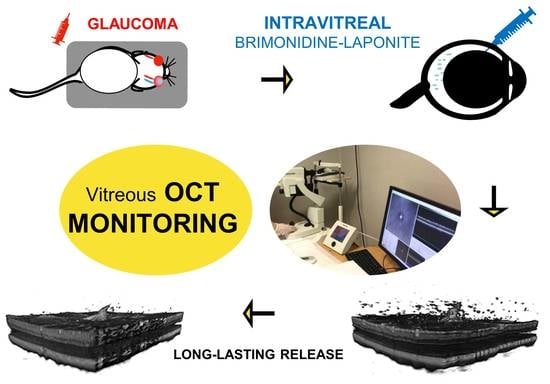
Monitoring New Long-Lasting Intravitreal Formulation for Glaucoma with Vitreous Images Using Optical Coherence Tomography
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Optical Coherence Tomography
2.3. Brimonidine–Laponite (BRI/LAP) Formulation and Analysis
2.4. In Vitro Release of BRI from BRI/LAP Formulation
2.5. Analysis of the Intravitreal Formulation Using OCT
2.6. Statistical Analysis
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Walters, T.R. Development and use of brimonidine in treating acute and chronic elevations of intraocular pressure: A review of safety, efficacy, dose response, and dosing studies. Surv. Ophthalmol. 1996, 41, S19–S26. [Google Scholar] [CrossRef]
- Nizari, S.; Guo, L.; Davis, B.M.; Normando, E.M.; Galvao, J.; Turner, L.; Bizrah, M.; Dehabadi, M.; Tian, K.; Cordeiro, M.F. Non-amyloidogenic effects of α2 adrenergic agonists: Implications for brimonidine-mediated neuroprotection. Cell Death Dis. 2016, 7, e2514. [Google Scholar] [CrossRef] [Green Version]
- Simó, R.; Hernández, C.; Porta, M.; Bandello, F.; Grauslund, J.; Harding, S.P.; Aldington, S.J.; Egan, C.; Frydkjaer-Olsen, U.; García-Arumí, J.; et al. Effects of Topically Administered Neuroprotective Drugs in Early Stages of Diabetic Retinopathy: Results of the EUROCONDOR Clinical Trial. Diabetes 2019, 68, 457–463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, K.E.; Jang, I.; Moon, H.; Kim, Y.J.; Jeoung, J.W.; Park, K.H.; Kim, H. Neuroprotective Effects of Human Serum Albumin Nanoparticles Loaded With Brimonidine on Retinal Ganglion Cells in Optic Nerve Crush Model. Investig. Opthalmol. Vis. Sci. 2015, 56, 5641. [Google Scholar] [CrossRef] [Green Version]
- Dossarps, D.; Bron, A.M.; Koehrer, P.; Aho-Glélé, L.S.; Creuzot-Garcher, C.; Berthon, L.; Maftouhi, Q.-E.; Bakhti, A.; Conrath, J.; Le Mer, Y.; et al. Endophthalmitis After Intravitreal Injections: Incidence, Presentation, Management, and Visual Outcome. Am. J. Ophthalmol. 2015, 160, 17–25.e1. [Google Scholar] [CrossRef]
- Tomás, H.; Alves, C.S.; Rodrigues, J. Laponite®: A key nanoplatform for biomedical applications? Nanomed. Nanotechnol. Biol. Med. 2018, 14, 2407–2420. [Google Scholar] [CrossRef]
- Prieto, E.; Vispe, E.; De Martino, A.; Idoipe, M.; Rodrigo, M.J.; Garcia-Martin, E.; Fraile, J.M.; Polo-Llorens, V.; Mayoral, J.A. Safety study of intravitreal and suprachoroidal Laponite clay in rabbit eyes. Graefe’s Arch. Clin. Exp. Ophthalmol. 2018, 256, 535–546. [Google Scholar] [CrossRef]
- Prieto, E.; Cardiel, M.J.; Vispe, E.; Idoipe, M.; Garcia-Martin, E.; Fraile, J.M.; Polo, V.; Mayoral, J.A.; Pablo, L.E.; Rodrigo, M.J. Dexamethasone delivery to the ocular posterior segment by sustained-release Laponite formulation. Biomed. Mater. 2020, 15, 065021. [Google Scholar] [CrossRef] [PubMed]
- Rodrigo, M.J.; Cardiel, M.J.; Fraile, J.M.; Mendez-Martinez, S.; Martinez-Rincon, T.; Subías, M.; Polo, V.; Ruberte, J.; Ramirez, T.; Vispe, E.; et al. Brimonidine-LAPONITE® intravitreal formulation has an ocular hypotensive and neuroprotective effect throughout 6 months of follow-up in a glaucoma animal model. Biomater. Sci. 2020, 8, 6246–6260. [Google Scholar] [CrossRef] [PubMed]
- Lapasin, R.; Abrami, M.; Grassi, G.; Šebenik, U. Rheology of Laponite-scleroglucan hydrogels. Carbohydr. Polym. 2017, 168, 290–300. [Google Scholar] [CrossRef] [PubMed]
- Holekamp, N.M. The Vitreous Gel: More than Meets the Eye. Am. J. Ophthalmol. 2010, 149, 32–36.e1. [Google Scholar] [CrossRef]
- Margolis, R. Diagnostic vitrectomy for the diagnosis and management of posterior uveitis of unknown etiology. Curr. Opin. Ophthalmol. 2008, 19, 218–224. [Google Scholar] [CrossRef]
- Bévalot, F.; Cartiser, N.; Bottinelli, C.; Fanton, L.; Guitton, J. Vitreous humor analysis for the detection of xenobiotics in forensic toxicology: A review. Forensic Toxicol. 2016, 34, 12–40. [Google Scholar] [CrossRef] [Green Version]
- Del Amo, E.M.; Rimpelä, A.-K.; Heikkinen, E.; Kari, O.K.; Ramsay, E.; Lajunen, T.; Schmitt, M.; Pelkonen, L.; Bhattacharya, M.; Richardson, D.; et al. Pharmacokinetic aspects of retinal drug delivery. Prog. Retin. Eye Res. 2017, 57, 134–185. [Google Scholar] [CrossRef]
- Uji, A.; Yoshimura, N. Microarchitecture of the Vitreous Body: A High-Resolution Optical Coherence Tomography Study. Am. J. Ophthalmol. 2016, 168, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Keane, P.A.; Karampelas, M.; Sim, D.A.; Sadda, S.R.; Tufail, A.; Sen, H.N.; Nussenblatt, R.B.; Dick, A.D.; Lee, R.W.; Murray, P.I.; et al. Objective Measurement of Vitreous Inflammation Using Optical Coherence Tomography. Ophthalmology 2014, 121, 1706–1714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sreekantam, S.; Macdonald, T.; Keane, P.; Sim, D.; Murray, P.; Denniston, A.K. Quantitative analysis of vitreous inflammation using optical coherence tomography in patients receiving sub-Tenon’s triamcinolone acetonide for uveitic cystoid macular oedema. Br. J. Ophthalmol. 2016, 101, 175–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernández-Ferreiro, A.; Luaces-Rodríguez, A.; Aguiar, P.; Pardo-Montero, J.; González-Barcia, M.; García-Varela, L.; Herranz, M.; Silva-Rodríguez, J.; Gil-Martínez, M.; Bermudez, M.; et al. Preclinical PET Study of Intravitreal Injections. Investig. Ophthalmol. Vis. Sci. 2017, 58, 2843–2851. [Google Scholar]
- Li, S.K.; Lizak, M.J.; Jeong, E.-K. MRI in ocular drug delivery. NMR Biomed. 2008, 21, 941–956. [Google Scholar] [CrossRef]
- Morrison, J.C.; Cepurna, W.O.; Johnson, E.C. Modeling glaucoma in rats by sclerosing aqueous outflow pathways to elevate intraocular pressure. Exp. Eye Res. 2015, 141, 23–32. [Google Scholar] [CrossRef] [Green Version]
- Chu, C.J.; Herrmann, P.; Carvalho, L.S.; Liyanage, S.E.; Bainbridge, J.W.B.; Ali, R.R.; Dick, A.D.; Luhmann, U.F. Assessment and In Vivo Scoring of Murine Experimental Autoimmune Uveoretinitis Using Optical Coherence Tomography. PLoS ONE 2013, 8, e63002. [Google Scholar] [CrossRef] [Green Version]
- Liba, O.; Lew, M.D.; SoRelle, E.D.; Dutta, R.; Sen, D.; Moshfeghi, D.M.; Chu, S.; De La Zerda, A. Speckle-modulating optical coherence tomography in living mice and humans. Nat. Commun. 2017, 8, 15845. [Google Scholar] [CrossRef] [Green Version]
- Fraile, J.M.; Garcia-Martin, E.; Gil, C.; Mayoral, J.A.; Pablo, L.; Polo-Llorens, V.; Prieto, E.; Vispe, E. Laponite as carrier for controlled in vitro delivery of dexamethasone in vitreous humor models. Eur. J. Pharm. Biopharm. 2016, 108, 83–90. [Google Scholar] [CrossRef] [Green Version]
- Kalapesi, F.B.; Coroneo, M.T.; Hill, M.A. Human ganglion cells express the alpha-2 adrenergic receptor: Relevance to neuroprotection. Br. J. Ophthalmol. 2005, 89, 758–763. [Google Scholar] [CrossRef] [Green Version]
- Lambert, W.S.; Carlson, B.J.; Van Der Ende, A.E.; Shih, G.; Dobish, J.N.; Calkins, D.J.; Harth, E. Nanosponge-Mediated Drug Delivery Lowers Intraocular Pressure. Transl. Vis. Sci. Technol. 2015, 4, 1. [Google Scholar] [CrossRef]
- Kuppermann, B.D.; Patel, S.S.; Boyer, D.S.; Augustin, A.J.; Freeman, W.R.; Kerr, K.J.; Guo, Q.; Schneider, S.; López, F.J. Phase 2 Study of the Safety and Efficacy of Brimonidine Drug Delivery System (Brimo Dds) Generation 1 in Patients with Geographic Atrophy Secondary to Age-Related Macular Degeneration. Retina 2021, 41, 144–155. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Mariscal, M.; Puerto, B.; Muñoz-Negrete, F.J.; De Juan, V.; Rebolleda, G. Acute and chronic optic nerve head biomechanics and intraocular pressure changes in patients receiving multiple intravitreal injections of anti-VEGF. Graefe’s Arch. Clin. Exp. Ophthalmol. 2019, 257, 2221–2231. [Google Scholar] [CrossRef] [PubMed]
- Koo, H.; Moon, H.; Han, H.; Na, J.H.; Huh, M.S.; Park, J.H.; Woo, S.J.; Park, K.H.; Kwon, I.C.; Kim, K.; et al. The movement of self-assembled amphiphilic polymeric nanoparticles in the vitreous and retina after intravitreal injection. Biomaterials 2012, 33, 3485–3493. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Xu, Z.; Liu, J.; Zhang, Z.; Chen, H.; Li, X.; Shi, S. Visual tracing of diffusion and biodistribution for amphiphilic cationic nanoparticles using photoacoustic imaging after ex vivo intravitreal injections. Int. J. Nanomed. 2016, 11, 5079–5086. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Le Luyer, C.; Lou, L.; Bovier, C.; Plenet, J.; Dumas, J.; Mugnier, J. A thick sol–gel inorganic layer for optical planar waveguide applications. Opt. Mater. 2001, 18, 211–217. [Google Scholar] [CrossRef]
- Schoonheydt, R.A. Functional hybrid clay mineral films. Appl. Clay Sci. 2014, 96, 9–21. [Google Scholar] [CrossRef]
- Gala, A. Observations on the Hydrogen Ion Concentration in the Vitreous Body of the Eye with Reference to Glaucoma. Br. J. Ophthalmol. 1925, 9, 516–519. [Google Scholar] [CrossRef] [Green Version]
- Mirzaei, M.; Gupta, V.B.; Chick, J.M.; Greco, T.M.; Wu, Y.; Chitranshi, N.; Wall, R.V.; Hone, E.; Deng, L.; Dheer, Y.; et al. Age-related neurodegenerative disease associated pathways identified in retinal and vitreous proteome from human glaucoma eyes. Sci. Rep. 2017, 7, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Lee, D.; Kim, K.-Y.; Noh, Y.H.; Chai, S.; Lindsey, J.D.; Ellisman, M.H.; Weinreb, R.N.; Ju, W.-K. Brimonidine Blocks Glutamate Excitotoxicity-Induced Oxidative Stress and Preserves Mitochondrial Transcription Factor A in Ischemic Retinal Injury. PLoS ONE 2012, 7, e47098. [Google Scholar] [CrossRef] [Green Version]
- Tawari, S.L.; Koch, D.L.; Cohen, C. Electrical Double-Layer Effects on the Brownian Diffusivity and Aggregation Rate of Laponite Clay Particles. J. Colloid Interface Sci. 2001, 240, 54–66. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, J.G. Optical coherence tomography for ultrahigh resolution in vivo imaging. Nat. Biotechnol. 2003, 21, 1361–1367. [Google Scholar] [CrossRef] [PubMed]
- Hartman, R.R.; Kompella, U.B. Intravitreal, Subretinal, and Suprachoroidal Injections: Evolution of Microneedles for Drug Delivery. J. Ocul. Pharmacol. Ther. 2018, 34, 141–153. [Google Scholar] [CrossRef] [PubMed]
- Moroi, S.E.; Reed, D.M.; Sanders, D.S.; AlMazroa, A.; Kagemann, L.; Shah, N.; Shekhawat, N.; Richards, J.E. Precision medicine to prevent glaucoma-related blindness. Curr. Opin. Ophthalmol. 2019, 30, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Korot, E.; Comer, G.M.; Steffens, T.; Antonetti, D.A. Algorithm for the Measure of Vitreous Hyperreflective Foci in Optical Coherence Tomographic Scans of Patients with Diabetic Macular Edema. JAMA Ophthalmol. 2016, 134, 15–20. [Google Scholar] [CrossRef]
- Sakamoto, T.; Ishibashi, T. Hyalocytes: Essential cells of the vitreous cavity in vitreoretinal pathophysiology? Retina 2011, 31, 222–228. [Google Scholar] [CrossRef]
- Vagaja, N.N.; Chinnery, H.R.; Binz, N.; Kezic, J.M.; Rakoczy, E.P.; McMenamin, P.G. Changes in Murine Hyalocytes Are Valuable Early Indicators of Ocular Disease. Investig. Ophthalmol. Vis. Sci. 2012, 53, 1445–1451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, X.; Hui, B.T.; Way, C.; Beese, S.; Adriano, A.; Keane, P.; Moore, D.J.; Denniston, A.K. Noninvasive Instrument-based Tests for Detecting and Measuring Vitreous Inflammation in Uveitis: A Systematic Review. Ocul. Immunol. Inflamm. 2020, 1–12. [Google Scholar] [CrossRef] [PubMed]








| TIME | OHT (>20 mmHg) EYES (in %) | Intraocular Pressure (X ± sd) | |||
|---|---|---|---|---|---|
| Non-Treated | Treated | Non-Treated | Treated | p | |
| BASELINE | 0 | 0 | 9.12 ± 1.48 | 8.86 ± 1.69 | 0.476 |
| 2 w | 88 | 4.8 | 23.34 ± 3.53 | 14.96 ± 4.16 | <0.001 |
| 4 w (1 m) | 91.7 | 28.1 | 25.26 ± 3.69 | 17.36 ± 4.10 | <0.001 |
| 6 w | 100 | 58.8 | 27.22 ± 3.15 | 20.64 ± 5.04 | <0.001 |
| 8 w (2 m) | 95 | 43.8 | 28.93 ± 7.11 | 19.85 ± 4.51 | <0.001 |
| 12 w (3 m) | 36.8 | 50 | 19.10 ± 3.07 | 19.70 ± 2.39 | 0.423 |
| 16 w (4 m) | 58.3 | 80 | 20.05 ± 4.35 | 21.79 ± 1.42 | 0.364 |
| 20 w (5 m) | 28.6 | 60 | 17.38 ± 2.87 | 21.19 ± 5.49 | 0.166 |
| 24 w (6 m) | 71.4 | 60 | 23.66 ± 5.45 | 23.26 ± 4.82 | 0.684 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodrigo, M.J.; Palomar, A.P.d.; Montolío, A.; Mendez-Martinez, S.; Subias, M.; Cardiel, M.J.; Martinez-Rincon, T.; Cegoñino, J.; Fraile, J.M.; Vispe, E.; et al. Monitoring New Long-Lasting Intravitreal Formulation for Glaucoma with Vitreous Images Using Optical Coherence Tomography. Pharmaceutics 2021, 13, 217. https://doi.org/10.3390/pharmaceutics13020217
Rodrigo MJ, Palomar APd, Montolío A, Mendez-Martinez S, Subias M, Cardiel MJ, Martinez-Rincon T, Cegoñino J, Fraile JM, Vispe E, et al. Monitoring New Long-Lasting Intravitreal Formulation for Glaucoma with Vitreous Images Using Optical Coherence Tomography. Pharmaceutics. 2021; 13(2):217. https://doi.org/10.3390/pharmaceutics13020217
Chicago/Turabian StyleRodrigo, Maria Jesus, Amaya Pérez del Palomar, Alberto Montolío, Silvia Mendez-Martinez, Manuel Subias, Maria Jose Cardiel, Teresa Martinez-Rincon, José Cegoñino, José Maria Fraile, Eugenio Vispe, and et al. 2021. "Monitoring New Long-Lasting Intravitreal Formulation for Glaucoma with Vitreous Images Using Optical Coherence Tomography" Pharmaceutics 13, no. 2: 217. https://doi.org/10.3390/pharmaceutics13020217
APA StyleRodrigo, M. J., Palomar, A. P. d., Montolío, A., Mendez-Martinez, S., Subias, M., Cardiel, M. J., Martinez-Rincon, T., Cegoñino, J., Fraile, J. M., Vispe, E., Mayoral, J. A., Polo, V., & Garcia-Martin, E. (2021). Monitoring New Long-Lasting Intravitreal Formulation for Glaucoma with Vitreous Images Using Optical Coherence Tomography. Pharmaceutics, 13(2), 217. https://doi.org/10.3390/pharmaceutics13020217