1. Introduction
Immunologic diseases are caused by an imbalance between the immune system function to protect the body from bacteria and viruses and tissue damage because of the immune response [
1]. Some kinds of autoimmune diseases are immunologic diseases, which are the result of identifying the patient’s own organs, tissues, and cells as foreign and activating an immune response against them. Individually, these diseases are rare, but as a group, they are the most common diseases in industrialized countries [
2], and they affect between 5 and 10% of the European and North American population [
3].
Sjögren’s syndrome (SS) is a chronic systemic autoimmune disease that can be suffered as a unique disease (primary SS) or can be a consequence of another autoimmune disease (secondary SS) [
4]. Primary SS is a highly prevalent, chronic, autoimmune exocrinopathy today, affecting from 0.2 to 3% of the general population. It is caused by the loss of central tolerance, which generates epithelitis and acinar atrophy due to predominantly inflammatory cell types which infiltrate into the exocrine glands and certain extraglandular tissues [
5]. It is characterized by keratoconjunctivitis sicca (dry eyes) and xerostomia (dry mouth) [
4,
6].
The European Study Group on Classification Criteria developed and validated a criteria classification for primary SS between 1989 and 1996. It was made observing 180 people, of which 76 were affected by primary SS and 104 were not. It is organized in a classification tree performance and has a sensitivity of 96.1% and a specificity of 94.2% [
7].
Different anti-inflammatory and immunomodulatory drugs are used in the treatment of ocular inflammatory and immunological diseases. Two examples are diclofenac, used as an anti-inflammatory agent, and cyclosporine, used an as anti-inflammatory and immunomodulatory drug [
8]. Baricitinib is an immunosuppressant drug that acts inhibiting selectively Janus kinases 1 and 2, among others, and reduces disease signs and symptoms by decreasing inflammation, cellular activation, and proliferation of key immune cells. Baricitinib has already been used for the treatment of atopic dermatitis through oral administration with good outcomes: oral baricitinib improved signs and resolved symptoms better than topic cyclosporin [
9]. Another advantage is that baricitinib has anti-inflammatory properties due to its therapeutic path. Now, baricitinib is orally administrated for the treatment of moderate-to-severe atopic dermatitis and rheumatoid arthritis, and it is also being studied for its oral administration for systemic erythematosusmatous, psoriasis, and primary SS [
10,
11]. The pilot study of baricitinib oral administration conducted in China using active SS patients seemed to show efficacy and safety [
12]. The actual treatment for primary SS is divided into topical treatment for the mouth and eyes to control the symptoms and avoid complications, and systemic treatment for parotid enlargement and extraglandular signs. Topical treatments are preventive: fluor is used to avoid periodontal diseases and chlorhexidine for electrostimulation; and for the eyes, artificial tears are used. Anti-inflammatory drugs and local ciclosporin, pilocarpine, or cevimeline secretagogue are used in both cases to stimulate saliva or lacrimal flow. Systemic treatments consist of glucocorticoids and different immunosuppressants [
13].
Liposomes are spherically shaped nano-sized to micro-sized vesicles composed of biodegradable natural or synthetic phospholipids. They are formed spontaneously in an aqueous medium so that inside the vesicles different agents can be encapsulated; the hydrophobic agents between the lipids and the hydrophilic ones in the aqueous core [
14]. Liposomes can have very different properties because of their composition, surface charge, size, phospholipid bilayer membrane, and method of preparation [
15,
16,
17]. One way for liposomes to be classified is by their size and number of bilayers: multilamellar liposome vesicles (MLV) and unilamellar vesicles (UV). The latter group has three more stages, as shown in
Figure 1.
The liposomes’ composition is biocompatible, biodegradable, and non-toxic, and the flexibility of their formulation allows for different sizes of liposomes that make it possible to use them as eye drops [
8]. These characteristics also help at the time of preparing an ophthalmic formulation, during which, some points need to be studied to avoid compatibility problems: the pH has to be in a range close to the physiologic pH, the osmolarity has to be isotonic with the tears and to prevent infections, and sterility is also necessary [
18]. The high capacity of entrapment relies on its ability to encapsulate a wide range of drugs, and having this advantage overcomes the common problem of drugs that are water-insoluble or poorly soluble in this kind of formulation [
19]. As for liposome size and charge for eye application, it has been shown that the interaction of liposomes with cornea follow this order: MLV
+ > SUV
+ > MLV
− > SUV
− > MLV [
8].
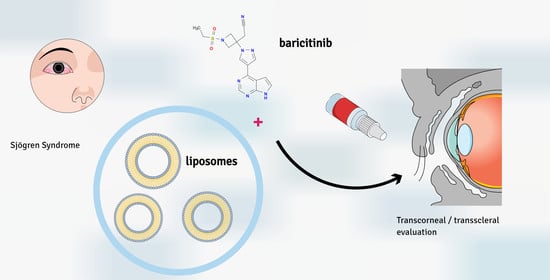
To our knowledge, no studies involving baricitinib administered by the ophthalmic route have been conducted. Stevenson and co-workers determined the efficacy of another Janus kinase inhibitor; 0.003% tofacitinib was applied ocularly in mice which had induced corneal thermocautery, resulting in a decrease in the interleukins [
20]. In another study, Hofauer and colleagues investigated the efficacy of liposomal agents for the symptoms of xerostomia, keratoconjunctivitis sicca, and rhinitis sicca in a clinical trial involving patients with Sjögren’s syndrome. The authors concluded that liposomes were an effective local approach since they significantly reduced the symptoms of xerostomia, keratoconjunctivitis sicca, and rhinitis sicca after 2 months of treatment [
21]. Taking into account the satisfactory results obtained by Stevenson et al. with tofacitinib and those obtained by Hofauer with liposomal agents, we aimed to formulate liposomes loading baricitinib for ophthalmic administration as an alternative or co-adjuvant treatment for Sjögren’s syndrome [
9]. Therefore, our intention with these formulations is to simplify the eye topical treatment to one step. We characterized two liposomes with two different lipids and we assessed the baricitinib release from the formulations as well as the capacity of baricitinib to penetrate the corneal and scleral tissues through ex vivo permeation tests. We also investigated the tolerability of the developed formulations on the eye by alternative in vitro methods, such as the HET-CAM technique and the evaluation of the cornea transparency. Finally, we conducted histological studies on the tissues after the permeation test.
4. Discussion
Two liposomes loading baricitinib were developed using two different lipids (Lα-P and POPE:POPG) with the aim of combining the effect of an immunomodulator and the effect of the lipids to supplement the tear film lipid layer. It is known that alterations in lipid composition, besides down-regulation in specific proteins or changes in the rheological behavior of the tears, are common in dry eye disease. Lipid-based formulations aim to mimic the tear film lipid layer by combining both components, the aqueous one and the lipid one [
36]. As Hofauer and co-workers in a previous work had applied liposomal agents on buccal, nasal, and ocular mucosa in patients with Sjögrens’ syndrome to alleviate symptoms such as xerostomia, keratoconjunctivis sicca, and rhinitis sicca [
21], and they had achieved positive results, it could be fruitful to load up liposomes with a specific immunomodulator, as it may result in synergistic effects, achieving an advance in the treatment.
Baricitinib has been used orally and no literature is available reporting nanostructured systems loading baricitinib for the topical route. It has been tested (only) once on the skin and there is very little information on formulating baricitinib in nano-systems. Bhaskarmurthy et al. [
37] investigated the potential of baricitinib in reducing the inflammation in ear oedema TPA-induced inflammation in mice; we can underscore that they used a solution of baricitinib in acetone:DMSO, and they were testing on the skin, not on the mucosa or eye. Our study, therefore, encourages further research, building on the potential of baricitinib and its use in ocular mucosa. Both liposomes exhibit suitable characteristics for the ophthalmic application: their smallness in size will not damage the cornea upon application, and their pH is close to the tears’ value (7.4–7.5), so no irritation is expected; additionally, the osmolality was also within the criterium. The liposomes should resist aggregation due to Waals attraction forces because the zeta potential value is highly negative [
38,
39]. The surface electrical study focuses on two aspects. First, the dependence of the lipid composition, and secondly, the influence of the pH and ionic strength on ZP.
One of the major constraints of liposomal systems is the vesicle aggregation, with the concomitant destabilization of the system [
40]. Moreover, the surface electrical charge of liposomes does play a fundamental role in the affinity on the corneal surface [
41]. Along the same lines, the study of the surface electrical properties provides the expected relevant information; the lipid composition of liposomes has a direct influence on ZP, due to the different net charges of the lipids used: POPE:POPG liposomes showed much more negativity than Lα-PC liposomes. Another question is that the surface charge might also determine the interaction of liposomes with the ocular membrane due to the high negative charge of its mucins.
Absolute values of ZP showed a marked increase when the pH was increased (
Figure 3). Changes in pH can affect the degree of lipid ionization. Specifically, the phosphate groups of the polar head of PC and PG are neutralized at acidic pH by the hydrogen ions of the dispersion medium. In contrast, as the pH value increased, that is, as the concentration of hydroxyl groups in the medium increased, a greater number of surface phosphate groups were dissociated. This determined the increase in the surface electric charge of these particles [
42]. Nanosystems with ZP between +30 mV and −30 mV are considered to possess low stability [
43]. The pH of tears is approximately 7.45 and ranges from 7.14 to 7.82, depending on diurnal and seasonal influences, or even 7.89 in dry eye patients with Sjögren’s disease [
44]. Under these conditions, our liposomal formulations would have values outside the range +30 mV/−30 mV, which, predictably, will provide suitable stability [
45].
The most frequently used aqueous vehicles in the preparation of eye drops are water for injection, isotonic sterile saline (SF), balanced salt solution (BSS®), and balanced salt solutions whose composition is similar to that of the internal ocular medium. Both the composition of these vehicles and physiologically buffer conditions mean that there are electrolytes of different valences that could influence the surface electrical characteristics of the liposomes. The electrolytes are mainly Na+, K+, Cl−, and HCO−, with lower levels of Mg2+ and Ca2+. In this way, the results of the electrokinetic analysis of the liposomes as a function of the ionic strength of the medium could be used to predict their stability in dispersion (aggregation tendency) and their mucoadhesive capacity.
The eye can tolerate tonicities within the equivalent range of 0.6–2% NaCl. However, to achieve isotonic solutions with tears, and to ensure that they are comfortable for the eye, an amount equivalent to 0.9% NaCl 0.15 M is generally used.
According to our results, shown in
Figure 4, as the concentration of the salts increases the counterions accumulate closer to the particle surface, which compresses the double layer and weakens repulsive forces by reducing ZP [
46].
Regarding the effect of AlCl
3, ZP values were positive across the whole range, probably due to the adsorption of this ion into the surface of the liposomes. Finally, a high concentration of electrolytes equivalent to an isotonic solution might produce charge reversal or a large drop, showing slightly positive values. This fact will cause large size aggregates and rapid settling, which could give rise to a flocculated system that is easy to redisperse [
47]. Additionally, thanks to their positive charge, they could interact better with the ocular film and prolong the residence time of the drug in the cornea, and they have increased the therapeutic interval [
41,
48].
A rapid release of baricitinib is observed within the first 4–6 h and it is followed by a slower drug release for both liposomes after these first six hours. Higher released amounts of baricitinib were obtained from the liposomes Lα-PC, about three-fold higher than the POPE:POPG liposomes, and this suggests that the lipid used in preparing the liposomes has a great impact on the extent of drug released. The release profile of both liposomes fitted to a one-site binding model corresponding to a hyperbola curve. The parameters of this model are Bmax, which corresponds to the maximum amount that can be released, and KD, which is the time needed to reach 50% of the drug released. Statistically significant differences were observed for Bmax. However, no statistical differences were found for KD, meaning that both liposomes release 50% of the drug within a similar time period (more or less in the first two and a half hours). Ansari et al. [
49] developed polymeric nanoparticles loading baricitinib with the aim of improving baricitinib’s bioavailability in order to reduce the dose, and in turn, reducing the side effects. The authors prepared nanoparticles with poly-lactic-co-glycolic acid, and they conducted a deep characterization, obtaining an optimized formulation that exhibited sustained release over 24 h, which fitted the Higuchi model.
Despite the fact that liposome Lα- PC showed a higher in vitro drug release, this was not limiting for POPE:POPG in the penetration and permeation through the cornea, where the amount retained in the tissue was similar for both liposomes. It was POPE:POPG that showed higher permeation. In contrast, Lα- PC was superior to POPE:POPG in the permeation and penetration of baricitinib into and through the sclera. This is probably due to the difference in the composition of sclera and cornea, whereas the latter is mainly composed of type I collagen and proteoglycans, the sclera is primarily composed of connective tissue [
50]. The amount of baricitinib retained in the corneal and scleral tissue would act as a reservoir and might enable a local anti-inflammatory and immunomodulatory effect without systemic side effects since the predicted plasma concentration at the steady-state (Css) is far below the concentration achieved in an oral administration [
51].
5. Conclusions
The HET-CAM technique is an ideal model for testing ocular irritation since the chorioallantoic membrane is a highly vascularized structure and it is sensitive to chemicals such as the conjunctiva [
52]. Both liposomes are supposed to be well-tolerated since no irritant potential was detected by the HET-CAM technique nor was any change observed in the histological analysis after the application of the liposomes on the corneal and scleral tissues. Additionally, no changes in the transparency of the cornea were observed either, meaning that the liposomes do not cause damage to the tissue exposed to them [
34]. In light of these promising results, further studies should be carried out and looked at so as to better assess the efficacy of the liposomes in vivo. For instance, a dry eye in mice models would allow for the evaluation of the efficacy of the liposomes similarly to the work of Stevenson et al. [
19,
20], in which the researchers tested tofacitinib, a JAK inhibitor, applied topically in dry eye-induced mice, and they monitored cytokines expression obtaining excellent outcomes in reducing the ocular inflammation. Since the products intended for ophthalmic use should be sterilized, in this sense, future studies should also consider extruding the liposomes through a 0.22 µm pore size, as well as, investigating the effect of the number of lipid layers composing the liposome on the drug release. Another important point for future studies is the shelf-life of the formulations, and stability studies should also be performed.
Two liposomal formulations have been developed for ocular delivery intended for alleviating dry eyes related to Sjögren’s syndrome. The liposomes were prepared using two different lipids, Lα-PC and POPE:POPG, both loading baricitinib, a Janus kinase inhibitor. Lα-PC led to higher flux, permeation, and retention in the sclera, whereas POPE:POPG led to higher flux and permeation in the cornea. The formulations showed no irritant effects on the chorioallantoic membrane. Additionally, the liposomes did not affect the cornea transparency when applied and the histological analysis did not reveal any structural alteration. The two liposomes have shown promising results for ocular application, and further studies, such as in vivo tests, should be conducted to evaluate their efficacy, and hence, confirm their suitability in the management of dry eyes in Sjögren’s syndrome.