The Effects of a Brief Lifestyle Intervention on the Health of Overweight Airline Pilots during COVID-19: A 12-Month Follow-Up Study
Abstract
:1. Introduction
2. Materials and Methods
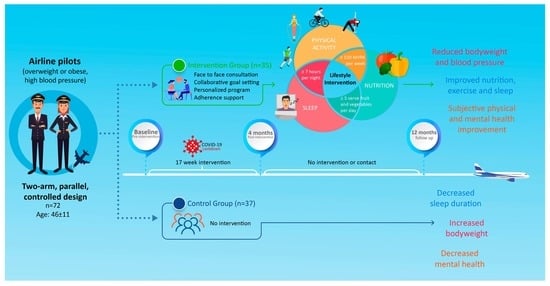
2.1. Design
2.2. Intervention Timing
2.3. Participants
2.4. Intervention Group
2.5. Control Group
2.6. Outcome Measures
2.7. Statistical Analysis
3. Results
3.1. Baseline Characteristics of the Study Population
3.2. Intervention Adherence
3.3. Body Mass, BMI, BP, and Pulse
3.4. Health Behaviors and Self-Rated Health
3.5. Additional Analysis: Four-Month Post-Intervention to 12-Month Follow-Up Change
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Dube, K.; Nhamo, G.; Chikodzi, D. COVID-19 pandemic and prospects for recovery of the global aviation industry. J. Air Transp. Manag. 2021, 92, 102022. [Google Scholar] [CrossRef]
- Sobieralski, J.B. COVID-19 and airline employment: Insights from historical uncertainty shocks to the industry. Transp. Res. Interdiscip. Perspect. 2020, 5, 100123. [Google Scholar] [CrossRef]
- Parmet, W.E.; Sinha, M.S. Covid-19—The law and limits of quarantine. N. Engl. J. Med. 2020, 382, e28. [Google Scholar] [CrossRef]
- McBride, E.; Arden, M.A.; Chater, A.; Chilcot, J. The impact of COVID-19 on health behaviour, well-being, and long-term physical health. Br. J. Health Psychol. 2021, 26, 259–270. [Google Scholar] [CrossRef] [PubMed]
- Douglas, M.; Katikireddi, S.V.; Taulbut, M.; McKee, M.; McCartney, G. Mitigating the wider health effects of covid-19 pandemic response. BMJ 2020, 369, m1557. [Google Scholar] [CrossRef]
- Hamer, M.; Kivimäki, M.; Gale, C.R.; Batty, G.D. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK. Brain Behav. Immun. 2020, 87, 184–187. [Google Scholar] [CrossRef] [PubMed]
- Naja, F.; Hamadeh, R. Nutrition amid the COVID-19 pandemic: A multi-level framework for action. Eur. J. Clin. Nutr. 2020, 74, 1117–1121. [Google Scholar] [CrossRef] [Green Version]
- Naughton, F.; Ward, E.; Khondoker, M.; Belderson, P.; Marie Minihane, A.; Dainty, J.; Hanson, S.; Holland, R.; Brown, T.; Notley, C. Health behaviour change during the UK COVID-19 lockdown: Findings from the first wave of the C-19 health behaviour and well-being daily tracker study. Br. J. Health Psychol. 2021, 26, 624–643. [Google Scholar] [CrossRef] [PubMed]
- Herle, M.; Smith, A.D.; Bu, F.; Steptoe, A.; Fancourt, D. Trajectories of eating behavior during COVID-19 lockdown: Longitudinal analyses of 22,374 adults. Clin. Nutr. ESPEN 2021, 42, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Abascal, E.G.; Martín-Díaz, M.D. Longitudinal study on affect, psychological well-being, depression, mental and physical health, prior to and during the COVID-19 pandemic in Spain. Pers. Individ. Differ. 2021, 172, 110591. [Google Scholar] [CrossRef] [PubMed]
- Ammar, A.; Trabelsi, K.; Brach, M.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of home confinement on mental health and lifestyle behaviours during the COVID-19 outbreak: Insight from the ECLB-COVID19 multicenter study. Biol. Sport 2021, 38, 9–21. [Google Scholar] [CrossRef]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; McDermott, D.; Schuch, F.; Smith, L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc. Med. 2021, 7, e000960. [Google Scholar] [CrossRef]
- Litton, M.; Beavers, A. The Relationship between Food Security Status and Fruit and Vegetable Intake during the COVID-19 Pandemic. Nutrients 2021, 13, 712. [Google Scholar] [CrossRef]
- Jahrami, H.; Bahammam, A.S.; Bragazzi, N.L.; Saif, Z.; Faris, M.; Vitiello, M.V. Sleep problems during the COVID-19 pandemic by population: A systematic review and meta-analysis. J. Clin. Sleep Med. 2021, 17, 299–313. [Google Scholar] [CrossRef]
- Valenzuela, P.L.; Carrera-Bastos, P.; Gálvez, B.G.; Ruiz-Hurtado, G.; Ordovas, J.M.; Ruilope, L.M.; Lucia, A. Lifestyle interventions for the prevention and treatment of hypertension. Nat. Rev. Cardiol. 2021, 18, 251–275. [Google Scholar] [CrossRef]
- Broussard, J.L.; Van Cauter, E. Disturbances of sleep and circadian rhythms: Novel risk factors for obesity. Curr. Opin. Endocrinol. Diabetes Obes. 2016, 23, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A. Obesity and the food environment: Dietary energy density and diet costs. Am. J. Prev. Med. 2004, 27, 154–162. [Google Scholar] [CrossRef]
- Cecchini, M.; Sassi, F.; Lauer, J.A.; Lee, Y.Y.; Guajardo-Barron, V.; Chisholm, D. Tackling of unhealthy diets, physical inactivity, and obesity: Health effects and cost-effectiveness. Lancet 2010, 376, 1775–1784. [Google Scholar] [CrossRef]
- Michalakis, K.; Panagiotou, G.; Ilias, I.; Pazaitou-Panayiotou, K. Obesity and COVID-19: A jigsaw puzzle with still missing pieces. Clin. Obes. 2021, 11, e12420. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Du, S.; Green, W.D.; Beck, M.A.; Algaith, T.; Herbst, C.H.; Alsukait, R.F.; Alluhidan, M.; Alazemi, N.; Shekar, M. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes. Rev. 2020, 21, e13128. [Google Scholar] [CrossRef]
- Tadic, M.; Saeed, S.; Grassi, G.; Taddei, S.; Mancia, G.; Cuspidi, C. Hypertension and COVID-19: Ongoing Controversies. Front. Cardiovasc. Med. 2021, 8, 639222. [Google Scholar] [CrossRef] [PubMed]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Adams Hillard, P.J.; Katz, E.S.; et al. National Sleep Foundation’s updated sleep duration recommendations: Final report. Sleep Health 2015, 1, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Bellavia, A.; Larsson, S.; Bottai, M.; Wolk, A.; Orsini, N. Fruit and vegetable consumption and all-cause mortality: A dose-response analysis. Am. J. Clin. Nutr. 2013, 98, 454–459. [Google Scholar] [CrossRef]
- Cappuccio, F.P.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Sleep Duration and All-Cause Mortality: A Systematic Review and Meta-Analysis of Prospective Studies. Sleep 2010, 33, 585–592. [Google Scholar] [CrossRef]
- Lear, S.A.A.; Hu, W.; Rangarajan, S.; Gasevic, D.; Leong, D.; Iqbal, R.; Casanova, A.; Swaminathan, S.; Anjana, R.M.; Kumar, R.; et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: The PURE study. Lancet 2017, 390, 2643–2654. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Wilson, P.W.; Kannel, W.B. Beyond established and novel risk factors: Lifestyle risk factors for cardiovascular disease. Circulation 2008, 117, 3031–3038. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mandolesi, L.; Polverino, A.; Montuori, S.; Foti, F.; Ferraioli, G.; Sorrentino, P.; Sorrentino, G. Effects of Physical Exercise on Cognitive Functioning and Wellbeing: Biological and Psychological Benefits. Front. Psychol. 2018, 9, 509. [Google Scholar] [CrossRef]
- Walsh, N.P.; Gleeson, M.; Shephard, R.J.; Gleeson, M.; Woods, J.A.; Bishop, N.C.; Fleshner, M.; Green, C.; Pedersen, B.K.; Hoffman-Goetz, L.; et al. Position statement. Part one: Immune function and exercise. Exerc. Immunol. Rev. 2011, 17, 6–63. [Google Scholar] [PubMed]
- Wilson, D.; Driller, M.; Johnston, B.; Gill, N. The effectiveness of a 17-week lifestyle intervention on health behaviors among airline pilots during COVID-19. The effectiveness of a 17-week lifestyle intervention on health behaviors among airline pilots during COVID-19. J. Sport Health Sci. 2021, 10, 333–340. [Google Scholar] [CrossRef]
- Baker, M.G.; Kvalsvig, A.; Verrall, A.J.; Telfar-Barnard, L.; Wilson, N. New Zealand’s elimination strategy for the COVID-19 pandemic and what is required to make it work. N. Z. Med. J. 2020, 133, 10–14. [Google Scholar] [PubMed]
- Ministry of Health. COVID-19 (Novel Coronavirus). 2020 2 July 2020 [Cited 2020 2 July 2020]. Available online: https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus?mega=Our%20work&title=COVID-19 (accessed on 27 April 2021).
- Donnelly, J.E.; Blair, S.N.; Jakicic, J.M.; Manore, M.M.; Rankin, J.W.; Smith, B.K.; American College of Sports Medicine. American College of Sports Medicine Position Stand. Appropriate Physical Activity Intervention Strategies for Weight Loss and Prevention of Weight Regain for Adults. Med. Sci. Sports Exerc. 2009, 41, 459–471. [Google Scholar] [CrossRef]
- Curioni, C.C.; Lourenço, P.M. Long-term weight loss after diet and exercise: A systematic review. Int. J. Obes. 2005, 29, 1168–1174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kulavic, K.; Hultquist, C.N.; McLester, J.R. A Comparison of Motivational Factors and Barriers to Physical Activity Among Traditional Versus Nontraditional College Students. J. Am. Coll. Health 2013, 61, 60–66. [Google Scholar] [CrossRef]
- Weinberg, R. Making Goals Effective: A Primer for Coaches. J. Sport Psychol. Action 2010, 1, 57–65. [Google Scholar] [CrossRef]
- El Assaad, M.A.; Topouchian, J.A.; Asmar, R.G. Evaluation of two devices for self-measurement of blood pressure according to the international protocol: The Omron M5-I and the Omron 705IT. Blood Press. Monit. 2003, 8, 127–133. [Google Scholar] [CrossRef]
- Civil Aviation Authority. Medical Manual Part 3—Clinical Aviation Medicine. 2021 [cited 2021 27/04/2021]. Available online: https://www.aviation.govt.nz/assets/publications/medical-manual/Med_Man_Part-3.pdf (accessed on 27 April 2021).
- Sesso, H.D.; Stampfer, M.J.; Rosner, B.; Hennekens, C.H.; Gaziano, J.M.; Manson, J.E.; Glynn, R.J. Systolic and Diastolic Blood Pressure, Pulse Pressure, and Mean Arterial Pressure as Predictors of Cardiovascular Disease Risk in Men. Hypertension 2000, 36, 801–807. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Methodology Report 2017/18: New Zealand Health Survey 2019 [Cited 2020 1/1/2020]. Available online: https://www.health.govt.nz/publication/methodology-report-2017-18-new-zealand-health-survey (accessed on 27 April 2021).
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Ware, J.E.; Keller, S.D.; Kosinski, M. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales; Health Institute, New England Medical Center: Boston, USA, 1995. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Taylor & Francis Group: Florence, Italy, 1988. [Google Scholar]
- Marchesini, G.; Montesi, L.; El Ghoch, M.; Brodosi, L.; Calugi, S.; Grave, R.D. Long-term weight loss maintenance for obesity: A multidisciplinary approach. Diabetes Metab. Syndr. Obesity Targets Ther. 2016, 9, 37–46. [Google Scholar] [CrossRef] [Green Version]
- Varkevisser, R.D.M.; Van Stralen, M.M.; Kroeze, W.; Ket, J.C.; Steenhuis, I. Determinants of weight loss maintenance: A systematic review. Obes. Rev. 2019, 20, 171–211. [Google Scholar] [CrossRef] [Green Version]
- Middleton, K.R.; Anton, S.D.; Perri, M. Long-Term Adherence to Health Behavior Change. Am. J. Lifestyle Med. 2013, 7, 395–404. [Google Scholar] [CrossRef] [Green Version]
- Lin, A.L.; Vittinghoff, E.; Olgin, J.E.; Pletcher, M.J.; Marcus, G.M. Body Weight Changes During Pandemic-Related Shelter-in-Place in a Longitudinal Cohort Study. JAMA Netw. Open 2021, 4, e212536. [Google Scholar] [CrossRef]
- Bakaloudi, D.R.; Barazzoni, R.; Bischoff, S.C.; Breda, J.; Wickramasinghe, K.; Chourdakis, M. Impact of the first COVID-19 lockdown on body weight: A combined systematic review and a meta-analysis. Clin. Nutr. 2021. [Google Scholar] [CrossRef]
- Houston, S.; Mitchell, S.; Evans, S. Prevalence of cardiovascular disease risk factors among UK commercial pilots. Eur. J. Cardiovasc. Prev. Rehabil. 2011, 18, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Johns, D.J.; Hartmann-Boyce, J.; Jebb, S.A.; Aveyard, P. Diet or Exercise Interventions vs Combined Behavioral Weight Management Programs: A Systematic Review and Meta-Analysis of Direct Comparisons. J. Acad. Nutr. Diet. 2014, 114, 1557–1568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, N.; Stewart, R.A.H.; Benatar, J.R. Intensity and duration of lifestyle interventions for long-term weight loss and association with mortality: A meta-analysis of randomised trials. BMJ Open 2019, 9, e029966. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elmer, P.J.; Obarzanek, E.; Vollmer, W.M.; Simons-Morton, D.; Stevens, V.J.; Young, D.R.; Lin, P.-H.; Champagne, C.; Harsha, D.W.; Svetkey, L.P.; et al. Effects of Comprehensive Lifestyle Modification on Diet, Weight, Physical Fitness, and Blood Pressure Control: 18-Month Results of a Randomized Trial. Ann. Intern. Med. 2006, 144, 485–495. [Google Scholar] [CrossRef]
- Stevens, V.J.; Obarzanek, E.; Cook, N.R.; Lee, I.-M.; Appel, L.J.; West, D.S.; Milas, N.C.; Mattfeldt-Beman, M.; Belden, L.; Bragg, C.; et al. Long-Term Weight Loss and Changes in Blood Pressure: Results of the Trials of Hypertension Prevention, Phase II. Ann. Intern. Med. 2001, 134, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Sheaves, B.; Goodwin, G.M.; Yu, L.-M.; Nickless, A.; Harrison, P.J.; Emsley, R.; Luik, A.I.; Foster, R.G.; Wadekar, V.; et al. The effects of improving sleep on mental health (OASIS): A randomised controlled trial with mediation analysis. Lancet Psychiatry 2017, 4, 749–758. [Google Scholar] [CrossRef] [Green Version]
- Kocevska, D.; Blanken, T.F.; Van Someren, E.J.; Rösler, L. Sleep quality during the COVID-19 pandemic: Not one size fits all. Sleep Med. 2020, 76, 86–88. [Google Scholar] [CrossRef] [PubMed]
- Franceschini, C.; Musetti, A.; Zenesini, C.; Palagini, L.; Scarpelli, S.; Quattropani, M.C.; Lenzo, V.; Freda, M.F.; Lemmo, D.; Vegni, E.; et al. Poor Sleep Quality and Its Consequences on Mental Health During the COVID-19 Lockdown in Italy. Front. Psychol. 2020, 11, 574475. [Google Scholar] [CrossRef]
- MacLean, P.S.; Bergouignan, A.; Cornier, M.; Jackman, M.R. Biology’s response to dieting: The impetus for weight regain. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2011, 301, R581–R600. [Google Scholar] [CrossRef] [Green Version]
- Elfhag, K.; Rossner, S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes. Rev. 2005, 6, 67–85. [Google Scholar] [CrossRef]
- Wakcher, S.; Cross, K.; Blackman, M.C. Personality Comparison of Airline Pilot Incumbents, Applicants, and the General Population Norms on the 16PF. Psychol. Rep. 2003, 92, 773–780. [Google Scholar] [CrossRef]


| Parameters | All Participants (n = 72) | Intervention (n = 35) | Control (n = 37) |
|---|---|---|---|
| Sex (f/m) | 11/61 | 7/28 | 4/33 |
| Age (year) | 45.8 ± 11.1 | 42.8 ± 10.4 | 48.7 ± 11.2 * |
| Height (cm) | 178.6 ± 7.2 | 178.5 ± 8.1 | 178.6 ± 6.3 |
| Body mass (kg) | 90.4 ± 13.9 | 91.7 ± 13.5 | 89.2 ± 14.5 |
| BMI (kg∙m2) | 28.3 ± 3.3 | 28.7 ± 3.3 | 27.9 ± 2.8 |
| Systolic BP (mmHg) | 134.4 ± 11.8 | 138.4 ± 10.6 | 130.6 ± 11.7 |
| Diastolic BP (mmHg) | 84.8 ± 8.3 | 86.7 ± 8.1 | 83.1 ± 8.2 |
| MAP (mmHg) | 101.3 ± 8.5 | 103.9 ± 8.0 | 98.9 ± 8.5 * |
| Pulse (bpm) | 68.7 ± 9.5 | 69.2 ± 7.8 | 68.1 ± 10.9 |
| Hours slept (h/day) | 7.3 ± 0.9 | 7.0 ± 0.8 | 7.6 ± 0.8 * |
| IPAQ-walk (min) | 102.4 ± 58.5 | 69.0 ± 37.9 | 134.0 ± 57.2 * |
| IPAQ-MVPA (min) | 144.5 ± 89.0 | 125.9 ± 79.7 | 162.1 ± 94.7 |
| F&V Intake (serve/day) | 3.5 ± 1.4 | 2.8 ± 1.3 | 4.1 ± 1.1 * |
| PCS-12 (score) | 46.7 ± 6.6 | 42.1 ± 4.1 | 51.1 ± 5.5 * |
| MCS-12 (score) | 49.1 ± 7.5 | 45.3 ± 8.2 | 52.7 ± 4.5 * |
| Short Haul (n, %) | 28 (39%) | 20 (57%) | 8 (22%) * |
| Long Haul (n, %) | 35 (49%) | 13 (37%) | 22 (59%) |
| Mixed Fleet (n, %) | 9 (12%) | 2 (6%) | 7 (19%) |
| Flights during lockdown (n) | 8.0 ± 7.4 | 7.9 ± 7.7 | 8.1 ± 7.2 |
| Flight hours after lockdown (h) | 152.1 ± 71.9 | 153.9 ± 63.8 | 150.5 ± 79.7 |
| Time (Months) | Intervention | Control | ANOVA (Time × Group Interaction) | Between Group ES | |||||
|---|---|---|---|---|---|---|---|---|---|
| (n = 35) | (n = 37) | ||||||||
| M | SD | Follow-Up Change (95% CI) | M | SD | Follow-Up Change (95% CI) | p | d | ||
| Body mass (kg) | 0 | 91.7 | 13.5 | 89.2 | 14.5 | 0.2, Trivial | |||
| 12 | 86.8 | 11.3 | −4.9 (−3.5–−6.3) | 90.5 | 14.5 | 1.3 (0.6–1.9) | <0.001 | −0.3, Small | |
| BMI (kg/m2) | 0 | 28.7 | 3.3 | 27.9 | 2.8 | 0.2, Trivial | |||
| 12 | 27.1 | 2.7 | −1.6 (−1.1–−2.0) | 28.3 | 3.7 | 0.4 (0.2–0.6) | <0.001 | −0.4, Small | |
| Systolic BP (mmHg) | 0 | 138.4 | 10.6 | 130.6 | 11.7 | 0.7 *, Moderate | |||
| 12 | 128.1 | 10.3 | −10.3 (−7.2–−13.5) | 134.4 | 9.9 | 3.8 (0.0–7.6) | <0.001 | −0.6 *, Moderate | |
| Diastolic BP (mmHg) | 0 | 86.7 | 8.1 | 83.1 | 8.2 | 0.4, Small | |||
| 12 | 78.9 | 8.0 | −7.8 (−5.0–−10.6) | 83.2 | 7.0 | 0.1 (−2.6–2.8) | <0.001 | −0.6 *, Moderate | |
| MAP (mmHg) | 0 | 103.9 | 8.0 | 98.9 | 8.5 | 0.6 *, Moderate | |||
| 12 | 95.3 | 7.6 | −8.6 (−6.0–−11.3) | 100.2 | 7.2 | 1.3 (−1.2–4.0) | <0.001 | −0.7 *, Moderate | |
| Pulse (bpm) | 0 | 69.2 | 7.8 | 68.1 | 10.9 | 0.1, Trivial | |||
| 12 | 63.4 | 8.5 | −5.8 (−3.8–−8.2) | 69.2 | 12.2 | 1.1 (−0.7–5.6) | <0.001 | −0.7 *, Moderate | |
| Hours slept (h/day) | 0 | 7.0 | 0.8 | 7.6 | 0.8 | −0.7 *, Moderate | |||
| 12 | 7.7 | 0.7 | 0.7 (0.4–1.1) | 7.5 | 0.7 | −0.1 (0.0–−0.3) | <0.001 | 0.4, Small | |
| PSQI Global (score) | 0 | 6.4 | 2.8 | 4.5 | 2.6 | 0.7 *, Moderate | |||
| 12 | 4.1 | 1.5 | −2.3 (−1.7–−3.2) | 5.0 | 2.7 | 0.5 (0.2–0.7) | <0.001 | −0.5 *, Small | |
| IPAQ-walk (min) | 0 | 69.0 | 37.9 | 134.0 | 57.2 | −1.3 **, Large | |||
| 12 | 102.3 | 69.2 | 33.3 (22.1–49.6) | 122.6 | 77.6 | −11.4 (−16.2–9.4) | <0.001 | −0.6 *, Moderate | |
| IPAQ-MVPA (min) | 0 | 125.9 | 79.7 | 162.1 | 94.7 | −0.4, Small | |||
| 12 | 227.0 | 83.0 | 101.1 (62.2–126.0) | 159.0 | 99.8 | −3.1 (−16.9–11.1) | <0.001 | 0.8 *, Moderate | |
| F&V Intake (serve/day) | 0 | 2.8 | 1.3 | 4.1 | 1.1 | −1.1 **, Moderate | |||
| 12 | 5.5 | 1.7 | 2.7 (2.0–3.2) | 3.9 | 1.3 | −0.2 (−0.5–0.1) | <0.001 | 1.1 **, Moderate | |
| PCS-12 (score) | 0 | 42.1 | 4.1 | 51.1 | 5.5 | −1.8 **, Large | |||
| 12 | 51.7 | 4.0 | 9.6 (7.1–10.8) | 50.7 | 4.9 | −0.4 (−1.3–0.2) | <0.001 | 0.1, Trivial | |
| MCS-12 (score) | 0 | 45.3 | 8.2 | 52.7 | 4.5 | −1.1 **, Moderate | |||
| 12 | 51.1 | 4.9 | 5.8 (3.6–8.0) | 51.8 | 4.7 | −0.9 (−0.1–−1.7) | <0.001 | 0.2, Trivial | |
| Time (Months) | Intervention (n = 35) | Effect Size | |||
|---|---|---|---|---|---|
| M | SD | Post-Follow-Up Change (95% CI) | d | ||
| Body mass (kg) | 4 | 87.7 | 12.8 | - | - |
| 12 | 86.8 | 11.3 | −0.97 (−1.81–0.1) | −0.47, small * | |
| BMI (kg/m2) | 4 | 27.5 | 3.1 | - | - |
| 12 | 27.1 | 2.7 | −0.32 (−0.58–0.07) | −0.44, small * | |
| Systolic BP (mmHg) | 4 | 130.9 | 11.1 | - | - |
| 12 | 128.1 | 10.3 | −2.89 (−6.09–0.32) | −0.31, small | |
| Diastolic BP (mmHg) | 4 | 83.8 | 9.7 | - | - |
| 12 | 78.9 | 8.0 | −4.86 (−7.56–−2.15) | −0.62, moderate ** | |
| MAP (mmHg) | 4 | 99.5 | 9.4 | - | - |
| 12 | 95.3 | 7.6 | −4.11 (−6.77–−1.46) | −0.53, small * | |
| Pulse (bpm) | 4 | 62.6 | 7.2 | - | - |
| 12 | 63.4 | 8.5 | 0.74 (−2.0–3.5) | 0.09, trivial | |
| Hours slept (h/day) | 4 | 7.8 | 1.0 | - | - |
| 12 | 7.7 | 0.7 | −0.11 (−0.27–0.05) | −0.23, small | |
| PSQI Global (score) | 4 | 4.1 | 1.8 | - | - |
| 12 | 4.1 | 1.5 | −0.09 (−0.31–0.14) | −0.13, trivial | |
| IPAQ-walk (min) | 4 | 94.3 | 96.5 | - | - |
| 12 | 102.3 | 69.2 | 8.0 (−10.4–26.4) | 0.15, trivial | |
| IPAQ-MVPA (min) | 4 | 207.6 | 79.0 | - | - |
| 12 | 227.0 | 82.6 | 19.7 (5.57–33.74) | 0.48, small * | |
| F&V Intake (serve/day) | 4 | 5.6 | 1.9 | - | - |
| 12 | 5.5 | 1.7 | −0.13 (−0.49–0.23) | 0.12, trivial | |
| PCS-12 (score) | 4 | 52.3 | 4.5 | - | - |
| 12 | 51.7 | 4.0 | −0.54 (−1.38–0.29) | −0.22, small | |
| MCS-12 (score) | 4 | 54.5 | 5.7 | - | - |
| 12 | 51.1 | 4.9 | −0.52 (−1.41–0.36) | −0.20, small | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilson, D.; Driller, M.; Winwood, P.; Johnston, B.; Gill, N. The Effects of a Brief Lifestyle Intervention on the Health of Overweight Airline Pilots during COVID-19: A 12-Month Follow-Up Study. Nutrients 2021, 13, 4288. https://doi.org/10.3390/nu13124288
Wilson D, Driller M, Winwood P, Johnston B, Gill N. The Effects of a Brief Lifestyle Intervention on the Health of Overweight Airline Pilots during COVID-19: A 12-Month Follow-Up Study. Nutrients. 2021; 13(12):4288. https://doi.org/10.3390/nu13124288
Chicago/Turabian StyleWilson, Daniel, Matthew Driller, Paul Winwood, Ben Johnston, and Nicholas Gill. 2021. "The Effects of a Brief Lifestyle Intervention on the Health of Overweight Airline Pilots during COVID-19: A 12-Month Follow-Up Study" Nutrients 13, no. 12: 4288. https://doi.org/10.3390/nu13124288
APA StyleWilson, D., Driller, M., Winwood, P., Johnston, B., & Gill, N. (2021). The Effects of a Brief Lifestyle Intervention on the Health of Overweight Airline Pilots during COVID-19: A 12-Month Follow-Up Study. Nutrients, 13(12), 4288. https://doi.org/10.3390/nu13124288