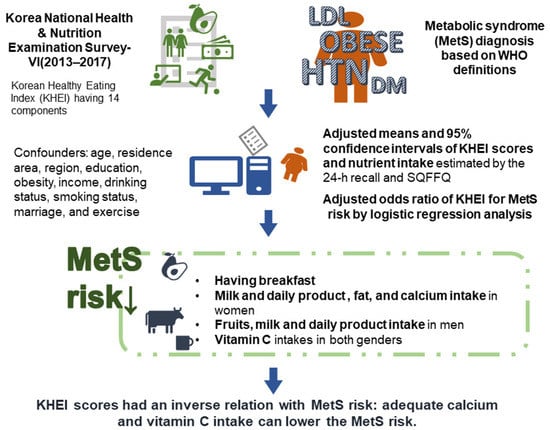
A Healthy Diet Rich in Calcium and Vitamin C Is Inversely Associated with Metabolic Syndrome Risk in Korean Adults from the KNHANES 2013–2017
Abstract
:1. Introduction
2. Methods
2.1. Design and Data Collection
2.2. Definition of Metabolic Syndrome
2.3. Laboratory Testing
2.4. Food and Nutrient Intakes from 24-h Recall and Food Frequency Questionnaire (FFQ)
2.5. Korean Healthy Eating Index (KHEI) Scores
2.6. Statistical Analysis
3. Results
3.1. General Population Features According to Metabolic Syndrome
3.2. Distribution of Socioeconomic and Lifestyle Variables of Participants According to Quartiles of KHEI Scores
3.3. KHEI Scores in Each Gender According to the Presence of Metabolic Syndrome (MetS)
3.4. Macronutrient Intake Estimated by 24-h Recall
3.5. Association of KHEI Scores with MetS Status
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Park, S.; Ahn, J.; Lee, B.K. Very-low-fat diets may be associated with increased risk of metabolic syndrome in the adult population. Clin. Nutr. 2016, 35, 1159–1167. [Google Scholar] [CrossRef]
- Park, S.; Kim, K.; Lee, B.K.; Ahn, J. Association of the Healthy Eating Index with Estimated Cardiovascular Age in Adults from the KNHANES 2013-2017. Nutrients 2020, 12, 2912. [Google Scholar] [CrossRef]
- Ahn, J.; Kim, N.S.; Lee, B.K.; Park Kim, S. Trends in the Intake of Fatty Acids and Their Food Source According to Obese Status Among Korean Adult Population Using KNHANES 2007-2017. Food Nutr. Bull. 2020, 41, 77–88. [Google Scholar] [CrossRef] [PubMed]
- Narayan, K.M.V.; Kanaya, A.M. Why are South Asians prone to type 2 diabetes? A hypothesis based on underexplored pathways. Diabetologia 2020, 63, 1103–1109. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.S.; Kim, B.C.; Daily, J.W.; Park, S. High genetic risk scores for impaired insulin secretory capacity doubles the risk for type 2 diabetes in Asians and is exacerbated by Western-type diets. Diabetes Metab Res. Rev. 2018, 34, e2944. [Google Scholar] [CrossRef]
- Lim, S. Eating a Balanced Diet: A Healthy Life through a Balanced Diet in the Age of Longevity. J. Obes. Metab. Syndr. 2018, 27, 39–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef] [Green Version]
- Brauer, P.; Royall, D.; Rodrigues, A. Use of the Healthy Eating Index in Intervention Studies for Cardiometabolic Risk Conditions: A Systematic Review. Adv. Nutr. 2021. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.; Kim, N.S.; Lee, B.K.; Park, S. Carbohydrate Intake Exhibited a Positive Association with the Risk of Metabolic Syndrome in Both Semi-Quantitative Food Frequency Questionnaires and 24-Hour Recall in Women. J. Korean Med. Sci 2017, 32, 1474–1483. [Google Scholar] [CrossRef] [Green Version]
- Yook, S.-M.; Park, S.; Moon, H.-K.; Kim, K.; Shim, J.E.; Hwang, J.-Y. Development of Korean Healthy Eating Index for adults using the Korea National Health and Nutrition Examination Survey data. J. Nutr. Health 2015, 48, 419–428. [Google Scholar] [CrossRef] [Green Version]
- Park, K.; Lim, S.; Park, Y.; Ju, W.; Shin, Y.; Yeom, H. Cardiovascular Disease Risk Factors and Obesity Levels in Korean Adults: Results from the Korea National Health and Nutrition Examination Survey, 2007–2015. Osong Public Health Res. Perspect. 2018, 9, 150–159. [Google Scholar] [CrossRef]
- Oh, S.S.; Kim, W.; Han, K.T.; Park, E.C.; Jang, S.I. Alcohol consumption frequency or alcohol intake per drinking session: Which has a larger impact on the metabolic syndrome and its components? Alcohol 2018, 71, 15–23. [Google Scholar] [CrossRef]
- Park, S.; Kang, S. Alcohol, Carbohydrate, and Calcium Intakes and Smoking Interactions with APOA5 rs662799 and rs2266788 were Associated with Elevated Plasma Triglyceride Concentrations in a Cross-Sectional Study of Korean Adults. J. Acad. Nutr. Diet. 2020, 120, 1318–1329.e1311. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Ahn, J.; Lee, B.K. Self-rated Subjective Health Status Is Strongly Associated with Sociodemographic Factors, Lifestyle, Nutrient Intakes, and Biochemical Indices, but Not Smoking Status: KNHANES 2007–2012. J. Korean Med. Sci 2015, 30, 1279–1287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, T.H.; Lee, M.J.; Yoo, K.B.; Han, E.; Choi, J.W. Association of Demographic and Socioeconomic Factors With Risk Factors for Chronic Kidney Disease. J. Prev. Med. Public Health 2015, 48, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Rezaianzadeh, A.; Namayandeh, S.-M.; Sadr, S.-M. National Cholesterol Education Program Adult Treatment Panel III Versus International Diabetic Federation Definition of Metabolic Syndrome, Which One is Associated with Diabetes Mellitus and Coronary Artery Disease? Int. J. Prev. Med. 2012, 3, 552–558. [Google Scholar]
- Validation of the Friedewald formula for estimating low density lipoprotein cholesterol: The Korea National Health and Nutrition Examination Survey, 2009 to 2011 FAU-Lee, Jongseok FAU-Jang, Sungok FAU-Jeong, Haemin FAU-Ryu, Ohk-Hyun. Korean J. Intern. Med. 2020, 35, 150–159. [CrossRef] [Green Version]
- Park, S.; Ham, J.O.; Lee, B.K. Effects of total vitamin A, vitamin C, and fruit intake on risk for metabolic syndrome in Korean women and men. Nutrition 2015, 31, 111–118. [Google Scholar] [CrossRef]
- Kim, Y.J.; Hwang, J.Y.; Kim, H.; Park, S.; Kwon, O. Diet quality, physical activity, and their association with metabolic syndrome in Korean adults. Nutrition 2019, 59, 138–144. [Google Scholar] [CrossRef]
- Kang, Y.; Kim, J. Gender difference on the association between dietary patterns and metabolic syndrome in Korean population. Eur. J. Nutr. 2016, 55, 2321–2330. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.; Kim, S.; Joung, H. Evidence-based approaches for establishing the 2015 Dietary Reference Intakes for Koreans. Nutr. Res. Pract. 2018, 12, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Martyn, D.; Darch, M.; Roberts, A.; Lee, H.Y.; Yaqiong Tian, T.; Kaburagi, N.; Belmar, P. Low-/No-Calorie Sweeteners: A Review of Global Intakes. Nutrients 2018, 10, 357. [Google Scholar] [CrossRef] [Green Version]
- Al-Ibrahim, A.A.; Jackson, R.T. Healthy eating index versus alternate healthy index in relation to diabetes status and health markers in US adults: NHANES 2007–2010. Nutr. J. 2019, 18, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwingshackl, L.; Hoffmann, G. Diet Quality as Assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension Score, and Health Outcomes: A Systematic Review and Meta-Analysis of Cohort Studies. J. Acad. Nutr. Diet. 2015, 115, 780–800.e785. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, K.; Schwingshackl, L.; Gottschald, M.; Knüppel, S.; Stelmach-Mardas, M.; Aleksandrova, K.; Boeing, H. Breakfast quality and cardiometabolic risk profiles in an upper middle-aged German population. Eur. J. Clin. Nutr. 2017, 71, 1312–1320. [Google Scholar] [CrossRef] [Green Version]
- Koyama, T.; Maekawa, M.; Ozaki, E.; Kuriyama, N.; Uehara, R. Daily Consumption of Coffee and Eating Bread at Breakfast Time Is Associated with Lower Visceral Adipose Tissue and with Lower Prevalence of Both Visceral Obesity and Metabolic Syndrome in Japanese Populations: A Cross-Sectional Study. Nutrients 2020, 12, 3090. [Google Scholar] [CrossRef]
- Lee, T.S.; Kim, J.S.; Hwang, Y.J.; Park, Y.C. Habit of Eating Breakfast Is Associated with a Lower Risk of Hypertension. J. Lifestyle Med. 2016, 6, 64–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ofori-Asenso, R.; Owen, A.J.; Liew, D. Skipping Breakfast and the Risk of Cardiovascular Disease and Death: A Systematic Review of Prospective Cohort Studies in Primary Prevention Settings. J. Cardiovasc. Dev. Dis 2019, 6, 30. [Google Scholar] [CrossRef] [Green Version]
- Maki, K.C.; Phillips-Eakley, A.K.; Smith, K.N. The Effects of Breakfast Consumption and Composition on Metabolic Wellness with a Focus on Carbohydrate Metabolism. Adv. Nutr. 2016, 7, 613S–621S. [Google Scholar] [CrossRef]
- Tian, Y.; Su, L.; Wang, J.; Duan, X.; Jiang, X. Fruit and vegetable consumption and risk of the metabolic syndrome: A meta-analysis. Public Health Nutr. 2018, 21, 756–765. [Google Scholar] [CrossRef]
- van den Brink, W.; van Bilsen, J.; Salic, K.; Hoevenaars, F.P.M.; Verschuren, L.; Kleemann, R.; Bouwman, J.; Ronnett, G.V.; van Ommen, B.; Wopereis, S. Current and Future Nutritional Strategies to Modulate Inflammatory Dynamics in Metabolic Disorders. Front. Nutr. 2019, 6, 129. [Google Scholar] [CrossRef] [Green Version]
- Traber, M.G.; Buettner, G.R.; Bruno, R.S. The relationship between vitamin C status, the gut-liver axis, and metabolic syndrome. Redox Biol. 2019, 21, 101091. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.K.; Chin, K.-Y.; Ima-Nirwana, S. Vitamin C: A Review on its Role in the Management of Metabolic Syndrome. Int. J. Med. Sci 2020, 17, 1625–1638. [Google Scholar] [CrossRef] [PubMed]
- Farag, H.A.M.; Hosseinzadeh-Attar, M.J.; Muhammad, B.A.; Esmaillzadeh, A.; El Bilbeisi, A.H. Effects of vitamin C supplementation with and without endurance physical activity on components of metabolic syndrome: A randomized, double-blind, placebo-controlled clinical trial. Clin. Nutr. Exp. 2019, 26, 23–33. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Chen, X.; Xu, Y.; Yang, J.; Du, L.; Li, K.; Zhou, Y. Milk consumption and multiple health outcomes: Umbrella review of systematic reviews and meta-analyses in humans. Nutr. Metab. 2021, 18, 7. [Google Scholar] [CrossRef]
- Park, S.; Kang, S.; Kim, D.S. Severe calcium deficiency increased visceral fat accumulation, down-regulating genes associated with fat oxidation, and increased insulin resistance while elevating serum parathyroid hormone in estrogen-deficient rats. Nutr. Res. 2020, 73, 48–57. [Google Scholar] [CrossRef]
- Han, D.; Fang, X.; Su, D.; Huang, L.; He, M.; Zhao, D.; Zou, Y.; Zhang, R. Dietary Calcium Intake and the Risk of Metabolic Syndrome: A Systematic Review and Meta-Analysis. Sci. Rep. 2019, 9, 19046. [Google Scholar] [CrossRef] [Green Version]
- Pannu, P.K.; Soares, M.J.; Piers, L.S.; Zhao, Y.; Ansari, Z. The association of vitamin D status and dietary calcium intake with individual components of the metabolic syndrome: A population-based study in Victoria, Australia. Cardiovasc. Endocrinol. 2017, 6, 136–144. [Google Scholar] [CrossRef]
- Park, S.; Kim, D.S.; Kang, S. Vitamin D deficiency impairs glucose-stimulated insulin secretion and increases insulin resistance by reducing PPAR-γ expression in nonobese Type 2 diabetic rats. J. Nutr. Biochem. 2016, 27, 257–265. [Google Scholar] [CrossRef]
- Pannu, P.K.; Zhao, Y.; Soares, M.J.; Piers, L.S.; Ansari, Z. The associations of vitamin D status and dietary calcium with the metabolic syndrome: An analysis of the Victorian Health Monitor survey. Public Health Nutr. 2017, 20, 1785–1796. [Google Scholar] [CrossRef] [Green Version]
| Classification Variables | Metabolic Syndrome | |||
|---|---|---|---|---|
| Yes (N = 2128) | No (N = 10,189) | p-Value * | ||
| Sex | Female | 1025 (19.7) | 3861 (80.3) | <0.01 |
| Male | 1103 (13.3) | 6328 (86.7) | ||
| Age group | 20–29 | 96 (5.8) | 1683 (94.2) | <0.01 |
| 30–39 | 324 (12.3) | 2536 (87.7) | ||
| 40–49 | 512 (17.4) | 2578 (82.6) | ||
| 50–59 | 769 (24.5) | 2382 (75.5) | ||
| 60–64 | 427 (29.6) | 1010 (70.4) | ||
| Residence | Urban | 1678 (15.6) | 8567 (84.4) | <0.01 |
| Rural | 450 (20.6) | 1622 (79.4) | ||
| Education | <High school | 658 (29.3) | 538 (70.7) | <0.01 |
| High school | 679 (18.8) | 2895 (81.2) | ||
| College | 793 (11.9) | 5756 (88.1) | ||
| Income | 1st Q | 305 (24.6) | 801 (75.4) | <0.01 |
| 2nd Q | 536 (17.1) | 2435 (82.9) | ||
| 3rd Q | 659 (15.8) | 3264 (84.2) | ||
| 4th Q | 619 (14.3) | 3660 (85.7) | ||
| Obesity | Lean | 5 (0.7) | 503 (99.3) | <0.01 |
| Normal | 571 (6.5) | 7248 (93.5) | ||
| Obese | 1552 (37.6) | 2438 (62.4) | ||
| Smoking status | Current smoker | 1130 (13) | 6599 (87) | <0.01 |
| Ex-smoker | 391 (18.4) | 1665 (81.6) | ||
| Non-smoker | 607 (23) | 1925 (77) | ||
| Drinking status | None | 632 (20.8) | 2355 (79.2) | <0.01 |
| Mild | 957 (13) | 5661 (87) | ||
| Moderate | 218 (15.7) | 1142 (84.3) | ||
| Severe | 321 (23.9) | 1031 (76.1) | ||
| Exercise | Yes | 973 (15.3) | 5087 (84.7) | <0.01 |
| No | 1155 (17.5) | 5102 (82.5) | ||
| Marriage | Yes | 1916 (18.7) | 8116 (81.3) | <0.01 |
| No | 207 (9.1) | 2072 (90.9) | ||
| Survey year | 2013 | 516 (15.1) | 2745 (84.9) | <0.01 |
| 2014 | 487 (15.5) | 2493 (84.5) | ||
| 2015 | 563 (17.5) | 2388 (82.5) | ||
| 2016 | 562 (17.6) | 2563 (82.4) | ||
| Classification Variables | KHEI Score | |||||
|---|---|---|---|---|---|---|
| Q1 (N = 1177) | Q2 (N = 2341) | Q3 (N = 2379) | Q4 (N = 3120) | p Value * | ||
| Sex | Female | 202 (6.1) | 1168 (33.4) | 1009 (27.2) | 1214 (33.3) | <0.01 |
| Male | 975 (19.6) | 1173 (21.9) | 1370 (24.6) | 1906 (33.9) | ||
| Age group | 20–29 | 307 (18.7) | 431 (29.4) | 343 (21.9) | 439 (30) | <0.01 |
| 30–39 | 307 (14.7) | 619 (31) | 572 (26.8) | 597 (27.5) | ||
| 40–49 | 253 (11.3) | 563 (26.9) | 574 (26.8) | 764 (35.1) | ||
| 50–59 | 201 (7.8) | 506 (24) | 614 (27.8) | 919 (40.4) | ||
| 60–64 | 109 (10.5) | 222 (23.3) | 276 (27.3) | 401 (38.9) | ||
| Residence | Urban | 977 (13.2) | 1901 (27.2) | 1957 (25.5) | 2637 (34.1) | <0.01 |
| Rural | 200 (12.1) | 440 (29.5) | 422 (27.7) | 483 (30.7) | ||
| Education | <high school | 247 (14.6) | 437 (29.8) | 420 (25.3) | 499 (30.2) | <0.01 |
| High school | 358 (14.4) | 652 (27.0) | 669 (26.7) | 844 (31.9) | ||
| College | 572 (12.6) | 1252 (27.2) | 1290 (25.6) | 1777 (35.2) | ||
| Income | 1st Q | 169 (20.6) | 238 (31.2) | 182 (22.3) | 184 (26) | <0.01 |
| 2nd Q | 367 (16.7) | 604 (30.4) | 559 (25) | 656 (27.9) | ||
| 3rd Q | 365 (13) | 752 (26.9) | 818 (27.8) | 939 (32.2) | ||
| 4th Q | 273 (8.6) | 738 (25.1) | 812 (25.6) | 1335 (40.7) | ||
| Obesity | Lean | 81 (22) | 107 (25.9) | 111 (23.7) | 131 (28.4) | <0.01 |
| Normal | 758 (13.3) | 1433 (26) | 1541 (25.8) | 2068 (34.9) | ||
| Obese | 338 (11) | 801 (31) | 727 (26.3) | 921 (31.7) | ||
| Smoking status | Current smoker | 790 (14) | 1260 (22.9) | 1490 (25.5) | 2171 (37.6) | <0.01 |
| Ex-smoker | 137 (9.6) | 380 (26.6) | 425 (28.2) | 555 (35.6) | ||
| Non-smoker | 250 (13.2) | 701 (39.9) | 464 (25) | 394 (22) | ||
| Drinking status | None | 263 (11.5) | 501 (25.2) | 602 (26.9) | 814 (36.4) | <0.01 |
| Mild | 605 (12.6) | 1164 (24.9) | 1275 (26.1) | 1804 (36.4) | ||
| Moderate | 148 (14.9) | 309 (32.6) | 254 (24.6) | 278 (27.9) | ||
| Severe | 161 (15.5) | 367 (38.3) | 248 (24.3) | 224 (21.9) | ||
| Exercise | Yes | 531 (12.2) | 1099 (26.6) | 1156 (25.9) | 1603 (35.2) | <0.01 |
| No | 646 (13.8) | 1242 (28.5) | 1223 (25.9) | 1517 (31.8) | ||
| Marriage | Yes | 837 (11.4) | 1794 (26.3) | 1937 (27.1) | 2600 (35.2) | <0.01 |
| No | 340 (17.4) | 545 (30.7) | 441 (22.7) | 519 (29.1) | ||
| Year | 2013 | 279 (11) | 602 (26.2) | 651 (26) | 907 (36.7) | <0.01 |
| 2014 | 284 (12.9) | 585 (27.9) | 590 (26.6) | 749 (32.7) | ||
| 2015 | 295 (13.6) | 560 (27.8) | 578 (25.9) | 757 (32.8) | ||
| 2016 | 319 (14.7) | 594 (28.4) | 560 (24.9) | 707 (31.9) | ||
| Classification | Female | Male | |||||
|---|---|---|---|---|---|---|---|
| Metabolic Syndrome | Normal | p-Value * | Metabolic Syndrome | Normal | p-Value * | ||
| Adequacy | Have breakfast | 6.72 (6.44~6.99) | 7.06 (6.95~7.18) | 0.019 | 6.66 (6.38~6.94) | 6.73 (6.59~6.87) | 0.65 |
| Mixed grains intake | 4.15 (4.02~4.27) | 4.13 (4.07~4.18) | 0.768 | 3.80 (3.65~3.96) | 3.78 (3.71~3.86) | 0.802 | |
| Total fruits intake | 3.72 (3.60~3.84) | 3.78 (3.74~3.83) | 0.319 | 2.27 (2.14~2.41) | 2.52 (2.45~2.59) | 0.002 | |
| Fresh fruits intake | 3.61 (3.49~3.73) | 3.68 (3.63~3.73) | 0.305 | 2.01 (1.88~2.14) | 2.25 (2.18~2.32) | 0.002 | |
| Total vegetable intake | 4.85 (4.81~4.89) | 4.88 (4.86~4.89) | 0.225 | 4.76 (4.70~4.82) | 4.80 (4.77~4.83) | 0.231 | |
| Vegetable intake excluding kimchi and pickled vegetables | 4.29 (4.19~4.39) | 4.33 (4.29~4.36) | 0.456 | 3.72 (3.60~3.83) | 3.79 (3.74~3.85) | 0.224 | |
| Meat, fish, eggs, and beans intake | 3.91 (3.76~4.06) | 4.02 (3.97~4.07) | 0.168 | 3.93 (3.81~4.06) | 3.95 (3.89~4.00) | 0.873 | |
| Milk and milk products intake | 3.23 (2.92~3.533) | 3.75 (3.63~3.87) | 0.002 | 3.05 (2.75~3.34) | 3.44 (3.29~3.59) | 0.026 | |
| Moderation | % of energy from saturated fatty acids | 9.46 (9.39~9.54) | 9.40 (9.36~9.43) | 0.068 | 9.47 (9.39~9.55) | 9.46 (9.42~9.49) | 0.81 |
| Sodium intake | 5.29 (5.04~5.54) | 5.26 (5.15~5.36) | 0.806 | 3.84 (3.57~4.12) | 3.85 (3.72~3.98) | 0.969 | |
| % of energy from sweets and beverage | 3.73 (3.58~3.88) | 3.64 (3.57~3.70) | 0.268 | 4.11 (3.97~4.26) | 3.96 (3.89~4.03) | 0.060 | |
| Balance of energy intake | % of energy from CHO | 3.16 (3.03~3.29) | 3.21 (3.16~3.26) | 0.452 | 3.21 (3.06~3.36) | 3.29 (3.22~3.35) | 0.337 |
| % of energy from fat | 4.01 (3.89~4.13) | 4.14 (4.11~4.18) | 0.044 | 3.98 (3.86~4.1) | 4.02 (3.97~4.07) | 0.546 | |
| Energy intake | 4.03 (3.91~4.16) | 3.93 (3.88~3.98) | 0.123 | 3.93 (3.78~4.08) | 3.94 (3.88~4.01) | 0.861 | |
| KHEI for all scores | 63.13 (62.42~63.84) | 64.21 (63.92~64.5) | 0.005 | 57.83 (57.11~58.55) | 58.91 (58.57~59.25) | 0.007 | |
| Female | Male | |||||
|---|---|---|---|---|---|---|
| Metabolic Syndrome | Normal | p-Value * | Metabolic Syndrome | Normal | p-Value * | |
| Energy (kcal/d) | 1808 (1764~1853) | 1812 (1792~1832) | 0.89 | 2401 (2339~2463) | 2406 (2374~2438) | 0.892 |
| Fat (En%) | 18.0 (17.6~18.4) | 18.6 (18.5~18.8) | 0.006 | 17.4 (17.0~17.8) | 17.6 (17.4~17.8) | 0.315 |
| Protein (En%) | 13.4 (13.2~13.5) | 13.5 (13.5~13.6) | 0.061 | 12.7 (12.5~12.8) | 12.6 (12.6~12.7) | 0.167 |
| Carbohydrate (En%) | 65.6 (65.1~66.2) | 65.1 (64.9~65.3) | 0.069 | 61.2 (60.6~61.8) | 61.4 (61.2~61.7) | 0.901 |
| Fiber (g/1000 kcal) | 8.89 (8.70~9.08) | 8.91 (8.82~9.00) | 0.271 | 11.17 (10.94~11.40) | 11.31 (11.22~11.40) | 0.842 |
| Calcium (mg/1000 kcal) | 213.3 (208.3~218.3) | 218.2 (216.0~220.3) | 0.002 | 248.7 (242.1~255) | 259.8 (257.4~262.1) | 0.09 |
| Iron (mg/1000 kcal) | 6.35 (6.24~6.45) | 6.31 (6.26~6.35) | 0.464 | 7.235 (7.121~7.348) | 7.281 (7.238~7.325) | 0.492 |
| V-C (mg/1000 kcal) | 40.4 (38.6~42.2) | 45.0 (43.9~46.2) | 0.003 | 65.2 (62.3~68.2) | 70.0 (68.8~71.2) | 0.001 |
| KHEI | Female | Male | All | |
|---|---|---|---|---|
| Model 1 | Q1 | Reference (1.000) | Reference (1.000) | Reference (1.000) |
| Q2 | 0.774 (0.606~0.988) | 0.694 (0.486~0.99) | 0.773 (0.639~0.935) | |
| Q3 | 0.697 (0.544~0.893) | 0.639 (0.451~0.905) | 0.694 (0.57~0.844) | |
| Q4 | 0.526 (0.42~0.657) | 0.475 (0.334~0.677) | 0.528 (0.439~0.636) | |
| Model 2 | Q1 | Reference (1.000) | Reference (1.000) | Reference (1.000) |
| Q2 | 0.818 (0.628~1.064) | 0.556 (0.379~0.816) | 0.75 (0.61~0.923) | |
| Q3 | 0.885 (0.678~1.155) | 0.527 (0.362~0.767) | 0.743 (0.602~0.916) | |
| Q4 | 0.692 (0.542~0.884) | 0.4 (0.272~0.587) | 0.582 (0.475~0.713) | |
| Model 3 | Q1 | Reference (1.000) | Reference (1.000) | Reference (1.000) |
| Q2 | 0.822 (0.631~1.071) | 0.593 (0.399~0.882) | 0.765 (0.619~0.946) | |
| Q3 | 0.892 (0.682~1.166) | 0.609 (0.412~0.902) | 0.794 (0.64~0.986) | |
| Q4 | 0.702 (0.55~0.897) | 0.486 (0.323~0.73) | 0.644 (0.52~0.798) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, S.; Kim, K.; Lee, B.-K.; Ahn, J. A Healthy Diet Rich in Calcium and Vitamin C Is Inversely Associated with Metabolic Syndrome Risk in Korean Adults from the KNHANES 2013–2017. Nutrients 2021, 13, 1312. https://doi.org/10.3390/nu13041312
Park S, Kim K, Lee B-K, Ahn J. A Healthy Diet Rich in Calcium and Vitamin C Is Inversely Associated with Metabolic Syndrome Risk in Korean Adults from the KNHANES 2013–2017. Nutrients. 2021; 13(4):1312. https://doi.org/10.3390/nu13041312
Chicago/Turabian StylePark, Sunmin, Kyungjin Kim, Byung-Kook Lee, and Jaeouk Ahn. 2021. "A Healthy Diet Rich in Calcium and Vitamin C Is Inversely Associated with Metabolic Syndrome Risk in Korean Adults from the KNHANES 2013–2017" Nutrients 13, no. 4: 1312. https://doi.org/10.3390/nu13041312
APA StylePark, S., Kim, K., Lee, B. -K., & Ahn, J. (2021). A Healthy Diet Rich in Calcium and Vitamin C Is Inversely Associated with Metabolic Syndrome Risk in Korean Adults from the KNHANES 2013–2017. Nutrients, 13(4), 1312. https://doi.org/10.3390/nu13041312