The Perceptions and Needs of French Parents and Pediatricians Concerning Information on Complementary Feeding
Abstract
:1. Introduction
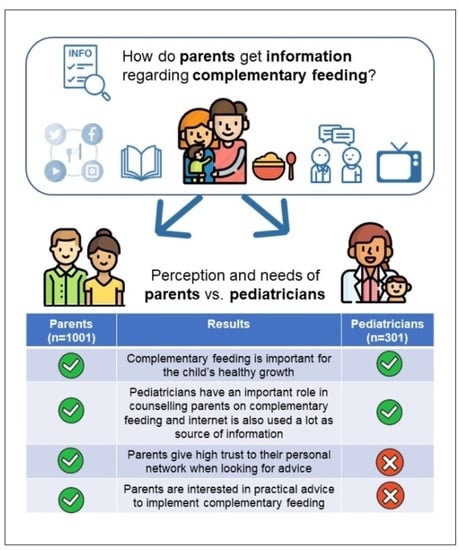
2. Materials and Methods
2.1. Web Surveys and Participant Sampling
2.2. Ethical Consideration
2.3. Data Analysis
3. Results
3.1. Study Populations
3.2. Perceptions of Parents and Pediatricians towards CoF and Feeding Children Aged 0–3
3.3. When Did Parents Look for Information on CoF and When Did Pediatricians Provide Advice?
3.4. Parents’ Perceptions about CoF Information and Pediatricians’ Perception about Parental Information Needs
3.5. Type of Content Parents Are Looking for Versus What Pediatricians Thought Is Important for Parents to Know
3.6. Sources Used by Parents to Learn About CoF (with Their Degrees of Influence), and Sources Pediatricians Thought Were Relevant for Parents
3.7. Appropriate Communication Formats According to Parents
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. “Appropriate Complementary Feeding”. e-Library of Evidence for Nutrition Actions (eLENA). Available online: https://www.who.int/elena/titles/complementary_feeding/en/#:~:text=Complementary%20feeding%20is%20defined%20as,needed%2C%20along%20with%20breast%20milk (accessed on 16 December 2020).
- Nicklaus, S. The Role of Dietary Experience in the Development of Eating Behavior during the First Years of Life. Ann. Nutr. Metab. 2017, 70, 241–245. [Google Scholar] [CrossRef] [Green Version]
- Alvarez-Pitti, J.; de Blas, A.; Lurbe, E. Innovations in Infant Feeding: Future Challenges and Opportunities in Obesity and Cardiometabolic Disease. Nutrients 2020, 12, 3508. [Google Scholar] [CrossRef] [PubMed]
- Theurich, M.A.; Grote, V.; Koletzko, B. Complementary feeding and long-term health implications. Nutr. Rev. 2020, 78, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Wood, A.C.; Blissett, J.; Brunstrom, J.M.; Carnell, S.; Faith, M.S.; Fisher, J.O.; Hayman, L.L.; Khalsa, A.S.; Hughes, S.O.; Miller, A.L.; et al. Caregiver Influences on Eating Behaviors in Young Children. J. Am. Hear. Assoc. 2020, 9, e014520. [Google Scholar] [CrossRef]
- Moura, A.F.; Aschemann-Witzel, J. A downturn or a window of opportunity? How Danish and French parents perceive changes in healthy eating in the transition to parenthood. Appetite 2020, 150, 104658. [Google Scholar] [CrossRef] [PubMed]
- Berge, J.M.; Tate, A.; Trofholz, A.; Fertig, A.R.; Miner, M.H.; Crow, S.; Neumark-Sztainer, D. Momentary Parental Stress and Food-Related Parenting Practices. Pediatrics 2017, 140, e20172295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gemmill, A.W.; Worotniuk, T.; Holt, C.J.; Skouteris, H.; Milgrom, J. Maternal Psychological Factors and Controlled Child Feeding Practices in Relation to Child Body Mass Index. Child. Obes. 2013, 9, 326–337. [Google Scholar] [CrossRef] [PubMed]
- Gouveia, M.; Canavarro, M.C.; Moreira, H. How can mindful parenting be related to emotional eating and overeating in childhood and adolescence? The mediating role of parenting stress and parental child-feeding practices. Appetite 2019, 138, 102–114. [Google Scholar] [CrossRef]
- Emley, E.A.; Taylor, M.B.; Musher-Eizenman, D.R. Mindful feeding and child dietary health. Eat. Behav. 2017, 24, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Norton, J.L.; Raciti, M.M. Co-creating healthful eating behaviors with very young children: The impact of information overload on primary caregivers. Health Mark. Q. 2016, 34, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Chouraqui, J.-P.; Tavoularis, G.; Emery, Y.; Francou, A.; Hébel, P.; Bocquet, M.; Hankard, R.; Turck, D. The French national survey on food consumption of children under 3 years of age—Nutri-Bébé 2013: Design, methodology, population sampling and feeding practices. Public Health Nutr. 2017, 21, 502–514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gildea, A.; Sloan, S.; Stewart, M. Sources of feeding advice in the first year of life: Who do parents value? Community Pract. J. Community Pract. Health Visit. Assoc. 2009, 82, 27–31. [Google Scholar]
- Demonteil, L.; Ksiazek, E.; Marduel, A.; Dusoulier, M.; Weenen, H.; Tournier, C.; Nicklaus, S. Patterns and predictors of food texture introduction in French children aged 4–36 months. Br. J. Nutr. 2018, 120, 1065–1077. [Google Scholar] [CrossRef]
- Díaz-Rodríguez, M.; Muñoz, C.P.; La Cruz, J.M.L.-D.; Fernández-Gutiérrez, M.; Bas-Sarmiento, P.; Ferriz-Mas, B.C. Effectiveness of a Multifactorial Intervention in the First 1000 Days of Life to Prevent Obesity and Overweight in Childhood: Study Protocol. Int. J. Environ. Res. Public Health 2020, 17, 2239. [Google Scholar] [CrossRef] [Green Version]
- Koletzko, B.; Fishbein, M.; Lee, W.S.; Moreno, L.; Mouane, N.; Mouzaki, M.; Verduci, E. Prevention of Childhood Obesity: A Position Paper of the Global Federation of International Societies of Paediatric Gastroenterology, Hepatology and Nutrition (FISPGHAN). J. Pediatr. Gastroenterol. Nutr. 2020, 70, 702–710. [Google Scholar] [CrossRef]
- Synnott, K.; Bogue, J.; Edwards, C.; Scott, J.; Higgins, S.; Norin, E.; Frías, D.; Amarri, S.; Ádám, R. Parental Perceptions of Feeding Practices in Five European Countries: An Exploratory Study. Eur. J. Clin. Nutr. 2007, 61, 946–956. [Google Scholar] [CrossRef] [Green Version]
- Bournez, M.; Ksiazek, E.; Charles, M.-A.; Lioret, S.; Brindisi, M.-C.; de Lauzon-Guillain, B.; Nicklaus, S. Frequency of Use of Added Sugar, Salt, and Fat in Infant Foods up to 10 Months in the Nationwide ELFE Cohort Study: Associated Infant Feeding and Caregiving Practices. Nutrients 2019, 11, 733. [Google Scholar] [CrossRef] [Green Version]
- Bournez, M.; Ksiazek, E.; Wagner, S.; Kersuzan, C.; Tichit, C.; Gojard, S.; Thierry, X.; Charles, M.-A.; Lioret, S.; de Lauzon-Guillain, B.; et al. Factors associated with the introduction of complementary feeding in the French ELFE cohort study. Matern. Child Nutr. 2017, 14, e12536. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, C.; Scholtens, P.A.; Lalanne, A.; Weenen, H.; Nicklaus, S. Development of healthy eating habits early in life. Review of recent evidence and selected guidelines. Appetite 2011, 57, 796–807. [Google Scholar] [CrossRef]
- Caton, S.J.; Ahern, S.M.; Hetherington, M. Vegetables by stealth. An exploratory study investigating the introduction of vegetables in the weaning period. Appetite 2011, 57, 816–825. [Google Scholar] [CrossRef]
- Nicklaus, S.; Remy, E. Early Origins of Overeating: Tracking Between Early Food Habits and Later Eating Patterns. Curr. Obes. Rep. 2013, 2, 179–184. [Google Scholar] [CrossRef] [Green Version]
- Service-public.fr. Suivi Médical De L’enfant: Examens Médicaux Obligatoires. Available online: https://www.service-public.fr/particuliers/vosdroits/F967 (accessed on 11 August 2020).
- Bocquet, A.; Vidailhet, M. Nutri-Bébé 2013 Study Part 2. How do French mothers feed their young children? Archives de Pédiatrie 2015, 22, 10S7–10S19. [Google Scholar] [CrossRef]
- ANSES. Avis De L’anses Relatif À L’actualisation Des Repères Alimentaires Du Pnns-Jeunes Enfants (0-3 Ans). 2019. Available online: https://www.anses.fr/fr/content/avis-de-lanses-relatif-%C3%A0-lactualisation-des-rep%C3%A8res-alimentaires-du-pnns-jeunes-enfants-0-3 (accessed on 19 February 2021).
- HCSP. Avis Relatif À La Révision Des Repères Alimentaires Pour Les Enfants Âgés De 0-36 Mois Et De 3-17 Ans. 2020. Available online: https://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=924 (accessed on 19 February 2021).
- INSEE. Statistics and Studies-Demography. 2015. Available online: https://www.insee.fr/fr/statistiques/3627376#consulter (accessed on 5 November 2019).
- Cochran, W. Sampling Techniques, 3rd ed.; John Wiley and Sons, Inc.: New York, NY, USA, 1977. [Google Scholar]
- Allcutt, C.; Sweeney, M.-R. An exploration of knowledge, attitudes and advice given by health professionals to parents in Ireland about the introduction of solid foods. A pilot study. BMC Public Health 2010, 10, 201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- R Foundation for Statistical Computing. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Savage, J.S.; Neshteruk, C.D.; Balantekin, K.N.; Birch, L.L. Low-Income Women’s Feeding Practices and Perceptions of Dietary Guidance: A Qualitative Study. Matern. Child Health J. 2016, 20, 2510–2517. [Google Scholar] [CrossRef] [PubMed]
- Tully, L.; Allen-Walker, V.; Spyreli, E.; McHugh, S.; Woodside, J.V.; Kearney, P.M.; McKinley, M.C.; Dean, M.; Kelly, C. Solid advice: Complementary feeding experiences among disadvantaged parents in two countries. Matern. Child Nutr. 2019, 15, 12801. [Google Scholar] [CrossRef]
- Heinig, M.J.; Follett, J.R.; Ishii, K.D.; Kavanagh-Prochaska, K.; Cohen, R.; Panchula, J. Barriers to Compliance with Infant-Feeding Recommendations Among Low-income Women. J. Hum. Lact. 2006, 22, 27–38. [Google Scholar] [CrossRef]
- Horodynski, M.; Olson, B.; Arndt, M.J.; Brophy-Herb, H.; Shirer, K.; Shemanski, R. Low-Income Mothers’ Decisions Regarding When and Why to Introduce Solid Foods to Their Infants: Influencing Factors. J. Community Health Nurs. 2007, 24, 101–118. [Google Scholar] [CrossRef]
- Kavanagh, K.F.; Habibi, M.; Anderson, K.; Spence, M. Caregiver- vs. Infant-Oriented Feeding: A Model of Infant-Feeding Strategies among Special Supplemental Nutrition Program for Women, Infants, and Children Participants in Rural East Tennessee. J. Am. Diet. Assoc. 2010, 110, 1485–1491. [Google Scholar] [CrossRef]
- Russell, C.G.; Taki, S.; Azadi, L.; Campbell, K.J.; Laws, R.; Elliott, R.; Denney-Wilson, E. A qualitative study of the infant feeding beliefs and behaviours of mothers with low educational attainment. BMC Pediatr. 2016, 16, 69. [Google Scholar] [CrossRef] [Green Version]
- Heinig, M.J.; Ishii, K.D.; Bañuelos, J.L.; Campbell, E.; O’Loughlin, C.; Becerra, L.E.V. Sources and Acceptance of Infant-Feeding Advice Among Low-Income Women. J. Hum. Lact. 2009, 25, 163–172. [Google Scholar] [CrossRef]
- Ashida, S.; Lynn, F.B.; A Williams, N.; Schafer, E.J. Competing infant feeding information in mothers’ networks: Advice that supports v. undermines clinical recommendations. Public Health Nutr. 2015, 19, 1200–1210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banti, T.; Carsin, A.; Chabrol, B.; Reynaud, R.; Fabre, A. Diversification alimentaire du nourrisson. Évaluation des pratiques en regard des recommandations françaises actuelles chez les pédiatres varois et les internes affectés à la faculté d’Aix-Marseille. Archives de Pédiatrie 2016, 23, 1018–1027. [Google Scholar] [CrossRef] [PubMed]
- Chouraqui, J.-P.; Delmas, B.; Le Bris, M.; Bellaiche, M.; Jung, C.; Hanh, T. Physicians advice, parental practice and adherence to doctor’s advice: An original survey on infant feeding. BMC Pediatr. 2019, 19, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, C.C.; Lumeng, J.C.; Miller, A.L. Development and preliminary validation of a feeding coparenting scale (FCS). Appetite 2019, 139, 152–158. [Google Scholar] [CrossRef]
- Kalinowski, A.; Krause, K.; Berdejo, C.; Harrell, K.; Rosenblum, K.; Lumeng, J.C. Beliefs about the Role of Parenting in Feeding and Childhood Obesity among Mothers of Lower Socioeconomic Status. J. Nutr. Educ. Behav. 2012, 44, 432–437. [Google Scholar] [CrossRef] [Green Version]
- Walton, K.; Haycraft, E.; Jewell, K.; Breen, A.; Simpson, J.R.; Haines, J. The Family Mealtime Observation Study (FaMOS): Exploring the Role of Family Functioning in the Association between Mothers’ and Fathers’ Food Parenting Practices and Children’s Nutrition Risk. Nutrients 2019, 11, 630. [Google Scholar] [CrossRef] [Green Version]
- Saxbe, D.; Rossin-Slater, M.; Goldenberg, D. The transition to parenthood as a critical window for adult health. Am. Psychol. 2018, 73, 1190–1200. [Google Scholar] [CrossRef]
- Martins, C.A. Transition to parenthood: Consequences on health and well-being. A qualitative study. Enfermería Clínica 2019, 29, 225–233. [Google Scholar] [CrossRef]
- Munns, A.; Watts, R.; Hegney, D.; Walker, R. Effectiveness and experiences of families and support workers participating in peer-led parenting support programs delivered as home visiting programs. JBI Database Syst. Rev. Implement. Rep. 2016, 14, 167–208. [Google Scholar] [CrossRef]
- Schwartz, C.; Madrelle, J.; Vereijken, C.; Weenen, H.; Nicklaus, S.; Hetherington, M. Complementary feeding and “donner les bases du goût” (providing the foundation of taste). A qualitative approach to understand weaning practices, attitudes and experiences by French mothers. Appetite 2013, 71, 321–331. [Google Scholar] [CrossRef]


| Parents (N = 1001) | Pediatricians (N = 301) | ||||
|---|---|---|---|---|---|
| Characteristics | N (%) | Characteristics | N (%) | ||
| Age | Less than 35 years old | 604 (60) | Age | ≤30 years old | 12 (4) |
| 31–40 years old | 78 (26) | ||||
| 41–50 years old | 45 (15) | ||||
| 51–60 years old | 75 (25) | ||||
| 35 years old and more | 397 (40) | ≥61 years old | 91 (30) | ||
| Age of the youngest child | <12 months | 277 (28) | Years of working experience | 0–10 years | 80 (26) |
| 12–23 months | 260 (26) | 11–20 years | 57 (19) | ||
| 24–35 months | 260 (26) | 21–30 years | 75 (25) | ||
| ≥36 months | 204 (20) | More than 30 years | 89 (30) | ||
| Gender | Men | 198 (20) | Gender | Men | 60 (20) |
| Women | 803 (80) | Women | 241 (80) | ||
| Parity | Primiparous | 388 (39) | Having children | Yes | 260 (86) |
| Multiparous | 613 (61) | No | 40 (14) | ||
| Education level 1 | <A level | 179 (18) | Working area | Rural | 29 (10) |
| ≥A level | 822 (82) | Urban | 272 (90) | ||
| Socio-professional category of the household reference parent 2 | High | 456 (46) | / | / | / |
| Low | 501 (50) | ||||
| No occupation/retired | 44 (4) | ||||
| Self-perception of household financial situation 3 | Good | 457 (46) | / | / | / |
| Difficult | 535 (53) | ||||
| No answer | 9 (1) | ||||
| Parents (N = 1001) | |
|---|---|
| Communication Format | N (%) |
| Subtotal Website or application | 79 (790) |
| Smartphone application | 43 (434) |
| Websites | 38 (383) |
| Interactive space on the Internet (Blogs, chats, forums…) | 35 (347) |
| Subtotal paper format | 58 (584) |
| Multi-page paper booklet | 42 (417) |
| 1-page paper brochure | 23 (232) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Rosso, S.; Schwartz, C.; Ducrot, P.; Nicklaus, S. The Perceptions and Needs of French Parents and Pediatricians Concerning Information on Complementary Feeding. Nutrients 2021, 13, 2142. https://doi.org/10.3390/nu13072142
De Rosso S, Schwartz C, Ducrot P, Nicklaus S. The Perceptions and Needs of French Parents and Pediatricians Concerning Information on Complementary Feeding. Nutrients. 2021; 13(7):2142. https://doi.org/10.3390/nu13072142
Chicago/Turabian StyleDe Rosso, Sofia, Camille Schwartz, Pauline Ducrot, and Sophie Nicklaus. 2021. "The Perceptions and Needs of French Parents and Pediatricians Concerning Information on Complementary Feeding" Nutrients 13, no. 7: 2142. https://doi.org/10.3390/nu13072142
APA StyleDe Rosso, S., Schwartz, C., Ducrot, P., & Nicklaus, S. (2021). The Perceptions and Needs of French Parents and Pediatricians Concerning Information on Complementary Feeding. Nutrients, 13(7), 2142. https://doi.org/10.3390/nu13072142