Reproducibility and Relative Validity of a Short Food Frequency Questionnaire in 9–10 Year-Old Children
Abstract
:1. Introduction
2. Materials and Methods
2.1. FFQ Development
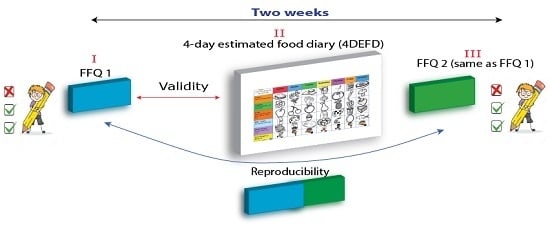
2.2. Data Collection
2.3. Validation Reference: 4DEFD
2.4. Anthropometric Measurements
2.5. Data Entry
2.6. Statistical Analysis
3. Results
3.1. Reproducibility: PEDALS FFQ One vs. PEDALS FFQ Two
3.2. Relative Validity: PEDALS FFQ vs. 4DEFD
4. Discussion
4.1. Reproducibility
4.2. Relative Validity
4.3. Strength and Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| FFQ | Food frequency questionnaire |
| PEDALS | Physical activity, Exercise, Diet And Lifestyle Study FFQ |
| 4DEFD | Four-day estimated food diary |
| SCC | Spearman’s correlation coefficients |
| ICC | Intraclass correlation coefficients |
| NZAFFQ | New Zealand Adolescent FFQ |
| CC% | Percentage correctly classified |
| GC% | Percentage grossly misclassified |
References
- Mikkilä, V.; Räsänen, L.; Laaksonen, M.M.L.; Juonala, M.; Viikari, J.; Pietinen, P.; Raitakari, O.T. Long-term dietary patterns and carotid artery intima media thickness: The Cardiovascular Risk in Young Finns Study. Br. J. Nutr. 2009, 102, 1507–1512. [Google Scholar] [CrossRef] [PubMed]
- Victora, C.G.; Adair, L.; Fall, C.; Hallal, P.C.; Martorell, R.; Richter, L.; Sachdev, H.S. Maternal and child undernutrition: Consequences for adult health and human capital. Lancet 2008, 371, 340–357. [Google Scholar] [CrossRef]
- Dietary Guidelines Advisory Committee. SCIENTIFIC Report of the 2015 Dietary Guidelines Advisory Committee. Available online: http://health.gov/dietaryguidelines/2015-scientific-report/ (accessed on 8 July 2015).
- Mikkilä, V.; Räsänen, L.; Raitakari, O.T.; Pietinen, P.; Viikari, J. Consistent dietary patterns identified from childhood to adulthood: The cardiovascular risk in Young Finns Study. Br. J. Nutr. 2005, 93, 923–931. [Google Scholar] [CrossRef] [PubMed]
- Northstone, K.; Emmett, P.M. Are dietary patterns stable throughout early and mid-childhood? A birth cohort study. Br. J. Nutr. 2008, 100, 1069–1076. [Google Scholar] [CrossRef] [PubMed]
- Hammond, J.; Nelson, M.; Chinn, S.; Rona, R.J. Validation of a food frequency questionnaire for assessing dietary intake in a study of coronary heart disease risk factors in children. Eur. J. Clin. Nutr. 1993, 47, 242–250. [Google Scholar] [PubMed]
- Cade, J.; Thompson, R.; Burley, V.; Warm, D. Development, validation and utilisation of food-frequency questionnaires—A review. Public Health Nutr. 2002, 5, 567–587. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.F.; Johansson, L.; Solvoll, K. Usefulness of a short food frequency questionnaire for screening of low intake of fruit and vegetable and for intake of fat. Eur. J. Public Health 2002, 12, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Willett, W. Reproducibility and validity of food-frequency questionnaires. In Nutritional Epidemiology; Larent, E., Willett, W., Eds.; Oxford University Press: Oxford, UK, 1998. [Google Scholar]
- Kobayashi, T.; Kamimura, M.; Imai, S.; Toji, C.; Okamoto, N.; Fukui, M.; Date, C. Reproducibility and validity of the food frequency questionnaire for estimating habitual dietary intake in children and adolescents. Nutr. J. 2011, 10, 27. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.F.; Nes, M.; Lillegaard, I.T.; Sandstad, B.; Bjørneboe, G.E.; Drevon, C.A. Evaluation of a quantitative food frequency questionnaire used in a group of Norwegian adolescents. Eur. J. Clin. Nutr. 1995, 49, 543–554. [Google Scholar] [PubMed]
- Rockett, H.R.; Breitenbach, M.; Frazier, A.L.; Witschi, J.; Wolf, A.M.; Field, A.E.; Colditz, G.A. Validation of a youth/adolescent food frequency questionnaire. Prev. Med. 1997, 26, 808–816. [Google Scholar] [CrossRef] [PubMed]
- Subar, A.F.; Thompson, F.E.; Kipnis, V.; Midthune, D.; Hurwitz, P.; McNutt, S.; McIntosh, A.; Rosenfeld, S. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: The Eating at America’s Table Study. Am. J. Epidemiol. 2001, 154, 1089–1099. [Google Scholar] [CrossRef] [PubMed]
- Schatzkin, A.; Kipnis, V.; Carroll, R.J.; Midthune, D.; Subar, A.F.; Bingham, S.; Schoeller, D.A.; Troiano, R.P.; Freedman, L.S. A comparison of a food frequency questionnaire with a 24-h recall for use in an epidemiological cohort study: Results from the biomarker-based Observing Protein and Energy Nutrition (OPEN) study. Int. J. Epidemiol. 2003, 32, 1054–1062. [Google Scholar] [CrossRef] [PubMed]
- Ambrosini, G.L.; O’Sullivan, T.A.; de Klerk, N.H.; Mori, T.A.; Beilin, L.J.; Oddy, W.H. Relative validity of adolescent dietary patterns: A comparison of a FFQ and 3 d food record. Br. J. Nutr. 2011, 105, 625–633. [Google Scholar] [CrossRef] [PubMed]
- Osler, M.; Heitmann, B.L. The validity of a short food frequency questionnaire and its ability to measure changes in food intake: A longitudinal study. Int. J. Epidemiol. 1996, 25, 1023–1029. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.E.; Watson, J.; Burrows, T. Measuring dietary intake in children and adolescents in the context of overweight and obesity. Int. J. Obes. 2010, 34, 1103–1115. [Google Scholar] [CrossRef] [PubMed]
- Burrows, T.L.; Truby, H.; Morgan, P.J.; Callister, R.; Davies, P.S.W.; Collins, C.E. A comparison and validation of child versus parent reporting of children’s energy intake using food frequency questionnaires versus food records: Who’S an accurate reporter? Clin. Nutr. Edinb. Scotl. 2013, 32, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, M.B.E.; Robson, P.J. Measurement of dietary intake in children. Proc. Nutr. Soc. 2000, 59, 279–293. [Google Scholar] [CrossRef] [PubMed]
- Flood, V.M.; Wen, L.M.; Hardy, L.L.; Rissel, C.; Simpson, J.M.; Baur, L.A. Reliability and validity of a short FFQ for assessing the dietary habits of 2–5-year-old children, Sydney, Australia. Public Health Nutr. 2014, 17, 498–509. [Google Scholar] [CrossRef] [PubMed]
- Lazarou, C.; Panagiotakos, D.B.; Kouta, C.; Matalas, A.L. Dietary and other lifestyle characteristics of Cypriot school children: Results from the nationwide CYKIDS study. BMC Public Health 2009, 9, 147. [Google Scholar] [CrossRef] [PubMed]
- Magarey, A.; Golley, R.; Spurrier, N.; Goodwin, E.; Ong, F. Reliability and validity of the Children’s Dietary Questionnaire; a new tool to measure children’s dietary patterns. Int. J. Pediatr. Obes. 2009, 4, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Kiwanuka, S.N.; Astrøm, A.N.; Trovik, T.A. Sugar snack consumption in Ugandan schoolchildren: Validity and reliability of a food frequency questionnaire. Community Dent. Oral Epidemiol. 2006, 34, 372–380. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.E.; Parnell, W.R.; Black, K.E.; Skidmore, P.M.L. Reliability and relative validity of a food frequency questionnaire to assess food group intakes in New Zealand adolescents. Nutr. J. 2012, 11, 65. [Google Scholar] [CrossRef] [PubMed]
- Bel-Serrat, S.; Mouratidou, T.; Pala, V.; Huybrechts, I.; Börnhorst, C.; Fernández-Alvira, J.M.; Hadjigeorgiou, C.; Eiben, G.; Hebestreit, A.; Lissner, L.; et al. Relative validity of the Children’s Eating Habits Questionnaire-food frequency section among young European children: The IDEFICS Study. Public Health Nutr. 2014, 17, 266–276. [Google Scholar] [CrossRef] [PubMed]
- De Keyzer, W.; Dekkers, A.; Van Vlaslaer, V.; Ottevaere, C.; Van Oyen, H.; De Henauw, S.; Huybrechts, I. Relative validity of a short qualitative food frequency questionnaire for use in food consumption surveys. Eur. J. Public Health 2013, 23, 737–742. [Google Scholar] [CrossRef] [PubMed]
- Lillegaard, I.T.; Overby, N.C.; Andersen, L.F. Evaluation of a short food frequency questionnaire used among Norwegian children. Food Nutr. Res. 2012, 56, 6399. [Google Scholar] [Green Version]
- Vereecken, C.A.; Rossi, S.; Giacchi, M.V.; Maes, L. Comparison of a short food-frequency questionnaire and derived indices with a seven-day diet record in Belgian and Italian children. Int. J. Public Health 2008, 53, 297–305. [Google Scholar] [CrossRef] [PubMed]
- Raitakari, O.T.; Juonala, M.; Kähönen, M.; Taittonen, L.; Laitinen, T.; Mäki-Torkko, N.; Järvisalo, M.J.; Uhari, M.; Jokinen, E.; Rönnemaa, T.; et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: The Cardiovascular Risk in Young Finns Study. JAMA 2003, 290, 2277–2283. [Google Scholar] [CrossRef] [PubMed]
- Saland, J.M. Update on the metabolic syndrome in children. Curr. Opin. Pediatr. 2007, 19, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. NZ Food NZ Children: Key Results of the 2002 National Children’s Nutrition Survey; Ministry of Health: Wellington, New Zealand, 2003.
- Willett, W. Reproducibility and validity of food frequency questionnaires. In Nutritional Epidemiology; Willett, W., Lenart, E., Eds.; Oxford University Press: Oxford, UK, 2013; pp. 96–141. [Google Scholar]
- Burrows, T.L.; Martin, R.J.; Collins, C.E. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labeled water. J. Am. Diet. Assoc. 2010, 110, 1501–1510. [Google Scholar] [CrossRef] [PubMed]
- Baranowski, T.; Dworkin, R.; Henske, J.C.; Clearman, D.R.; Dunn, J.K.; Nader, P.R.; Hooks, P.C. The accuracy of children’s self-reports of diet: Family Health Project. J. Am. Diet. Assoc. 1986, 86, 1381–1385. [Google Scholar] [PubMed]
- Baranowski, T.; Domel, S.B. A cognitive model of children’s reporting of food intake. Am. J. Clin. Nutr. 1994, 59, 212S–217S. [Google Scholar] [PubMed]
- Frank, G.C. Taking a bite out of eating behavior: Food records and food recalls of children. J. Sch. Health 1991, 61, 198–200. [Google Scholar] [CrossRef] [PubMed]
- Department of Human Nutrition. Diet Assessment Photos; University of Otago: Dunedin, New Zealand, 2000. [Google Scholar]
- Cole, T.J.; Flegal, K.M.; Nicholls, D.; Jackson, A.A. Body mass index cut offs to define thinness in children and adolescents: International survey. BMJ 2007, 335, 194. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef] [PubMed]
- Kuczmarski, R.J.; Ogden, C.L.; Grummer-Strawn, L.M.; Flegal, K.M.; Guo, S.S.; Wei, R.; Mei, L.R.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. CDC growth charts: United States. Adv. Data 2000, 314, 1–27. [Google Scholar] [PubMed]
- Engle, A.; Lynn, L.L.; Koury, K.; Boyar, A.P. Reproducibility and comparability of a computerized, self-administered food frequency questionnaire. Nutr. Cancer 1990, 13, 281–292. [Google Scholar] [CrossRef] [PubMed]
- Øverby, N.C.; Johannesen, E.; Jensen, G.; Skjaevesland, A.K.; Haugen, M. Test-retest reliability and validity of a web-based food-frequency questionnaire for adolescents aged 13–14 to be used in the Norwegian Mother and Child Cohort Study (MoBa). Food Nutr. Res. 2014, 58, 23956. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cade, J.E.; Burley, V.J.; Warm, D.L.; Thompson, R.L.; Margetts, B.M. Food-frequency questionnaires: A review of their design, validation and utilisation. Nutr. Res. Rev. 2004, 17, 5–22. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Cicchetti, D.V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. Assess. 1994, 6, 284–290. [Google Scholar] [CrossRef]
- Wilson, J.H. Essential Statistics; Pearson/Prentice Hall: New Jersey, NJ, USA, 2004; pp. 201–223. [Google Scholar]
- Andersen, L.F.; Bere, E.; Kolbjornsen, N.; Klepp, K.I. Validity and reproducibility of self-reported intake of fruit and vegetable among 6th graders. Eur. J. Clin. Nutr. 2004, 58, 771–777. [Google Scholar] [CrossRef] [PubMed]
- Vereecken, C.A.; Maes, L. A Belgian study on the reliability and relative validity of the Health Behaviour in School-Aged Children food-frequency questionnaire. Public Health Nutr. 2003, 6, 581–588. [Google Scholar] [CrossRef] [PubMed]
- Rockell, J.E.; Skidmore, P.M.L.; Parnell, W.R.; Wilson, N. What children eat during afternoons and evenings: Is it important? Public Health Nutr. 2011, 14, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Metcalf, P.A.; Scragg, R.K.R.; Sharpe, S.; Fitzgerald, E.D.H.; Schaaf, D.; Watts, C. Short-term repeatability of a food frequency questionnaire in New Zealand children aged 1–14 years. Eur. J. Clin. Nutr. 2003, 57, 1498–1503. [Google Scholar] [CrossRef] [PubMed]
- Del Pino, D.L.; Friedman, R. Adaptation and validation of an FFQ for 6–10-year-old children. Public Health Nutr. 2011, 14, 826–834. [Google Scholar] [CrossRef] [PubMed]
- Matos, S.M.A.; Prado, M.S.; Santos, C.A.S.T.; D’Innocenzo, S.; Assis, A.M.O.; Dourado, L.S.; Oliveira, N.S.; Rodrigues, L.C.; Barreto, M.L. Validation of a food frequency questionnaire for children and adolescents aged 4 to 11 years living in Salvador, Bahia. Nutr. Hosp. 2012, 27, 1114–1119. [Google Scholar] [PubMed]
- Pampaloni, B.; Bartolini, E.; Barbieri, M.; Piscitelli, P.; Di Tanna, G.L.; Giolli, L.; Brandi, M.L. Validation of a food-frequency questionnaire for the assessment of calcium intake in schoolchildren aged 9–10 years. Calcif. Tissue Int. 2013, 93, 23–38. [Google Scholar] [CrossRef] [PubMed]
- Scagliusi, F.B.; Garcia, M.T.; Indiani, A.L.C.; Cardoso, M.A. Relative validity of a food-frequency questionnaire developed to assess food intake of schoolchildren living in the Brazilian Western Amazon. Cad. Saúde Pública 2011, 27, 2197–2206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, A.M.R.; Lewis, R.D. Disagreement of energy and macronutrient intakes estimated from a food frequency questionnaire and 3-day diet record in girls 4 to 9 years of age. J. Am. Diet. Assoc. 2004, 104, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Haftenberger, M.; Heuer, T.; Heidemann, C.; Kube, F.; Krems, C.; Mensink, G.B.M. Relative validation of a food frequency questionnaire for national health and nutrition monitoring. Nutr. J. 2010, 9, 36. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, G.; Sjoberg, A.; Lissner, L.; Moreno, L.A. Food patterns and nutrient intake in relation to childhood obesity. In Epidemiology of Obesity in Children and Adolescents; Moreno, L.A., Pigeto, I., Ahrens, W., Eds.; Springer: New York, NY, USA, 2011. [Google Scholar]
- Thompson, F.; Subar, A. Dietary assessment methodology. In Nutrition in the Prevention and Treatment of Disease, 3rd ed.; Coulston, A., Boushey, C., Ferruzzi, M.G., Eds.; Elsevier Academic Press: San Diego, CA, USA, 2008; pp. 3–39. [Google Scholar]
- Quigley, R.; Taylor, R.; Scragg, R. Is Consuming Breakfast Important for Academic Performance, Maintaining A Healthy Body Weight, and Improving Nutrient Intake and Lifestyle Habits in Children; The Scientific Committee of the Agencies for Nutrition Action: Wellington, New Zealand, 2007. [Google Scholar]
- Block, G.; Thompson, F.E.; Hartman, A.M.; Larkin, F.A.; Guire, K.E. Comparison of two dietary questionnaires validated against multiple dietary records collected during a 1-year period. J. Am. Diet. Assoc. 1992, 92, 686–693. [Google Scholar] [PubMed]
- Araujo, M.C.; Yokoo, E.M.; Pereira, R.A. Validation and calibration of a semiquantitative food frequency questionnaire designed for adolescents. J. Am. Diet. Assoc. 2010, 110, 1170–1177. [Google Scholar] [CrossRef] [PubMed]
- Truthmann, J.; Mensink, G.B.M.; Richter, A. Relative validation of the KiGGS Food Frequency Questionnaire among adolescents in Germany. Nutr. J. 2011, 10, 133. [Google Scholar] [CrossRef] [PubMed]
- Kolodziejczyk, J.K.; Merchant, G.; Norman, G.J. Reliability and validity of child/adolescent food frequency questionnaires that assess foods and/or food groups. J. Pediatr. Gastroenterol. Nutr. 2012, 55, 4–13. [Google Scholar] [CrossRef] [PubMed]
| Food Items/Groups List in the PEDALS FFQ after Aggregation (23 Items) | N $ | Complete List of Food Items/Groups List in the PEDALS FFQ before Aggregation (28 Items) | |
|---|---|---|---|
| 1 | Fruits | 1 | Fruits |
| 2 | Vegetables | 2 | Vegetables (excluding potato) |
| 2 | Potato (such as mashed, boiled) | ||
| 3 | Trim milk (green) (including on cereals, milo, hot chocolate) # | 3 | Trim milk (green) (including on cereals, milo, hot chocolate) |
| 4 | Standard milk (blue) (including on cereals, milo, hot chocolate) * | 4 | Standard milk (blue) (including on cereals, milo, hot chocolate) |
| 5 | Cheese | 5 | Cheese |
| 6 | Yoghurt | 6 | Yoghurt |
| 7 | Ice-cream | 7 | Ice-cream |
| 8 | Processed meat (such as meat pies, sausage, sausage roll, salami, luncheon, bacon, ham) | 8 | Processed meat (such as meat pies, sausage, sausage roll, salami, luncheon, bacon, ham) |
| 9 | Other meats (such as mince, beef, chicken) | 9 | Other meats (such as mince, beef, chicken) |
| 10 | Fish (including canned tuna or salmon, fish cakes, fish fingers, fish pie, battered fish) | 10 | Fish (including canned tuna or salmon, fish cakes, fish fingers, fish pie, battered fish) |
| 11 | Non-dairy drinks | 11 | Fruit juice (such as orange juice, apple juice, Raro, Refresh, Keri, Twist, Ribena) |
| 11 | Diet fizzy drinks (such as Diet Coke, Pepsi Max, Sprite Zero and any other light or sugar free varieties) | ||
| 11 | Fizzy drinks (such as Coke, Pepsi, Sprite, L&P, Fanta, Ginger Beer) | ||
| 12 | Breakfast cereals | 12 | Breakfast cereals |
| 13 | White bread | 13 | White bread |
| 14 | Brown/wholemeal bread | 14 | Brown/wholemeal bread |
| 15 | Rice, rice based dishes | 15 | Rice, rice based dishes |
| 16 | Pasta (such as spaghetti, macaroni), noodles | 16 | Pasta (such as spaghetti, macaroni), noodles |
| 17 | Salty snacks | 17 | Potato chips, potato snacks, corn chips |
| 17 | Hot chips, wedges, French fries | ||
| 18 | Biscuits, cakes, muffins, doughnuts, fruit pies | 18 | Biscuits, cakes, muffins, doughnuts, fruit pies |
| 19 | Lollies $$ | 19 | Lollies |
| 20 | Sweet snacks | 20 | Snack bars (such as muesli bar, fruit bar, rice bubble bar) |
| 20 | Chocolate, chocolate bars | ||
| 21 | Tomato sauce, ketchup | 21 | Tomato sauce, ketchup |
| 22 | Peanut butter, Nutella | 22 | Peanut butter, Nutella |
| 23 | Jam, honey | 23 | Jam, honey |
| Food Group | SCC | ICC | CC% | GM% | SCC (NZAFFQ) | ICC (NZAFFQ) |
|---|---|---|---|---|---|---|
| Fruits | 0.66 | 0.63 | 58 | 8 | 0.57 | 0.83 |
| Vegetables † | 0.66 | 0.60 | 60 | 2 | 0.42 | - |
| Trim milk (green) | 0.70 | 0.54 | 70 | 6 | 0.87 | 0.79 |
| Standard milk (blue) | 0.57 | 0.43 | 70 | 6 | 0.83 | 0.78 |
| Cheese | 0.57 | 0.40 | 60 | 10 | 0.67 | 0.58 |
| Yogurt | 0.74 | 0.48 | 64 | 2 | 0.79 | 0.84 |
| Ice cream | 0.61 | 0.64 | 68 | 12 | 0.64 | 0.79 |
| Processed meat | 0.40 | 0.38 | 52 | 14 | - | - |
| Other meats | 0.48 | 0.43 | 44 | 12 | - | - |
| Fish | 0.67 | 0.43 | 62 | 8 | 0.76 | 0.67 |
| Non-dairy drinks †† | 0.82 | 0.75 | 80 | 0 | - | - |
| Breakfast cereals | 0.75 | 0.72 | 82 | 2 | 0.78 | 0.74 |
| White bread | 0.77 | 0.78 | 72 | 4 | 0.78 | 0.64 |
| Brown/wholemeal bread | 0.58 | 0.48 | 56 | 8 | 0.80 | 0.72 |
| Rice, rice based dishes | 0.70 | 0.73 | 68 | 6 | - | - |
| Pasta (such as spaghetti, macaroni), noodles | 0.45 | 0.44 | 48 | 10 | - | - |
| Salty snacks ‡ | 0.74 | 0.73 | 66 | 0 | - | - |
| Biscuits, cakes, muffins, doughnuts, fruit pies | 0.59 | 0.38 | 56 | 8 | 0.65 | 0.62 |
| Lollies | 0.82 | 0.75 | 72 | 0 | - | - |
| Sweet snacks § | 0.63 | 0.35 | 70 | 10 | - | - |
| Tomato sauce, ketchup | 0.65 | 0.41 | 60 | 4 | - | - |
| Peanut butter, Nutella | 0.75 | 0.70 | 66 | 2 | 0.79 | 0.73 |
| Jam, honey | 0.77 | 0.72 | 64 | 2 | - | - |
| Food Group | SCC | CC% (PEDALS FFQ One) | GM% | SCC (NZAFFQ) |
|---|---|---|---|---|
| Fruits | 0.28 | 38 | 16 | 0.34 |
| Vegetables † | 0.31 | 44 | 16 | 0.37 |
| Trim milk (green) | 0.45 | 60 ¶ | 40 ¶ | 0.59 |
| Standard milk (blue) | 0.50 | 44 | 6 | 0.70 |
| Cheese | 0.34 | 42 | 10 | 0.40 |
| Yogurt | 0.46 | 48 | 10 | 0.46 |
| Ice cream | 0.30 | 44 | 14 | 0.42 |
| Processed meat | 0.36 | 42 | 14 | - |
| Other meats | 0.13 | 48 | 18 | - |
| Fish | 0.14 | 52 ¶ | 48 ¶ | 0.34 |
| Non-dairy drinks †† | 0.39 | 48 | 14 | - |
| Breakfast cereals | 0.47 | 54 | 10 | 0.67 |
| White bread | 0.42 | 48 | 10 | 0.40 |
| Brown/wholemeal bread | 0.41 | 46 | 6 | 0.36 |
| Rice, rice based dishes | 0.38 | 44 | 10 | - |
| Pasta (such as spaghetti, macaroni), noodle | 0.07 | 34 | 26 | - |
| Salty snacks ‡ | 0.31 | 42 | 14 | - |
| Biscuits, cakes, muffins, doughnuts, fruit pies | 0.26 | 44 | 16 | 0.56 |
| Lollies | 0.25 | 38 | 14 | - |
| Sweet snacks § | 0.40 | 50 | 14 | - |
| Tomato sauce, ketchup | −0.11 | 24 ¶ | 76 ¶ | - |
| Peanut butter, Nutella | 0.58 | 70 ¶ | 30 ¶ | 0.37 |
| Jam, honey | 0.37 | 52 | 14 | - |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saeedi, P.; Skeaff, S.A.; Wong, J.E.; Skidmore, P.M.L. Reproducibility and Relative Validity of a Short Food Frequency Questionnaire in 9–10 Year-Old Children. Nutrients 2016, 8, 271. https://doi.org/10.3390/nu8050271
Saeedi P, Skeaff SA, Wong JE, Skidmore PML. Reproducibility and Relative Validity of a Short Food Frequency Questionnaire in 9–10 Year-Old Children. Nutrients. 2016; 8(5):271. https://doi.org/10.3390/nu8050271
Chicago/Turabian StyleSaeedi, Pouya, Sheila A. Skeaff, Jyh Eiin Wong, and Paula M. L. Skidmore. 2016. "Reproducibility and Relative Validity of a Short Food Frequency Questionnaire in 9–10 Year-Old Children" Nutrients 8, no. 5: 271. https://doi.org/10.3390/nu8050271
APA StyleSaeedi, P., Skeaff, S. A., Wong, J. E., & Skidmore, P. M. L. (2016). Reproducibility and Relative Validity of a Short Food Frequency Questionnaire in 9–10 Year-Old Children. Nutrients, 8(5), 271. https://doi.org/10.3390/nu8050271