Engagement in Healthcare Systems: Adopting Digital Tools for a Sustainable Approach
Abstract
:1. Introduction
2. Literature Review
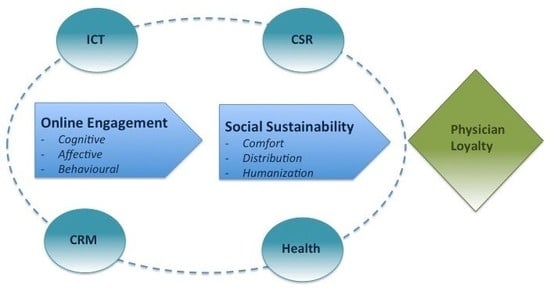
3. Theoretical Framework
- (a)
- Customer engagement in health engagement platforms defined as touch points that allow individuals to integrate resources and co-create value with each other and the firm beyond purchase [4,29,32,50], and identified through the cognitive component, which referred to the cognitive processing activated by the customer of the brand/organization during the consumer/brand interaction [51]; the affective component refers to the degree of affection that the consumer has for the brand in the consumer–brand/organization interaction [51], and the behavioral component is defined as the time, energy, and effort that a consumer spends on the brand/organization during the consumer–brand interaction [51].
- (b)
- Social sustainability is defined as a genuine and credible long-term engagement in all business activities that are lived with consciousness and responsibility [52]. In this paper, we adapted the social sustainability scale used by Capolongo et al. [53] and Buffoli et al. [45] to measure social sustainability in health engagement platforms. This construct is identified through the “distribution” component (which considers the efficiency of the access paths and distribution of health engagement platform), the “comfort” component (which considers the online health environment through qualitative data such as quality and usefulness of information, inclusiveness of information), and the “humanization” component (regarding the relationship between the patient and doctors, social aspects, safety and security, collaboration, and wellness perception in the engagement platform).
- (c)
- User satisfaction is referred to “as a customer’s overall evaluation of the performance experienced with an engagement platform and is viewed as a consequence of customer engagement within the engagement platform” [32].
- (d)
- Physician loyalty in the engagement platform context, defined not only as retention, but also “as behavioral intention to continuously use engagement platforms with their present service providers as well as their inclinations to recommend this tool to others” [32] (p. 692). In the following sub sections, the research hypotheses are detailed and the theoretical assumptions underlying the relationships between the analytical constructs are described.
3.1. Influence on Social Sustainability of Engagement in Digital Health Platforms
3.2. Social Sustainability and Engagement in Physician Loyalty
4. Methodology
Measurement Development
5. Results
5.1. Descriptive Analysis of Sample
5.2. Effect of Engagement Dimensions on Social Sustainability and Loyalty
6. Discussion
Limitations
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
Ethical Approval
Informed Consent
References
- De Rosis, S.; Barsanti, S. Patient satisfaction, e-health and the evolution of the patient–general practitioner relationship: Evidence from an Italian survey. Health Policy 2016, 120, 1279–1292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Graves, M.; Doucet, S.; Dubé, A.; Johnson, M. Health professionals’ and patients’ perceived barriers and facilitators to collaborating when communicating through the use of information and communication technologies. J. Interprof. Educ. Pract. 2018, 10, 85–91. [Google Scholar] [CrossRef]
- Papa, A.; Mital, M.; Pisano, P.; Del Giudice, M. E-health and wellbeing monitoring using smart healthcare devices: An empirical investigation. Technol. Forecast. Soc. Chang. 2018. [Google Scholar] [CrossRef]
- Breidbach, C.F.; Brodie, R.J. Engagement platforms in the sharing economy: Conceptual foundations and research directions. J. Serv. Theory Pract. 2017, 27, 761–777. [Google Scholar] [CrossRef]
- Viglia, G.; Pera, R.; Bigné, E. The determinants of stakeholder engagement in digital platforms. J. Bus. Res. 2018, 89, 404–410. [Google Scholar] [CrossRef]
- Driessen, P.H.; Kok, R.A.W.; Hillebrand, B. Mechanisms for stakeholder integration: Bringing virtual stakeholder dialogue into organizations. J. Bus. Res. 2013, 66, 1465–1472. [Google Scholar] [CrossRef] [Green Version]
- McColl-Kennedy, J.R.; Vargo, S.L.; Dagger, T.S.; Sweeney, J.C.; van Kasteren, Y. Health Care Customer Value Cocreation Practice Styles. J. Serv. Res. 2012, 15, 370–389. [Google Scholar] [CrossRef]
- Fiksdal, A.S.; Kumbamu, A.; Jadhav, A.S.; Cocos, C.; Nelsen, L.A.; Pathak, J.; McCormick, J.B. Evaluating the process of online health information searching: A qualitative approach to exploring consumer perspectives. J. Med. Internet Res. 2014, 16, e224. [Google Scholar] [CrossRef]
- Peine, A.; Moors, E.H.M. Valuing health technology—Habilitating and prosthetic strategies in personal health systems. Technol. Forecast. Soc. Chang. 2015, 93, 68–81. [Google Scholar] [CrossRef]
- Zhao, J.; Wang, T.; Fan, X. Patient value co-creation in online health communities: Social identity effects on customer knowledge contributions and membership continuance intentions in online health communities. J. Serv. Manag. 2015, 26, 72–96. [Google Scholar] [CrossRef]
- Osei-Frimpong, K.; Wilson, A.; Lemke, F. Patient co-creation activities in healthcare service delivery at the micro level: The influence of online access to healthcare information. Technol. Forecast. Soc. Chang. 2018, 126, 14–27. [Google Scholar] [CrossRef] [Green Version]
- Cotten, S.R.; Gupta, S.S. Characteristics of online and offline health information seekers and factors that discriminate between them. Soc. Sci. Med. 2004, 59, 1795–1806. [Google Scholar] [CrossRef] [PubMed]
- Osei-Frimpong, K.; Wilson, A.; Owusu-Frimpong, N. Service experiences and dyadic value co-creation in healthcare service delivery: A CIT approach. J. Serv. Theory Pract. 2015, 25, 443–462. [Google Scholar] [CrossRef]
- Bitner, M.J.; Booms, B.H.; Tetreault, M.S. The Service Encounter: Diagnosing Favorable and Unfavorable Incidents. J. Mark. 1990, 54, 71. [Google Scholar] [CrossRef]
- Wilkin, C.L.; Campbell, J.; Moore, S.; Simpson, J. Creating value in online communities through governance and stakeholder engagement. Int. J. Account. Inf. Syst. 2018, 30, 56–68. [Google Scholar] [CrossRef]
- Barrett, M.I.; Orlikowski, W.J. Creating value in online communities: The sociomaterial configuring of strategy, platform, and stakeholder engagement. Inf. Syst. Res. 2016, 27, 704–723. [Google Scholar] [CrossRef]
- Barile, S.; Saviano, M. Complexity and Sustainability in Management: Insights from a Systems Perspective. In Social Dynamics in a Systems Perspective; Barile, S., Pellicano, M., Polese, M., Eds.; Springer: Cham, Switzerland, 2018; pp. 39–63. [Google Scholar]
- Barile, S.; Quattrociocchi, B.; Calabrese, M.; Iandolo, F. Sustainability and the viable systems approach: Opportunities and issues for the governance of the territory. Sustainability 2018, 10, 790. [Google Scholar] [CrossRef]
- Hajli, M.N. Developing online health communities through digital media. Int. J. Inf. Manag. 2014, 34, 311–314. [Google Scholar] [CrossRef]
- Polese, F.; Botti, A.; Grimaldi, M.; Monda, A.; Vesci, M. Social innovation in smart tourism ecosystems: How technology and institutions shape sustainable value co-creation. Sustainability 2018, 10, 140. [Google Scholar] [CrossRef]
- Testa, M.; Malandrino, O.; Sessa, M.R.; Supino, S.; Sica, D. Long-term sustainability from the perspective of cullet recycling in the container glass industry: Evidence from Italy. Sustainability 2017, 9, 1752. [Google Scholar] [CrossRef]
- Devin, B.L.; Lane, A.B. Communicating Engagement in Corporate Social Responsibility: A Meta-Level Construal of Engagement. J. Public Relat. Res. 2014, 26, 436–454. [Google Scholar] [CrossRef]
- Font, X.; Guix, M.; Bonilla-Priego, M.J. Corporate social responsibility in cruising: Using materiality analysis to create shared value. Tour. Manag. 2016, 53, 175–186. [Google Scholar] [CrossRef]
- Sloan, P. Redefining stakeholder Engagement: From Control to Collaboration. J. Corp. Citizsh. 2009, 39, 25–40. [Google Scholar]
- Lawrence, A.T. The drivers of stakeholder engagement. J. Corp. Citizsh. 2002, 6, 71–85. [Google Scholar] [CrossRef]
- Greenwood, M. Stakeholder Engagement: Beyond the Myth of Corporate Responsibility. J. Bus. Ethics 2007, 74, 315–327. [Google Scholar] [CrossRef]
- Manetti, G. The quality of stakeholder engagement in sustainability reporting: Empirical evidence and critical points. Corp. Soc. Responsib. Environ. Manag. 2011, 18, 110–122. [Google Scholar] [CrossRef]
- Paine, K.D. Measure What Matters: Online Tools for Understanding Customers, Social Media, Engagement, and Key Relationships; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Breidbach, C.F.; Brodie, R.; Hollebeek, L. Beyond virtuality: From engagement platforms to engagement ecosystems. Manag. Serv. Qual. 2014, 24, 592–611. [Google Scholar] [CrossRef]
- Vargo, S.L.; Lusch, R.F. Service-dominant logic: Continuing the evolution. J. Acad. Mark. Sci. 2008, 36, 1–10. [Google Scholar] [CrossRef]
- Mustak, M.; Jaakkola, E.; Halinen, A. Customer participation and value creation: A systematic review and research implications. Manag. Serv. Qual. 2013, 23, 341–359. [Google Scholar] [CrossRef]
- Marino, V.; Lo Presti, L. Engagement, satisfaction and customer behavior-based CRM performance. J. Serv. Theory Pract. 2018, 28, 682–707. [Google Scholar] [CrossRef]
- Ramaswamy, V.; Ozcan, K. Brand value co-creation in a digitalized world: An integrative framework and research implications. Int. J. Res. Mark. 2016, 33, 93–106. [Google Scholar] [CrossRef]
- Ind, N.; Bjerke, R. The concept of participatory market orientation: An organisation-wide approach to enhancing brand equity. J. Brand Manag. 2007, 15, 135–145. [Google Scholar] [CrossRef]
- Berry, L.L. Cultivating Service Brand Equity. J. Acad. Mark. Sci. 2000, 28, 128–137. [Google Scholar] [CrossRef]
- Brodie, R.J.; Whittome, J.R.M.; Brush, G.J. Investigating the service brand: A customer value perspective. J. Bus. Res. 2009, 62, 345–355. [Google Scholar] [CrossRef]
- Gregory, A. Involving Stakeholders in Developing Corporate Brands: The Communication Dimension. J. Mark. Manag. 2007, 23, 59–73. [Google Scholar] [CrossRef]
- Merz, M.A.; He, Y.; Vargo, S.L. The evolving brand logic: A service-dominant logic perspective. J. Acad. Mark. Sci. 2009, 37, 328–344. [Google Scholar] [CrossRef]
- Dessart, L.; Veloutsou, C.; Morgan-Thomas, A. Consumer engagement in online brand communities: A social media perspective. J. Prod. Brand Manag. 2015, 24, 28–42. [Google Scholar] [CrossRef]
- Hennig-Thurau, T.; Malthouse, E.C.; Friege, C.; Gensler, S.; Lobschat, L.; Rangaswamy, A.; Skiera, B. The impact of new media on customer relationships. J. Serv. Res. 2010, 13, 311–330. [Google Scholar] [CrossRef]
- Jahn, B.; Kunz, W. How to transform consumers into fans of your brand. J. Serv. Manag. 2012, 23, 344–361. [Google Scholar] [CrossRef]
- Raacke, J.; Bonds-Raacke, J.B. MySpace and Facebook: Applying the uses and gratifications theory to exploring friend-networking sites. Cyberpsychol. Behav. 2008, 11, 169–174. [Google Scholar] [CrossRef]
- Baglioni, A.C.S. Ergonomics in planning and reconstruction. G. Ital. Med. Lav. Ergon. 2002, 24, 405–409. [Google Scholar] [PubMed]
- Origgi, L.; Buffoli, M.; Capolongo, S.; Signorelli, C. Light wellbeing in hospital: Research, development and indications. Ann. Ig. 2011, 23, 55–62. [Google Scholar] [PubMed]
- Buffoli, M.; Capolongo, S.; Bottero, M.; Cavagliato, E.; Speranza, S.; Volpatti, L. Sustainable Healthcare: How to assess and improve healthcare structures’ sustainability. Ann. Ig. 2013, 25, 411–418. [Google Scholar] [PubMed]
- Granovetter, M.S. The Stregth of Weak Ties. Am. J. Sociol. 1973, 78, 1360–1380. [Google Scholar] [CrossRef]
- Woodcraft, S. Social Sustainability and New Communities: Moving from Concept to Practice in the UK. Procedia Soc. Behav. Sci. 2012, 68, 29–42. [Google Scholar] [CrossRef] [Green Version]
- Huq, F.A.; Stevenson, M.; Zorzini, M. Social sustainability in developing country suppliers: An exploratory study in the ready made garments industry of Bangladesh. Int. J. Oper. Prod. Manag. 2014, 34, 610–638. [Google Scholar] [CrossRef]
- Hussain, M.; Ajmal, M.M.; Gunasekaran, A.; Khan, M. Exploration of social sustainability in healthcare supply chain. J. Clean. Prod. 2018, 203, 977–989. [Google Scholar] [CrossRef]
- Blasco-Arcas, L.; Hernandez-Ortega, B.L.; Jimenez-Martinez, J. Engagement platforms: The role of emotions in fostering customer engagement and brand image in interactive media. J. Serv. Theory Pract. 2016, 26, 559–589. [Google Scholar] [CrossRef]
- Hollebeek, L.; Glynn, M.S.; Brodie, R.J. Consumer brand engagement in social media: Conceptualisation, scale development and validation. J. Interact. Mark. 2014, 28, 149–165. [Google Scholar] [CrossRef]
- Baumgartner, R.J.; Ebner, D. Corporate sustainability strategies: Sustainability profiles and maturity levels. Sustain. Dev. 2010, 18, 76–89. [Google Scholar] [CrossRef]
- Capolongo, S.; Gola, M.; Di Noia, M.; Nickolova, M.; Nachiero, D.; Rebecchi, A.; Settimo, G.; Vittori, G.; Buffoli, M. Social sustainability in healthcare facilities: A rating tool for analysing and improving social aspects in environments of care. Ann. dell’Istituto Super. Sanità 2016, 52, 15–23. [Google Scholar] [CrossRef]
- Rogers, M. Social sustainability and the art of engagement—The small towns: Big picture experience. Local Environ. 2005, 10, 109–124. [Google Scholar] [CrossRef]
- Max-Neef, M.; Elizalde, A.; Hopenhayn, M. Human Scale Development: Conception, Application and Further Reflections; Apex Press: New York, NY, USA, 1991. [Google Scholar]
- Sarmah, B.; Islam, J.U.; Rahman, Z. Sustainability, social responsibility and value co-creation: A case study based approach. Procedia Soc. Behav. Sci. 2015, 189, 314–319. [Google Scholar] [CrossRef]
- Aquilani, B.; Silvestri, C.; Ioppolo, G.; Ruggieri, A. The challenging transition to bio-economies: Towards a new framework integrating corporate sustainability and value co-creation. J. Clean. Prod. 2018, 172, 4001–4009. [Google Scholar] [CrossRef]
- Arnold, M. Fostering sustainability by linking co-creation and relationship management concepts. J. Clean. Prod. 2017, 140, 179–188. [Google Scholar] [CrossRef]
- Kohli, R.; Piontek, F.; Ellington, T.; VanOsdol, T.; Shepard, M.; Brazel, G. Managing customer relationships through E-business decision support applications: A case of hospital–physician collaboration. Decis. Support. Syst. 2001, 32, 171–187. [Google Scholar] [CrossRef]
- Adams, S.A. Blog-based applications and health information: Two case studies that illustrate important questions for Consumer Health Informatics (CHI) research. Int. J. Med. Inform. 2010, 79, e89–e96. [Google Scholar] [CrossRef] [PubMed]
- Adams, S.A. Revisiting the online health information reliability debate in the wake of “web 2.0”: An inter-disciplinary literature and website review. Int. J. Med. Inform. 2010, 79, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Murray, E.; Lo, B.; Pollack, L.; Donelan, K.; Catania, J.; White, M.; Zapert, K.; Turner, R. The impact of health information on the internet on the physician-patient relationship: Patient perceptions. Arch. Intern. Med. 2003, 163, 1727–1734. [Google Scholar] [CrossRef] [PubMed]
- Ciasullo, M.V.; Polese, F.; Troisi, O.; Carrubbo, L. How Service Innovation Contributes to Co-Create Value in Service Networks. In Exploring Services Science; Borangiu, T., Dragoicea, M., Nóvoa, H., Eds.; Springer: Cham, Switzerland, 2016; Volume 247. [Google Scholar]
- Conti, L. La sanità avrà il suo New Deal. L’Infermiere 2006, 5, 2–3. Available online: http://www.fnopi.it/archivio_news/download/615_1302201735_173.pdf (accessed on 25 November 2018).
- Garcés, J.; Ródenas, F.; Sanjosé, V. Towards a new welfare state: The social sustainability principle and health care strategies. Health Policy 2003, 65, 201–215. [Google Scholar] [CrossRef]
- Collins, E.; Kearins, K.; Roper, J. The risks of relying on stakeholder engagement for the achievement of sustainability. Electr. J. Radic. Org. Theory 2005, 9, 81–101. [Google Scholar]
- Sirgy, M.J. Theoretical perspectives guiding QOL indicator projects. Soc. Indic. Res. 2011, 103, 1–22. [Google Scholar] [CrossRef]
- Bowden, J.L.H. The Process of Customer Engagement: A Conceptual Framework. J. Mark. Theory Pract. 2009, 17, 63–74. [Google Scholar] [CrossRef]
- Tsai, W.H.S.; Men, R.L. Social messengers as the new frontier of organization-public engagement: A WeChat study. Public Relat. Rev. 2018, 44, 419–429. [Google Scholar] [CrossRef]
- Bowden, J. Customer Engagement: A Framework for Assessing Customer-Brand Relationships: The Case of the Restaurant Industry. J. Hosp. Mark. Manag. 2009, 18, 574–596. [Google Scholar] [CrossRef]
- Deng, Z.; Lu, Y.; Wei, K.K.; Zhang, J. Understanding customer satisfaction and loyalty: An empirical study of mobile instant messages in China. Int. J. Inf. Manag. 2010, 30, 289–300. [Google Scholar] [CrossRef]
- Dovaliene, A.; Masiulyte, A.; Piligrimiene, Z. The relations between customer engagement, perceived value and satisfaction: The case of mobile applications. Procedia Soc. Behav. Sci. 2015, 213, 659–664. [Google Scholar] [CrossRef]
- Kim, Y.H.; Kim, D.J.; Wachter, K. A study of Mobile User Engagement (MoEN): Engagement motivations, perceived value, satisfaction, and continued engagement intention. Decis. Support Syst. 2013, 56, 361–370. [Google Scholar] [CrossRef]
- Wang, Y.; Po Lo, H.; Chi, R.; Yang, Y. An integrated framework for customer value and customer-relationship-management performance: A customer-based perspective from China. Manag. Serv. Qual. Int. J. 2004, 14, 169–182. [Google Scholar] [CrossRef]
- Todres, L.; Galvin, K.T.; Holloway, I. The humanization of healthcare: A value framework for qualitative research. Int. J. Qual. Stud. Health Well-Being 2009, 4, 68–77. [Google Scholar] [CrossRef] [Green Version]
- Ugolini, M.; Rossato, C.; Baccarani, C. A five-senses perspective to quality in hospitals. TQM J. 2014, 26, 284–299. [Google Scholar] [CrossRef]
- Barile, S.; Orecchini, F.; Saviano, M.; Farioli, F. People, technology, and governance for sustainability: The contribution of systems and cyber-systemic thinking. Sustain. Sci. 2018, 13, 1197–1208. [Google Scholar] [CrossRef]



| Index | M | DS | Min | Max |
|---|---|---|---|---|
| Cognitive processing | 4.45 | 1.36 | 4.07 | 4.84 |
| Affection | 3.76 | 1.54 | 3.58 | 4.24 |
| Activation | 3.48 | 1.52 | 3.63 | 3.56 |
| Satisfaction | 4.63 | 1.32 | 4.46 | 4.74 |
| Physician loyalty | 4.61 | 1.41 | 4.59 | 4.78 |
| Comfort | 5.16 | 1.17 | 5.09 | 5.22 |
| Distribution | 5.06 | 1.15 | 4.81 | 5.26 |
| Humanization | 4.95 | 1.20 | 4.85 | 5.12 |
| Variable | Count | % | |
|---|---|---|---|
| Gender | Female | 56 | 19 |
| Male | 239 | 81 | |
| Age | <25 | 0 | 0 |
| 25–35 | 5 | 1.7 | |
| 36–45 | 4 | 1.4 | |
| 46–55 | 41 | 13.9 | |
| 56–65 | 144 | 48.8 | |
| >65 | 101 | 34.2 | |
| Use of engagement platform | <1 | 14 | 4.7 |
| 1 year | 29 | 9.8 | |
| 2 years | 32 | 10.8 | |
| >2 years | 220 | 74.6 | |
| Physician’s qualification | |||
| General medicine | 33 | 11.3 | |
| Pediatrics | 26 | 8.9 | |
| Surgery | 19 | 6.5 | |
| Cardiology | 19 | 6.5 | |
| Gastroenterology and endocrinology | 14 | 4.8 | |
| Psychiatry and psychotherapy | 13 | 4.4 | |
| Neurology | 12 | 4.1 | |
| Geriatrics | 7 | 2.4 | |
| Gynecology | 9 | 3.1 | |
| Others | 111 | 37.9 | |
| Cell empty | 30 | 10.2 |
| Model 1 * | Model 2 ** | Model 3 *** | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Comfort | Distribution | Humanization | |||||||
| Standardized Coefficient | t | Sig. | Standardized Coefficients | t | Sig. | Standardized Coefficients | t | Sig. | |
| (Constant) | 7.932 | 8.447 | 7.724 | ||||||
| Cognitive processing | 0.512 | 6.537 | 0.000 *** | 0.405 | 5.180 | 0.000 *** | 0.365 | 4.791 | 0.000 *** |
| Affection | 0.117 | 1.278 | 0.202 | 0.228 | 2.493 | 0.013 ** | 0.266 | 2.998 | 0.003 *** |
| Activation | 128 | 1.734 | 0.084 * | 0.131 | 1.775 | 0.077 * | 0.156 | 2.168 | 0.031 ** |
| Age | 0.009 | 0.221 | 0.825 | 0.019 | 0.431 | 0.667 | 0.009 | 0.223 | 0.824 |
| Gender | −0.021 | −0.491 | 0.624 | −0.050 | −1.151 | 0.251 | −0.049 | −1.172 | 0.242 |
| Adjusted R2 | 0.507 | 0.508 | 0.535 |
| Model 4 **** | |||
|---|---|---|---|
| Physician Loyalty | |||
| Standardized Coefficients | t | Sig. | |
| (Constant) | 0.195 | ||
| Cognitive processing | −0.015 | −0.240 | 0.811 |
| Affection | 0.257 | 3.747 | 0.000 *** |
| Activation | 0.080 | 1.389 | 0.166 |
| Age | −0.013 | −0.413 | 0.680 |
| Gender | 0.014 | 0.432 | 0.666 |
| Comfort | 0.120 | 1.474 | 0.142 |
| Distribution | 0.048 | 0.495 | 0.621 |
| Humanization | 0.157 | 1.993 | 0.047 ** |
| Satisfaction | 0.310 | 4.571 | 0.000 *** |
| Adjusted R2 | 0.734 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lo Presti, L.; Testa, M.; Marino, V.; Singer, P. Engagement in Healthcare Systems: Adopting Digital Tools for a Sustainable Approach. Sustainability 2019, 11, 220. https://doi.org/10.3390/su11010220
Lo Presti L, Testa M, Marino V, Singer P. Engagement in Healthcare Systems: Adopting Digital Tools for a Sustainable Approach. Sustainability. 2019; 11(1):220. https://doi.org/10.3390/su11010220
Chicago/Turabian StyleLo Presti, Letizia, Mario Testa, Vittoria Marino, and Pierpaolo Singer. 2019. "Engagement in Healthcare Systems: Adopting Digital Tools for a Sustainable Approach" Sustainability 11, no. 1: 220. https://doi.org/10.3390/su11010220
APA StyleLo Presti, L., Testa, M., Marino, V., & Singer, P. (2019). Engagement in Healthcare Systems: Adopting Digital Tools for a Sustainable Approach. Sustainability, 11(1), 220. https://doi.org/10.3390/su11010220