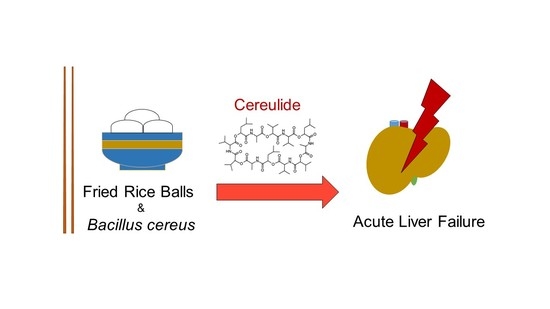
Acute Liver Failure after Ingestion of Fried Rice Balls: A Case Series of Bacillus cereus Food Poisonings
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Population and Study Design
4.2. Laboratory and Toxicological Analyses
4.3. Statistical Analyses
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Messelhäußer, U.; Ehling-Schulz, M. Bacillus cereus—A multifaceted opportunistic pathogen. Curr. Clin. Microbiol. Rep. 2018, 5, 120–125. [Google Scholar] [CrossRef] [Green Version]
- Ehling-Schulz, M.; Lereclus, D.; Koehler, T.M. The Bacillus cereus group: Bacillus species with pathogenic potential. Microbiol. Spectr. 2019, 7, 875–902. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, R.; Jessberger, N.; Ehling-Schulz, M.; Märtlbauer, E.; Granum, P.E. The food poisoning toxins of Bacillus cereus. Toxins 2021, 13, 98. [Google Scholar] [CrossRef]
- Rouzeau-Szynalski, K.; Stollewerk, K.; Messelhäusser, U.; Ehling-Schulz, M. Why be serious about emetic Bacillus cereus: Cereulide production and industrial challenges. Food Microbiol. 2020, 85, 103279. [Google Scholar] [CrossRef]
- Mahler, H.; Pasi, A.; Kramer, J.M.; Schulte, P.; Scoging, A.C.; Bär, W.; Krähenbühl, S. Fulminant liver failure in association with the emetic toxin of Bacillus cereus. N. Engl. J. Med. 1997, 336, 1142–1148. [Google Scholar] [CrossRef]
- Naranjo, M.; Denayer, S.; Botteldoorn, N.; Delbrassinne, L.; Veys, J.; Waegenaere, J.; Sirtaine, N.; Driesen, R.B.; Sipido, K.R.; Mahillon, J.; et al. Sudden death of a young adult associated with Bacillus cereus food poisoning. J. Clin. Microbiol. 2011, 49, 4379–4381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shiota, M.; Saitou, K.; Mizumoto, H.; Matsusaka, M.; Agata, N.; Nakayama, M.; Kage, M.; Tatsumi, S.; Okamoto, A.; Yamaguchi, S.; et al. Rapid detoxification of cereulide in Bacillus cereus food poisoning. Pediatrics 2010, 125, e951–e955. [Google Scholar] [CrossRef]
- Pósfay-Barbe, K.M.; Schrenzel, J.; Frey, J.; Studer, R.; Korff, C.; Belli, D.C.; Parvex, P.; Rimensberger, P.C.; Schäppi, M.G. Food poisoning as a cause of acute liver failure. Pediatr. Infect. Dis. J. 2008, 27, 846–847. [Google Scholar] [CrossRef] [PubMed]
- Tschiedel, E.; Rath, P.M.; Steinmann, J.; Becker, H.; Dietrich, R.; Paul, A.; Felderhoff-Müser, U.; Dohna-Schwake, C. Lifesaving liver transplantation for multi-organ failure caused by Bacillus cereus food poisoning. Pediatr. Transplant. 2015, 19, E11–E14. [Google Scholar] [CrossRef]
- Saleh, M.; Al Nakib, M.; Doloy, A.; Jacqmin, S.; Ghiglione, S.; Verroust, N.; Poyart, C.; Ozier, Y. Bacillus cereus, an unusual cause of fulminant liver failure: Diagnosis may prevent liver transplantation. J. Med. Microbiol. 2012, 61, 743–745. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ichikawa, K.; Gakumazawa, M.; Inaba, A.; Shiga, K.; Takeshita, S.; Mori, M.; Kikuchi, N. Acute encephalopathy of Bacillus cereus mimicking Reye syndrome. Brain Dev. 2010, 32, 688–690. [Google Scholar] [CrossRef]
- Dierick, K.; Van Coillie, E.; Swiecicka, I.; Meyfroidt, G.; Devlieger, H.; Meulemans, A.; Hoedemaekers, G.; Fourie, L.; Heyndrickx, M.; Mahillon, J. Fatal family outbreak of Bacillus cereus-associated food poisoning. J. Clin. Microbiol. 2005, 43, 4277–4279. [Google Scholar] [CrossRef] [Green Version]
- Colaco, C.M.G.; Basile, K.; Draper, J.; Ferguson, P.E. Fulminant Bacillus cereus food poisoning with fatal multi-organ failure. BMJ Case Rep. 2021, 14, e238716. [Google Scholar] [CrossRef]
- Ehling-Schulz, M.; Guinebretiere, M.H.; Monthán, A.; Berge, O.; Fricker, M.; Svensson, B. Toxin gene profiling of enterotoxic and emetic Bacillus cereus. FEMS Microbiol. Lett. 2006, 260, 232–240. [Google Scholar] [CrossRef] [Green Version]
- Ehling-Schulz, M.; Svensson, B.; Guinebretiere, M.H.; Lindbäck, T.; Andersson, M.; Schulz, A.; Fricker, M.; Christiansson, A.; Granum, P.E.; Märtlbauer, E.; et al. Emetic toxin formation of Bacillus cereus is restricted to a single evolutionary lineage of closely related strains. Microbiology 2005, 151, 183–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bauer, T.; Sipos, W.; Stark, T.D.; Käser, T.; Knecht, C.; Brunthaler, R.; Saalmüller, A.; Hofmann, T.; Ehling-Schulz, M. First Insights into within Host Translocation of the Bacillus cereus Toxin Cereulide Using a Porcine Model. Front. Microbiol. 2018, 9, 2652. [Google Scholar] [CrossRef] [Green Version]
- Messelhäusser, U.; Frenzel, E.; Blöchinger, C.; Zucker, R.; Kämpf, P.; Ehling-Schulz, M. Emetic Bacillus cereus are more volatile than thought: Recent foodborne outbreaks and prevalence studies in Bavaria (2007–2013). Biomed. Res. Int. 2014, 2014, 465603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marxen, S.; Stark, T.D.; Rütschle, A.; Lücking, G.; Frenzel, E.; Scherer, S.; Ehling-Schulz, M.; Hofmann, T. Multiparametric Quantitation of the Bacillus cereus Toxins Cereulide and Isocereulides A–G in Foods. J. Agric. Food Chem. 2015, 63, 8307–8313. [Google Scholar] [CrossRef]
- Yamaguchi, M.; Kawai, T.; Kitagawa, M.; Kumeda, Y. A new method for rapid and quantitative detection of the Bacillus cereus emetic toxin cereulide in food products by liquid chromatography-tandem mass spectrometry analysis. Food Microbiol. 2013, 34, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Reuben, A.; Koch, D.G.; Lee, W.M.; Acute Liver Failure Study Group. Drug-induced acute liver failure: Results of a U.S. multicenter, prospective study. Hepatology 2010, 52, 2065–2076. [Google Scholar] [CrossRef] [Green Version]
- Decleer, M.; Jovanovic, J.; Vakula, A.; Udovicki, B.; Agoua, R.E.K.; Madder, A.; De Saeger, S.; Rajkovic, A. Oxygen Consumption Rate Analysis of Mitochondrial Dysfunction Caused by Bacillus cereus Cereulide in Caco-2 and HepG2 Cells. Toxins 2018, 10, 266. [Google Scholar] [CrossRef] [Green Version]
- Beaumier, M.; Rioult, J.P.; Georges, M.; Brocheriou, I.; Lobbedez, T.; Lanot, A. Mushroom Poisoning Presenting with Acute Kidney Injury and Elevated Transaminases. Kidney Int. Rep. 2019, 4, 877–881. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stollings, J.L.; Wheeler, A.P.; Rice, T.W. Incidence and characterization of acute kidney injury after acetaminophen overdose. J. Crit. Care 2016, 35, 191–194. [Google Scholar] [CrossRef]
- Li, D.; Lin, R.; Xu, Y.; Chen, Q.; Deng, F.; Deng, Y.; Wen, J. Cereulide Exposure Caused Cytopathogenic Damages of Liver and Kidney in Mice. Int. J. Mol. Sci. 2021, 22, 9148. [Google Scholar] [CrossRef]
- Stravitz, R.T.; Kramer, A.H.; Davern, T.; Shaikh, A.O.; Caldwell, S.H.; Mehta, R.L.; Blei, A.T.; Fontana, R.J.; McGuire, B.M.; Rossaro, L.; et al. Acute Liver Failure Study Group. Intensive care of patients with acute liver failure: Recommendations of the U.S. Acute Liver Failure Study Group. Crit. Care Med. 2007, 35, 2498–2508. [Google Scholar] [CrossRef] [Green Version]
- Lee, W.M.; Squires, R.H., Jr.; Nyberg, S.L.; Doo, E.; Hoofnagle, J.H. Acute liver failure: Summary of a workshop. Hepatology 2008, 47, 1401–1415. [Google Scholar] [CrossRef] [Green Version]
- Mossel, D.A.; Koopman, M.J.; Jongerius, E. Enumeration of Bacillus cereus in foods. Appl. Microbiol. 1967, 15, 650–653. [Google Scholar] [CrossRef]
- Ehling-Schulz, M.; Fricker, M.; Scherer, S. Identification of emetic toxin producing Bacillus cereus strains by a novel molecular assay. FEMS Microbiol. Lett. 2004, 232, 189–195. [Google Scholar] [CrossRef] [Green Version]
- Guinebretiere, M.H.; Fagerlund, A.; Granum, P.E.; Nguyen-The, C. Rapid discrimination of cytK-1 and cytK-2 genes in Bacillus cereus strains by a novel duplex PCR system. FEMS Microbiol. Lett. 2006, 259, 74–80. [Google Scholar] [CrossRef] [Green Version]
- Anastassiades, M.; Lehotay, S.J.; Stajnbaher, D.; Schenck, F.J. Fast and easy multiresidue method employing acetonitrile extraction/partitioning and dispersive solid-phase extraction for the determination of pesticide residues in produce. J. AOAC Int. 2003, 86, 412–431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bauer, T.; Stark, T.; Hofmann, T.; Ehling-Schulz, M. Development of a stable isotope dilution analysis for the quantification of the Bacillus cereus toxin cereulide in foods. J. Agric. Food Chem. 2010, 58, 1420–1428. [Google Scholar] [CrossRef] [PubMed]
- Marxen, S.; Stark, T.D.; Frenzel, E.; Rütschle, A.; Lücking, G.; Pürstinger, G.; Pohl, E.E.; Scherer, S.; Ehling-Schulz, M.; Hofmann, T. Chemodiversity of cereulide, the emetic toxin of Bacillus cereus. Anal. Bioanal. Chem. 2015, 407, 2439–2453. [Google Scholar] [CrossRef] [PubMed]


| Time after Ingestion | 8 h | 13 h | 22 h | 29 h | 36 h | 41 h | 58 h | 82 h | Normal Range |
|---|---|---|---|---|---|---|---|---|---|
| Leucocytes [G/L] | 18.3 | 19.4 | 16.3 | 15.5 | 13.4 | 12.6 | 9.1 | 5.1 | 3.9–10.4 |
| Erythrocytes [T/L] | 6.1 | 5.5 | 5.0 | 4.9 | 4.7 | 5.0 | 5.0 | 4.1 | 4.0–5.2 |
| Haemoglobin [g/dL] | 18.6 | 16.5 | 15.0 | 14.8 | 14.3 | 15.2 | 14.9 | 12.6 | 11.6–15.5 |
| Haematocrit [%] | 53 | 48 | 43 | 43 | 42 | 44 | 44 | 37 | 35–45 |
| Platelets [G/L] | 310 | 321 | 274 | 249 | 219 | 205 | 174 | 111 | 140–440 |
| CRP [mg/L] | 5 | 9 | 47 | 65 | 75 | 86 | 75 | 54 | <5.0 |
| Procalcitonin [ng/mL] | n.d. | 1.4 | 2.2 | 2.2 | 2.0 | 1.8 | 1.5 | 1.2 | <0.5 |
| Sodium [mmol/L] | 143 | 142 | 136 | 136 | 137 | 137 | 141 | 140 | 135–145 |
| Potassium [mmol/L] | 4.5 | 4.6 | 4.7 | 4.6 | 4.4 | 4.2 | 3.8 | 4.0 | 3.5–5.0 |
| Chloride [mmol/L] | 103 | 101 | 99 | 99 | 99 | 97 | 99 | 101 | 98–107 |
| Calcium [mmol/L] | 2.3 | 2.3 | 2.1 | 2.2 | 2.1 | 2.2 | 2.2 | 2.2 | 2.2–2.7 |
| Creatinine [mg/dL] | 1.3 | 1.2 | 1.1 | 1.2 | 1.3 | 1.4 | 1.3 | 1.3 | 0.5–0.9 |
| Urea [mg/dL] | 38 | 38 | 35 | 33 | 33 | 36 | 45 | 56 | 10–39 |
| Bilirubin [mg/dL] | 1.1 | 1.5 | 1.8 | 2.3 | 2.7 | 3.1 | 3.2 | 3.6 | 0.1–1.2 |
| AP [U/L] | 90 | 95 | 93 | 95 | 99 | 105 | 106 | 76 | 35–105 |
| GGT [U/L] | 21 | 29 | 26 | 32 | 41 | 52 | 62 | 56 | <40 |
| CHE [U/L] | 13,615 | 7416 | 5900 | 5527 | 5249 | 5410 | 5027 | 3637 | >4600 |
| AST [U/L] | 61 | 540 | 9014 | 11,578 | 9973 | 8494 | 3660 | 1081 | <35 |
| ALT [U/L] | 59 | 542 | 7856 | 8959 | 7785 | 7462 | 5361 | 2763 | <35 |
| Ammonia [μmol/L] | n.d. | n.d. | 119 | 116 | 104 | 104 | 129 | 132 | <50 |
| CK [U/L] | 161 | 163 | 526 | 1180 | 1799 | 2186 | 1951 | 1444 | <170 |
| LDH [U/L] | 311 | 619 | 7453 | 8112 | 6239 | 5063 | 2328 | 711 | <250 |
| Prothrombin time [%] | 34 | 30 | 19 | 17 | 16 | 17 | 22 | 38 | 70–130 |
| PT INR | 2.2 | 2.4 | 3.7 | 4.1 | 4.3 | 4.1 | 3.2 | 2.0 | |
| aPTT [sec] | 41 | 39 | 52 | 55 | 56 | 56 | 52 | 48 | 27–35 |
| Fibrinogen [mg/dL] | 191 | 214 | 153 | 138 | 136 | 128 | 124 | 139 | 180–400 |
| Antithrombin III [%] | 92 | 78 | 60 | 58 | 53 | 47 | 42 | 40 | 80–13 |
| Factor V [%] | n.d. | 12 | 9 | 8 | 8 | 9 | 15 | 35 | >70 |
| Albumin [g/dL] | 4.5 | 4.5 | 3.6 | 3.5 | 3.3 | 3.3 | 3.3 | 3.6 | 3.5–5.3 |
| Lactate [mmol/L] | n.d. | 9.9 | 5.0 | 5.4 | 5.8 | 5.8 | 2.7 | 1.9 | 0.5–2.2 |
| Time after Ingestion | 8 h (n = 4) | 19 h (n = 4) | 25 h (n = 4) | 37 h (n = 4) | 61 h (n = 3) | Normal Range |
|---|---|---|---|---|---|---|
| Leucocytes [G/L] | 21.9 ± 1.8 | 13.5 ± 0.9 | 10.6 ± 0.5 | 7.2 ± 0.7 | 4.7 ± 0.1 | 3.9–10.4 |
| Erythrocytes [T/L] | 4.7 ± 0.2 | 4.4 ± 0.2 | 4.1 ± 0.1 | 4.0 ± 0.1 | 4.1 ± 0.1 | 4.0–5.2 |
| Haemoglobin [g/dL] | 14.0 ± 0.4 | 13.3 ± 0.2 | 12.6 ± 0.2 | 12.3 ± 0.3 | 12.1 ± 0.1 | 11.6–15.5 |
| Haematocrit [%] | 41.6 ± 1.1 | 39.0 ± 0.5 | 36.7 ± 0.6 | 36.2 ± 0.8 | 36.0 ± 0.2 | 35–45 |
| Platelets [G/L] | 302 ± 50 | 294 ± 44 | 253 ± 37 | 228 ± 36 | 226 ± 29 | 140–440 |
| CRP [mg/L] | 1.7 ± 1.1 | 15.7 ± 2.3 | 25.8 ± 4.4 | 47.5 ± 12.7 | 30.2 ± 8.5 | <5.0 |
| Sodium [mmol/L] | 137 ± 1 | 136 ± 1 | 137 ± 1 | 137 ± 1 | 140 ± 1 | 135–145 |
| Potassium [mmol/L] | 3.7 ± 0.2 | 3.8 ± 0.1 | 3.7 ± 0.1 | 3.8 ± 0.1 | 4.0 ± 0.1 | 3.5–5.0 |
| Chloride [mmol/L] | 103 ± 1 | 103 ± 1 | 104 ± 1 | 103 ± 1 | 106 ± 1 | 98–107 |
| Calcium [mmol/L] | 2.2 ± 0.1 | 2.1 ± 0.1 | 2.1 ± 0.1 | 2.1 ± 0.1 | 2.1 ± 0.1 | 2.2–2.7 |
| Creatinine [mg/dL] | 0.8 ± 0.1 | 1.1 ± 0.3 | 0.8 ± 0.1 | 0.8 ± 0.1 | 0.7 ± 0.1 | 0.5–0.9 |
| Urea [mg/dL] | 35 ± 4 | 41 ± 7 | 30 ± 3 | 27 ± 3 | 18 ± 3 | 10–39 |
| Bilirubin [mg/dL] | n.d. | 0.7 ± 0.1 | 1.1 ± 0.3 | 0.9 ± 0.4 | 0.4 ± 0.1 | 0.1–1.2 |
| AP [U/L] | 68 ± 2 | 59 ± 2 | 65 ± 1 | 59 ± 3 | 55 ± 5 | 35–105 |
| GGT [U/L] | 18 ± 1 | 15 ± 1 | 15 ± 1 | 14 ± 1 | 16 ± 1 | <40 |
| AST [U/L] | 37 ± 5 | 43 ± 4 | 39 ± 5 | 39 ± 4 | 35 ± 5 | <35 |
| ALT [U/L] | 38 ± 1 | 22 ± 7 | 22 ± 6 | 21 ± 5 | 17 ± 3 | <35 |
| LDH [U/L] | 302 ± 50 | 304 ± 22 | 248 ± 9 | 249 ± 16 | 224 ± 22 | <250 |
| Prothrombin time [%] | 114 ± 7 | 97 ± 3 | 89 ± 1 | 87 ± 3 | 97 ± 4 | 70–130 |
| PT INR | 0.93 ± 0.03 | 1.01 ± 0.01 | 1.06 ± 0.01 | 1.07 ± 0.02 | 1.01 ± 0.03 | |
| aPTT [sec] | n.d. | 27 ± 2 | 27 ± 2 | 29 ± 2 | n.d. | 27–35 |
| Fibrinogen [mg/dL] | n.d. | 237 ± 7 | 235 ± 6 | 306 ± 24 | n.d. | 180–400 |
| Antithrombin III [%] | n.d. | 101 ± 3 | 96 ± 3 | 96 ± 2 | n.d. | 80–130 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schreiber, N.; Hackl, G.; Reisinger, A.C.; Zollner-Schwetz, I.; Eller, K.; Schlagenhaufen, C.; Pietzka, A.; Czerwenka, C.; Stark, T.D.; Kranzler, M.; et al. Acute Liver Failure after Ingestion of Fried Rice Balls: A Case Series of Bacillus cereus Food Poisonings. Toxins 2022, 14, 12. https://doi.org/10.3390/toxins14010012
Schreiber N, Hackl G, Reisinger AC, Zollner-Schwetz I, Eller K, Schlagenhaufen C, Pietzka A, Czerwenka C, Stark TD, Kranzler M, et al. Acute Liver Failure after Ingestion of Fried Rice Balls: A Case Series of Bacillus cereus Food Poisonings. Toxins. 2022; 14(1):12. https://doi.org/10.3390/toxins14010012
Chicago/Turabian StyleSchreiber, Nikolaus, Gerald Hackl, Alexander C. Reisinger, Ines Zollner-Schwetz, Kathrin Eller, Claudia Schlagenhaufen, Ariane Pietzka, Christoph Czerwenka, Timo D. Stark, Markus Kranzler, and et al. 2022. "Acute Liver Failure after Ingestion of Fried Rice Balls: A Case Series of Bacillus cereus Food Poisonings" Toxins 14, no. 1: 12. https://doi.org/10.3390/toxins14010012
APA StyleSchreiber, N., Hackl, G., Reisinger, A. C., Zollner-Schwetz, I., Eller, K., Schlagenhaufen, C., Pietzka, A., Czerwenka, C., Stark, T. D., Kranzler, M., Fickert, P., Eller, P., & Ehling-Schulz, M. (2022). Acute Liver Failure after Ingestion of Fried Rice Balls: A Case Series of Bacillus cereus Food Poisonings. Toxins, 14(1), 12. https://doi.org/10.3390/toxins14010012