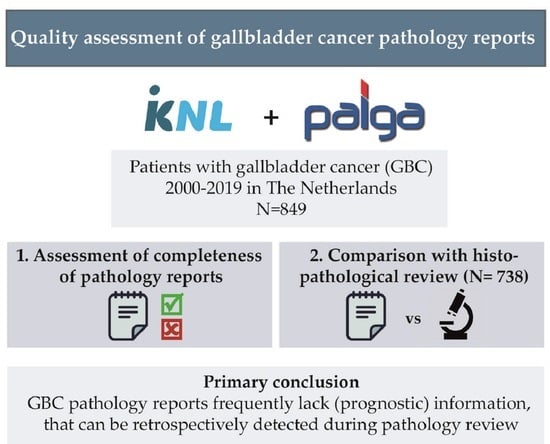
Quality Assessment of Gallbladder Cancer Pathology Reports: A Dutch Nationwide Study
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Review of Pathology Reports
2.3. Review of Histopathology
2.4. Outcomes
2.5. Statistics
3. Results
3.1. Demographic Characteristics
3.2. Overall Completeness of the Reports
3.3. Comparison between Pathology Report and Pathology Review
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Are, C.; Ahmad, H.; Ravipati, A.; Croo, D.; Clarey, D.; Smith, L.; Price, R.R.; Butte, J.M.; Gupta, S.; Chaturvedi, A.; et al. Global epidemiological trends and variations in the burden of gallbladder cancer. J. Surg. Oncol. 2017, 115, 580–590. [Google Scholar] [CrossRef] [PubMed]
- Soreide, K.; Guest, R.V.; Harrison, E.M.; Kendall, T.J.; Garden, O.J.; Wigmore, S.J. Systematic review of management of incidental gallbladder cancer after cholecystectomy. Br. J. Surg. 2019, 106, 32–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chatelain, D.; Fuks, D.; Farges, O.; Attencourt, C.; Pruvot, F.R.; Regimbeau, J.M. Pathology report assessment of incidental gallbladder carcinoma diagnosed from cholecystectomy specimens: Results of a French multicentre survey. Dig. Liver Dis. 2013, 45, 1056–1060. [Google Scholar] [CrossRef] [PubMed]
- IKNL. Galweg- en Galblaascarcinoom. Available online: https://richtlijnendatabase.nl/richtlijn/galweg_en_galblaascarcinoom/algemeen.html (accessed on 26 March 2021).
- Burt, A.D.; Alves, V.; Clouston, A.D.; Guido, M.; Hübscher, S.G.; Kakar, S.; Ng, I.O.; Nyun Park, Y.; Reeves, H.L.; Wyatt, J.; et al. Intrahepatic Cholangiocarcinoma, Perihilar Cholangiocarcinoma and Hepatocellular Carcinoma Histopathology Reporting Guide; International Collaboration on Cancer Reporting: Sydney, Australia, 2020; ISBN 978-1-922324-09-2. [Google Scholar]
- Burt, A.D.; Alves, V.; Bedossa, P.; Clouston, A.; Guido, M.; Hubscher, S.; Kakar, S.; Ng, I.; Park, Y.N.; Reeves, H.; et al. Data set for the reporting of intrahepatic cholangiocarcinoma, perihilar cholangiocarcinoma and hepatocellular carcinoma: Recommendations from the International Collaboration on Cancer Reporting (ICCR). Histopathology 2018, 73, 369–385. [Google Scholar] [CrossRef] [PubMed]
- College of American Pathologists. Protocol for the Examination of Specimens From Patients with Carcinoma of the Gallbladder. Available online: https://documents.cap.org/protocols/cp-gihepatobiliary-gallbladder-20-4100.pdf (accessed on 26 March 2021).
- Bogart, S. SankeyMATIC. Available online: http://sankeymatic.com/ (accessed on 16 March 2021).
- Shindoh, J.; de Aretxabala, X.; Aloia, T.A.; Roa, J.C.; Roa, I.; Zimmitti, G.; Javle, M.; Conrad, C.; Maru, D.M.; Aoki, T.; et al. Tumor location is a strong predictor of tumor progression and survival in T2 gallbladder cancer: An international multicenter study. Ann. Surg. 2015, 261, 733–739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, H.; Choi, D.W.; Park, J.Y.; Youn, S.; Kwon, W.; Heo, J.S.; Choi, S.H.; Jang, K.T. Surgical Strategy for T2 Gallbladder Cancer According to Tumor Location. Ann. Surg. Oncol. 2015, 22, 2779–2786. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.K.; Lee, W.; Jang, J.Y.; Kim, H.G.; Kim, J.M.; Kwag, S.J.; Park, J.H.; Kim, J.Y.; Park, T.; Jeong, S.H.; et al. Validation of the oncologic effect of hepatic resection for T2 gallbladder cancer: A retrospective study. World J. Surg. Oncol. 2019, 17, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, W.; Jeong, C.Y.; Jang, J.Y.; Kim, Y.H.; Roh, Y.H.; Kim, K.W.; Kang, S.H.; Yoon, M.H.; Seo, H.I.; Yun, S.P.; et al. Do hepatic-sided tumors require more extensive resection than peritoneal-sided tumors in patients with T2 gallbladder cancer? Results of a retrospective multicenter study. Surgery 2017, 162, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Phang, P.T.; MacFarlane, J.K.; Taylor, R.H.; Cheifetz, R.E.; Davis, N.; Hay, J.H.; McGregor, G.; Speers, C.; Sullivan, B.J.; Pitts, J.; et al. Effects of positive resection margin and tumor distance from anus on rectal cancer treatment outcomes. Am. J. Surg. 2002, 183, 504–508. [Google Scholar] [CrossRef]
- Sluijter, C.E.; van Lonkhuijzen, L.R.; van Slooten, H.J.; Nagtegaal, I.D.; Overbeek, L.I. The effects of implementing synoptic pathology reporting in cancer diagnosis: A systematic review. Virchows Arch. 2016, 468, 639–649. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baranov, N.S.; Nagtegaal, I.D.; van Grieken, N.C.T.; Verhoeven, R.H.A.; Voorham, Q.J.M.; Rosman, C.; van der Post, R.S. Synoptic reporting increases quality of upper gastrointestinal cancer pathology reports. Virchows Arch. 2019, 475, 255–259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murari, M.; Pandey, R. A synoptic reporting system for bone marrow aspiration and core biopsy specimens. Arch. Pathol. Lab. Med. 2006, 130, 1825–1829. [Google Scholar] [CrossRef] [PubMed]
- Yunker, W.K.; Matthews, T.W.; Dort, J.C. Making the most of your pathology: Standardized histopathology reporting in head and neck cancer. J. Otolaryngol. Head Neck Surg. 2008, 37, 48–55. [Google Scholar] [PubMed]

| All (n = 849) | <2013 (n = 684) | >2013 (n = 165) | p-Value | Academic (n = 143) | Non-Academic (n = 706) | p-Value | |
|---|---|---|---|---|---|---|---|
| No. of Cases Reported (%) | No. of Cases Reported (%) | No. of Cases Reported (%) | No. of Cases Reported (%) | No. of Cases Reported (%) | |||
| Clinical parameters | |||||||
| Procedure | 372 (43.8%) | 277 (40.5%) | 95 (57.6%) | <0.0001 | 92 (64.3%) | 280 (39.7%) | <0.0001 |
| Indication | 733 (86.3%) | 582 (85.1%) | 151 (91.5%) | 0.0310 | 136 (95.1%) | 597 (84.6%) | 0.0008 |
| Neoadjuvant treatment | 1 (0.1%) | 0 (0.0%) | 1 (0.6%) | 0.0416 | 1 (0.7%) | 0 (0.0%) | 0.0262 |
| Gross macroscopic features * | |||||||
| Tumor location | 283 (33.3%) | 209 (30.6%) | 74 (44.8%) | 0.0005 | 77 (53.8%) | 206 (29.2%) | <0.0001 |
| Tumor side (hepatic vs. serosal) | 173 (20.4%) | 120 (17.5%) | 53 (32.1%) | <0.0001 | 57 (39.9%) | 116 (16.4%) | <0.0001 |
| Macroscopic appearance | 268 (31.6%) | 200 (29.2%) | 68 (41.2%) | 0.0030 | 61 (42.7%) | 207 (29.3%) | 0.0018 |
| Tumor size | 357 (42.0%) | 264 (38.6%) | 93 (56.4%) | <0.0001 | 93 (65.0%) | 264 (37.4%) | <0.0001 |
| Microscopic features | |||||||
| Histologic type | 845 (99.5%) | 682 (99.7%) | 163 (98.8%) | 0.1215 | 143 (100%) | 702 (99.4%) | 0.3669 |
| T-stage | 737 (86.8%) | 583 (85.2%) | 154 (93.3%) | 0.0058 | 130 (90.9%) | 607 (86.0%) | 0.1120 |
| T1a vs. T1b (where applicable) a | 104/107 (97.2%) | 83/86 (96.5%) | 21/21 (100%) | 0.3853 | 16/16 (100%) | 88/91 (96.7%) | 0.4613 |
| N-stage | 298 (35.1%) | 216 (31.6%) | 82 (49.7%) | <0.0001 | 89 (62.2%) | 209 (29.6%) | <0.0001 |
| Tumor grade | 636 (74.9%) | 507 (74.1%) | 129 (78.2%) | 0.2804 | 93 (65.0%) | 543 (76.9%) | 0.0028 |
| Cystic duct margin | 657 (77.4%) | 517 (75.6%) | 140 (84.8%) | 0.0107 | 111 (77.6%) | 546 (77.3%) | 0.9407 |
| Distance to resection plane reported b | 45/440 (10.2%) | 21/333 (6.3%) | 24/107 (22.4%) | <0.0001 | 16/76 (21.1%) | 29/364 (8%) | 0.0006 |
| Liver margin | 349 (41.1%) | 258 (37.7%) | 91 (55.2%) | <0.0001 | 89 (62.2%) | 260 (36.8%) | <0.0001 |
| Distance to resection plane reported b | 58/211 (27.5%) | 34/152 (22.4%) | 24/59 (40.7%) | 0.0075 | 28/89 (31.5%) | 30/122 (24.6%) | 0.2696 |
| Lymphatic invasion | 157 (18.5%) | 97 (14.2%) | 60 (36.4%) | <0.0001 | 42 (29.4%) | 115 (16.3%) | 0.0002 |
| Venous invasion | 218 (25.7%) | 132 (19.3%) | 86 (36.4%) | <0.0001 | 62 (43.4%) | 156 (22.1%) | <0.0001 |
| Perineural invasion | 219 (25.8%) | 136 (19.9%) | 83 (36.4%) | <0.0001 | 64 (44.8%) | 155 (22%) | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Bitter, T.J.J.; de Savornin-Lohman, E.A.J.; de Reuver, P.R.; Versteeg, V.S.; Vink-Börger, E.; Verheij, J.; Nagtegaal, I.D.; van der Post, R.S. Quality Assessment of Gallbladder Cancer Pathology Reports: A Dutch Nationwide Study. Cancers 2021, 13, 2977. https://doi.org/10.3390/cancers13122977
de Bitter TJJ, de Savornin-Lohman EAJ, de Reuver PR, Versteeg VS, Vink-Börger E, Verheij J, Nagtegaal ID, van der Post RS. Quality Assessment of Gallbladder Cancer Pathology Reports: A Dutch Nationwide Study. Cancers. 2021; 13(12):2977. https://doi.org/10.3390/cancers13122977
Chicago/Turabian Stylede Bitter, Tessa J. J., Elise A. J. de Savornin-Lohman, Philip R. de Reuver, Valerie Sophie Versteeg, Elisa Vink-Börger, Joanne Verheij, Iris D. Nagtegaal, and Rachel S. van der Post. 2021. "Quality Assessment of Gallbladder Cancer Pathology Reports: A Dutch Nationwide Study" Cancers 13, no. 12: 2977. https://doi.org/10.3390/cancers13122977
APA Stylede Bitter, T. J. J., de Savornin-Lohman, E. A. J., de Reuver, P. R., Versteeg, V. S., Vink-Börger, E., Verheij, J., Nagtegaal, I. D., & van der Post, R. S. (2021). Quality Assessment of Gallbladder Cancer Pathology Reports: A Dutch Nationwide Study. Cancers, 13(12), 2977. https://doi.org/10.3390/cancers13122977