1. Introduction
Cannabis sativa L. is a plant rich in secondary plant metabolites as it contains cannabinoids, terpenes, flavonoids, amino acids, fatty acids, phytosterols, vitamins, and minerals [
1]. Cannabis flowers, also known as inflorescences, possess a range of potential medicinal properties such as analgesic, anti-inflammatory, and antiemetic effects [
2,
3,
4]. Additionally, cannabis flowers have shown promise in aiding sleep, stimulating appetite, and modulating neurological conditions like epilepsy [
5,
6]. Academic research is progressively expanding to explore the medicinal capabilities of cannabis flowers and their constituents.
Cannabinoids, such as tetrahydrocannabinol (THC), cannabidiol (CBD), cannabidiolic acid (CBDA), cannabigerol (CBG), or cannabichromene (CBC) are lipophilic constituents of
Cannabis sativa L. that are poorly soluble in water (2–10 μg/mL) [
7], which is the result of their lipophilic nature (log P 6–7) [
8]. This is a limitation for cannabinoid oral administration as only dissolved compounds can be absorbed across the gastrointestinal epithelium [
9], which results in low bioavailability (THC: 4–12%; CBD: ≈6%) [
10,
11]. The solubility of a molecule is a key determinant of its gastrointestinal fate and poorly soluble compounds may require formulation strategies, such as micronization, lipid-based formulations, or complexation, to improve their solubility and enhance their oral bioavailability [
12,
13]. However, findings in the literature in this field focus on work with pure cannabinoids, not extracts, excluding the entourage effect between cannabis plant components. The vast potential of the phenomenon of synergy between biologically active compounds may be reflected in pharmacotherapy or phytotherapy only after they cross biological barriers, which is only possible for dissolved substances. So far, research to improve the solubility of cannabinoids has focused on improving the solubility of CBD as a result of encapsulation, including nano-emulsions, Pickering emulsions, and inclusion complexes [
14]. For example, a recently published article by Wang et al. describes zein and whey protein composite nanoparticles of CBD prepared by a modified anti-solvent method in which the water solubility of CBD was increased by 465–505 times and increased pharmacokinetic parameters [
14]. Research to improve the solubility of THC included the use of cyclodextrins in the case of Δ
9-THC and Δ
8-THC; for the second substance, it resulted in not only an increase of aqueous solubility but also in the increase of stability and transcorneal permeation [
15,
16].
Another way to overcome poor cannabinoid solubility in water is by using inhalation as a delivery method in smoking or vaporizing. When a cannabis flower or concentrate is heated to a high enough temperature, the cannabinoids are vaporized and can be inhaled, and they have better bioavailability after inhalation. The value ranges from 10% to 35% for THC and varies among patients due to divergence in number, duration, interval of puffs, breath hold time, inhalation volume, used device, and the site of deposition within the respiratory system; for CBD, the average value is 11–45% [
11]. An alternative is to use sublingual drops, which are an extract diluted in a carrier oil to ensure the dissolution of cannabinoids, allowing for rapid absorption through the oral mucosa [
17]. The bioavailability of cannabinoids after sublingual administration was assessed for CBD as 13–19%, whilst for THC it was 13–14% [
18].
All activities to improve the bioavailability of cannabinoids are aimed at better use of the pharmacological activity of individual cannabinoids—or their mixtures—with a specific potency of individual cannabinoids. Current literature reports confirm neuroprotective, anti-epileptic [
19], and sedative effects, which are associated with the achievement of therapeutic goals within the central nervous system. For example, CBD has demonstrated anxiolytic and calming effects in preclinical and clinical studies [
20,
21,
22,
23]. By interacting with serotonin receptors and enhancing the action of gamma-aminobutyric acid (GABA), CBD may promote relaxation and potentially aid in managing sleep disturbances and insomnia [
24]. The modulation of ion channels, neurotransmitter systems, and anti-inflammatory activity are among the proposed mechanisms through which CBD exerts its antiseizure properties [
25]. CBD reduces neuronal excitability through functional antagonism of GPR55 receptors, desensitization of TRPV1 receptors, and inhibition of adenosine transport [
26]. Neuroimaging investigations have revealed noteworthy changes in brain activity and connectivity patterns during both resting states and while engaging in cognitive tasks following the administration of CBD [
27]. CBD has been found to reduce the accumulation of amyloid-beta (Aβ) plaques and decrease the hyperphosphorylation of tau proteins, which are central pathological features of Alzheimer’s disease [
28]. There are not many studies about CBDA or CBC on the nervous system; rather the majority of studies concern CBD and THC. THC interacts with the endocannabinoid system’s CB1 receptors, regulating neurotransmitter release, pain perception, and immune responses [
29,
30]. However, the use of plant material with a high THC content, even for medicinal purposes, could be deemed illegal in many countries across the globe [
31]. The findings indicate that both CBDA and THCA possess properties that may be beneficial in combating Alzheimer’s disease. These cannabinoids can alleviate memory impairments and enhance the brain’s ability to withstand higher levels of calcium (Ca
2+), Aβ, and hyperphosphorylated tau (p-tau) in the hippocampus [
32]. Moreover, a substantial concentration of CBDA effectively reduces neurotoxicity induced by rotenone [
32]. In the rat maximal electroshock seizure test, it has been observed that CBDA exhibits anticonvulsant properties [
33]. CBC interacts with specific TRP cation channels, namely TRPA1, TRPV1, and TRPV8, which play crucial roles in pain relief and inflammation regulation [
34]. Upon binding to these receptors, CBC induces an antinociceptive effect within the brain. CBC positively influenced the viability of adult neural stem progenitor cells during in vitro differentiation, upregulating the marker nestin while downregulating the astrocyte marker Glial fibrillary acidic protein, possibly involving adenosine signaling and ATP modulation in the process [
35]. CBC might be also a potential neuronal differentiation inducer for NSC-34 cells (a hybridoma between spinal cord cells from the embryos of mice and neuroblastoma) [
36]. In addition to the affinity of cannabinoids to selected receptors, there are also non-specific mechanisms of their action within the central nervous system. There are literature reports, including the results published by us, confirming the scavenging of free radicals [
37,
38,
39]. Recent articles present the variety of antioxidant mechanisms of cannabinoids [
38,
40,
41].
Polyvinyl caprolactam-polyvinyl acetate-polyethylene glycol (Soluplus) is an amphiphilic copolymer composed of hydrophilic and lipophilic segments. This structure allows Soluplus to form micelles or colloidal structures when dispersed in water [
42] increasing the solubility of various compounds like curcumin [
43], hesperidin [
44], pterostilbene [
45], or itraconazole [
46]. Magnesium aluminometasilicate (Neusilin US2) is an amorphous, porous material with a high surface area and adsorption capacity. Its porous structure can adsorb hydrophobic molecules onto its surface or within its pores and increase the solubility of compounds such as naringenin [
47], caffeic acid [
48], and celecoxib [
49].
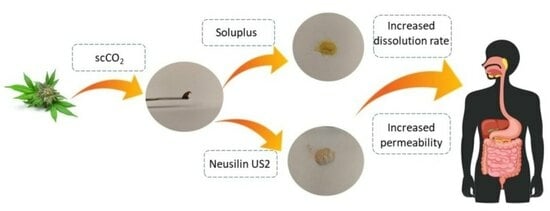
In order to justify the need to increase the solubility and, as a result, the bioavailability of phytocannabinoids present in the inflorescences of
Cannabis sp., we undertook work to improve the solubility of cannabinoids, CBD, CBDA, and CBC whose structures are presented in
Figure 1, by preparing delivery systems with biopolymer (Soluplus) and Neusilin US2 to achieve better bioavailability. Limited research regarding the enhancement of solubility for cannabinoids within whole extracts, rather than isolated or synthesized forms, and notably, the lack of data on dissolution profiles and membrane permeability of CBC and CBDA ensures the novelty of the study.
2. Materials and Methods
2.1. Materials
Cannabis sativa plant material, Białobrzeskie, Tygra, Henola varieties, was donated from the Experimental Station for the Cultivar Testing in Chrząstowo, belonging to the Research Centre for Cultivar Testing in Słupia Wielka. The agricultural details are presented in
Supplementary Materials. The plant material for the study was collected after hemp plants reached the maturation phase, i.e., from the moment of seed formation to the first seed. Immediately after collection, two samples of 500 g each were separated and dried to an absolutely dry mass. The entire drying period lasted twenty hours. The temperature in the oven was maintained at no higher than 50 °C for the first 6 hours and the oven temperature was maintained at 105 °C for the remaining 14 h of drying.
Food-grade CO2 was provided by Air Liquide Polska (Cracow, Poland). Soluplus® (polyvinyl caprolactam-polyvinyl acetate-polyethylene glycol graft copolymer), was supplied by BASF SE (Ludwigshafen, Germany). Neusilin US2 (magnesium aluminometasilicate) was kindly provided by Fuji Chemical Industry (Minato, Tokyo). Cannabinoid standards (CBD–CAS: 13956-29-1, CBDA–CAS: 1244-58-2, and CBC–CAS: 20675-51-8) were purchased from Sigma-Aldrich (Poznan, Poland). Trifluoroacetic acid and acetonitrile (high-performance liquid chromatography [HPLC] grade) were provided by Merck (Darmstadt, Germany). The chemicals 2,2-Diphenyl-1-picrylhydrazyl, iron (III) chloride hexahydrate, 2,2′-azino-bis(3-ethylbenzothiazoline-6-sulfonic acid), neocuproine, 2,4,6-Tri(2-pyridyl)-s-triazine, trolox, Trizma® Base, Trizma® hydrochloride, butyrylcholine iodide, acetylcholine iodide, acetylcholinesterase, butyrylcholinesterase, 5,5-dithiobis-2-nitrobenzoic acid, tyrosinase, galantamine, azelaic acid were purchased from Sigma-Aldrich (Schnelldorf, Germany). Sodium chloride, sodium dihydrogen phosphate, sodium hydrogen phosphate, and dimethyl sulfoxide were obtained from Avantor Performance Materials (Gliwice, Poland). Ammonium acetate, an analytical weighed amount of HCl, 1 N, and methanol were supplied by Chempur (Piekary Śląskie, Poland). Cupric chloride dihydrate, acetic acid (99.5%), and ethanol (96%) were supplied by POCH (Gliwice, Poland). Prisma HT, GIT, BBB lipid solution, an acceptor sink buffer, and a brain sink buffer were supplied by Pion Inc. (Forest Row, East Sussex, UK). High-quality pure water was prepared using a Direct-Q 3 UV purification system (Millipore, Molsheim, France; model Exil SA 67120). FaSSIF and FeSSIF were purchased from Biorelevant (London, UK).
2.2. Preparation of the Systems of Cannabis sativa (Henola Variety) Inflorescences Extract-Carriers
The extract of Cannabis sativa inflorescences was obtained using the dynamic supercritical CO2 (scCO2) extraction process (SFT-120, shim-pol, Izabelin, Polska). In total, 6.5 g of dried plant material was placed in the extraction vessel and extracted under 6000 psi at 50 °C with 250 mL of CO2. The extraction yield was calculated as the mass of extract obtained and subjected to drying (to remove any water from the eventually frozen needle) (g) divided by the mass (g) of plant material placed in the extractor and expressed as a percentage (%). The choice of the Henola extract (HiE) was based on the screening studies on three varieties (Białobrzeskie, Tygra, and Henola) of leaves and inflorescences and their neuroprotective potential (data not presented). After extraction, the antioxidant studies and inhibition of enzymes (acetylcholinesterase, butyrylcholinesterase, and tyrosinase) connected with neurodegeneration were repeated.
Next, the extracts were dried in a vacuum at 50 °C, weighed, and suspended in methanol (if the process was repeated to obtain more extract, at this stage the extracts were combined together), winterized, and filtered (
Figure 2). For fluid extracts (HiE), carriers (Neusilin US2, Soluplus, or lactose for apparent solubility study) were added in a 1:1 mass ratio to the earlier weight of the extract. Systems were dried on rota-vapor at 50 °C until dry and grounded in mortar.
2.3. Chromatographic Analysis
The cannabinoid profile (CBD, CBDA, and CBC) of the extract, and during the apparent solubility and permeability study, was analyzed using the ultra-high-performance liquid chromatography with the diode array detector (HPLC-DAD) method, Shimadzu Corp. (Kyoto, Japan). The previously described method was used [
37]. The analysis was conducted on a CORTECS Shield RP18 stationary phase, 2.7 µm; 150 mm × 4.6 mm, with a mobile phase consisting of 0.1% trifluoroacetic acid (41%) and acetonitrile (41:59,
v/
v). The flow rate was set to 2.0 mL/min, and the column temperature was maintained at 35 °C. The injection volume was 10.0 µL, and the detection wavelength was set at 228 nm, with an analysis time of 50 min. The retention times for each cannabinoid were as follows: CBD at approximately 5.83 min, CBDA at approximately 6.42 min, and CBC at 14.57 min. The LabSolutions LC software (version 1.86 SP2) from Shimadzu Corp. (Kyoto, Japan) was used to obtain chromatograms. The method was validated according to ICH guidelines for current research, the validation parameters are collected in
Table S1 (Supplementary Materials).
2.4. Apparent Solubility of Cannabinoids
The dissolution rate was determined in the paddle apparatus (Agilent Technologies, Santa Clara, CA, USA). HiE had a thick, oily consistency, so for the purpose of apparent solubility study it was combined with lactose; the preparation steps were the same as for Neusilin US2 and Soluplus (HiE–control). The systems and control (600 mg) were placed into two gelatin capsules. The capsules were placed into coiled sinkers for floating prevention. The test was carried out in triplicate for 180 min in a pH 1.2 of 0.1 N hydrochloric acid, a pH 6.8 of phosphate buffer, Fasted State Simulated Intestinal Fluid (FaSSIF), and Fed State Simulated Intestinal Fluid (FeSSIF).
FaSSIF and FeSSIF dissolution media are more complex solutions specifically designed to simulate the conditions of the human small intestine under fasted and fed conditions. FaSSIF and FeSSIF contain natural surfactants present in the gut to simulate gastrointestinal fluids much more accurately than conventional dissolution media, and they simulate the conditions of the human intestine in a fasted state and after a meal [
50]. Sodium taurocholate is included to replicate the role of bile acids in facilitating lipid absorption and emulsification. Lecithin is incorporated to mimic the presence of phospholipids, which play a vital role in the formation of mixed micelles that enhance the solubilization of lipophilic compounds. The buffer ensures a stable pH in the intestinal fluid (6.5 for FaSSIF and 5.0 for FeSSIF), and sodium chloride is added to ensure physiological osmolarity (a FaSSIF of 270 Osm/L and FeSSIF of 670 Osm/L) [
51].
The vessels were filled with 500 mL of media at the temperature set at 310.15 K and the rotation speed of 100 rpm. At specific time intervals, 2.0 mL of the sample was taken out and immediately replaced with an equal amount of fresh medium at the same temperature. The percentage cumulative cannabinoid release (% CBD, CBDA, and CBC) was measured at different time points (5, 10, 15, 30, 45, 60, 90, 120, and 180 min) for each formulation. The samples were then passed through a filter with a pore size of 0.22 μm and analyzed using high-performance liquid chromatography (HPLC). Sample chromatograms from the dissolution study are presented in
Figure S1 (Supplementary Materials). The standard deviation (SD) was also calculated for each time point and delivery system.
The differences and similarities between the apparent solubility profiles were determined by the two-factor values,
f1 and
f2, introduced by Moore and Flanner [
52] with the use of the following equations:
where
n is the number of time points,
Rj is the percentage of the reference dissolved substance in the medium,
Tj is the percentage of the dissolved tested substance, and t is the time point. Dissolution profiles are described as similar when the
f1 value is close to 0, or
f2 is close to 100 (between 50 and 100) [
53]. The similarities and dissimilarities between profiles were marked in the figures with letters. If profiles share the same letter, they are similar.
The data from the dissolution studies were graphically correlated to mathematical models: zero-order, first-order, Higuchi’s model, and Korsmeyer–Peppas model in MS Excel (version 1808, Microsoft Corporation, Redmond, WA, USA) [
54,
55]. The mathematical equations of kinetic models are described below:
where F is the fraction of the released drug, k is the constant associated with the release, and t is the time (h).
2.5. Permeability Study of Cannabinoids
The permeability of cannabinoids through biological membranes was measured using the Parallel Artificial Membrane Permeability Assay (PAMPA) model. The study was conducted in the gastrointestinal (GIT) and blood-brain barrier (BBB) models. The model consists of two 96-well microfilter plates, the donor and the acceptor plate. The wells were separated by a 120 μm thick microfilter disc coated with a 20% (
w/
v) dodecane solution of a lecithin mixture (Pion Inc., Billerica, MA, USA). The extract was diluted and the systems were dissolved (or suspended, centrifuged, and filtered) in dimethyl sulfoxide (DMSO) and placed in the donor solutions, which were adjusted to 6.8 for GIT application and pH 7.4 for BBB. The BBB permeability was only studied for extract, as Neusilin US2 does not leave the GIT. The plates were incubated at 310.15 K for 3 h for the GIT and BBB assay in a humidity-saturated atmosphere. After incubation, the plates were separated and the concentration of CBD and CBDA, as their concentration in the extract was the highest, was determined using the HPLC-DAD method. Each measurement was repeated six times. CBC was present in a quantifiable concentration only in the BBB study, thus, it was not determined in GIT conditions. The
Papp was calculated using the following formulas:
where
VD is the donor volume,
VA is the acceptor volume,
Cequilibrium is the equilibrium concentration (
),
S is the membrane area, and
t is the incubation time (in seconds).
Substances with a
Papp in the GIT model below 0.1 × 10
−6 cm/s are considered to have poor permeability, compounds with 0.1 × 10
−6 cm/s ≤
Papp < 1 × 10
−6 cm/s are classified as mediocre permeable, and compounds found as well permeable have a
Papp ≥ 1 × 10
−6 cm/s [
56]. Compounds whose
Papp in the BBB model is <2.0 × 10
−6 cm/s are known as poorly permeable. Compounds with questionable permeability have
Papp values in the range of 2.0 to 4.0 × 10
−6 cm/s. Substances that have a
Papp value greater than 4.0 × 10
−6 cm/s are regarded as highly permeable [
57].
2.6. Biological Activity Studies
The extract and systems antioxidant activity was studied by four assays: DPPH, ABTS, CUPRAC, and FRAP. Two of them determine the ability to scavenge free radicals (DPPH and ABTS), whilst the other assays check the possibility of performing redox reactions (CUPRAC and FRAP). A linear regression equation between the trolox concentration and its scavenging percentage (DPPH and ABTS) or absorbance (CUPRAC and FRAP) was built. Thus, the results, presented as mg trolox/g plant material, were calculated through the equation according to the antioxidant properties of the extracts in all four assays [
58,
59]. Pure excipients showed no antioxidant potential under test conditions.
To perform the DPPH assay, a 96-well plate was used and the samples were measured spectrophotometrically [
60]. The main reagent was a methanol solution of DPPH at a concentration of 0.2 mM. To initiate the assay, 25.0 µL of the system/trolox solution was mixed with 175.0 µL of the DPPH solution. The plate was then incubated in the dark at room temperature while shaking for 30 min. After the incubation period, the absorbances were obtained using a plate reader (Multiskan GO, Thermo Fisher Scientific, Waltham, MA, USA) at 517 nm. The absorbance (A) was also measured for a blank sample, which consisted of a mixture of DPPH solution and solvent at 517 nm. Each sample was tested for its absorbance at 517 nm. The inhibition of DPPH radicals by the studies’ systems/trolox was calculated using the equation:
where
Ao is the absorbance of the control sample and
Ai is the absorbance of the test sample. Each measurement was repeated six times.
As another assay to determine the scavenging radical potential, the ABTS study [
61], was also performed. This study is based on the production of green cation radicals through the loss of electrons by nitrogen atoms of ABTS caused by potassium persulfate. During the assay, the green ABTS radical can be converted into a colorless neutral form in the presence of an antioxidant. In this assay, 200.0 μL of ABTS
•+ solution and 10.0 μL of the system/trolox solution were pipetted into 96-well plates and incubated for 10 min in the dark at room temperature while shaking [
62]. After incubation, the absorbance values were measured at λ = 734 nm using a plate reader (Multiskan GO, Thermo Fisher Scientific, Waltham, MA, USA). The mixture of solvent and ABTS (control) and the wells filled with system and water (systems’ absorbance) at 734 nm were also studied. The inhibition of ABTS
•+ was calculated using the following equation:
where:
A0—The absorbance of the control;
A1—The absorbance of the sample.
To determine the reducing potential of the systems, the CUPRAC assay [
63] was used. In this assay, the antioxidants’ phenolic groups undergo oxidation to form quinones, while the bluish neocuproine and copper (II) ion complex is reduced to the yellow neocuproine and copper (I) ion complex. To perform this study, a mixture of 50.0 µL of the system/trolox solution and 150.0 µL of the CUPRAC reagent was added to the plate and then incubated for 30 min at room temperature while shaking in the dark [
62]. The control and systems’ own absorbance were also measured simultaneously. The absorbance was measured at a wavelength of 450 nm using a plate reader (Multiskan GO, Thermo Fisher Scientific, Waltham, MA, USA) after the 30 min incubation period. The analysis was performed using six replicates.
The FRAP technique was also used to determine the reducing properties of the systems, which involves reducing colorless Fe
3+ ion to Fe
2+ to form a dark blue complex with 2,4,6-tris(2-pyridyl)-1,3,5-triazine (TPTZ) [
62]. In this method, 25.0 µL of the system/trolox solution and 175.0 µL of the FRAP mixture (consisting of 25 mL acetate buffer, 2.5 mL TPTZ solution, and 2.5 mL of FeCl
3·6H
2O solution) were applied to the plate and incubated in dark conditions at 37 °C for 30 min. The control and systems’ absorbance were also measured. Subsequently, the absorbance was measured at λ = 593 nm using a plate reader (Multiskan GO, Thermo Fisher Scientific, Waltham, MA, USA). The analysis was performed using six replicates.
The neuroprotective effect of cannabinoids was assessed against the possibility of inhibiting enzymes whose expression is associated with neurodegenerative changes.
As a standard inhibitor of esterases, galantamine was chosen, while for tyrosinase, azelaic acid was selected [
64,
65]. A linear regression equation that relates the standard concentration of a substance to its ability to inhibit an enzyme, as measured by the percentage of potential inhibition was created. An equation to calculate the standard equivalent for each extract based on its inhibitory properties in all three assays was obtained. The results were presented as a galantamine equivalent (GALAE) (mg galantamine/g plant material) for AChe and BChE assays and as an azelaic acid equivalent (AzAE) (mg azelaic acid/g plant material) [
66,
67,
68,
69,
70,
71].
The inhibition of acetylcholinesterase (AChE) and butyrylcholinesterase (BChE) was carried out using a colorimetric Ellman et al. modified assay [
72]. This method requires artificial substrates (thiocholine esters). Thiocholine is liberated during the enzymatic reactions with 5,5′-dithio-bis-(2-nitrobenzoic) acid (DTNB), and the 3-carboxy-4-nitrothiolate anion (TNB anion) is formed. The potential to inhibit AChE and BChe was measured according to the increase in the thiocholine color in a 96-well plate. In total, 60.0 μL of 0.05 M Tris-HCl buffer (pH of 8.0), 10.0 μL of test solution, and 30.0 μL of AChE/BChE solution at a concentration of 0.2 U/mL were added to the wells. Subsequently, the plate was incubated for 5 min at 37 °C while shaking. Next, 30.0 μL acetylthiocholine iodide (ATCI)/butyrylthiocholine iodide (BTCI) at a concentration of 1.5 mM and 125.0 μL of 0.3 mM DTNB solution (5,5′-dithiobis-(2-nitrobenzoic acid)) were added to the wells. The plate was then incubated for another 20 min under the same conditions. A blank sample (the reaction mixture without the enzyme, with an increase in the volume of Tris-HCl buffer), a control sample (the solvent instead of the test sample), and a blank sample for the control sample (the reaction mixture without the enzyme, with an increase in the volume of Tris-HCl buffer) were also prepared. The measurements were performed at a wavelength of 405 nm. The analysis was performed using six replicates. The percentage of inhibition of AChE and BChE by the test samples was calculated using the following formula:
where:
A1—The absorbance of the test sample;
A1b—The absorbance of the blank of the test sample;
A0—The absorbance of control;
A0b—The absorbance of the blank of control.
The tyrosinase inhibition assay measures the activity of an inhibitor to prevent L-DOPA from accessing the tyrosinase active site. This leads to a decrease in the color intensity of the solution, which indicates enzyme inhibition [
73]. To conduct the assay, 75.0 μL of 0.1 M phosphate buffer (pH 6.8) was added to each well of a 96-well plate, followed by 25.0 μL of the extract and 50.0 μL of enzyme solution (192 U/mL). The plate was shaken at room temperature for 10 min, after which 50 μL of 2.0 mM L-DOPA was added to each well and incubated for an additional 20 min under the same conditions. In addition to the test sample, a blank for the test sample (without enzyme, the volume of phosphate buffer was elevated), a control sample (with solvent instead of the test sample), and a blank sample for the control (without enzyme) were also prepared. The absorbance of the samples was measured at 475 nm. Each measurement was repeated six times. The percentage inhibition of the tyrosinase by the samples was calculated using an equation:
where:
A1—The absorbance of the test sample;
A1b—The absorbance of the blank of the test sample;
A0—The absorbance of control;
A0b—The absorbance of the blank of control.
2.7. Statistical Analysis
Statistical analysis of results obtained in permeability assay, and in antioxidant activity study, was performed with the use of Statistica 13.3 software (StatSoft Poland, Krakow, Poland). Data are presented as mean values ± standard deviations. Experimental data were analyzed using the skewness and kurtosis tests to determine the normality of each distribution, and Levene’s test assessed the equality of variances. Statistical significance was determined using a one-way analysis of variance (ANOVA), followed by the Bonferroni post hoc test (to compare the experimental results acquired for cannabinoids in extract and in the systems). Differences were considered significant at p < 0.05.
4. Discussion
Henola inflorescences were extracted with scCO
2. scCO
2 extraction is widely recognized as a green extraction method. CO
2 functions as a non-polar solvent, and in its supercritical state, it is a good choice for efficiently extracting lipophilic compounds like cannabinoids from plant material [
84]. Its selectivity, safety, and environmentally friendly characteristics further contribute to its suitability for this purpose [
85,
86]. Furthermore, the use of CO
2 as a solvent eliminates the need for harsh organic solvents, resulting in a pure extract without the risk of residual solvent contamination [
87,
88,
89]. scCO
2 extraction is particularly advantageous for extracting cannabinoids from cannabis plant material due to the lipophilic character of these compounds. In its supercritical state, CO
2 exhibits both gas-like diffusion and liquid-like solvency, allowing it to penetrate the plant matrix efficiently and dissolve target compounds [
90]. Alcohol extraction is a common method for cannabinoids, extracting a wide range of compounds, but it may also pull undesirable components like chlorophyll and is considered a less environmentally friendly method than scCO
2 [
91]. Hydrocarbon extraction offers high yields due to its strong solvent power, yet it poses safety risks due to flammable solvents and requires extensive post-extraction purification [
91]. Unlike solvent-based techniques, such as ethanol or hydrocarbon extraction, scCO
2 is a non-toxic solvent that leaves no residual solvents in the final product, ensuring the purity and safety of extracted cannabinoids. Co-dispersion delivery systems of HiE with Neusilin US2 and Soluplus were prepared with a solvent-evaporation technique, which is a relatively simple, cost-effective, and scalable method [
92]. The straightforward nature of the method allows for efficient and cost-effective production of bulk quantities of the desired systems, making it suitable for various industrial applications including pharmaceuticals, cosmetics, and materials engineering. An important aspect was obtaining co-dispersions in powder form for a future oral formulation, which was provided by both Neusilin US2 and Soluplus.
CBD, CBDA, and CBC from HiE did not dissolve in the pharmacopeial media (pH 1.2 and 6.8) as 1% of dissolution was not exceeded in any case within 180 min of the study. Considering CBDA’s approximate pKa value of 2.9 [
93], CBDA primarily exists in its acidic form under both acidic (pH 1.2) and neutral (pH 6.8) conditions. The improved dissolution rate at pH 6.8 suggests that the neutral environment favors CBDA solubility and release. The approximate pKa value of CBC is around 9.5–10.3 [
94], and it is similar to CBD (pKa 9.3–10.3 [
94,
95]). In the highly acidic environment of pH 1.2, CBC exhibited a similarly low dissolution rate compared to CBD and CBDA. These results suggest that CBC, like CBD and CBDA, has limited solubility and dissolution in highly acidic conditions, which may be attributed to its weakly basic nature. In a phosphate buffer at pH 6.8, CBC demonstrated improved dissolution rates compared to pH 1.2, suggesting enhanced solubility in more neutral environments. In view of the literature reports, the decomposition of cannabinoids in an acidic environment during this study cannot be ruled out [
96]. It can, therefore, be assumed that such a low percentage of cannabinoid release in acidic conditions might be due to the poor solubility in the stomach environment, but also due to the degradation of the CBD, CBDA, or CBC.
The solubility and dissolution behavior of cannabinoids, such as CBD, CBDA, and CBC, can vary significantly depending on the pH of the surrounding environment and the presence of specific surfactants. This is visible in the case of the dissolution of cannabinoids from HiE before co-dispersion delivery systems preparation in FaSSIF and FeSSIF as they reached 20–31% and 37–40%, respectively. The dissolution profile of cannabinoids was notably higher in both FaSSIF and FeSSIF compared to the pharmacopeial media. This indicates that the presence of natural surfactants present in FaSSIF and FeSSIF better simulates the complex environment of the gut, leading to a more efficient release of CBD, CBDA, and CBC. Surfactants are amphiphilic molecules, meaning they have both hydrophobic and hydrophilic regions. The presence of surfactants in the solution can help solubilize cannabinoids by forming micelles or emulsions. What is more important, the better solubility of cannabinoids in post-meal conditions was indicated, which was also proven in other studies [
97]. The increase in the bioaccessibility of CBD with food could be explained by the fact that micelle formation from hydrolyzed lipids aids in the bioaccessibility of hydrophobic molecules [
98]. How cannabinoids are administered, as well as the meal with which they are taken, is a very important aspect to receive the appropriate pharmacological response.
An increase in apparent solubility of cannabinoids was obtained due to co-dispersion delivery systems with Neusilin US2 and Soluplus. Neusilin US2 is a type of synthetic magnesium aluminosilicate which is a porous material with a significant surface area, porosity, and adsorption capacity. Its structure consists of a three-dimensional network of interconnected particles with numerous pores and channels. When Neusilin US2 is in contact with water, its porous structure can adsorb hydrophobic molecules like cannabinoids onto its surface or within its pores [
99]. This adsorption effectively increases the apparent solubility of the cannabinoids by creating a reservoir of the drug in a more readily available form. The layered structure allows the material to have both hydrophilic and hydrophobic regions [
100]. This dual nature is advantageous for its adsorption capabilities. The hydrophilic regions can interact with water molecules, while the hydrophobic regions can interact with hydrophobic compounds such as cannabinoids (CBD, CBDA, and CBC). Neusilin might also form complexes as a result of acid–base reactions, ion–dipole interactions, and hydrogen bonding [
101].
The greatest results were, however, obtained for the co-dispersion delivery systems with Soluplus, which has an amphiphilic graft copolymer structure comprising three main components: polyvinyl caprolactam, polyvinyl acetate, and polyethylene glycol [
102]. The polyvinyl caprolactam and polyvinyl acetate segments contribute to the polymer’s lipophilic properties, while the PEG segment imparts hydrophilicity [
42]. This arrangement allows Soluplus to self-assemble into micelles when placed in an aqueous environment, effectively encapsulating hydrophobic cannabinoids within the micellar core [
103]. The polyethylene glycol component in the structure also has a steric stabilizing effect on the micelles [
104]. The hydrophilic segments of Soluplus might face outward, interacting with the surrounding water molecules, while the lipophilic segments interact with the cannabinoids, promoting their dispersion within the micelles. Cannabinoids might interact with Soluplus by the formation of hydrogen bonds with their hydroxyl groups [
44].
In the literature, in vitro release profiles of CBD and zein and zein-WP nanoparticles in simulated gastric fluid (SGF) and simulated intestinal fluid (SIF) are provided [
105]. The free CBD has low bioaccessibility, and only 29% of CBD was detected after SIF digestion. CBD, zein, and zein-WP nanoparticles showed lower sustained release during simulated gastric fluid. Pure CBD has a low solubility profile in both SIF and SGF, with less than 3% within 1 h and less than 10% of CBD released in 48 h [
106]. CBD-Silica cast in PVA films show a significantly increased dissolution profile of SIF and SGF, with about 3–7% of CBD released in 1 h and about 40–45% of released CBD in 48 h. Poor solubility of CBD from hemp oil products like oral drops, capsules, and tablets in an acidic medium was also confirmed as 0% of CBD released in FaSSGF, besides one beverage enhancer [
107]. Koch et al. [
108] conducted a study on the dissolution properties of CBD formulations in a phosphate buffer with a pH of 6.8 and 0.5% sodium lauryl sulfate. They discovered that CBD-cyclodextrin formulations processed through freeze-drying or spray-drying, as well as CBD-mesoporous silica formulations processed through subcritical CO
2 or atmospheric impregnation exhibited a considerable increase in their ability to dissolve in water. The study highlighted Kollidon
® VA64 as the excipient that displayed the greatest improvement in aqueous solubility. However, these studies are based on pure CBD, not on extracts, where there is no possible entourage effect between components of the extract. To the best of the authors’ knowledge, the release profiles for CBDA and CBC were studied for the first time.
In the current study, the differences in CBD, CBDA, and CBC profiles were mostly noticeable at the beginning of the studies, determining the speed of dissolution of cannabinoids, as well as increasing their dissolution rate, which is very important as orally administered preparations have the latest onset of action compared to other routes of administration, which can be accelerated by orally administered systems with e.g., Soluplus.
Delivery systems are also prepared to enhance the solubility and permeability of various compounds as it is presented in the literature [
109,
110,
111]. The higher solubility of CBD and CBDA led to more efficient absorption and permeability across the gastrointestinal tract. The improved dissolution rate, increased concentration gradient, and enhanced transport contribute to the higher permeability coefficient observed in the systems compared to the pure extract in the PAMPA study. Achieving higher gastrointestinal permeability is crucial for obtaining higher oral bioavailability as it allows for more efficient absorption into the bloodstream from the gastrointestinal tract.
Oxidative stress occurs when there is an imbalance between the production of reactive oxygen species (ROS) and the body’s ability to detoxify them. While some ROS play important roles in cellular signaling and immune function, excess ROS can damage cellular components such as proteins, lipids, and DNA. Oxidative damage has been linked to several chronic diseases such as cancer, cardiovascular disease, and neurodegenerative disorders. Antioxidants neutralize harmful free radicals in the body and reduce inflammation, support the immune system, protect the brain, slow down the aging process, and improve cardiovascular health. These compounds can help protect neurons from oxidative damage, reduce inflammation, and promote cell survival, which can slow down or prevent the progression of neurodegenerative diseases. Cannabinoids exhibit various mechanisms of antioxidant properties [
112]. The phenolic hydroxyl groups present in cannabinoid structures play a role in scavenging free radicals [
113]. HiE antioxidant activity was slightly improved after preparing co-dispersion delivery systems; however, the changes were often not statistically significant. Similar results were observed for the inhibition of the enzymes related to neuroprotection. The increased solubility of secondary plant metabolites might have influenced their biological activity; however, this phenomenon does not always occur [
114].