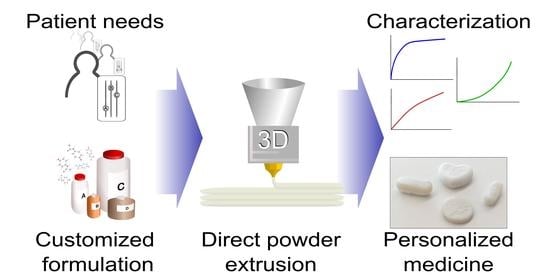
Direct Powder Extrusion of Paracetamol Loaded Mixtures for 3D Printed Pharmaceutics for Personalized Medicine via Low Temperature Thermal Processing
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials, Reagents and Reference Products
2.2. Equipment
2.3. HPLC Analysis
2.4. Processing and Characterization
2.5. Release Studies
2.5.1. Assay
2.5.2. Dissolution Studies
2.6. Thermal Characterization
2.7. 3D Print
3. Results
3.1. Extrusion of the Samples
3.2. Solubility and Release Curves
3.2.1. Preliminary Screening
3.2.2. Dissolution Studies
3.2.3. Ageing of the Samples
3.3. Thermal Characterization
3.4. 3 DP Pills
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cutler, R.L.; Fernandez-Llimos, F.; Frommer, M.; Benrimoj, C.; Garcia-Cardenas, V. Economic impact of medication non-adherence by disease groups: A systematic review. BMJ Open 2018, 8, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Gast, A.; Mathes, T. Medication adherence influencing factors-An (updated) overview of systematic reviews. Syst. Rev. 2019, 8, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Vermeire, E.; Hearnshaw, H.; Van Royen, P.; Denekens, J. Patient adherence to treatment: Three decades of research. A comprehensive review. J. Clin. Pharm. Ther. 2001, 26, 331–342. [Google Scholar] [CrossRef]
- Kini, V.; Michael Ho, P. Interventions to Improve Medication Adherence: A Review. JAMA J. Am. Med. Assoc. 2018, 320, 2461–2473. [Google Scholar] [CrossRef] [PubMed]
- Coskun, S.; Bagcivan, G. Associated factors with treatment adherence of patients diagnosed with chronic disease: Relationship with health literacy. Appl. Nurs. Res. 2021, 57, 151368. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, G.L.; Lula-Barros, D.S.; Silva, D.L.M.; Leite, S.N. Factors related to adherence to treatment from the perspective of the old person. Rev. Bras. Geriatr. Gerontol. 2020, 23, e200160. [Google Scholar] [CrossRef]
- Goyanes, A.; Madla, C.M.; Umerji, A.; Duran Piñeiro, G.; Giraldez Montero, J.M.; Lamas Diaz, M.J.; Gonzalez Barcia, M.; Taherali, F.; Sánchez-Pintos, P.; Couce, M.-L.; et al. Automated therapy preparation of isoleucine formulations using 3D printing for the treatment of MSUD: First single-centre, prospective, crossover study in patients. Int. J. Pharm. 2019, 567, 118497. [Google Scholar] [CrossRef]
- Herrada-Manchón, H.; Rodríguez-González, D.; Alejandro Fernández, M.; Suñé-Pou, M.; Pérez-Lozano, P.; García-Montoya, E.; Aguilar, E. 3D printed gummies: Personalized drug dosage in a safe and appealing way. Int. J. Pharm. 2020, 587, 119687. [Google Scholar] [CrossRef]
- Goyanes, A.; Scarpa, M.; Kamlow, M.; Gaisford, S.; Basit, A.W.; Orlu, M. Patient acceptability of 3D printed medicines. Int. J. Pharm. 2017, 530, 71–78. [Google Scholar] [CrossRef]
- Schork, N.J. Personalized medicine: Time for one-person trials. Nature 2015, 520, 609–611. [Google Scholar] [CrossRef]
- Eap, C.B. Personalized prescribing: A new medical model for clinical implementation of psychotropic drugs. Dialogues Clin. Neurosci. 2016, 18, 313–322. [Google Scholar]
- Brustugun, J.; Notaker, N.; Paetz, L.H.; Tho, I.; Bjerknes, K. Adjusting the dose in paediatric care: Dispersing four different aspirin tablets and taking a proportion. Eur. J. Hosp. Pharm. 2019, 28, 76–82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rautamo, M.; Kvarnström, K.; Sivén, M.; Airaksinen, M.; Lahdenne, P.; Sandler, N. A Focus Group Study about Oral Drug Administration Practices at Hospital Wards—Aspects to Consider in Drug Development of Age-Appropriate Formulations for Children. Pharmaceutics 2020, 12, 109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goole, J.; Amighi, K. 3D printing in pharmaceutics: A new tool for designing customized drug delivery systems. Int. J. Pharm. 2016, 499, 376–394. [Google Scholar] [CrossRef]
- Prasad, L.K.; Smyth, H. 3D Printing technologies for drug delivery: A review. Drug Dev. Ind. Pharm. 2016, 42, 1019–1031. [Google Scholar] [CrossRef]
- Siamidi, A.; Tsintavi, M.E.; Rekkas, D.; Vlachou, M. 3D-Printed Modified-Release Tablets: A Review of the Recent Advances. Mol. Pharmacol. 2020, 1–13. [Google Scholar]
- Jamróz, W.; Szafraniec, J.; Kurek, M.; Jachowicz, R. 3D printing in pharmaceutical and medical applications. Pharm. Res. 2018, 35, Article 176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seoane-Viaño, I.; Januskaite, P.; Alvarez-Lorenzo, C.; Basit, A.W.; Goyanes, A. Semi-solid extrusion 3D printing in drug delivery and biomedicine: Personalised solutions for healthcare challenges. J. Control Release 2021, 332, 367–389. [Google Scholar] [CrossRef] [PubMed]
- Censi, R.; Gigliobianco, M.R.; Casadidio, C.; Di Martino, P. Hot melt extrusion: Highlighting physicochemical factors to be investigated while designing and optimizing a hot melt extrusion process. Pharmaceutics 2018, 10, 89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ligon, S.C.; Liska, R.; Stampfl, J.; Gurr, M.; Mülhaupt, R. Polymers for 3D Printing and Customized Additive Manufacturing. Chem. Rev. 2017, 117, 10212–10290. [Google Scholar] [CrossRef] [Green Version]
- Zhang, B.; Song, J. 3D-Printed Biomaterials for Guided Tissue Regeneration. Small Methods 2018, 1700306, 1700306. [Google Scholar] [CrossRef]
- Konta, A.A.; García-Piña, M.; Serrano, D.R. Personalised 3D printed medicines: Which techniques and polymers are more successful? Bioengineering 2017, 4, 79. [Google Scholar] [CrossRef] [Green Version]
- Goyanes, A.; Allahham, N.; Trenfield, S.J.; Stoyanov, E.; Gaisford, S.; Basit, A.W. Direct powder extrusion 3D printing: Fabrication of drug products using a novel single-step process. Int. J. Pharm. 2019, 567, 118471. [Google Scholar] [CrossRef]
- Goyanes, A.; Buanz, A.B.M.; Basit, A.W.; Gaisford, S. Fused-filament 3D printing (3DP) for fabrication of tablets. Int. J. Pharm. 2014, 476, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Li Chew, S.; de Mohac, L.M.; Raimi-Abraham, B.T. 3D-Printed Solid Dispersion Drug Products. Pharmaceutics 2019, 11, 1–12. [Google Scholar]
- Đuranović, M.; Obeid, S.; Madžarević, M.; Cvijić, S.; Ibrić, S. Paracetamol extended release FDM 3D printlets: Evaluation of formulation variables on printability and drug release. Int. J. Pharm. 2020, 592, 120053. [Google Scholar] [CrossRef]
- Gorkem Buyukgoz, G.; Soffer, D.; Defendre, J.; Pizzano, G.M.; Davé, R.N. Exploring tablet design options for tailoring drug release and dose via fused deposition modeling (FDM) 3D printing. Int. J. Pharm. 2020, 591, 119987. [Google Scholar] [CrossRef]
- Henry, S.; Samaro, A.; Marchesini, F.H.; Shaqour, B.; Macedo, J.; Vanhoorne, V.; Vervaet, C. Extrusion-based 3D printing of oral solid dosage forms: Material requirements and equipment dependencies. Int. J. Pharm. 2021, 598, 120361. [Google Scholar] [CrossRef]
- Ayyoubi, S.; Cerda, J.R.; Fernández-García, R.; Knief, P.; Lalatsa, A.; Marie Healy, A.; Serrano, D.R. 3D printed spherical mini-tablets: Geometry versus composition effects in controlling dissolution from personalised solid dosage forms. Int. J. Pharm. 2021, 597, 120336. [Google Scholar] [CrossRef]
- Zhang, J.; Yang, W.; Vo, A.Q.; Feng, X.; Ye, X.; Kim, D.W.; Repka, M.A. Hydroxypropyl methylcellulose-based controlled release dosage by melt extrusion and 3D printing: Structure and drug release correlation. Carbohydr. Polym. 2017, 177, 49–57. [Google Scholar] [CrossRef]
- Goyanes, A.; Fina, F.; Martorana, A.; Sedough, D.; Gaisford, S.; Basit, A.W. Development of modified release 3D printed tablets (printlets) with pharmaceutical excipients using additive manufacturing. Int. J. Pharm. 2017, 527, 21–30. [Google Scholar] [CrossRef]
- Fina, F.; Goyanes, A.; Rowland, M.; Gaisford, S.; Basit, A.W. 3D printing of tunable zero-order release printlets. Polymers (Basel) 2020, 12, 1769. [Google Scholar] [CrossRef] [PubMed]
- Ong, J.J.; Awad, A.; Martorana, A.; Gaisford, S.; Stoyanov, E.; Basit, A.W.; Goyanes, A. 3D printed opioid medicines with alcohol-resistant and abuse-deterrent properties. Int. J. Pharm. 2020, 579, 119169. [Google Scholar] [CrossRef]
- Rouaz, K.; Chiclana-Rodríguez, B.; Nardi-Ricart, A.; Suñé-Pou, M.; Mercadé-Frutos, D.; Suñé-Negre, J.M.; Pérez-Lozano, P.; García-Montoya, E. Excipients in the Paediatric Population: A Review. Pharmaceutics 2021, 13, 387. [Google Scholar] [CrossRef]
- Rowe, R.C.; Sheskey, P.J.; Quinn, M.E. Handbook of Pharmaceutical Excipients; Pharmaceutical Press: London, UK, 2009; ISBN 9780853697923. [Google Scholar]
- Gohel, M.C.; Jogani, P.D. A review of co-processed directly compressible excipients. J. Pharm. Pharm. Sci. 2005, 8, 76–93. [Google Scholar] [PubMed]
- Khaled, S.A.; Alexander, M.R.; Wildman, R.D.; Wallace, M.J.; Sharpe, S.; Yoo, J.; Roberts, C.J. 3D extrusion printing of high drug loading immediate release paracetamol tablets. Int. J. Pharm. 2018, 538, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Voura, C.; Gruber, M.M.; Schroedl, N.; Strohmeier, D.; Eitzinger, B.; Bauer, W.; Brenn, G.; Khinast, J.G.; Zimmer, A. Printable medicines: A microdosing device for producing personalised medicines. Pharm. Technol. Eur. 2011, 23, 32–36. [Google Scholar]
- Liu, H.; Xie, F.; Yu, L.; Chen, L.; Li, L. Thermal processing of starch-based polymers. Prog. Polym. Sci. 2009, 34, 1348–1368. [Google Scholar] [CrossRef]
- Szabó-Révész, P.; Szepes, A. Potato starch in pharmaceutical technology-A review. Glob. Sci. 2009, 3, 109–117. [Google Scholar]
- Efthimiadou, E.K.; Metaxa, A.; Kordas, G. Modified Polysaccharides as Drug Delivery. Polysacch. Bioact. Biotechnol. 2014, 1–26. [Google Scholar]
- Liu, X.; Wang, Y.; Yu, L.; Tong, Z.; Chen, L.; Liu, H.; Li, X. Thermal degradation and stability of starch under different processing conditions. Starch/Staerke 2013, 65, 48–60. [Google Scholar] [CrossRef]
- Nafchi, A.M.; Moradpour, M.; Saeidi, M.; Alias, A.K. Thermoplastic starches: Properties, challenges, and prospects. Starch/Staerke 2013, 65, 61–72. [Google Scholar] [CrossRef]
- Wang, S.; Chao, C.; Huang, S.; Yu, J. Starch Structure, Functionality and Application in Foods; Springer Nature: Singapore, 2020; ISBN 9789811506222. [Google Scholar]
- Aviara, N.A.; Igbeka, J.C.; Nwokocha, L.M.; Engineering, E.R. Physicochemical properties of sorghum (sorghum bicolor l. Moench) starch as affected by drying temperature. Agric. Eng. Int. CIGR J. 2010, 12, 85–94. [Google Scholar]
- Ratnayake, W.S.; Jackson, D.S. Chapter 5 Starch Gelatinization. Adv. Food Nutr. Res. 2008, 55, 221–268. [Google Scholar]
- Bialleck, S.; Rein, H. Preparation of starch-based pellets by hot-melt extrusion. Eur. J. Pharm. Biopharm. 2011, 79, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Francis, M.F.; Piredda, M.; Winnik, F.M. Solubilization of poorly water soluble drugs in micelles of hydrophobically modified hydroxypropylcellulose copolymers. J. Control Release 2003, 93, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Dürig, T.; Karan, K. Binders in Wet Granulation. In Handbook of Pharmaceutical Wet Granulation; Elsevier: Amsterdam, The Netherlands, 2019; pp. 317–349. ISBN 9780128104606. [Google Scholar]
- Loreti, G.; Maroni, A.; Del Curto, M.D.; Melocchi, A.; Gazzaniga, A.; Zema, L. Evaluation of hot-melt extrusion technique in the preparation of HPC matrices for prolonged release. Eur. J. Pharm. Sci. 2014, 52, 77–85. [Google Scholar] [CrossRef]
- Jaiswar, D.R.; Pawar, J.N.; Amin, P.D. Hot Melt Extrusion: Continuous Process of Preparation of Sustained Released Matrix Tablet by Using Hydroxypropylcellulose. Am. J. PharmTech Res. 2015, 6, 295–312. [Google Scholar]
- Prodduturi, S.; Urman, K.L.; Otaigbe, J.U.; Repka, M.A. Stabilization of hot-melt extrusion formulations containing solid solutions using polymer blends. AAPS PharmSciTech 2007, 8, E152–E161. [Google Scholar] [CrossRef] [Green Version]
- Azam, R.S.M.; Zhang, M.; Bhandari, B.; Yang, C. Effect of Different Gums on Features of 3D Printed Object Based on Vitamin-D Enriched Orange Concentrate. Food Biophys. 2018, 13, 250–262. [Google Scholar] [CrossRef]
- Chen, H.; Xie, F.; Chen, L.; Zheng, B. Effect of rheological properties of potato, rice and corn starches on their hot-extrusion 3D printing behaviors. J. Food Eng. 2019, 244, 150–158. [Google Scholar] [CrossRef] [Green Version]
- Liu, Z.; Chen, H.; Zheng, B.; Xie, F.; Chen, L. Understanding the structure and rheological properties of potato starch induced by hot-extrusion 3D printing. Food Hydrocoll. 2020, 105, 105812. [Google Scholar] [CrossRef]
- Parada, J.; Aguilera, J.M.; Brennan, C. Effect of guar gum content on some physical and nutritional properties of extruded products. J. Food Eng. 2011, 103, 324–332. [Google Scholar] [CrossRef]
- Wang, J.; Jin, Z.; Yuan, X. Preparation of resistant starch from starch-guar gum extrudates and their properties. Food Chem. 2007, 101, 20–25. [Google Scholar] [CrossRef]
- Brennan, M.A.; Monro, J.A.; Brennan, C.S. Effect of inclusion of soluble and insoluble fibres into extruded breakfast cereal products made with reverse screw configuration. Int. J. Food Sci. Technol. 2008, 43, 2278–2288. [Google Scholar] [CrossRef]
- Dikeman, C.L.; Fahey, G.C. Viscosity as related to dietary fiber: A review. Crit. Rev. Food Sci. Nutr. 2006, 46, 649–663. [Google Scholar] [CrossRef]
- Saini, S.; Garg, R. Design expert assisted mathematical optimization of solubility and study of fast disintegrating tablets of Lercanidipine Hydrochloride. J. Drug Deliv. Ther. 2019, 9, 172–180. [Google Scholar] [CrossRef]
- Shi, K.; Salvage, J.P.; Maniruzzaman, M.; Nokhodchi, A. Role of release modifiers to modulate drug release from fused deposition modelling (FDM) 3D printed tablets. Int. J. Pharm. 2021, 597, 120315. [Google Scholar] [CrossRef]
- Goyanes, A.; Robles Martinez, P.; Buanz, A.; Basit, A.W.; Gaisford, S. Effect of geometry on drug release from 3D printed tablets. Int. J. Pharm. 2015, 494, 657–663. [Google Scholar] [CrossRef] [PubMed]
- Arafat, B.; Wojsz, M.; Isreb, A.; Forbes, R.T.; Isreb, M.; Ahmed, W.; Arafat, T.; Alhnan, M.A. Tablet fragmentation without a disintegrant: A novel design approach for accelerating disintegration and drug release from 3D printed cellulosic tablets. Eur. J. Pharm. Sci. 2018, 118, 191–199. [Google Scholar] [CrossRef]
- Pietrzak, K.; Isreb, A.; Alhnan, M.A. A flexible-dose dispenser for immediate and extended release 3D printed tablets. Eur. J. Pharm. Biopharm. 2015, 96, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.V. A DSC study of some biomaterials relevant to pharmaceutical industry. J. Therm. Anal. Calorim. 2013, 112, 791–793. [Google Scholar] [CrossRef]
- Chuanxing, F.; Qi, W.; Hui, L.; Quancheng, Z.; Wang, M. Effects of Pea Protein on the Properties of Potato Starch-Based 3D Printing Materials. Int. J. Food Eng. 2018, 14, 1–10. [Google Scholar] [CrossRef]
- Lin, C.L.; Lin, J.H.; Lin, J.J.; Chang, Y.H. Properties of High-Swelling Native Starch Treated by Heat-Moisture Treatment with Different Holding Times and Iterations. Molecules 2020, 25, 5528. [Google Scholar] [CrossRef] [PubMed]






| Sample | Paracetamol (%) | Starch (%) | HPC (%) | Guar Gum (%) | Added Water (%) | Total Moisture (%) |
|---|---|---|---|---|---|---|
| FG05702500A | 5 | 70 | 25 | 0 | 2.1 | 9.1 |
| FG20552500A | 20 | 55 | 25 | 0 | 1.65 | 7.15 |
| FG35402500A | 35 | 40 | 25 | 0 | 1.2 | 5.2 |
| FG50252500A | 50 | 25 | 25 | 0 | 0.75 | 3.25 |
| FG05652505A | 5 | 65 | 25 | 5 | 1.95 | 8.75 |
| FG20502505A | 20 | 50 | 25 | 5 | 1.5 | 6.8 |
| FG35352505A | 35 | 35 | 25 | 5 | 1.05 | 4.85 |
| FG50202505A | 50 | 20 | 25 | 5 | 0.6 | 2.9 |
| FG05602510A | 5 | 60 | 25 | 10 | 1.8 | 8.4 |
| FG20452510A | 20 | 45 | 25 | 10 | 1.35 | 6.45 |
| FG35302510A | 35 | 30 | 25 | 10 | 0.9 | 4.5 |
| FG50152510A | 50 | 15 | 25 | 10 | 0.45 | 2.55 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mendibil, X.; Tena, G.; Duque, A.; Uranga, N.; Campanero, M.Á.; Alonso, J. Direct Powder Extrusion of Paracetamol Loaded Mixtures for 3D Printed Pharmaceutics for Personalized Medicine via Low Temperature Thermal Processing. Pharmaceutics 2021, 13, 907. https://doi.org/10.3390/pharmaceutics13060907
Mendibil X, Tena G, Duque A, Uranga N, Campanero MÁ, Alonso J. Direct Powder Extrusion of Paracetamol Loaded Mixtures for 3D Printed Pharmaceutics for Personalized Medicine via Low Temperature Thermal Processing. Pharmaceutics. 2021; 13(6):907. https://doi.org/10.3390/pharmaceutics13060907
Chicago/Turabian StyleMendibil, Xabier, Gaizka Tena, Alaine Duque, Nerea Uranga, Miguel Ángel Campanero, and Jesús Alonso. 2021. "Direct Powder Extrusion of Paracetamol Loaded Mixtures for 3D Printed Pharmaceutics for Personalized Medicine via Low Temperature Thermal Processing" Pharmaceutics 13, no. 6: 907. https://doi.org/10.3390/pharmaceutics13060907
APA StyleMendibil, X., Tena, G., Duque, A., Uranga, N., Campanero, M. Á., & Alonso, J. (2021). Direct Powder Extrusion of Paracetamol Loaded Mixtures for 3D Printed Pharmaceutics for Personalized Medicine via Low Temperature Thermal Processing. Pharmaceutics, 13(6), 907. https://doi.org/10.3390/pharmaceutics13060907