Carnosine Did Not Affect Vascular and Metabolic Outcomes in Patients with Prediabetes and Type 2 Diabetes: A 14-Week Randomized Controlled Trial
Abstract
:1. Introduction
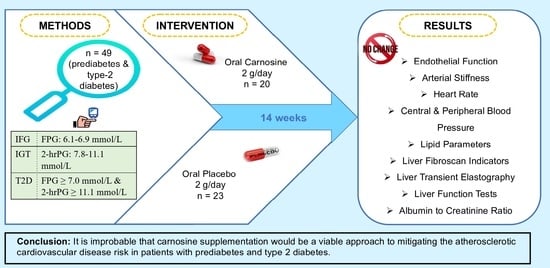
2. Materials and Methods
2.1. Study Design and Participants
2.2. Ethics
2.3. Sample Size Calculation
2.4. Screening
2.5. Intervention and Random Assignment
2.6. Outcome Measures
2.6.1. Anthropometric Measurements
2.6.2. Blood Pressure
2.6.3. Lipid Profile
2.6.4. Liver Fibroscan
2.6.5. Liver Function Tests and Renal Outcomes
2.6.6. Endothelial Function
2.6.7. Arterial Stiffness and Central Pressure
2.6.8. International Physical Activity Questionnaire (IPAQ)
2.6.9. Record of Habitual Diet
2.7. Statistical Analysis
3. Results
3.1. Study Population and Baseline Characteristics
3.2. Effect of Carnosine Supplementation on Hepatorenal Outcomes
3.3. Effect of Carnosine Supplementation on Cardiovascular Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- IDF Diabetes Atlas. Diabetes around the World in 2021. Available online: https://diabetesatlas.org/ (accessed on 7 July 2021).
- Ma, C.-X.; Ma, X.-N.; Guan, C.-H.; Li, Y.-D.; Mauricio, D.; Fu, S.-B. Cardiovascular disease in type 2 diabetes mellitus: Progress toward personalized management. Cardiovasc. Diabetol. 2022, 21, 74. [Google Scholar] [CrossRef]
- International Diabetes Federation. Diabetes and Cardiovascular Disease. Available online: https://idf.org/cvd (accessed on 7 July 2021).
- Rangel, E.B.; Rodrigues, C.O.; De Sa, J.R. Micro-and macrovascular complications in diabetes mellitus: Preclinical and clinical studies. J. Diabetes Res. 2019, 2019, 2161085. [Google Scholar] [CrossRef]
- Takeda, Y.; Matoba, K.; Sekiguchi, K.; Nagai, Y.; Yokota, T.; Utsunomiya, K.; Nishimura, R. Endothelial dysfunction in diabetes. Biomedicines 2020, 8, 182. [Google Scholar] [CrossRef] [PubMed]
- Palladino, R.; Tabak, A.G.; Khunti, K.; Valabhji, J.; Majeed, A.; Millett, C.; Vamos, E.P. Association between pre-diabetes and microvascular and macrovascular disease in newly diagnosed type 2 diabetes. BMJ Open Diabetes Res. Care 2020, 8, e001061. [Google Scholar] [CrossRef] [PubMed]
- Hahad, O.; Wild, P.S.; Prochaska, J.H.; Schulz, A.; Hermanns, I.; Lackner, K.J.; Pfeiffer, N.; Schmidtmann, I.; Beutel, M.; Gori, T. Endothelial function assessed by digital volume plethysmography predicts the development and progression of type 2 diabetes mellitus. J. Am. Heart Assoc. 2019, 8, e012509. [Google Scholar] [CrossRef]
- Tousoulis, D.; Kampoli, A.-M.; Stefanadis, C. Diabetes mellitus and vascular endothelial dysfunction: Current perspectives. Curr. Vasc. Pharmacol. 2012, 10, 19–32. [Google Scholar] [CrossRef]
- Odegaard, A.O.; Jacobs, D.R.; Sanchez, O.A.; Goff, D.C.; Reiner, A.P.; Gross, M.D. Oxidative stress, inflammation, endothelial dysfunction and incidence of type 2 diabetes. Cardiovasc. Diabetol. 2016, 15, 51. [Google Scholar] [CrossRef] [PubMed]
- Chirinos, J.A. Large artery stiffness and new-onset diabetes. Am. Heart Assoc. 2020, 127, 1499–1501. [Google Scholar] [CrossRef]
- Chmielewska, K.; Dzierzbicka, K.; Inkielewicz-Stępniak, I.; Przybyłowska, M. Therapeutic potential of carnosine and its derivatives in the treatment of human diseases. Chem. Res. Toxicol. 2020, 33, 1561–1578. [Google Scholar] [CrossRef]
- Menini, S.; Iacobini, C.; Fantauzzi, C.B.; Pugliese, G. L-carnosine and its derivatives as new therapeutic agents for the prevention and treatment of vascular complications of diabetes. Curr. Med. Chem. 2020, 27, 1744–1763. [Google Scholar] [CrossRef]
- Feehan, J.; Hariharan, R.; Buckenham, T.; Handley, C.; Bhatnagar, A.; Baba, S.P.; de Courten, B. Carnosine as a potential therapeutic for the management of peripheral vascular disease. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 2289–2296. [Google Scholar] [CrossRef]
- Menon, K.; de Courten, B.; Magliano, D.J.; Ademi, Z.; Liew, D.; Zomer, E. The Cost-Effectiveness of Supplemental Carnosine in Type 2 Diabetes. Nutrients 2022, 14, 215. [Google Scholar] [CrossRef] [PubMed]
- Menini, S.; Iacobini, C.; Ricci, C.; Scipioni, A.; Fantauzzi, C.B.; Giaccari, A.; Salomone, E.; Canevotti, R.; Lapolla, A.; Orioli, M. D-Carnosine octylester attenuates atherosclerosis and renal disease in ApoE null mice fed a Western diet through reduction of carbonyl stress and inflammation. Br. J. Pharmacol. 2012, 166, 1344–1356. [Google Scholar] [CrossRef] [PubMed]
- Aldini, G.; Orioli, M.; Rossoni, G.; Savi, F.; Braidotti, P.; Vistoli, G.; Yeum, K.J.; Negrisoli, G.; Carini, M. The carbonyl scavenger carnosine ameliorates dyslipidaemia and renal function in Zucker obese rats. J. Cell Mol. Med. 2011, 15, 1339–1354. [Google Scholar] [CrossRef]
- Albrecht, T.; Schilperoort, M.; Zhang, S.; Braun, J.D.; Qiu, J.; Rodriguez, A.; Pastene, D.O.; Krämer, B.K.; Köppel, H.; Baelde, H. Carnosine attenuates the development of both type 2 diabetes and diabetic nephropathy in BTBR ob/ob mice. Sci. Rep. 2017, 7, 44492. [Google Scholar] [CrossRef]
- Mong, M.-C.; Chao, C.-Y.; Yin, M.-C. Histidine and carnosine alleviated hepatic steatosis in mice consumed high saturated fat diet. Eur. J. Pharmacol. 2011, 653, 82–88. [Google Scholar] [CrossRef]
- Ali, S.; Rasul, A.; Latif, N.; Aleem, S.B.; Zia, R.; Khan, B. Effect of Levo-Carnosine on Biomarkers of Oxidative Stress and Hepatotoxicity in Cisplatin-Treated Male Sprague Dawley Rats. Pak. Armed Forces Med. J. 2022, 72, 1334–1338. [Google Scholar]
- Fujii, T.; Takaoka, M.; Muraoka, T.; Kurata, H.; Tsuruoka, N.; Ono, H.; Kiso, Y.; Tanaka, T.; Matsumura, Y. Preventive effect of L-carnosine on ischemia/reperfusion-induced acute renal failure in rats. Eur. J. Pharmacol. 2003, 474, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Schön, M.; Mousa, A.; Berk, M.; Chia, W.L.; Ukropec, J.; Majid, A.; Ukropcová, B.; De Courten, B. The potential of carnosine in brain-related disorders: A comprehensive review of current evidence. Nutrients 2019, 11, 1196. [Google Scholar] [CrossRef]
- Menon, K.A.; Mousa, A.; Courten, B.D. Effect of carnosine supplementation on cardiometabolic risk factors in obesity, prediabetes, and diabetes—A meta-analysis of randomized controlled trials. Diabetes 2018, 67 (Suppl. 1), 55-LB. [Google Scholar] [CrossRef]
- Lombardi, C.; Carubelli, V.; Lazzarini, V.; Vizzardi, E.; Bordonali, T.; Ciccarese, C.; Castrini, A.I.; Dei Cas, A.; Nodari, S.; Metra, M. Effects of oral administration of orodispersible levo-carnosine on quality of life and exercise performance in patients with chronic heart failure. Nutrition 2015, 31, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Siriwattanasit, N.; Satirapoj, B.; Supasyndh, O. Effect of Oral carnosine supplementation on urinary TGF-β in diabetic nephropathy: A randomized controlled trial. BMC Nephrol. 2021, 22, 236. [Google Scholar] [CrossRef]
- Peng, W.; Mao, P.; Liu, L.; Chen, K.; Zhong, Y.; Xia, W.; Guo, Q.; Tan, S.C.; Rahmani, J.; Varkaneh, H.K. Effect of carnosine supplementation on lipid profile, fasting blood glucose, HbA1C and insulin resistance: A systematic review and meta-analysis of long-term randomized controlled trials. Complement. Ther. Med. 2020, 48, 102241. [Google Scholar] [CrossRef]
- Chan, A.-W.; Tetzlaff, J.M.; Gøtzsche, P.C.; Altman, D.G.; Mann, H.; Berlin, J.A.; Dickersin, K.; Hróbjartsson, A.; Schulz, K.F.; Parulekar, W.R. SPIRIT 2013 explanation and elaboration: Guidance for protocols of clinical trials. BMJ 2013, 346, e7586. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- De Courten, B.; Jakubova, M.; De Courten, M.P.; Kukurova, I.J.; Vallova, S.; Krumpolec, P.; Valkovic, L.; Kurdiova, T.; Garzon, D.; Barbaresi, S. Effects of carnosine supplementation on glucose metabolism: Pilot clinical trial. Obesity 2016, 24, 1027–1034. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.M.M.; Zimmet, P.Z. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus. Provisional report of a WHO consultation. Diabet. Med. 1998, 15, 539–553. [Google Scholar] [CrossRef]
- Afdhal, N.H. Fibroscan (transient elastography) for the measurement of liver fibrosis. Gastroenterol. Hepatol. 2012, 8, 605. [Google Scholar]
- Cheng, K.; Cameron, J.D.; Tung, M.; Mottram, P.M.; Meredith, I.T.; Hope, S.A. Association of left ventricular motion and central augmentation index in healthy young men. J. Hypertens. 2012, 30, 2395–2402. [Google Scholar] [CrossRef]
- Wilkinson, I.B.; McEniery, C.M.; Schillaci, G.; Boutouyrie, P.; Segers, P.; Donald, A.; Chowienczyk, P.J. ARTERY Society guidelines for validation of non-invasive haemodynamic measurement devices: Part 1, arterial pulse wave velocity. Artery Res. 2010, 4, 34–40. [Google Scholar] [CrossRef]
- Zoungas, S.; Cameron, J.D.; Kerr, P.G.; Wolfe, R.; Muske, C.; McNeil, J.J.; McGrath, B.P. Association of carotid intima-medial thickness and indices of arterial stiffness with cardiovascular disease outcomes in CKD. Am. J. Kidney Dis. 2007, 50, 622–630. [Google Scholar] [CrossRef]
- Martin, C.A.; Cameron, J.D.; Chen, S.S.; McGrath, B.P. Two hour glucose post loading: A biomarker of cardiovascular risk in isolated clinic hypertension. J. Hypertens. 2011, 29, 749–757. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Boldyrev, A.A.; Aldini, G.; Derave, W. Physiology and pathophysiology of carnosine. Physiol. Rev. 2013, 93, 1803–1845. [Google Scholar] [CrossRef]
- Chengappa, K.R.; Turkin, S.R.; DeSanti, S.; Bowie, C.R.; Brar, J.S.; Schlicht, P.J.; Murphy, S.L.; Hetrick, M.L.; Bilder, R.; Fleet, D. A preliminary, randomized, double-blind, placebo-controlled trial of L-carnosine to improve cognition in schizophrenia. Schizophr. Res. 2012, 142, 145–152. [Google Scholar] [CrossRef]
- Creighton, J.V.; de Souza Gonçalves, L.; Artioli, G.G.; Tan, D.; Elliott-Sale, K.J.; Turner, M.D.; Doig, C.L.; Sale, C. Physiological Roles of Carnosine in Myocardial Function and Health. Adv. Nutr. 2022, 13, 1914–1929. [Google Scholar] [CrossRef]
- Baye, E.; Ukropcova, B.; Ukropec, J.; Hipkiss, A.; Aldini, G.; De Courten, B. Physiological and therapeutic effects of carnosine on cardiometabolic risk and disease. Amino Acids 2016, 48, 1131–1149. [Google Scholar] [CrossRef] [PubMed]
- Aldini, G.; de Courten, B.; Regazzoni, L.; Gilardoni, E.; Ferrario, G.; Baron, G.; Altomare, A.; D’Amato, A.; Vistoli, G.; Carini, M. Understanding the antioxidant and carbonyl sequestering activity of carnosine: Direct and indirect mechanisms. Free Radic. Res. 2021, 55, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Brown, B.E.; Kim, C.H.; Torpy, F.R.; Bursill, C.A.; McRobb, L.S.; Heather, A.K.; Davies, M.J.; Van Reyk, D.M. Supplementation with carnosine decreases plasma triglycerides and modulates atherosclerotic plaque composition in diabetic apo E−/− mice. Atherosclerosis 2014, 232, 403–409. [Google Scholar] [CrossRef]
- Barski, O.A.; Xie, Z.; Baba, S.P.; Sithu, S.D.; Agarwal, A.; Cai, J.; Bhatnagar, A.; Srivastava, S. Dietary carnosine prevents early atherosclerotic lesion formation in apolipoprotein E–Null mice. Arterioscler. Thromb. Vasc. Biol. 2013, 33, 1162–1170. [Google Scholar] [CrossRef]
- Menini, S.; Iacobini, C.; Ricci, C.; Fantauzzi, C.B.; Pugliese, G. Protection from diabetes-induced atherosclerosis and renal disease by D-carnosine-octylester: Effects of early vs late inhibition of advanced glycation end-products in Apoe-null mice. Diabetologia 2015, 58, 845–853. [Google Scholar] [CrossRef] [PubMed]
- Jukić, I.; Kolobarić, N.; Stupin, A.; Matić, A.; Kozina, N.; Mihaljević, Z.; Mihalj, M.; Šušnjara, P.; Stupin, M.; Ćurić, Ž.B. Carnosine, small but mighty—Prospect of use as functional ingredient for functional food formulation. Antioxidants 2021, 10, 1037. [Google Scholar] [CrossRef] [PubMed]
- Gimbrone Jr, M.A.; García-Cardeña, G. Endothelial cell dysfunction and the pathobiology of atherosclerosis. Circ. Res. 2016, 118, 620–636. [Google Scholar] [CrossRef] [PubMed]
- Daiber, A.; Steven, S.; Weber, A.; Shuvaev, V.V.; Muzykantov, V.R.; Laher, I.; Li, H.; Lamas, S.; Münzel, T. Targeting vascular (endothelial) dysfunction. Br. J. Pharmacol. 2017, 174, 1591–1619. [Google Scholar] [CrossRef] [PubMed]
- Young, H.; Benton, D.; Carter, N. The effect of chicken extract on mood, cognition and heart rate variability. Nutrients 2015, 7, 887–904. [Google Scholar] [CrossRef]
- Nagai, K.; Tanida, M.; Niijima, A.; Tsuruoka, N.; Kiso, Y.; Horii, Y.; Shen, J.; Okumura, N. Role of L-carnosine in the control of blood glucose, blood pressure, thermogenesis, and lipolysis by autonomic nerves in rats: Involvement of the circadian clock and histamine. Amino Acids 2012, 43, 97–109. [Google Scholar] [CrossRef]
- Al-Sawalha, N.A.; Alshogran, O.Y.; Awawdeh, M.S.; Almomani, B.A. The effects of l-Carnosine on development of metabolic syndrome in rats. Life Sci. 2019, 237, 116905. [Google Scholar] [CrossRef]
- Niijima, A.; Okui, T.; Matsumura, Y.; Yamano, T.; Tsuruoka, N.; Kiso, Y.; Nagai, K. Effects of L-carnosine on renal sympathetic nerve activity and DOCA-salt hypertension in rats. Auton. Neurosci. 2002, 97, 99–102. [Google Scholar] [CrossRef]
- Greene, S.M.; Margolis, F.L.; Grillo, M.; Fisher, H. Enhanced carnosine (β-alanyl-L-histidine) breakdown and histamine metabolism following treatment with compound 4880. Eur. J. Pharmacol. 1984, 99, 79–84. [Google Scholar] [CrossRef]
- Ririe, D.G.; Roberts, P.R.; Shouse, M.N.; Zaloga, G.P. Vasodilatory actions of the dietary peptide carnosine. Nutrition 2000, 16, 168–172. [Google Scholar] [CrossRef]
- Szcześniak, D.; Budzeń, S.; Kopeć, W.; Rymaszewska, J. Anserine and carnosine supplementation in the elderly: Effects on cognitive functioning and physical capacity. Arch. Gerontol. Geriatr. 2014, 59, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.T. Resting heart rate and relation to disease and longevity: Past, present and future. Scand. J. Clin. Lab. Investig. 2019, 79, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Yapislar, H.; Taskin, E. L-carnosine alters some hemorheologic and lipid peroxidation parameters in nephrectomized rats. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2014, 20, 399. [Google Scholar]
- Vickers, N.J. Animal communication: When i’m calling you, will you answer too? Curr. Biol. 2017, 27, R713–R715. [Google Scholar] [CrossRef]
- Rashid, I.; van Reyk, D.M.; Davies, M.J. Carnosine and its constituents inhibit glycation of low-density lipoproteins that promotes foam cell formation in vitro. FEBS Lett. 2007, 581, 1067–1070. [Google Scholar] [CrossRef]
- Kim, M.Y.; Kim, E.J.; Kim, Y.-N.; Choi, C.; Lee, B.-H. Effects of α-lipoic acid and L-carnosine supplementation on antioxidant activities and lipid profiles in rats. Nutr. Res. Pract. 2011, 5, 421–428. [Google Scholar] [CrossRef] [PubMed]
- Baye, E.; Ukropec, J.; De Courten, M.P.; Vallova, S.; Krumpolec, P.; Kurdiova, T.; Aldini, G.; Ukropcova, B.; De Courten, B. Effect of carnosine supplementation on the plasma lipidome in overweight and obese adults: A pilot randomised controlled trial. Sci. Rep. 2017, 7, 17458. [Google Scholar] [CrossRef] [PubMed]
- Jamshidzadeh, A.; Heidari, R.; Latifpour, Z.; Ommati, M.M.; Abdoli, N.; Mousavi, S.; Azarpira, N.; Zarei, A.; Zarei, M.; Asadi, B. Carnosine ameliorates liver fibrosis and hyperammonemia in cirrhotic rats. Clin. Res. Hepatol. Gastroenterol. 2017, 41, 424–434. [Google Scholar] [CrossRef]
- Peters, V.; Schmitt, C.P.; Zschocke, J.; Gross, M.-L.; Brismar, K.; Forsberg, E. Carnosine treatment largely prevents alterations of renal carnosine metabolism in diabetic mice. Amino Acids 2012, 42, 2411–2416. [Google Scholar] [CrossRef]
- Şahin, S.; Burukoğlu Dönmez, D. Effects of carnosine (beta-alanyl-L-histidine) in an experimental rat model of acute kidney injury due to septic shock. Med. Sci. Monit. 2018, 24, 305–316. [Google Scholar] [CrossRef]
- Janssen, B.; Hohenadel, D.; Brinkkoetter, P.; Peters, V.; Rind, N.; Fischer, C.; Rychlik, I.; Cerna, M.; Romzova, M.; de Heer, E. Carnosine as a protective factor in diabetic nephropathy: Association with a leucine repeat of the carnosinase gene CNDP1. Diabetes 2005, 54, 2320–2327. [Google Scholar] [CrossRef] [PubMed]
- Aydın, A.F.; Küçükgergin, C.; Bingül, İ.; Doğan-Ekici, I.; Doğru-Abbasoğlu, S.; Uysal, M. Effect of carnosine on renal function, oxidation and glycation products in the kidneys of high-fat diet/streptozotocin-induced diabetic rats. Exp. Clin. Endocrinol. Diabetes 2017, 125, 282–289. [Google Scholar]
- Rodriguez-Niño, A.; Pastene, D.O.; Hettler, S.A.; Qiu, J.; Albrecht, T.; Vajpayee, S.; Perciaccante, R.; Gretz, N.; Bakker, S.J.; Krämer, B.K. Influence of carnosine and carnosinase-1 on diabetes-induced afferent arteriole vasodilation: Implications for glomerular hemodynamics. Am. J. Physiol.-Ren. Physiol. 2022, 323, F69–F80. [Google Scholar] [CrossRef] [PubMed]
- Riedl, E.; Pfister, F.; Braunagel, M.; Brinkkötter, P.; Sternik, P.; Deinzer, M.; Bakker, S.J.; Henning, R.H.; van den Born, J.; Krämer, B.K. Carnosine prevents apoptosis of glomerular cells and podocyte loss in STZ diabetic rats. Cell. Physiol. Biochem. 2011, 28, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Elbarbary, N.S.; Ismail, E.A.R.; El-Naggar, A.R.; Hamouda, M.H.; El-Hamamsy, M. The effect of 12 weeks carnosine supplementation on renal functional integrity and oxidative stress in pediatric patients with diabetic nephropathy: A randomized placebo-controlled trial. Pediatr. Diabetes 2018, 19, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Ranganathan, P.; Pramesh, C.; Aggarwal, R. Common pitfalls in statistical analysis: Intention-to-treat versus per-protocol analysis. Perspect. Clin. Res. 2016, 7, 144. [Google Scholar] [CrossRef]

| Characteristic | Carnosine Group (n = 20) | Placebo Group (n = 23) |
|---|---|---|
| Age, year | 53.7 (48.5–59.4) a | 52 (42.3–59.3) |
| Men, n (%) | 14 (70) | 16 (69.56) |
| Caucasian | 11 (55) | 11 (47.82) |
| South and Central Asian | 6 (30) | 6 (26.08) |
| Southeast and Northeast Asian | 3 (15) | 5 (21.73) |
| Other b | - | 1 (4.34) |
| Total energy, kj | 7935.80 ± 1303.64 | 8206.88 ± 1319.38 |
| Physical activity c, IPAQ-METS score d | 2400 (798–4878) | 1332 (390–2736) |
| Weight, kg | 86.92 ± 21.22 | 82.02 ± 13.61 |
| BMI, kg/m2 | 30.54 ± 4.74 | 28.29 ± 3.66 |
| HOMA-IR | 2.88 ± 1.39 | 2.35 ± 1.08 |
| HbA1c, % | 6.48 ± 0.63 | 6.65 ± 0.83 |
| SBP, mmHg | 124.94 ± 12.97 | 122.62 ± 11.46 |
| DBP, mmHg | 81.94 ± 8.59 | 80.71 ± 5.81 |
| Family history of diabetes e, n (%) | 5 (25) | 4 (17.39) |
| Patients with T2DM, n | 11 (55) | 17 (73.91) |
| Dyslipidaemia, n | 2 (10) | 4 (17.39) |
| Nephropathy, n | 2 (10) | 2 (8.69) |
| Oral glucose-lowering agents, n | 7 (35) | 7 (30.43) |
| Diet therapy, n | 5 (25) | 10 (43.47) |
| No treatment, n | 8 (40) | 6 (26.08) |
| Outcome Variable | Carnosine Group (n = 20) | Placebo Group (n = 23) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-Up | p a | Change | Baseline | Follow-Up | p b | Change | p c | ||
| Lipid profile | TG (mmol/L) | 1.66 ± 0.88 d | 1.58 ± 0.73 | >0.99 | −0.01 | 1.72 ± 0.67 | 1.86 ± 0.75 | >0.99 | 0.02 | 0.231 |
| TC (mmol/L) | 5.36 ± 0.89 | 5.29 ± 0.71 | >0.99 | −0.003 | 5.30 ± 0.97 | 5.14 ± 0.85 | >0.99 | −0.01 | 0.428 | |
| LDL-C (mmol/L) | 3.36 ± 0.6 | 3.42 ± 0.57 | >0.99 | 0.05 | 3.19 ± 0.6 | 3.04 ± 0.55 | >0.99 | −0.14 | 0.060 | |
| HDL-C (mmol/L) | 1.13 ± 0.26 | 1.1 ± 0.23 | >0.99 | −0.03 | 1.19 ± 0.26 | 1.15 ± 0.26 | >0.99 | −0.03 | 0.810 | |
| LDL-C/HDL-C | 3.1 ± 0.85 | 3.15 ± 0.79 | >0.99 | 0.11 | 2.81 ± 0.68 | 2.68 ± 0.75 | >0.99 | −0.13 | 0.100 | |
| Hepatic outcomes | ALT (U/L) | 38.32 ± 18.64 | 36 ± 15.50 | >0.99 | −2.32 | 38.19 ± 16.34 | 34.33 ± 15.55 | 0.39 | −3.86 | 0.321 |
| GGT (U/L) | 34.47 ± 13.35 | 34.53 ± 12.90 | >0.99 | 0.05 | 34.33 ± 12.57 | 32.57 ± 12.13 | >0.99 | −1.76 | 0.476 | |
| ALP (U/L) | 82.63 ± 18.23 | 79.42 ± 16.13 | >0.99 | −3.21 | 79.57 ± 22.06 | 75.48 ± 18.35 | >0.99 | −4.10 | 0.569 | |
| IQR | 33.17 ± 9.57 | 27.17 ± 11.28 | >0.99 | −6 | 34.53 ± 14.01 | 30.53 ± 11.39 | >0.99 | −4 | 0.470 | |
| Median stiffness (KPa) | 5.66 ± 2.00 | 5.72 ± 1.59 | >0.99 | 0.01 | 5.13 ± 1.64 | 5.51 ± 1.24 | >0.99 | 0.04 | 0.826 | |
| IQR to Median stiffness | 0.13 ± 0.06 | 0.15 ± 0.07 | >0.99 | 0.02 | 0.13 ± 0.06 | 0.13 ± 0.05 | >0.99 | 0.004 | 0.390 | |
| CAP (dB/m) | 290.6 ± 72.21 | 301 ± 61.86 | >0.99 | 10.4 | 288.56 ± 61.04 | 293.78 ± 64.68 | >0.99 | 5.22 | 0.655 | |
| Renal outcomes | Sodium (mmol/L) | 139 (137–140) e | 138 (137–139) | >0.99 | −0.21 | 138 (137–140) | 138.5 (137–140) | >0.99 | 0.09 | 0.521 |
| Potassium (mmol/L) | 4.23 ± 0.26 | 4.16 ± 0.22 | >0.99 | −0.06 | 4.20 ± 0.25 | 4.19 ± 0.20 | >0.99 | −0.009 | 0.555 | |
| Bicarbonate (mmol/L) | 25.63 ± 2.21 | 25.63 ± 2.40 | >0.99 | 0 | 25.91 ± 1.74 | 25.68 ± 2.12 | >0.99 | −0.23 | 0.763 | |
| Urea (mmol/L) | 5.24 ± 0.87 | 5.43 ± 1.14 | >0.99 | 0.18 | 5.18 ± 1.21 | 5.68 ± 1.54 | 0.91 | 0.5 | 0.385 | |
| Total bilirubin (µmol/L) | 11.63 ± 3.71 | 12.32 ± 3.93 | >0.99 | 0.68 | 12.67 ± 3.90 | 12.14 ± 4.54 | >0.99 | −0.52 | 0.200 | |
| Albumin (g/L) | 40.37 ± 3.27 | 39 ± 2.90 | 0.13 | −1.37 | 41.29 ± 2.75 | 40.24 ± 1.94 | >0.99 | −1.05 | 0.198 | |
| Creatinine (µmol/L) | 64.21 ± 8.86 | 66.63 ± 8.00 | 0.37 | 2.42 | 71.86 ± 15.99 | 73.27 ± 16.68 | >0.99 | 1.41 | 0.765 | |
| ACR | 9.60 ± 1.37 | 8.91 ± 1.17 | 0.007 | −0.69 | 8.99 ± 2.12 | 8.58 ± 2.06 | 0.32 | −0.41 | 0.541 | |
| Outcome Variable | Carnosine Group (n = 20) | Placebo Group (n = 23) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-Up | p a | Change | Baseline | Follow-Up | p b | Change | p c | ||
| EndoPAT | SBP (mmHg) | 122.76 ± 14.77 d | 121.24 ± 13.17 | >0.99 | −1.53 | 122.72 ± 12.48 | 122.94 ± 16.41 | >0.99 | 0.22 | 0.667 |
| DBP (mmHg) | 80.65 ± 8.25 | 79.59 ± 7.59 | >0.99 | −1.47 | 82.11 ± 7.07 | 82.50 ± 9.40 | >0.99 | 0.67 | 0.421 | |
| BMI (kg/m2) | 29.73 ± 4.28 | 29.68 ± 4.31 | >0.99 | −0.09 | 27.81 ± 2.88 | 27.73 ± 3.08 | >0.99 | −0.07 | 0.981 | |
| LnRHI | 1 ± 0.2 | 0.75 ± 0.22 | >0.99 | −0.24 | 0.96 ± 0.68 | 0.68 ± 0.28 | >0.99 | −0.27 | 0.437 | |
| HR (bpm) | 65.53 ± 9.50 | 67.12 ± 7.83 | >0.99 | 1.76 | 69.61 ± 11.34 | 68.94 ± 6.83 | >0.99 | 0.39 | 0.923 | |
| AI% | 2.24 ± 8.12 | 5.53 ± 13.24 | >0.99 | 3.53 | 7.61 ± 10.01 | 4.89 ± 18.64 | >0.99 | −2.39 | 0.321 | |
| AI@75bpm (%) | 0.24 ± 12.26 | 2.24 ± 12.60 | >0.99 | 2.24 | 7.35 ± 14.12 | 7.18 ± 12.25 | >0.99 | 2.41 | 0.579 | |
| HRV (ms) | 29.85 ± 12.01 | 30.27 ± 10.92 | >0.99 | 0.41 | 33.57 ± 6.31 | 36.57 ± 13.19 | >0.99 | 2.99 | 0.420 | |
| LF (m/s2) | 224.05 ± 64.71 | 190.71 ± 74.23 | >0.99 | −33.33 | 185.10 ± 77.38 | 135.38 ± 55.18 | >0.99 | −49.71 | 0.132 | |
| HF (m/s2) | 88.70 ± 50.17 | 126.06 ± 59.64 | >0.99 | 37.36 | 123.21 ± 36.25 | 125.94 ± 74.14 | >0.99 | 2.72 | 0.570 | |
| LF/HF | 3.05 ± 1.34 | 1.82 ± 0.94 | 0.08 | −1.22 | 1.78 ± 1.51 | 1.27 ± 0.82 | >0.99 | −0.42 | 0.562 | |
| Complior | Peripheral BP | |||||||||
| SBP (mmHg) | 120.44 ± 15.37 | 124.07 ± 10.37 | >0.99 | 3.63 | 120.03 ± 11.87 | 120.9 ± 12.16 | >0.99 | 0.86 | 0.334 | |
| DBP (mmHg) | 78.6 ± 8.6 | 79.03 ± 5.77 | >0.99 | 0.37 | 80.72 ± 6.56 | 79.04 ± 8.51 | >0.99 | −1.67 | 0.724 | |
| MAP (mmHg) | 93.05 ± 9.88 | 94.24 ± 5.71 | >0.99 | 1.18 | 93.57 ± 7.25 | 92.7 ± 8.39 | >0.99 | −0.85 | 0.451 | |
| PP (mmHg) | 42.27 ± 10.38 | 45.23 ± 11.26 | >0.99 | 2.96 | 39.25 ± 10.39 | 41.80 ± 8.50 | >0.99 | 2.55 | 0.573 | |
| HR (bpm) | 63.17 ± 8.82 | 67.41 ± 9.84 | >0.99 | 4.24 | 70 ± 10.77 | 70.67 ± 8.94 | >0.99 | 0.67 | 0.985 | |
| Central BP | ||||||||||
| cSBP (mmHg) | 114.74 ± 17.74 | 116.08 ± 10.89 | >0.99 | 1.34 | 115.3 ± 14.56 | 110.67 ± 13.50 | >0.99 | −4.65 | 0.095 | |
| cDBP (mmHg) | 78.81 ± 8.91 | 79.23 ± 6.09 | >0.99 | 0.42 | 81 ± 7.06 | 80.1 ± 8.30 | >0.99 | −0.9 | 1.00 | |
| cPP (mmHg) | 36.42 ± 10.7 | 38.37 ± 10.23 | >0.99 | 1.94 | 34.45 ± 12.51 | 32.01 ± 9.53 | >0.99 | −2.43 | 0.123 | |
| PP amplification (mmHg) | 1.19 ± 0.23 | 1.22 ± 0.27 | >0.99 | 0.02 | 1.18 ± 0.21 | 1.35 ± 0.23 | >0.99 | 0.17 | 0.127 | |
| Pulse wave analysis | ||||||||||
| CF PWV (m/s) | 7.4 (6.2–8.5) e | 7.6 (2.4–8.5) | >0.99 | −1.19 | 7.1 (5.7–7.8) | 7.1 (6.5–8.4) | >0.99 | 0.23 | 0.123 | |
| Alx (%) | 13.9 (−13.8–18.9) | 8.2 (−17.8–15.7) | >0.99 | −6.87 | 9.2 (−26.9–25.3) | 13.1 (−7.6–25) | >0.99 | 9.07 | 0.339 | |
| AP (mmHg) | 9.6 (4.5–12.3) | 7.6 (4.8–14) | >0.99 | −0.46 | 7.5 (4.2–16.5) | 8 (3.2–15.7) | >0.99 | −1.8 | 0.585 | |
| SEVR (%) | 105.22 ± 46.60 | 99.05 ± 42.24 | >0.99 | −6.17 | 102.28 ± 50.23 | 109.62 ± 47.36 | >0.99 | 7.33 | 0.482 | |
| LVET (ms) | 415.51 ± 80.20 | 430.90 ± 121.32 | >0.99 | 15.38 | 406.62 ± 135.64 | 386.25 ± 86.80 | >0.99 | −20.37 | 0.227 | |
| Max dp/dt (mmHg/s) | 720 (499.9–940) | 896.6 (643.3–1021.6) | >0.99 | 110.42 | 584.1 (456.6–793.7) | 661.6 (343.3–822.5) | >0.99 | −76.85 | 0.055 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saadati, S.; Cameron, J.; Menon, K.; Hodge, A.; Lu, Z.X.; de Courten, M.; Feehan, J.; de Courten, B. Carnosine Did Not Affect Vascular and Metabolic Outcomes in Patients with Prediabetes and Type 2 Diabetes: A 14-Week Randomized Controlled Trial. Nutrients 2023, 15, 4835. https://doi.org/10.3390/nu15224835
Saadati S, Cameron J, Menon K, Hodge A, Lu ZX, de Courten M, Feehan J, de Courten B. Carnosine Did Not Affect Vascular and Metabolic Outcomes in Patients with Prediabetes and Type 2 Diabetes: A 14-Week Randomized Controlled Trial. Nutrients. 2023; 15(22):4835. https://doi.org/10.3390/nu15224835
Chicago/Turabian StyleSaadati, Saeede, James Cameron, Kirthi Menon, Alexander Hodge, Zhong X. Lu, Maximilian de Courten, Jack Feehan, and Barbora de Courten. 2023. "Carnosine Did Not Affect Vascular and Metabolic Outcomes in Patients with Prediabetes and Type 2 Diabetes: A 14-Week Randomized Controlled Trial" Nutrients 15, no. 22: 4835. https://doi.org/10.3390/nu15224835
APA StyleSaadati, S., Cameron, J., Menon, K., Hodge, A., Lu, Z. X., de Courten, M., Feehan, J., & de Courten, B. (2023). Carnosine Did Not Affect Vascular and Metabolic Outcomes in Patients with Prediabetes and Type 2 Diabetes: A 14-Week Randomized Controlled Trial. Nutrients, 15(22), 4835. https://doi.org/10.3390/nu15224835