The Sum of Plasma Fatty Acids iso16:0, iso17:0, trans11-18:1, cis9, trans11-CLA, and cis6-18:1 as Biomarker of Dairy Intake Established in an Intervention Study and Validated in the EPIC Cohort of Gipuzkoa
Abstract
:1. Introduction
2. Materials and Methods
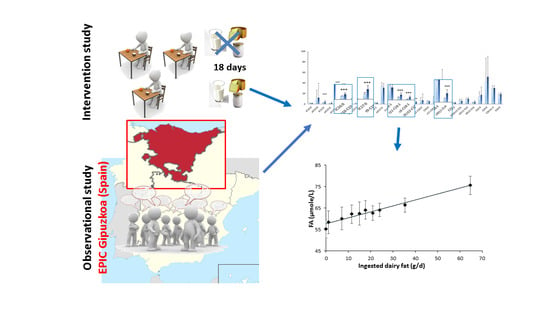
2.1. Intervention Study
2.2. Observational Study
2.3. Fatty Acids Analysis
2.4. Plasma Biochemical Parameters Analysis
2.5. Statistical Analysis
3. Results
3.1. Intervention Study
3.2. Observational Study
3.3. Comparative Analysis
3.4. Biochemical Parameters
4. Discussions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Thorning, T.K.; Raben, A.; Thorning, T.; Soedamah-Muthu, S.S.; Givens, I.; Astrup, A. Milk and dairy products: Good or bad for human health? An assessment of the totality of scientific evidence. Food Nutr. Res. 2016, 60, 32527. [Google Scholar] [CrossRef] [Green Version]
- Mazidi, M.; Mikhailidis, D.P.; Sattar, N.; Howard, G.; Graham, I.; Banach, M. Consumption of dairy product and its association with total and cause specific mortality—A population-based cohort study and meta-analysis. Clin. Nutr. 2019, 38, 2833–2845. [Google Scholar] [CrossRef] [PubMed]
- Jensen, R.G. The composition of bovine milk lipids: January 1995 to December 2000. J. Dairy Sci. 2002, 85, 295–350. [Google Scholar] [CrossRef]
- Prado, L.A.; Schmidely, P.; Nozière, P.; Ferlay, A. Milk saturated fatty acids, odd- and branched-chain fatty acids, and isomers of C18:1, C18:2, and C18:3n-3 according to their duodenal flows in dairy cows: A meta-analysis approach. J. Dairy Sci. 2019, 102, 3053–3070. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pranger, I.G.; Joustra, M.L.; Corpeleijn, E.; Muskiet, F.A.J.; Kema, I.P.; Singh-Povel, C.; Oude Elferink, S.J.W.H.; Bakker, S.J.L. Fatty acids as biomarkers of total dairy and dairy fat intakes: A systematic review and meta-analysis. Nutr. Rev. 2018, 77, 46–63. [Google Scholar] [CrossRef] [PubMed]
- Ratnayake, W.N. Concerns about the use of 15:0, 17:0, and trans-16:1n–7 as biomarkers of dairy fat intake in recent observational studies that suggest beneficial effects of dairy food on incidence of diabetes and stroke. Am. J. Clin. Nutr. 2015, 101, 1102–1103. [Google Scholar] [CrossRef]
- Jenkins, B.; West, J.A.; Koulman, A. A Review of Odd-Chain Fatty Acid Metabolism and the Role of Pentadecanoic Acid (C15:0) and Heptadecanoic Acid (C17:0) in Health and Disease. Molecules 2015, 20, 2425. [Google Scholar] [CrossRef] [Green Version]
- Pranger, I.G.; Corpeleijn, E.; Muskiet, F.A.J.; Kema, I.P.; Singh-Povel, C.; Bakker, S.J.L. Circulating fatty acids as biomarkers of dairy fat intake: Data from the Lifelines Biobank and Cohort Study. Biomarkers 2019, 24, 360–372. [Google Scholar] [CrossRef]
- Sun, Q.; Ma, J.; Campos, H.; Hu, F.B. Plasma and erythrocyte biomarkers of dairy fat intake and risk of ischemic heart disease. Am. J. Clin. Nutr. 2007, 86, 929–937. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodríguez, I.T.; Ballart, J.F.; Pastor, G.C.; Jordà, E.B.; Val, V.A. Validación de un cuestionario de frecuencia de consumo alimentario corto: Reproducibilidad y validez [Validation of a short questionnaire on frequency of dietary intake: Reproducibility and validity]. Nutr Hosp. 2008, 23, 242–252. [Google Scholar]
- Mataix Verdú, F.J. Tabla de Composición de Alimentos, 5th ed.; Universidad de Granada, Instituto de Nutrición y Tecnología de los Alimentos: Granada, Spain, 2011. [Google Scholar]
- Riboli, E.; Kaaks, R. The EPIC Project: Rationale and study design. European Prospective Investigation into Cancer and Nutrition. ije 1997, 26, S6. [Google Scholar] [CrossRef] [PubMed]
- EPIC Group of Spain. Relative validity and reproducibility of a diet history questionnaire in Spain. I. Foods. European Prospective Investigation into Cancer and Nutrition. ije 1997, 26 (Suppl. 1), S91–S99. [Google Scholar] [CrossRef] [Green Version]
- Bondia-Pons, I.; Morera-Pons, S.; Castellote, A.I.; López-Sabater, M.C. Determination of phospholipid fatty acids in biological samples by solid-phase extraction and fast gas chromatography. J. Chromatogr. A 2006, 1116, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Bondia-Pons, I.; Moltó-Puigmartí, C.; Castellote, A.I.; López-Sabater, M.C. Determination of conjugated linoleic acid in human plasma by fast gas chromatography. J. Chromatogr. A 2007, 1157, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Kelley, J.L.; Kruski, A.W. Density gradient ultracentrifugation of serum lipoproteins in a swinging bucket rotor. Meth. Enzymol. 1986, 128, 170–181. [Google Scholar] [CrossRef]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef]
- Nimmanapalli, H.; Kasi, A.; Devapatla, P.; Nuttakki, V. Lipid ratios, atherogenic coefficient and atherogenic index of plasma as parameters in assessing cardiovascular risk in type 2 diabetes mellitus. Int. J. Res. Med. Sci. 2017, 4, 2863–2869. [Google Scholar] [CrossRef] [Green Version]
- Varela-Moreiras, G.; Ruiz, E.; Valero, T.; Avila, J.M.; del Pozo, S. The Spanish diet: An update. Nutr. Hosp. 2013, 28 (Suppl. 5), 13–20. [Google Scholar] [CrossRef]
- Baylin, A.; Campos, H. The use of fatty acid biomarkers to reflect dietary intake. Curr. Opin. Lipidol. 2006, 17, 22–27. [Google Scholar] [CrossRef]
- De Oliveira Otto, C.; Nettleton, J.A.; Lemaitre, R.N.; Steffen, L.M.; Kromhout, D.; Rich, S.S.; Tsai, M.Y.; Jacobs, D.R.; Mozaffarian, D. Biomarkers of dairy fatty acids and risk of cardiovascular disease in the multi-ethnic study of atherosclerosis. J. Am. Heart Assoc. 2013, 2, e000092. [Google Scholar] [CrossRef] [Green Version]
- Pintus, S.; Murru, E.; Carta, G.; Cordeddu, L.; Batetta, B.; Accossu, S.; Pistis, D.; Uda, S.; Elena Ghiani, M.; Mele, M.; et al. Sheep cheese naturally enriched in α-linolenic, conjugated linoleic and vaccenic acids improves the lipid profile and reduces anandamide in the plasma of hypercholesterolaemic subjects. Br. J. Nutr. 2013, 109, 1453–1462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tricon, S.; Burdge, G.C.; Jones, E.L.; Russell, J.J.; El-Khazen, S.; Moretti, E. Effects of dairy products naturally enriched with cis-9, trans-11 conjugated linoleic acid on the blood lipid profile in healthy middle-aged men. Am. J. Clin. Nutr. 2006, 83, 744–753. [Google Scholar] [CrossRef] [Green Version]
- Hodson, L.; Eyles, H.C.; McLachlan, K.J.; Bell, M.L.; Green, T.J.; Skeaff, C.M. Plasma and Erythrocyte Fatty Acids Reflect Intakes of Saturated and n–6 PUFA within a Similar Time Frame. J. Nutr. 2014, 144, 33–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdullah, M.M.H.; Cyr, A.; Lépine, M.; Labonté, M.; Couture, P.; Jones, P.J.H.; Lamarche, B. Recommended dairy product intake modulates circulating fatty acid profile in healthy adults: A multi-centre cross-over study. Br. J. Nutr. 2015, 113, 435–444. [Google Scholar] [CrossRef] [Green Version]
- Skeaff, C.M.; Hodson, L.; McKenzie, J.E. Dietary-induced changes in fatty acid composition of human plasma, platelet, and erythrocyte lipids follow a similar time course. J. Nutr. 2006, 136, 565–569. [Google Scholar] [CrossRef] [Green Version]
- Fuhrman, B.J.; Barba, M.; Krogh, V.; Micheli, A.; Pala, V.; Lauria, R.; Chajes, V.; Riboli, E.; Sieri, S.; Berrino, F.; et al. Erythrocyte Membrane Phospholipid Composition as a Biomarker of Dietary Fat. Ann. Nutr. Metab. 2006, 50, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.F.; Solvoll, K.; Johansson, L.R.K.; Salminen, I.; Aro, A.; Drevon, C.A. Evaluation of a Food Frequency Questionnaire with Weighed Records, Fatty Acids, and Alpha-Tocopherol in Adipose Tissue and Serum. Am. J. Epidemiol. 1999, 150, 75–87. [Google Scholar] [CrossRef] [Green Version]
- von Houwelingen, A.C.; Kester, A.D.; Kromhout, D.; Hornstra, G. Comparison between habitual intake of polyunsaturated fatty acids and their concentrations in serum lipid fractions. Eur. J. Clin. Nutr. 1989, 43, 11–20. [Google Scholar]
- Furtado, J.D.; Beqari, J.; Campos, H. Comparison of the Utility of Total Plasma Fatty Acids Versus those in Cholesteryl Ester, Phospholipid, and Triglyceride as Biomarkers of Fatty Acid Intake. Nutrients 2019, 11, 2081. [Google Scholar] [CrossRef] [Green Version]
- Wolk, A.; Furuheim, M.; Vessby, B. Fatty acid composition of adiopse tissue and serum lipids are valid biological markers of dairy fat intake in men. J. Nutr. 2001, 131, 828–833. [Google Scholar] [CrossRef] [Green Version]
- Brevik, A.; Veierod, M.; Drevon, C.; Andersen, L. Evaluation of the odd fatty acids 15:0 and 17:0 in serum and adipose tissue as markers of intake of milk and dairy fat. Eur J. Clin. Nutr. 2005, 59, 1417–1422. [Google Scholar] [CrossRef]
- Santaren, I.D.; Watkins, S.M.; Liese, A.D.; Wagenknecht, L.E.; Rewers, M.J.; Haffner, S.M.; Lorenzo, C.; Hanley, A.J. Serum pentadecanoic acid (15:0), a short-term marker of dairy food intake, is inversely associated with incident type 2 diabetes and its underlying disorders. Am. J. Clin. Nutr. 2014, 100, 1532–1540. [Google Scholar] [CrossRef] [Green Version]
- Yakoob, M.Y.; Shi, P.; Willett, W.C.; Rexrode, K.M.; Campos, H.; Orav, E.J.; Hu, F.B.; Mozaffarian, D. Circulating Biomarkers of Dairy Fat and Risk of Incident Diabetes Mellitus Among Men and Women in the United States in Two Large Prospective Cohorts. Circulation 2016, 133, 1645–1654. [Google Scholar] [CrossRef] [Green Version]
- Jaudszus, A.; Kramer, R.; Pfeuffer, M.; Roth, A.; Jahreis, G.; Kuhnt, K. trans Palmitoleic acid arises endogenously from dietary vaccenic acid. Am. J. Clin. Nutr. 2014, 99, 431–435. [Google Scholar] [CrossRef] [Green Version]
- Mayneris-Perxachs, J.; Bondia-Pons, I.; Moltó-Puigmartí, C.; Pairó, M.; Castellote, A.I.; López-Sabater, M.C. Diet and plasma evaluation of the main isomers of conjugated linoleic acid and trans-fatty acids in a population sample from Mediterranean north-east Spain. Food Chem. 2010, 123, 296–305. [Google Scholar] [CrossRef]
- Zong, G.; Sun, Q.; Yu, D.; Zhu, J.; Sun, L.; Ye, X.; Li, H.; Jin, Q.; Zheng, H.; Hu, F.B.; et al. Dairy Consumption, Type 2 Diabetes, and Changes in Cardiometabolic Traits: A Prospective Cohort Study of Middle-Aged and Older Chinese in Beijing and Shanghai. Diabetes Care 2014, 37, 56–63. [Google Scholar] [CrossRef] [Green Version]
- Laverroux, S.; Glasser, F.; Gillet, M.; Joly, C.; Doreau, M. Isomerization of Vaccenic Acid to cis and trans C18:1 Isomers During Biohydrogenation by Rumen Microbes. Lipids 2011, 46, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Abilleira, E.; Collomb, M.; Schlichtherle-Cerny, H.; Virto, M.; de Renobales, M.; Barron, L.J.R. Winter/Spring Changes in Fatty Acid Composition of Farmhouse Idiazabal Cheese Due to Different Flock Management Systems. J. Agric. Food Chem. 2009, 57, 4746–4753. [Google Scholar] [CrossRef]
- Aslibekyan, S.; Campos, H.; Baylin, A. Biomarkers of dairy intake and the risk of heart disease. Nutr. Metab. Cardiovasc. Dis. 2012, 22, 1039–1045. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia-Closas, R.; Berenguer, A.; González, C.A. Changes in food supply in Mediterranean countries from 1961 to 2001. Public Health Nutr. 2006, 9, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Agricultura, Pesca, Alimentación y Medio Ambiente de España. El Consumo Alimentario en España Año 2011. Available online: https://www.mapa.gob.es/es/alimentacion/temas/consumo-tendencias/panel-de-consumo-alimentario/ultimos-datos/default.aspx/ (accessed on 23 October 2020).
- Bouvard, V.; Loomis, D.; Guyton, K.Z.; Grosse, Y.; Ghissassi, F.E.; Benbrahim-Tallaa, L.; Guha, N.; Mattock, H.; Straif, K. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015, 16, 1599–1600. [Google Scholar] [CrossRef] [Green Version]
- Hjartåker, A.; Lagiou, A.; Slimani, N.; Lund, E.; Chirlaque, M.; Vasilopoulou, E.; Zavitsanos, X.; Berrino, F.; Sacerdote, C.; Ocké, M.; et al. Consumption of dairy products in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort: Data from 35955 24-hour dietary recalls in 10 European countries. Public Health Nutr. 2002, 5, 1259–1271. [Google Scholar] [CrossRef] [Green Version]
- Newby, P.K.; Weismayer, C.; Åkesson, A.; Tucker, K.L.; Wolk, A. Long-Term Stability of Food Patterns Identified by Use of Factor Analysis among Swedish Women. J. Nutr. 2006, 136, 626–633. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saadatian-Elahi, M.; Slimani, N.; Chajès, V.; Jenab, M.; Goudable, J.; Biessy, C.; Ferrari, P.; Byrnes, G.; Autier, P.; Peeters, P.H.; et al. Plasma phospholipid fatty acid profiles and their association with food intakes: Results from a cross-sectional study within the European Prospective Investigation into Cancer and Nutrition. Am. J. Clin. Nutr. 2009, 89, 331–346. [Google Scholar] [CrossRef] [Green Version]
- Drouin-Chartier, J.; Côté, J.A.; Labonté, M.; Brassard, D.; Tessier-Grenier, M.; Desroches, S.; Couture, P.; Lamarche, B. Comprehensive Review of the Impact of Dairy Foods and Dairy Fat on Cardiometabolic Risk. Adv. Nutr. 2016, 7, 1041–1051. [Google Scholar] [CrossRef] [PubMed]
- Huth, P.J.; Park, K.M. Influence of Dairy Product and Milk Fat Consumption on Cardiovascular Disease Risk: A Review of the Evidence. Adv. Nutr. 2012, 3, 266–285. [Google Scholar] [CrossRef] [Green Version]
- Patel, P.S.; Sharp, S.J.; Jansen, E.; Luben, R.N.; Khaw, K.; Wareham, N.J.; Forouhi, N.G. Fatty acids measured in plasma and erythrocyte-membrane phospholipids and derived by food-frequency questionnaire and the risk of new-onset type 2 diabetes: A pilot study in the European Prospective Investigation into Cancer and Nutrition (EPIC)–Norfolk cohort. Am. J. Clin. Nutr. 2010, 92, 1214–1222. [Google Scholar] [CrossRef]



| Dairy Product | Intake, Mean (SD) 1 | Dairy Fat Ingested, g/day 2 |
|---|---|---|
| Whole milk | 266.7 (140.5) mL/day | 9.62 (5.23) |
| Full fat yogurt | 182.9 (76.7) g/day | 6.33 (2.68) |
| Fat cheese | 55.9 (25.4) g/day | 17.3 (8.74) |
| Others 3 | 38.9 (25.1) g/day | 1.59 (1.46) |
| Total | 544.3 (149.7) g/day | 33.1 (9.22) |
| Fatty Acids | Baseline | No Dairy | With Dairy | SEM | p1 | Pearson Correlation 2 |
|---|---|---|---|---|---|---|
| MCSFA | ||||||
| 10:0 | 27.87 b | 26.82 b | 32.88 a | 0.53 | <0.001 | 0.145 |
| 12:0 | 94.08 b | 104.0 b | 113.4 a | 1.78 | <0.001 | 0.155 |
| 14:0 | 99.83 b | 90.08 c | 153.1 a | 7.15 | 0.001 | 0.741 *** |
| 15:0 | 36.66 a | 32.78 b | 34.40 a,b | 0.68 | 0.008 | 0.085 |
| Sum | 261.28 b | 253.6 b | 333.8 a | 1.68 | <0.001 | 0.314 *** |
| LCSFA | ||||||
| 16:0 | 1996 a,b | 1868 b | 2231 a | 107.61 | <0.001 | 0.377 ** |
| 17:0 | 21.02 b | 18.61 b | 24.53 a | 0.70 | <0.001 | 0.613 *** |
| 18:0 | 692.9 | 607.0 | 669.6 | 19.44 | 0.150 | 0.050 |
| 20:0 | 4.79 | 5.474 | 5.189 | 0.15 | 0.065 | 0.045 |
| 21:0 | 2.68 | 2.224 | 2.614 | 0.10 | 0.129 | −0.058 |
| 22:0 | 13.86 | 13.92 | 17.39 | 1.41 | 0.356 | 0.022 |
| 24:0 | 48.25 | 42.26 | 51.82 | 6.07 | 0.230 | −0.038 |
| 26:0 | 18.95 a | 16.39 b | 19.03 a | 0.49 | 0.001 | 0.396 ** |
| Sum | 2737 b | 2574 b | 3021 a | 127.30 | 0.001 | 0.234 ** |
| ΣSFA | 2930 b | 2827 b | 3355 a | 134.16 | <0.001 | 0.240 |
| ΣOCFA | 60.36 a | 53.61 b | 61.59 a | 1.19 | <0.001 | 0.146 |
| BCSFA | ||||||
| iso14:0 | 1.414 | 1.665 | 1.655 | 0.05 | 0.059 | 0.108 |
| anteiso14:0 | 1.993 | 4.970 | 3.859 | 0.95 | 0.060 | −0.024 |
| iso15:0 | 3.275 b | 1.949 c | 4.555 a | 0.26 | <0.001 | −0.167 |
| anteiso15:0 | 1.632 a | 0.7894 b | 2.278 a | 0.13 | <0.001 | 0.192 |
| iso16:0 | 5.599 b | 3.955 c | 6.867 a | 2.45 | <0.001 | −0.026 |
| anteiso16:0 | 0.6568 | 0.5472 | 0.4586 | 0.03 | 0.068 | |
| iso17:0 | 12.89 a | 6.495 b | 13.67 a | 0.73 | <0.001 | 0.667 *** |
| anteiso17:0 | 33.95 | 33.49 | 30.84 | 1.22 | 0.247 | 0.345 ** |
| Sum | 61.42 | 56.06 | 66.98 | 3.05 | 0.073 | −0.005 |
| c-MUFA | ||||||
| cis9-14:1 | 23.07 b | 15.98 c | 28.70 a | 1.05 | <0.001 | 0.746 *** |
| cis9-16:1 | 129.1 a | 103.8 b | 128.8 a | 12.08 | 0.004 | 0.769 *** |
| cis10-17:1 | 11.40 | 10.48 | 10.65 | 0.26 | 0.048 | 0.179 |
| cis6-18:1 | 2.353 b | 0.9266 c | 4.014 a | 0.40 | <0.001 | 0.518 *** |
| cis9-18:1 | 1768 | 1788 | 1932 | 116.22 | 0.179 | 0.469 ** |
| cis11-18:1 | 132.0 b | 145.4 a | 131.7 b | 4.26 | 0.019 | 0.461 ** |
| cis11-20:1 | 11.41 | 10.70 | 10.33 | 0.58 | 0.478 | 0.286 * |
| cis13-22:1 | 120.5 | 88.84 | 118.8 | 4.92 | 0.688 | 0.521 ** |
| Sum | 2197 | 2182 | 2374 | 134.62 | 0.113 | 0.464 ** |
| t-MUFA | ||||||
| trans10-15:1 | 1.783 a,b | 1.496 b | 1.703 a | 0.05 | 0.041 | 0.265 * |
| trans9-16:1 | 2.243 | 1.827 | 2.256 | 0.12 | 0.179 | 0.178 |
| trans9-18:1 | 16.78 | 20.34 | 17.92 | 1.13 | 0.139 | 0.117 |
| trans11-18:1 | 5.422 b | 3.294 c | 7.533 a | 0.36 | <0.001 | 0.694 *** |
| Sum | 26.70 | 26.95 | 29.41 | 1.45 | 0.277 | 0.303 ** |
| PUFA | ||||||
| trans9, trans12-18:2 | 4.615 | 6.434 | 4.604 | 1.01 | 0.250 | |
| cis9, cis12-18:2 | 3470 | 3231 | 3507 | 110.06 | 0.161 | 0.304 * |
| 18:3 ω-6 | 161.1 a | 121.4 b | 135.0 a,b | 6.80 | 0.003 | 0.511 *** |
| 18:3 ω-3 | 40.93 a,b | 32.53 b | 43.44 a | 2.32 | 0.014 | 0.679 *** |
| 20:4 ω-6 | 945.4 | 904.9 | 923.1 | 25.72 | 0.420 | 0.346 ** |
| 20:5 ω-3 | 24.81 b | 29.15 a | 30.42 a | 0.69 | <0.001 | 0.646 *** |
| 22:6 ω-3 | 326.1 | 333.3 | 339.5 | 13.68 | 0.691 | 0.486 *** |
| Sum | 4933 | 4659 | 4986 | 136.53 | 0.155 | 0.178 |
| CLA | ||||||
| cis9, trans11-CLA | 10.74 a | 4.858 b | 13.34 a | 0.86 | <0.001 | 0.821 *** |
| trans10, cis12-CLA | 4.193 | 6.434 | 5.933 | 0.36 | 0.045 | 0.034 |
| cis9, cis11-CLA | 11.60 | 8.877 | 9.93 | 0.41 | 0.036 | 0.338 ** |
| trans9, trans11-CLA | 4.142 a,b | 2.886 b | 4.228 a | 0.25 | 0.005 | 0.387 ** |
| Sum | 30.70 a,b | 23.09 b | 33.43 a | 1.40 | 0.001 | 0.474 *** |
| TOTAL | 10230 a,b | 9778 b | 10849 a | 391.62 | 0.017 | 0.221 |
| Intervention Study | Observational Study (Plasma) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Plasma (Model 1) | Erythrocytes (Model 2) | Model 3 | Model 4 | |||||||
| Fatty acid | R2 | B a | R2 b | R2 | B a | R2 c | R2 | B a | R2 | B a |
| 14:0 | 0.849 *** | 1.980 | 0.809 | 0.787 *** | 0.401 | 0.755 | ||||
| 14:1 | 0.835 *** | 0.383 | 0.802 | 0.598 *** | 0.113 | 0.581 | ||||
| 15:0 | 0.130 *** | 0.141 | 0.232 *** | 0.277 | ||||||
| iso15:0 | 0.495 *** | 0.074 | 0.426 | |||||||
| anteiso15:0 | 0.729 *** | 0.044 | 0.664 | 0.402 * | 0.005 | 0.134 | ||||
| iso16:0 | 0.769 *** | 0.092 | 0.737 | 0.136 *** | 0.042 | 0.259 *** | 0.103 | |||
| 17:0 | 0.697 *** | 0.205 | 0.605 | 0.423 ** | 0.097 | 0.424 | 0.140 *** | 0.079 | 0.235 *** | 0.242 |
| iso17:0 | 0.793 *** | 0.241 | 0.743 | 0.572 *** | 0.109 | 0.530 | 0.134 *** | 0.105 | 0.262 *** | 0.246 |
| trans11-18:1 | 0.771 *** | 0.133 | 0.735 | 0.604 *** | 0.043 | 0.593 | 0.115 *** | 0.066 | 0.261 *** | 0.121 |
| cis6-18:1 | 0.712 *** | 0.087 | 0.679 | 0.777 *** | 0.049 | 0.777 | 0.141 ** | 0.037 | ||
| cis9, trans11-CLA | 0.804 *** | 0.282 | 0.780 | 0.768 *** | 0.097 | 0.752 | 0.062 ** | 0.099 | 0.201 *** | 0.233 |
| Sum d | 0.871 *** | 0.827 | 0.849 | 0.131 *** | 0.335 | 0.260 *** | 0.740 | |||
| Sum e | 0.774 *** | 0.301 | 0.761 | |||||||
| Dairy Consumption (g/day) | ||||||
|---|---|---|---|---|---|---|
| <0.71 | 9.37–217.74 | 221.43–351.25 | >351.25 | |||
| Number | 35 | 38 | 38 | 40 | ||
| Plasma fatty acids | SEM | p1 | ||||
| 15:0 | 17.92 c | 22.53 b | 22.61 b | 27.08 a | 0.63 | <0.001 |
| anteiso15 | 0.8840 b | 1.210 a,b | 1.191 a,b | 1.580 a | 0.07 | 0.012 |
| iso16 | 7.265 b | 8.229 a,b | 8.216 a,b | 9.087 a | 0.26 | 0.005 |
| iso17:0 | 17.66 b | 22.60 a | 23.67 a | 23.23 a | 0.56 | <0.001 |
| trans9-16:1 | 1.360 b | 1.637 b | 1.767 a | 1.702 a,b | 0.05 | 0.045 |
| cis9-16:1 | 263.3 a | 216.7 a,b | 177.0 b | 168.2 b | 11.87 | 0.001 |
| 17:0 | 20.28 b | 23.08 a,b | 22.97 a,b | 24.67 a | 0.43 | 0.004 |
| trans11-18:1 | 6.752 b | 9.658 a,b | 9.807 a | 10.84 a | 0.34 | <0.001 |
| cis6-18:1 | 2.050 b | 3.318 a,b | 3.369 a,b | 3.554 a | 0.17 | 0.008 |
| cis9, trans11-CLA | 16.82 | 20.52 | 20.63 | 20.50 | 0.59 | 0.066 |
| Biochemical Parameters | Intervention Study | Observational Study | ||||
|---|---|---|---|---|---|---|
| r 1 | r 2 | r 3 | r 1 | r 2 | r 3 | |
| TG, mg/dL | 0.089 | 0.121 | 0.324 * | −0.069 | −0.057 | 0.204 * |
| TC, mg/dL | 0.064 | 0.189 | 0.459 ** | −0.026 | −0.003 | 0.382 ** |
| LDL-C, mg/dL | 0.139 | 0.203 | 0.348 * | 0.008 | 0.009 | 0.328 ** |
| HDL-C, mg/dL | −0.091 | 0.060 | 0.341 * | −0.050 | 0.004 | 0.206 * |
| TC/HDL-C | 0.229 | 0.178 | 0.110 | 0.025 | −0.019 | 0.112 |
| AIP | 0.247 | 0.179 | 0.207 | −0.052 | −0.045 | 0.007 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berriozabalgoitia, A.; Gordoa, J.C.R.d.; Renobales, M.d.; Amores, G.; Barron, L.J.R.; Amiano, P.; Dorronsoro, M.; Perea, Z.; Virto, M. The Sum of Plasma Fatty Acids iso16:0, iso17:0, trans11-18:1, cis9, trans11-CLA, and cis6-18:1 as Biomarker of Dairy Intake Established in an Intervention Study and Validated in the EPIC Cohort of Gipuzkoa. Nutrients 2021, 13, 702. https://doi.org/10.3390/nu13020702
Berriozabalgoitia A, Gordoa JCRd, Renobales Md, Amores G, Barron LJR, Amiano P, Dorronsoro M, Perea Z, Virto M. The Sum of Plasma Fatty Acids iso16:0, iso17:0, trans11-18:1, cis9, trans11-CLA, and cis6-18:1 as Biomarker of Dairy Intake Established in an Intervention Study and Validated in the EPIC Cohort of Gipuzkoa. Nutrients. 2021; 13(2):702. https://doi.org/10.3390/nu13020702
Chicago/Turabian StyleBerriozabalgoitia, Alaitz, Juan Carlos Ruiz de Gordoa, Mertxe de Renobales, Gustavo Amores, Luis Javier R. Barron, Pilar Amiano, Miren Dorronsoro, Zelai Perea, and Mailo Virto. 2021. "The Sum of Plasma Fatty Acids iso16:0, iso17:0, trans11-18:1, cis9, trans11-CLA, and cis6-18:1 as Biomarker of Dairy Intake Established in an Intervention Study and Validated in the EPIC Cohort of Gipuzkoa" Nutrients 13, no. 2: 702. https://doi.org/10.3390/nu13020702
APA StyleBerriozabalgoitia, A., Gordoa, J. C. R. d., Renobales, M. d., Amores, G., Barron, L. J. R., Amiano, P., Dorronsoro, M., Perea, Z., & Virto, M. (2021). The Sum of Plasma Fatty Acids iso16:0, iso17:0, trans11-18:1, cis9, trans11-CLA, and cis6-18:1 as Biomarker of Dairy Intake Established in an Intervention Study and Validated in the EPIC Cohort of Gipuzkoa. Nutrients, 13(2), 702. https://doi.org/10.3390/nu13020702