen, D.L.; Massich, M.D.; Wang, X.-Q.; Iordanov, H.; Mirkin, C.A.; Paller, A.S. Topical delivery of siRNA-based spherical nucleic acid nanoparticle conjugates for gene regulation. Proc. Natl. Acad. Sci. USA 2012, 109, 11975–11980. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, D.; Zhao, D.; Wang, X.; Li, C.; Yang, T.; Du, L.; Wei, Z.; Cheng, Q.; Cao, H.; Liang, Z.; et al. Efficient delivery of nucleic acid molecules into skin by combined use of microneedle roller and flexible interdigitated electroporation array. Theranostics 2018, 8, 2361–2376. [Google Scholar] [CrossRef]
- Dul, M.; Stefanidou, M.; Porta, P.; Serve, J.; O’Mahony, C.; Malissen, B.; Henri, S.; Levin, Y.; Kochba, E.; Wong, F.S.; et al. Hydrodynamic gene delivery in human skin using a hollow microneedle device. J. Control. Release 2017, 265, 120–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brownstone, N.D.; Hong, J.; Mosca, M.; Hadeler, E.; Liao, W.; Bhutani, T.; Koo, J. Biologic Treatments of Psoriasis: An Update for the Clinician. Biologics 2021, 15, 39–51. [Google Scholar]
- Harrison, G.A. Insulin in alcoholic solution by the mouth. Br. Med. J. 1923, 2, 1204–1205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- New, R. Oral Delivery of Biologics via the Intestine. Pharmaceutics 2020, 13, 18. [Google Scholar] [CrossRef]
- Tuvia, S.; Atsmon, J.; Teichman, S.L.; Katz, S.; Salama, P.; Pelled, D.; Landau, I.; Karmeli, I.; Bidlingmaier, M.; Strasburger, C.J.; et al. Oral Octreotide Absorption in Human Subjects: Comparable Pharmacokinetics to Parenteral Octreotide and Effective Growth Hormone Suppression. J. Clin. Endocrinol. Metab. 2012, 97, 2362–2369. [Google Scholar] [CrossRef] [Green Version]
- Overgaard, R.V.; Navarria, A.; Ingwersen, S.H.; Bækdal, T.A.; Kildemoes, R.J. Clinical Pharmacokinetics of Oral Semaglutide: Analyses of Data from Clinical Pharmacology Trials. Clin. Pharmacokinet. 2021, 60, 1335–1348. [Google Scholar] [CrossRef] [PubMed]
- Buckley, S.T.; Bækdal, T.A.; Vegge, A.; Maarbjerg, S.J.; Pyke, C.; Ahnfelt-Rønne, J.; Madsen, K.G.; Schéele, S.G.; Alanentalo, T.; Kirk, R.K.; et al. Transcellular stomach absorption of a derivatized glucagon-like peptide-1 receptor agonist. Sci. Transl. Med. 2018, 10, eaar7047. [Google Scholar] [CrossRef] [PubMed]
- Maher, S.; Brayden, D.J.; Casettari, L.; Illum, L. Application of Permeation Enhancers in Oral Delivery of Macromolecules: An Update. Pharmaceutics 2019, 11, 41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Twarog, C.; Fattah, S.; Heade, J.; Maher, S.; Fattal, E.; Brayden, D.J. Intestinal Permeation Enhancers for Oral Delivery of Macromolecules: A Comparison between Salcaprozate Sodium (SNAC) and Sodium Caprate (C(10)). Pharmaceutics 2019, 11, 78. [Google Scholar] [CrossRef] [Green Version]
- Tuvia, S.; Pelled, D.; Marom, K.; Salama, P.; Levin-Arama, M.; Karmeli, I.; Idelson, G.H.; Landau, I.; Mamluk, R. A Novel Suspension Formulation Enhances Intestinal Absorption of Macromolecules Via Transient and Reversible Transport Mechanisms. Pharm. Res. 2014, 31, 2010–2021. [Google Scholar] [CrossRef] [Green Version]
- Salama, P.; Mamluk, R.; Marom, K.; Weinstein, I.; Tzabari, M. Chiasma, Inc. Pharmaceutical Compositions and Related Methods of Delivery. U.S. Patent 8,535,695, 17 September 2013. [Google Scholar]
- Maher, S.; Leonard, T.W.; Jacobsen, J.; Brayden, D.J. Safety and efficacy of sodium caprate in promoting oral drug absorption: From in vitro to the clinic. Adv. Drug Deliv. Rev. 2009, 61, 1427–1449. [Google Scholar] [CrossRef]
- Leonard, T.W.; Lynch, J.; McKenna, M.J.; Brayden, D.J. Promoting absorption of drugs in humans using medium-chain fatty acid-based solid dosage forms: GIPET. Expert. Opin. Drug Deliv. 2006, 3, 685–692. [Google Scholar] [CrossRef]
- Halberg, I.B.; Lyby, K.; Wassermann, K.; Heise, T.; Plum-Mörschel, L.; Zijlstra, E. The Effect of Food Intake on the Pharmacokinetics of Oral Basal Insulin: A Randomised Crossover Trial in Healthy Male Subjects. Clin. Pharm. 2019, 58, 1497–1504. [Google Scholar] [CrossRef] [Green Version]
- Brayden, D.J.; Hill, T.A.; Fairlie, D.P.; Maher, S.; Mrsny, R.J. Systemic delivery of peptides by the oral route: Formulation and medicinal chemistry approaches. Adv. Drug Deliv. Rev. 2020, 157, 2–36. [Google Scholar] [CrossRef]
- Banerjee, A.; Ibsen, K.; Brown, T.; Chen, R.; Agatemor, C.; Mitragotri, S. Ionic liquids for oral insulin delivery. Proc. Natl. Acad. Sci. USA 2018, 115, 7296–7301. [Google Scholar] [CrossRef] [Green Version]
- Mitragotri, S.; Banerjee, A.; Brown, T.; Ibsen, K.; Agatemor, C. Ionic Liquids For Internal Delivery. U.S. Patent 16,762,361, 16 November 2018. [Google Scholar]
- Tillman, L.G.; Geary, R.S.; Hardee, G.E. Oral delivery of antisense oligonucleotides in man. J. Pharm. Sci. 2008, 97, 225–236. [Google Scholar] [CrossRef]
- Ionis. Ionis Highlights Achievements, Commercial Strategy and Technology Advancements at Investor Day. 2020. Available online: www.ionispharma.com (accessed on 7 July 2021).
- Taylor, N.P. Ionis Taps Progenity to Create Oral Antisense Therapies. 2021. Available online: https://www.fiercepharma.com/drug-delivery/ionis-taps-progenity-to-create-oral-antisense-therapies (accessed on 7 July 2021).
- Hyun, E.J.; Hasan, M.N.; Kang, S.H.; Cho, S.; Lee, Y.K. Oral siRNA delivery using dual transporting systems to efficiently treat colorectal liver metastasis. Int. J. Pharm. 2019, 555, 250–258. [Google Scholar] [CrossRef]
- O’Driscoll, C.M.; Bernkop-Schnürch, A.; Friedl, J.D.; Préat, V.; Jannin, V. Oral delivery of non-viral nucleic acid-based therapeutics—Do we have the guts for this? Eur. J. Pharm. Sci. 2019, 133, 190–204. [Google Scholar] [CrossRef] [PubMed]
- Alnylam Pharmaceuticals. Alnylam Announces Progress with RNAi Therapeutics Platform, Including Oral Route of Administration and CNS and Ocular Delivery. 2019. Available online: https://www.biospace.com/article/releases/alnylam-announces-progress-with-rnai-therapeutics-platform-including-oral-route-of-administration-and-cns-and-ocular-delivery-/ (accessed on 16 May 2021).
- DNAlite. Gatrointestinal Gene Therapy Create Better Biological Medicines. 2021. Available online: https://www.dnalite.com/ (accessed on 27 July 2021).
- Granhall, C.; Donsmark, M.; Blicher, T.M.; Golor, G.; Søndergaard, F.L.; Thomsen, M.; Bækdal, T.A. Safety and Pharmacokinetics of Single and Multiple Ascending Doses of the Novel Oral Human GLP-1 Analogue, Oral Semaglutide, in Healthy Subjects and Subjects with Type 2 Diabetes. Clin. Pharmacokinet. 2019, 58, 781–791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hellriegel, E.T.; Bjornsson, T.D.; Hauck, W.W. Interpatient variability in bioavailability is related to the extent of absorption: Implications for bioavailability and bioequivalence studies. Clin. Pharmacol. Ther. 1996, 60, 601–607. [Google Scholar] [CrossRef]
- Halberg, I.B.; Lyby, K.; Wassermann, K.; Heise, T.; Zijlstra, E.; Plum-Morschel, L. Efficacy and safety of oral basal insulin versus subcutaneous insulin glargine in type 2 diabetes: A randomised, double-blind, phase 2 trial. Lancet Diabetes Endocrinol. 2019, 7, 179–188. [Google Scholar] [CrossRef]
- Moroz, E.; Matoori, S.; Leroux, J.C. Oral delivery of macromolecular drugs: Where we are after almost 100years of attempts. Adv. Drug Deliv. Rev. 2016, 101, 108–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caffarel-Salvador, E.; Abramson, A.; Langer, R.; Traverso, G. Oral delivery of biologics using drug-device combinations. Curr. Opin. Pharm. 2017, 36, 8–13. [Google Scholar] [CrossRef]
- Imran, M.; Rani Therapeutics LLC. Therapeutic Agent Preparations Comprising Liraglutide for Delivery into a Lumen of the Intestinal Tract Using a Swallowable Drug Delivery Device. U.S. Patent 8,809,271, 19 August 2014. [Google Scholar]
- Dhalla, A.K.; Al-Shamsie, Z.; Beraki, S.; Dasari, A.; Fung, L.C.; Fusaro, L.; Garapaty, A.; Gutierrez, B.; Gratta, D.; Hashim, M.; et al. A robotic pill for oral delivery of biotherapeutics: Safety, tolerability, and performance in healthy subjects. Drug Deliv. Transl. Res. 2021, 1–12. [Google Scholar]
- Abramson, A.; Caffarel-Salvador, E.; Khang, M.; Dellal, D.; Silverstein, D.; Gao, Y.; Frederiksen, M.R.; Vegge, A.; Hubálek, F.; Water, J.J.; et al. An ingestible self-orienting system for oral delivery of macromolecules. Science 2019, 363, 611–615. [Google Scholar] [CrossRef] [Green Version]
- Abramson, A.; Caffarel-Salvador, E.; Soares, V.; Minahan, D.; Tian, R.Y.; Lu, X.; Dellal, D.; Gao, Y.; Kim, S.; Wainer, J.; et al. A luminal unfolding microneedle injector for oral delivery of macromolecules. Nat. Med. 2019, 25, 1512–1518. [Google Scholar] [CrossRef]
- Babaee, S.; Pajovic, S.; Kirtane, A.R.; Shi, J.; Caffarel-Salvador, E.; Hess, K.; Collins, J.E.; Tamang, S.; Wahane, A.V.; Hayward, A.M.; et al. Temperature-responsive biometamaterials for gastrointestinal applications. Sci. Transl. Med. 2019, 11, eaau8581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biograil. Available online: https://biograil.com/ (accessed on 16 August 2021).
- Progenity™. Oral Biotherapeutics Drug-Device Combinations Using Progenity’s Novel Drug Delivery System (in Development). 2021. Available online: https://www.progenity.com/innovation/oral-biotherapeutics (accessed on 28 July 2021).
- Baywind Bioventures. Propel Biologics™ JetCAP™. 2021. Available online: http://baywindbio.com/jetcap/ (accessed on 28 July 2021).
- Rhodes, C.; Casillas, J.; Baywind Bioventures. Capsule Device for Delivery of Active Agent to Gastrointestinal Tract. U.S. Patent 62/722,083, 23 August 2018. [Google Scholar]
- Aran, K.; Chooljian, M.; Paredes, J.; Rafi, M.; Lee, K.; Kim, A.Y.; An, J.; Yau, J.F.; Chum, H.; Conboy, I.; et al. An oral microjet vaccination system elicits antibody production in rabbits. Sci. Transl. Med. 2017, 9, eaaf6413. [Google Scholar] [CrossRef]
- Artmonov, V.; Yanovitska, J.; Hashimshony, D.; Cohen, J. The development of intestinal mucoadhesive layers for a novel device for oral delivery of macromolecules through the intestinal wall. Pharmaceutics 2021, 13. under review. [Google Scholar]
- Abramson, A.; Frederiksen, M.R.; Vegge, A.; Jensen, B.; Poulsen, M.; Mouridsen, B.; Jespersen, M.O.; Kirk, R.K.; Windum, J.; Hubalek, F.; et al. Oral delivery of systemic monoclonal antibodies, peptides and small molecules using gastric auto-injectors. Nat. Biotechnol. 2021, 1–7. [Google Scholar] [CrossRef]
- Pillai, O.; Kumar, N.; Dey, C.S.; Borkute, S.; Nagalingam, S.; Panchagnula, R. Transdermal iontophoresis of insulin. Part 1: A study on the issues associated with the use of platinum electrodes on rat skin. J Pharm. Pharmacol. 2003, 55, 1505–1513. [Google Scholar] [CrossRef]
- France, M.M.; Del Rio, T.; Travers, H.; Raftery, E.; Xu, K.; Langer, R.; Traverso, G.; Lennerz, J.K.; Schoellhammer, C.M. Ultra-rapid drug delivery in the oral cavity using ultrasound. J. Control. Release 2019, 304, 1–6. [Google Scholar] [CrossRef]
- Caffarel-Salvador, E.; Kim, S.; Soares, V.; Tian, R.Y.; Stern, S.R.; Minahan, D.; Yona, R.; Lu, X.; Zakaria, F.R.; Collins, J.; et al. A microneedle platform for buccal macromolecule delivery. Sci. Adv. 2021, 7, eabe2620. [Google Scholar] [CrossRef]
- Banerjee, A.; Wong, J.; Gogoi, R.; Brown, T.; Mitragotri, S. Intestinal micropatches for oral insulin delivery. J. Drug Target. 2017, 25, 608–615. [Google Scholar] [CrossRef]
- Banerjee, A.; Chen, R.; Arafin, S.; Mitragotri, S. Intestinal iontophoresis from mucoadhesive patches: A strategy for oral delivery. J. Control. Release 2019, 297, 71–78. [Google Scholar] [CrossRef]
- Nemeth, C.L.; Lykins, W.R.; Tran, H.; ElSayed, M.E.H.; Desai, T.A. Bottom-Up Fabrication of Multilayer Enteric Devices for the Oral Delivery of Peptides. Pharm. Res. 2019, 36, 89. [Google Scholar] [CrossRef]
- Fox, C.B.; Cao, Y.; Nemeth, C.L.; Chirra, H.D.; Chevalier, R.W.; Xu, A.M.; Melosh, N.A.; Desai, T.A. Fabrication of Sealed Nanostraw Microdevices for Oral Drug Delivery. ACS Nano 2016, 10, 5873–5881. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jørgensen, J.R.; Jepsen, M.L.; Nielsen, L.H.; Dufva, M.; Nielsen, H.M.; Rades, T.; Boisen, A.; Müllertz, A. Microcontainers for oral insulin delivery—In vitro studies of permeation enhancement. Eur. J. Pharm. Biopharm. 2019, 143, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Kong, Y.L.; Zou, X.; McCandler, C.A.; Kirtane, A.R.; Ning, S.; Zhou, J.; Abid, A.; Jafari, M.; Rogner, J.; Minahan, D.; et al. 3D-Printed Gastric Resident Electronics. Adv. Mater. Technol. 2019, 4, 1800490. [Google Scholar] [CrossRef] [Green Version]
- Van der Schaar, P.J.; Dijksman, J.F.; Broekhuizen-de Gast, H.; Shimizu, J.; van Lelyveld, N.; Zou, H.; Iordanov, V.; Wanke, C.; Siersema, P.D. A novel ingestible electronic drug delivery and monitoring device. Gastrointest. Endosc. 2013, 78, 520–528. [Google Scholar] [CrossRef] [PubMed]
- Becker, D.; Zhang, J.; Heimbach, T.; Penland, R.C.; Wanke, C.; Shimizu, J.; Kulmatycki, K. Novel orally swallowable IntelliCap® device to quantify regional drug absorption in human GI tract using diltiazem as model drug. AAPS PharmSciTech 2014, 15, 1490–1497. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Skin Disease | Clinical Trial | Phase | Company | Biological | Administration Route | Treatment | Estimated Completion Date |
|---|---|---|---|---|---|---|---|
| Ex vivoapproaches | |||||||
| Netherton’s syndrome | NCT01545323 | I | Great Ormond Street Hospital for Children NHS Foundation Trust | N/A | Skin graft | Autologous epidermal sheet graft from ex vivo SPINK5 gene-corrected keratinocyte stem cells using a lentiviral vector | April 2018 |
| JEB | NCT03490331/2016-000095-17 | I/II | Holostem Terapie Avanzate | N/A | Skin graft | Autologous cultured epidermal grafts genetically corrected with gamma-retroviral vectors carrying COL17A1 | December 2021 |
| RDEB | NCT02984085 | I/II | Holostem Terapie Avanzate | N/A | Skin graft | Autologous cultured epidermal grafts genetically corrected with gamma-retroviral vectors carrying COL7A1 | December 2020 |
| RDEB | NCT02493816/2014-004884-19 | I | King’s College London | N/A | Skin graft | Intradermal injection of SIN lentiviral virus-mediated COL7A1 gene-modified autologous fibroblasts in adults | March 2018 |
| RDEB | 2016-002790-35 | I/II | INSERM | N/A | Skin graft | Autologous skin equivalent grafts genetically corrected with a COL7A1-encoding SIN retroviral vector | Unknown |
| RDEB | NCT04186650 | I/II | Institut National de la Santé et de la Recherche Médicale | N/A | Skin graft | Autologous skin equivalent grafts genetically corrected with a COL7A1-encoding SIN retroviral vector | September 2021 |
| RDEB | NCT01263379 | I/II | Stanford University (with NIAMS and Abeona Therapeutics) | LZRSE | Skin graft | COL7A1 engineered autologous epidermal sheets transfected ex vivo using a retrovirus | December 2025 |
| RDEB | NCT02810951 | I/II | Castle Creek Pharmaceutical | FCX-007 | Intradermal injection | Genetically modified autologous fibroblasts to produce type VII collagen | December 2033 |
| RDEB | NCT04213261 | III | Castle Creek Pharmaceutical | FCX-007 | Intradermal injection | Genetically modified autologous fibroblasts to produce type VII collagen | December 2036 |
| RDEB | NCT04227106 | III | Abeona Therapeutics | EB-101 | Skin graft | Autologous RDEB keratinocytes isolated from skin biopsies and transduced with a recombinant retrovirus containing COL7A1 | April 2022 |
| In vivoapproaches | |||||||
| ARCI | NCT04047732 | I/II | Krystal Biotech | KB105 | Topical | Replication-defective, non-integrating HSV-1 expressing human transglutaminase 1 | March 2025 |
| DEB | NCT03536143 | II | Krystal Biotech | B-VEC (previously KB103) | Topical | Replication-defective, non-integrating HSV-1 expressing human type VIII collagen | March 2024 |
| DEB | NCT04491604 | III | Krystal Biotech | B-VEC (previously KB103) | Topical | Replication-defective, non-integrating HSV-1 expressing human type VII collagen | August 2021 |
| Hypertrophic scar | NCT04540900 | I | Krystal Biotech | KB301 | Intradermal injection | Replication-defective, non-integrating HSV-1 expressing human type III collagen | January 2022 |
| Skin Disease | Clinical Trial | Phase | Company | Biological | Administration Route | Treatment | Estimated Completion Date |
|---|---|---|---|---|---|---|---|
| AD | NCT02079688 | II | Sterna Biologicals GmbH & Co. KG | SB011 | Topical | DNAzyme hgd40 targeting GATA3, a highly mutated transcription factor | January 2017 |
| DEB | NCT03605069 | I/II | Wings Therapeutics | QR-313 | Topical | 21-nucleotide ASO designed to hybridize to a specific sequence in the COL7A1 pre-messenger RNA | September 2020 |
| Hypertrophic scar | NCT02956317 | I/II | Sirnaomics | STP705 | Intradermal injection | Two siRNA oligonucleotides, targeting TGF-β1 and Cox-2 mRNA, respectively, formulated in nanoparticles | January 2018 |
| Hypertrophic scar | NCT02205476 | II | Pfizer | PF-06473871 | Intradermal injection | Anti-CTGF antisense oligonucleotide | January 2015 |
| Hypertrophic scar | NCT02030275/NCT02246465 | II | RXi Pharmaceuticals | RXI-109 | Intradermal injection | Self-delivering RNAi compound targeting CTGF | June 2016 |
| Hypertrophic scar | NCT04012099 | II | Hugel | BMT101 | Intradermal injection | Cell penetrating asymmetric siRNA targeting human CTGF | August 2022 |
| Hypertrophic scar | NCT04877756 | II | Olix Pharmaceuticals | OLX10010 | Intradermal injection | Cell penetrating asymmetric siRNA targeting human CTGF | March 2023 |
| PC | NCT00716014 | I | Pachyonychia Congenita Project | TD101 | Intralesional injection | siRNA designed to target a mutation of the PC keratin K6a | August 2008 |
| Psoriasis | Unknown | I | Purdue Pharma, Exicure | AST-005 | Topical | Nanoparticle-based SNA to knockdown a tumor necrosis factor gene | August 2016 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Søgaard, P.P.; Lind, M.; Christiansen, C.R.; Petersson, K.; Clauss, A.; Caffarel-Salvador, E. Future Perspectives of Oral Delivery of Next Generation Therapies for Treatment of Skin Diseases. Pharmaceutics 2021, 13, 1722. https://doi.org/10.3390/pharmaceutics13101722
Søgaard PP, Lind M, Christiansen CR, Petersson K, Clauss A, Caffarel-Salvador E. Future Perspectives of Oral Delivery of Next Generation Therapies for Treatment of Skin Diseases. Pharmaceutics. 2021; 13(10):1722. https://doi.org/10.3390/pharmaceutics13101722
Chicago/Turabian StyleSøgaard, Pia Pernille, Marianne Lind, Chatpakorn Rassemeena Christiansen, Karsten Petersson, Adam Clauss, and Ester Caffarel-Salvador. 2021. "Future Perspectives of Oral Delivery of Next Generation Therapies for Treatment of Skin Diseases" Pharmaceutics 13, no. 10: 1722. https://doi.org/10.3390/pharmaceutics13101722
APA StyleSøgaard, P. P., Lind, M., Christiansen, C. R., Petersson, K., Clauss, A., & Caffarel-Salvador, E. (2021). Future Perspectives of Oral Delivery of Next Generation Therapies for Treatment of Skin Diseases. Pharmaceutics, 13(10), 1722. https://doi.org/10.3390/pharmaceutics13101722