Research Progress of Indole Alkaloids: Targeting MAP Kinase Signaling Pathways in Cancer Treatment
Abstract
:Simple Summary
Abstract
1. Introduction
2. MAPK Signaling Pathway in Cancer
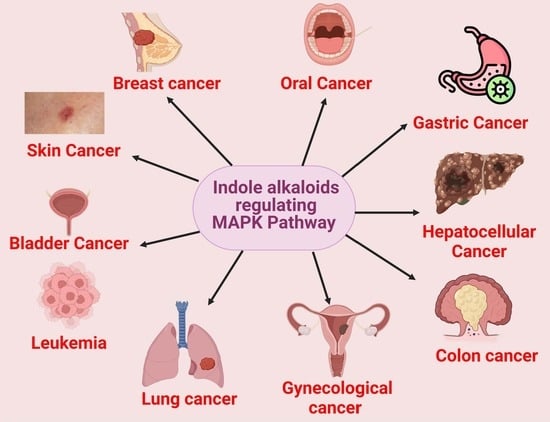
3. Indole Alkaloids Targeting MAPK in Cancers
3.1. Evodiamine
3.2. Vinorelbine
3.3. Hirsutine
3.4. Fumigaclavine C
3.5. Flavopereirine
3.6. Evodiagenine
3.7. 3,3′-Diindolylmethane
3.8. Idole-3-Carbinol
3.9. Notoamide G
3.10. Vinblastine
3.11. Vincristine
3.12. Sclerotiamides C
3.13. Ellipticine
3.14. Chaetoglobosin K
3.15. Jerantinine B
3.16. Harmalacidine
3.17. L20
3.18. 11-Methoxytabersonine
3.19. Calothrixin A
3.20. Harmol
3.21. Chaetoglobosin G
3.22. 3α-Acetonyltabersonine
3.23. Isomahanine
3.24. Dehydrocrenatidine
4. Clinical Trials
5. Toxicity and Adverse Effects
6. Conclusions and Future Perspective
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chu, J.J.; Mehrzad, R. The Biology of Cancer. In The Link Between Obesity and Cancer; Elsevier: Amsterdam, The Netherlands, 2023; pp. 35–45. [Google Scholar]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Anand, P.; Kunnumakara, A.B.; Sundaram, C.; Harikumar, K.B.; Tharakan, S.T.; Lai, O.S.; Sung, B.; Aggarwal, B.B. Cancer Is a Preventable Disease That Requires Major Lifestyle Changes. Pharm. Res. 2008, 25, 2097–2116. [Google Scholar] [CrossRef] [PubMed]
- Debela, D.T.; Muzazu, S.G.Y.; Heraro, K.D.; Ndalama, M.T.; Mesele, B.W.; Haile, D.C.; Kitui, S.K.; Manyazewal, T. New Approaches and Procedures for Cancer Treatment: Current Perspectives. SAGE Open Med. 2021, 9, 20503121211034370. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Pan, W.; Liu, S.; Shen, Z.; Xu, Y.; Hu, L. ERK/MAPK Signalling Pathway and Tumorigenesis. Exp. Ther. Med. 2020, 19, 1997–2007. [Google Scholar] [CrossRef] [PubMed]
- Rezatabar, S.; Karimian, A.; Rameshknia, V.; Parsian, H.; Majidinia, M.; Kopi, T.A.; Bishayee, A.; Sadeghinia, A.; Yousefi, M.; Monirialamdari, M.; et al. RAS/MAPK Signaling Functions in Oxidative Stress, DNA Damage Response and Cancer Progression. J. Cell. Physiol. 2019, 234, 14951–14965. [Google Scholar] [CrossRef]
- Ahmed, T.; Zulfiqar, A.; Arguelles, S.; Rasekhian, M.; Nabavi, S.F.; Silva, A.S.; Nabavi, S.M. Map Kinase Signaling as Therapeutic Target for Neurodegeneration. Pharmacol. Res. 2020, 160, 105090. [Google Scholar] [CrossRef]
- Shi, L.; Qin, H.; Jin, X.; Yang, X.; Lu, X.; Wang, H.; Wang, R.; Yu, D.; Feng, B. The Natural Phenolic Peperobtusin A Induces Apoptosis of Lymphoma U937 Cells via the Caspase Dependent and P38 MAPK Signaling Pathways. Biomed. Pharmacother. 2018, 102, 772–781. [Google Scholar] [CrossRef]
- Anjum, J.; Mitra, S.; Das, R.; Alam, R.; Mojumder, A.; Emran, T.B.; Islam, F.; Rauf, A.; Hossain, M.J.; Aljohani, A.S.M.; et al. A Renewed Concept on the MAPK Signaling Pathway in Cancers: Polyphenols as a Choice of Therapeutics. Pharmacol. Res. 2022, 184, 106398. [Google Scholar] [CrossRef]
- Wei, J.; Liu, R.; Hu, X.; Liang, T.; Zhou, Z.; Huang, Z. MAPK Signaling Pathway-Targeted Marine Compounds in Cancer Therapy. J. Cancer Res. Clin. Oncol. 2021, 147, 3–22. [Google Scholar] [CrossRef]
- Burotto, M.; Chiou, V.L.; Lee, J.M.; Kohn, E.C. The MAPK Pathway across Different Malignancies: A New Perspective. Cancer 2014, 120, 3446–3456. [Google Scholar] [CrossRef]
- Tay, K.-C.; Tan, L.T.-H.; Chan, C.K.; Hong, S.L.; Chan, K.-G.; Yap, W.H.; Pusparajah, P.; Lee, L.-H.; Goh, B.-H. Formononetin: A Review of Its Anticancer Potentials and Mechanisms. Front. Pharmacol. 2019, 10, 820. [Google Scholar] [CrossRef]
- Santarpia, L.; Lippman, S.M.; El-Naggar, A.K. Targeting the MAPKRASRAF Signaling Pathway in Cancer Therapy. Expert Opin. Ther. Targets 2012, 16, 103–119. [Google Scholar] [CrossRef]
- Wu, Q.; Wu, W.; Fu, B.; Shi, L.; Wang, X.; Kuca, K. JNK Signaling in Cancer Cell Survival. Med. Res. Rev. 2019, 39, 2082–2104. [Google Scholar] [CrossRef]
- Wu, H.L.; Fu, X.Y.; Cao, W.Q.; Xiang, W.Z.; Hou, Y.J.; Ma, J.K.; Wang, Y.; Fan, C.D. Induction of Apoptosis in Human Glioma Cells by Fucoxanthin via Triggering of ROS-Mediated Oxidative Damage and Regulation of MAPKs and PI3K-AKT Pathways. J. Agric. Food Chem. 2019, 67, 2212–2219. [Google Scholar] [CrossRef]
- Lee, S.; Rauch, J.; Kolch, W. Targeting MAPK Signaling in Cancer: Mechanisms of Drug Resistance and Sensitivity. Int. J. Mol. Sci. 2020, 21, 1102. [Google Scholar] [CrossRef] [PubMed]
- Gul, W.; Hamann, M.T. Indole Alkaloid Marine Natural Products: An Established Source of Cancer Drug Leads with Considerable Promise for the Control of Parasitic, Neurological and Other Diseases. Life Sci. 2005, 78, 442–453. [Google Scholar] [CrossRef] [PubMed]
- Ullah, A.; Ullah, N.; Nawaz, T.; Aziz, T. Molecular Mechanisms of Sanguinarine in Cancer Prevention and Treatment. Anticancer Agents Med. Chem. 2022, 23, 765–778. [Google Scholar] [CrossRef]
- Gongora-Castillo, E.; Childs, K.L.; Fedewa, G.; Hamilton, J.P.; Liscombe, D.K.; Magallanes-Lundback, M.; Mandadi, K.K.; Nims, E.; Runguphan, W.; Vaillancourt, B. Development of Transcriptomic Resources for Interrogating the Biosynthesis of Monoterpene Indole Alkaloids in Medicinal Plant Species. PLoS ONE 2012, 7, e52506. [Google Scholar] [CrossRef] [PubMed]
- Pearson, G.; Robinson, F.; Beers Gibson, T.; Xu, B.; Karandikar, M.; Berman, K.; Cobb, M.H. Mitogen-Activated Protein (MAP) Kinase Pathways: Regulation and Physiological Functions. Endocr. Rev. 2001, 22, 153–183. [Google Scholar]
- Kudaravalli, S.; den Hollander, P.; Mani, S.A. Role of P38 MAP Kinase in Cancer Stem Cells and Metastasis. Oncogene 2022, 41, 3177–3185. [Google Scholar] [CrossRef] [PubMed]
- Hong, B.; Li, H.; Zhang, M.; Xu, J.; Lu, Y.; Zheng, Y.; Qian, J.; Chang, J.T.; Yang, J.; Yi, Q. P38 MAPK Inhibits Breast Cancer Metastasis through Regulation of Stromal Expansion. Int. J. Cancer 2015, 136, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Molnár, Á.; Theodoras, A.M.; Zon, L.I.; Kyriakis, J.M. Cdc42Hs, but Not Rac1, Inhibits Serum-Stimulated Cell Cycle Progression at G1/S through a Mechanism Requiring P38/RK. J. Biol. Chem. 1997, 272, 13229–13235. [Google Scholar] [CrossRef]
- Thang, W.; Lui, H.T. MAPK Signal Pathways in the Regulation of Cell Proliferation in Mammalian Cells. Cell Res. 2002, 12, 9–18. [Google Scholar]
- Nebreda, A.R.; Porras, A. P38 MAP Kinases: Beyond the Stress Response. Trends Biochem. Sci. 2000, 25, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Kogushi-Nishi, H.; Jinnin, M.; Kobayashi, Y.; Muchemwa, F.C.; Hirano, A.; Makino, T.; Fukushima, S.; Masuguchi, S.; Ishihara, T.; Inoue, Y. Role of C-Jun N-terminal Kinase Isoforms in the Cellular Activity of Melanoma Cell Lines. Clin. Exp. Dermatol. 2013, 38, 890–896. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-R.; Tan, T.-H. The C-Jun N-Terminal Kinase Pathway and Apoptotic Signaling. Int. J. Oncol. 2000, 16, 651–713. [Google Scholar] [CrossRef]
- Srivastava, R.K.; Mi, Q.-S.; Hardwick, J.M.; Longo, D.L. Deletion of the Loop Region of Bcl-2 Completely Blocks Paclitaxel-Induced Apoptosis. Proc. Natl. Acad. Sci. USA 1999, 96, 3775–3780. [Google Scholar] [CrossRef]
- Yamamoto, K.; Ichijo, H.; Korsmeyer, S.J. BCL-2 Is Phosphorylated and Inactivated by an ASK1/Jun N-Terminal Protein Kinase Pathway Normally Activated at G2/M. Mol. Cell. Biol. 1999, 19, 8469–8478. [Google Scholar] [CrossRef]
- Tournier, C.; Hess, P.; Yang, D.D.; Xu, J.; Turner, T.K.; Nimnual, A.; Bar-Sagi, D.; Jones, S.N.; Flavell, R.A.; Davis, R.J. Requirement of JNK for Stress-Induced Activation of the Cytochrome c- Mediated Death Pathway. Science 2000, 288, 870–874. [Google Scholar] [CrossRef]
- Davis, R.J. Signal Transduction by the JNK Group of MAP Kinases. Cell 2000, 103, 239–252. [Google Scholar] [CrossRef]
- Kohno, M.; Tanimura, S.; Ozaki, K. Targeting the Extracellular Signal-Regulated Kinase Pathway in Cancer Therapy. Biol. Pharm. Bull. 2011, 34, 1781–1784. [Google Scholar] [CrossRef] [PubMed]
- Rubinfeld, H.; Seger, R. The ERK Cascade: A Prototype of MAPK Signaling. Mol. Biotechnol. 2005, 31, 151–174. [Google Scholar] [CrossRef]
- Singh, D.; Bhartiya, J. FSH-FSHR3-Stem Cells in Ovary Surface Epithelium: Basis for Adult Ovarian Biology, Failure, Aging and Cancer. Reproduction 2015, 149, R35–R48. [Google Scholar]
- Rao, A.; Herr, D.R. G Protein-Coupled Receptor GPR19 Regulates E-Cadherin Expression and Invasion of Breast Cancer Cells. Biochim. Biophys. Acta–Mol. Cell Res. 2017, 1864, 1318–1327. [Google Scholar] [CrossRef]
- Tang, Q.; Wu, J.J.; Zheng, F.; Chen, Y.Q.; Hann, S.S. Emodin Increases Expression of Insulin-like Growth Factor Binding Protein 1 through Activation of MEK/ERK/AMPKα and Interaction of PPARγ and Sp1 in Lung Cancer. Cell. Physiol. Biochem. 2017, 41, 339–357. [Google Scholar] [CrossRef] [PubMed]
- Du, J.; Wang, X.-F.; Zhou, Q.-M.; Zhang, T.-L.; Lu, Y.-Y.; Zhang, H.; Su, S.-B. Evodiamine Induces Apoptosis and Inhibits Metastasis in MDA-MB-231 Human Breast Cancer Cells in Vitro and in Vivo. Oncol. Rep. 2013, 30, 685–694. [Google Scholar] [CrossRef]
- Urosevic, J.; Garcia-Albeniz, X.; Planet, E.; Real, S.; Céspedes, M.V.; Guiu, M.; Fernandez, E.; Bellmunt, A.; Gawrzak, S.; Pavlovic, M. Colon Cancer Cells Colonize the Lung from Established Liver Metastases through P38 MAPK Signalling and PTHLH. Nat. Cell Biol. 2014, 16, 685–694. [Google Scholar] [CrossRef]
- Chien, C.-C.; Wu, M.-S.; Shen, S.-C.; Ko, C.-H.; Chen, C.-H.; Yang, L.-L.; Chen, Y.-C. Activation of JNK Contributes to Evodiamine-Induced Apoptosis and G2/M Arrest in Human Colorectal Carcinoma Cells: A Structure-Activity Study of Evodiamine. PLoS ONE 2014, 9, e99729. [Google Scholar] [CrossRef]
- Hong, Z.; Wang, Z.; Zhou, B.; Wang, J.; Tong, H.; Liao, Y.; Zheng, P.; Jamshed, M.B.; Zhang, Q.; Chen, H. Effects of Evodiamine on PI3K/Akt and MAPK/ERK Signaling Pathways in Pancreatic Cancer Cells. Int. J. Oncol. 2020, 56, 783–793. [Google Scholar] [CrossRef]
- Lijuan, W.; Xiaoying, J.; Zipei, C.; Wenlu, L. Evodiamine Induces Extrinsic and Intrinsic Apoptosis of Ovarian Cancer Cells via the Mitogen-Activated Protein Kinase/Phosphatidylinositol-3-Kinase/Protein Kinase B Signaling Pathways. J. Tradit. Chin. Med. 2016, 36, 353–359. [Google Scholar] [CrossRef]
- Zhang, Y.; Wu, L.-J.; Tashiro, S.-I.; Onodera, S.; Ikejima, T. Evodiamine Induces Tumor Cell Death through Different Pathways: Apoptosis and Necrosis. Acta Pharmacol. Sin. 2004, 25, 83–89. [Google Scholar]
- Shi, C.-S.; Li, J.-M.; Chin, C.-C.; Kuo, Y.-H.; Lee, Y.-R.; Huang, Y.-C. Evodiamine Induces Cell Growth Arrest, Apoptosis and Suppresses Tumorigenesis in Human Urothelial Cell Carcinoma Cells. Anticancer Res. 2017, 37, 1149–1159. [Google Scholar]
- Liu, A.J.; Wang, S.H.; Chen, K.C.; Kuei, H.P.; Shih, Y.L.; Hou, S.Y.; Chiu, W.T.; Hsiao, S.H.; Shih, C.M. Evodiamine, a Plant Alkaloid, Induces Calcium/JNK-Mediated Autophagy and Calcium/Mitochondria-Mediated Apoptosis in Human Glioblastoma Cells. Chem. Biol. Interact. 2013, 205, 20–28. [Google Scholar] [CrossRef]
- Hong, J.-Y.; Park, S.H.; Min, H.-Y.; Park, H.J.; Lee, S.K. Anti-Proliferative Effects of Evodiamine in Human Lung Cancer Cells. J. Cancer Prev. 2014, 19, 7. [Google Scholar] [CrossRef]
- Liem, A.A.; Appleyard, M.; O’Neill, M.A.; Hupp, T.R.; Chamberlain, M.P.; Thompson, A.M. Doxorubicin and Vinorelbine Act Independently via P53 Expression and P38 Activation Respectively in Breast Cancer Cell Lines. Br. J. Cancer 2003, 88, 1281–1284. [Google Scholar] [CrossRef]
- Lou, C.; Yokoyama, S.; Saiki, I.; Hayakawa, Y. Selective Anticancer Activity of Hirsutine against HER2-positive Breast Cancer Cells by Inducing DNA Damage. Oncol. Rep. 2015, 33, 2072–2076. [Google Scholar] [CrossRef]
- Li, Y.X.; Himaya, S.W.A.; Dewapriya, P.; Zhang, C.; Kim, S.K. Fumigaclavine C from a Marine-Derived Fungus Aspergillus Fumigatus Induces Apoptosis in MCF-7 Breast Cancer Cells. Mar. Drugs 2013, 11, 5063–5086. [Google Scholar] [CrossRef]
- Yeh, H.T.; Tsai, Y.S.; Chen, M.S.; Li, Y.Z.; Lin, W.C.; Lee, Y.R.; Tseng, Y.S.; Sheu, S.M. Flavopereirine Induces Cell Cycle Arrest and Apoptosis via the AKT/P38 MAPK/ERK1/2 Signaling Pathway in Human Breast Cancer Cells. Eur. J. Pharmacol. 2019, 863, 172658. [Google Scholar] [CrossRef]
- Li, J.M.; Huang, Y.C.; Kuo, Y.H.; Cheng, C.C.; Kuan, F.C.; Chang, S.F.; Lee, Y.R.; Chin, C.C.; Shi, C.S. Flavopereirine Suppresses the Growth of Colorectal Cancer Cells through P53 Signaling Dependence. Cancers 2019, 11, 1034. [Google Scholar] [CrossRef]
- Xu, C.; Wang, Q.; Feng, X.; Bo, Y. Effect of Evodiagenine Mediates Photocytotoxicity on Human Breast Cancer Cells MDA-MB-231 through Inhibition of PI3K/AKT/MTOR and Activation of P38 Pathways. Fitoterapia 2014, 99, 292–299. [Google Scholar] [CrossRef]
- Ye, Y.; Ye, F.; Li, X.; Yang, Q.; Zhou, J.; Xu, W.; Aschner, M.; Lu, R.; Miao, S. 3,3′-Diindolylmethane Exerts Anti-Proliferation and Apoptosis Induction by TRAF2-P38 Axis in Gastric Cancer. Anticancer Drugs 2021, 32, 189. [Google Scholar] [CrossRef]
- Zhu, J.; Li, Y.; Guan, C.; Chen, Z. Anti-Proliferative and pro-Apoptotic Effects of 3,3′-Diindolylmethane in Human Cervical Cancer Cells. Oncol. Rep. 2012, 28, 1063–1068. [Google Scholar] [CrossRef]
- Khwaja, F.S.; Wynne, S.; Posey, I.; Djakiew, D. 3,3′-Diindolylmethane Induction of P75NTR-Dependent Cell Death via the P38 Mitogen-Activated Protein Kinase Pathway in Prostate Cancer Cellsp75NTR-Dependent Cell Death DIM Induction via P38 MAPK. Cancer Prev. Res. 2009, 2, 566–571. [Google Scholar] [CrossRef] [PubMed]
- Vivar, O.I.; Lin, C.-L.; Firestone, G.L.; Bjeldanes, L.F. 3,3′-Diindolylmethane Induces a G1 Arrest in Human Prostate Cancer Cells Irrespective of Androgen Receptor and P53 Status. Biochem. Pharmacol. 2009, 78, 469–476. [Google Scholar] [CrossRef]
- Ping, J.; Li, J.; Liao, Z.; Shang, L.; Wang, H. Indole-3-Carbinol Inhibits Hepatic Stellate Cells Proliferation by Blocking NADPH Oxidase/Reactive Oxygen Species/P38 MAPK Pathway. Eur. J. Pharmacol. 2011, 650, 656–662. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.; Zhang, T.; Liu, D.; Guan, G.; Huang, J.; Proksch, P.; Chen, X.; Lin, W. Notoamide-Type Alkaloid Induced Apoptosis and Autophagy: Via a P38/JNK Signaling Pathway in Hepatocellular Carcinoma Cells. RSC Adv. 2019, 9, 19855–19868. [Google Scholar] [CrossRef]
- Deacon, K.; Mistry, P.; Chernoff, J.; Blank, J.L.; Patel, R. P38 Mitogen-Activated Protein Kinase Mediates Cell Death and P21-Activated Kinase Mediates Cell Survival during Chemotherapeutic Drug-Induced Mitotic Arrest. Mol. Biol. Cell 2003, 14, 2071–2087. [Google Scholar] [CrossRef]
- Zhu, B.; Wang, P.; Zhang, X.D.; Jiang, C.C.; Chen, L.H.; Avery-Kiejda, K.A.; Watts, R.; Hersey, P. Activation of Jun N-Terminal Kinase Is a Mediator of Vincristine-Induced Apoptosis of Melanoma Cells. Anticancer Drugs 2008, 19, 189–200. [Google Scholar] [CrossRef]
- Guo, X.; Meng, Q.; Liu, J.; Wu, J.; Jia, H.; Liu, D.; Gu, Y.; Liu, J.; Huang, J.; Fan, A.; et al. Sclerotiamides C-H, Notoamides from a Marine Gorgonian-Derived Fungus with Cytotoxic Activities. J. Nat. Prod. 2022, 85, 1067–1078. [Google Scholar] [CrossRef]
- Kim, J.Y.; Lee, S.G.; Chung, J.-Y.; Kim, Y.-J.; Park, J.-E.; Koh, H.; Han, M.S.; Park, Y.C.; Yoo, Y.H.; Kim, J.-M. Ellipticine Induces Apoptosis in Human Endometrial Cancer Cells: The Potential Involvement of Reactive Oxygen Species and Mitogen-Activated Protein Kinases. Toxicology 2011, 289, 91–102. [Google Scholar] [CrossRef]
- Li, B.; Gao, Y.; Rankin, G.O.; Rojanasakul, Y.; Cutler, S.J.; Tu, Y.; Chen, Y.C. Chaetoglobosin K Induces Apoptosis and G2 Cell Cycle Arrest through P53-Dependent Pathway in Cisplatin-Resistant Ovarian Cancer Cells. Cancer Lett. 2015, 356, 418–433. [Google Scholar] [CrossRef] [PubMed]
- Alhuthali, H.M.; Bradshaw, T.D.; Lim, K.-H.; Kam, T.-S.; Seedhouse, C.H. The Natural Alkaloid Jerantinine B Has Activity in Acute Myeloid Leukemia Cells through a Mechanism Involving C-Jun. BMC Cancer 2020, 20, 629. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhang, Z.; Wang, Y.; He, X. Cytotoxic Indole Alkaloids against Human Leukemia Cell Lines from the Toxic Plant Peganum harmala. Toxins 2015, 7, 4507–4518. [Google Scholar] [CrossRef]
- Long, Q.; Xiao, X.; Yi, P.; Liu, Y.; Varier, K.M.; Rao, Q.; Song, J.; Qiu, J.; Wang, C.; Liu, W.; et al. L20, a Calothrixin B Analog, Induces Intrinsic Apoptosis on HEL Cells through ROS/γ-H2AX/P38 MAPK Pathway. Biomed. Pharmacother. 2021, 137, 111336. [Google Scholar] [CrossRef] [PubMed]
- Ge, D.; Tao, H.-R.; Fang, L.; Kong, X.-Q.; Han, L.-N.; Li, N.; Xu, Y.-X.; Li, L.-Y.; Yu, M.; Zhang, H. 11-Methoxytabersonine Induces Necroptosis with Autophagy through AMPK/MTOR and JNK Pathways in Human Lung Cancer Cells. Chem. Pharm. Bull. 2020, 68, 244–250. [Google Scholar] [CrossRef]
- Yang, X.; Gao, J.; Guo, J.; Zhao, Z.; Zhang, S.L.; He, Y. Anti-Lung Cancer Activity and Inhibitory Mechanisms of a Novel Calothrixin A Derivative. Life Sci. 2019, 219, 20–30. [Google Scholar] [CrossRef]
- Abe, A.; Yamada, H.; Moriya, S.; Miyazawa, K. The β-Carboline Alkaloid Harmol Induces Cell Death via Autophagy but Not Apoptosis in Human Non-Small Cell Lung Cancer A549 Cells. Biol. Pharm. Bull. 2011, 34, 1264–1272. [Google Scholar] [CrossRef]
- Chen, J.; Guo, Q.; Zhang, J.; Yin, Z.; Song, W.; He, B.; Zhang, Y.; Zhang, W.; Chen, L. Chaetoglobosin G Inhibits Proliferation, Autophagy and Cell Cycle of Lung Cancer Cells through EGFR/MEK/ERK Signaling Pathway. Pharmazie 2020, 75, 642–645. [Google Scholar]
- Li, Y.; Zhao, Y.; Zhou, X.; Ni, W.; Dai, Z.; Yang, D.; Hao, J.; Luo, L.; Liu, Y.; Luo, X.; et al. Cytotoxic Indole Alkaloid 3α-Acetonyltabersonine Induces Glioblastoma Apoptosis via Inhibition of DNA Damage Repair. Toxins 2017, 9, 150. [Google Scholar] [CrossRef]
- Utaipant, T.; Athipornchai, A.; Suksamrarn, A.; Chunsrivirot, S.; Chunglok, W. Isomahanine Induces Endoplasmic Reticulum Stress and Simultaneously Triggers P38 MAPK-Mediated Apoptosis and Autophagy in Multidrug-Resistant Human Oral Squamous Cell Carcinoma Cells. Oncol. Rep. 2017, 37, 1243–1252. [Google Scholar] [CrossRef]
- Ho, H.Y.; Lin, C.C.; Chuang, Y.C.; Lo, Y.S.; Hsieh, M.J.; Chen, M.K. Apoptotic Effects of Dehydrocrenatidine via JNK and ERK Pathway Regulation in Oral Squamous Cell Carcinoma. Biomed. Pharmacother. 2021, 137, 111362. [Google Scholar] [CrossRef]
- Ali, A.; Sidorova, T.S.; Matesic, D.F. Dual Modulation of JNK and Akt Signaling Pathways by Chaetoglobosin K in Human Lung Carcinoma and Ras-Transformed Epithelial Cells. Investig. New Drugs 2013, 31, 525–534. [Google Scholar] [CrossRef]
- Qin, R.; You, F.M.; Zhao, Q.; Xie, X.; Peng, C.; Zhan, G.; Han, B. Naturally Derived Indole Alkaloids Targeting Regulated Cell Death (RCD) for Cancer Therapy: From Molecular Mechanisms to Potential Therapeutic Targets. J. Hematol. Oncol. 2022, 15, 133. [Google Scholar] [CrossRef] [PubMed]
- Mitra, S.; Prova, S.R.; Sultana, S.A.; Das, R.; Nainu, F.; Emran, T.B.; Tareq, A.M.; Uddin, M.S.; Alqahtani, A.M.; Dhama, K.; et al. Therapeutic Potential of Indole Alkaloids in Respiratory Diseases: A Comprehensive Review. Phytomedicine 2021, 90, 153649. [Google Scholar] [CrossRef] [PubMed]
- Almagro, L.; Fernández-Pérez, F.; Pedreño, M.A. Indole Alkaloids from Catharanthus Roseus: Bioproduction and Their Effect on Human Health. Molecules 2015, 20, 2973–3000. [Google Scholar] [CrossRef] [PubMed]
- Gregory, R.K.; Smith, I.E. Vinorelbine- a Clinical Review. Br. J. Cancer 2000, 82, 1907–1913. [Google Scholar] [CrossRef]
- Zhang, Y.; Yang, S.H.; Guo, X.L. New Insights into Vinca Alkaloids Resistance Mechanism and Circumvention in Lung Cancer. Biomed. Pharmacother. 2017, 96, 659–666. [Google Scholar] [CrossRef]
- Le Chevalier, T.; Brisgand, D.; Douillard, J.Y.; Pujol, J.L.; Alberola, V.; Monnier, A.; Riviere, A.; Lianes, P.; Chomy, P.; Cigolari, S. Randomized Study of Vinorelbine and Cisplatin versus Vindesine and Cisplatin versus Vinorelbine Alone in Advanced Non-Small-Cell Lung Cancer: Results of a European Multicenter Trial Including 612 Patients. Lung Cancer 1994, 11, 340–341. [Google Scholar] [CrossRef]
- Tabchi, S.; Blais, N.; Campeau, M.P.; Tehfe, M. Single-Center Comparison of Multiple Chemotherapy Regimens for Concurrent Chemoradiotherapy in Unresectable Stage III Non-Small-Cell Lung Cancer. Cancer Chemother. Pharmacol. 2017, 79, 381–387. [Google Scholar] [CrossRef]
- Spigel, D.R.; Hainsworth, J.D.; Lane, C.M.; Clark, B.; Burris, H.A.; Greco, F.A. Phase II Trial of Vinflunine in Relapsed Small Cell Lung Cancer. J. Thorac. Oncol. 2010, 5, 874–878. [Google Scholar] [CrossRef]
- Talbot, D.C.; Margery, J.; Dabouis, G.; Dark, G.; Taylor, H.; Boussemart, H.; Cadic, V.; Pinel, M.C.; Rivière, A.; Ollivier, L.; et al. Phase II Study of Vinflunine in Malignant Pleural Mesothelioma. J. Clin. Oncol. 2007, 25, 4751–4756. [Google Scholar] [CrossRef] [PubMed]
- Meng, Y.; Jin, J.; Gong, C.; Miao, H.; Tao, Z.; Li, T.; Cao, J.; Wang, L.; Wang, B.; Zhang, J.; et al. Phase II Study of Chidamide in Combination with Cisplatin in Patients with Metastatic Triple-Negative Breast Cancer. Ann. Palliat. Med. 2021, 10, 11255–11264. [Google Scholar] [CrossRef]
- Bates, S.; Kang, M.; Meadows, B.; Bakke, S.; Choyke, P.; Merino, M.; Goldspiel, B.; Chico, I.; Smith, T.; Chen, C.; et al. A Phase I Study of Infusional Vinblastine in Combination with the P-Glycoprotein Antagonist PSC 833 (Valspodar). Cancer 2001, 92, 1577–1590. [Google Scholar] [CrossRef]
- Sonawane, T.; Azaz, S.; Hemant, K.; Liji, T. Epididymal Toxicity Associated with Vincristine Treatment. Indian J. Pharm. Sci. 2019, 81, 514–520. [Google Scholar] [CrossRef]
- Kukula-Koch, W.A.; Widelski, J. Alkaloids; Elsevier: Amsterdam, The Netherlands, 2017; ISBN 9780128020999. [Google Scholar]
- Harding, K.; Bergman, N.; Smith, A.; Lindley, S.; Szivek, A.; Milner, R.; Brawner, W.; Lejeune, A. Response Rate to a Single Dose of Vinblastine Administered to Dogs with Treatment-Naive Multicentric Lymphoma. Vet. Comp. Oncol. 2018, 16, 636–641. [Google Scholar] [CrossRef]
- Li, F.; Dong, Y.Z.; Zhang, D.; Zhang, X.M.; Lin, Z.J.; Zhang, B. Molecular Mechanisms Involved in Druginduced Liver Injury Caused by Urate-Lowering Chinese Herbs: A Network Pharmacology Study and Biology Experiments. PLoS ONE 2019, 14, e0216948. [Google Scholar] [CrossRef]
- Sun, Q.; Xie, L.; Song, J.; Li, X. Evodiamine: A Review of Its Pharmacology, Toxicity, Pharmacokinetics and Preparation Researches. J. Ethnopharmacol. 2020, 262, 113164. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Ma, L.; Li, S.; Cui, K.; Lei, L.; Ye, Z. Evaluation of the Cardiotoxicity of Evodiamine In Vitro and In Vivo. Molecules 2017, 22, 943. [Google Scholar] [CrossRef]


| Compounds | Cancer Type | Findings | Ref. |
|---|---|---|---|
| Evodiamine | Breast cancer | The p38 MAPK and ERK pathways are controlled by evodiamine. | [37] |
| Colon cancer | JNK activation induces apoptosis triggered by evodiamine | [39] | |
| Pancreatic cancer | Evodiamine dose-dependently stopped AKT, ERK1/2, and P38-MAPK phosphorylation. | [40] | |
| Ovarian cancer | When evodiamine is present, PI3K/Akt, p38 MAPK, and ERK1/2 MAPK activation may result in cell death. | [41] | |
| Skin cancer | Evodiamine induced caspase-mediated apoptosis and necrosis through the activation of p38 and ERK MAPK. | [42] | |
| Bladder cancer | When evodiamine was added to 5637 and HT1197 cells, the P38-MAPK and some of the JNK pathways became more active while ERK pathway only became less active in 5637 cells. | [43] | |
| Neural cancer | Glioma cells are destroyed by evodiamine via autophagy triggered by intracellular calcium/JNK signaling and apoptosis triggered by calcium/mitochondria. | [44] | |
| Lung cacner | p-ERK and ERK-MAPK expression was inhibited by evodiamine. | [45] | |
| Vinorelbine | Breast cancer | Vinorelbine increased P38-MAPK activity in breast cancer cells MCF-7 and MDA-MB-468. | [46] |
| Hirsutine | Breast cancer | In addition to activating the p38-MAPK pathway, DNA damage signaling was induced in MDA-MB-453 cells | [47] |
| Fumigaclavine C | Breast cancer | Fumigaclavine C dose-dependently reduced JNK, ERK 1/2, and P38-MAPK phosphorylation. | [48] |
| Flavopereirine | Breast cancer | Flavopereirine causes MDA-MB-231 cell death via cell cycle arrest and AKT/P38-MAPK signaling pathway. | [49] |
| Colon cancer | Flavopereirine elicited a decrease in cellular viability, impeded progression of the cell cycle, and prompted apoptosis via P53 signaling. | [50] | |
| Evodiagenine | Breast cancer | Evodiagenine may inhibit PI3K/AKT/mTOR and increase P38-MAPK phosphorylation to cause photocytotoxicity | [51] |
| 3,3′-Diindolylmethane | Gastric cancer | 3,3′-diindolylmethane inhibits gastric cancer proliferation and triggers apoptosis via altering the TRAF2/p38-MAPK signaling pathway. | [52] |
| Cervical cancer | The MAPK and PI3K signaling pathways have been shown to be involved in 3,3′-Diindolylmethane’s pro-apoptotic actions on cervical cancer cells. | [53] | |
| Prostate cancer | 3,3′-Diindolylmethane as an indole capable of eliciting p75NTR-dependent apoptosis in prostate cancer cells via the p38-MAPK pathway. | [54] | |
| Prostate cancer | In DU145 cells, 3,3′-diindolylmethane activates the p38-MAPK pathway in order to activate p27Kip1 and stop the cell cycle in G1. | [55] | |
| Idole-3-carbinol | Hepatocellular cancer | Indole-3-carbinol may inhibit the hepatic stellate cell growth by blocking the NADPH oxidase/ROS/p38-MAPK pathway. | [56] |
| Notoamide G | Hepatocellular cancer | Notoamide G triggered a P38/JNK pathway, which resulted in the induction of apoptosis and autophagy | [57] |
| Vincristine | Cervical cancer | Vincristine caused a mitotic arrest, and only the cells that were experiencing a mitotic arrest had p38-MAPK active. | [58] |
| Skin cancer | Apoptosis produced by vincristine is JNK/MAPK activation dependent in at least some melanoma cell lines. | [59] | |
| Vinblastine | Cervical cancer | Vinblastine induced mitotic arrest and selectively activated p38-MAPK in mitotically arrested cells. | [58] |
| Sclerotiamides C | Cervical cancer | Sclerotiamide C has been observed to prompt apoptosis in HeLa cells through the mechanisms of cell cycle arrest, ROS production activation, and regulation of proteins related to apoptosis within the MAPK signaling pathway. | [60] |
| Ellipticine | Endometrial cancer | In RL95-2 cells, apoptosis can be induced by ellipticine through ROS and the MAPKs activation | [61] |
| Chaetoglobosin K | Ovarian cancer | Chaetoglobosin K increased P38-MAPK phosphorylation in ovarian cancer cells, causing G2 arrest through cyclin B1 and death | [62] |
| Jerantinine B | Leukemia | Jerantinine B caused cell death, and phospho-kinase arrays revealed increased and activated total and phosphorylated c-Jun/JNK (S63) levels. | [63] |
| Harmalacidine | Leukemia | Harmalacidine’s cytotoxic action targeted mitochondrial and PTKs-Ras/Raf/ERK pathways. | [64] |
| L20 | Leukemia | Through damaging DNA and p38-MAPK pathway modification, L20 caused mitochondrial driven apoptosis and G2/M arrest | [65] |
| 11-Methoxytabersonine | Lung cancer | The autophagy induced by 11-methoxytabersonine was discovered to occur through the activation of JNK signaling systems. | [66] |
| Calothrixin A | Lung cancer | Calothrixin A acted against lung cancer by blocking Topo I. This caused the cell cycle to stop and the cells to move, as well as apoptosis and autophagy through the PI3K/Akt/JNK/p53 pathway. | [67] |
| Harmol | Lung cancer | MEK/ERK inhibitor U0126 stopped autophagy in part by blocking the ERK1/2 pathway. | [68] |
| Chaetoglobosin G | Lung cancer | Chaetoglobosin G clearly stopped the growth of A549 cells, and it may have done this by causing autophagy in A549 cells via the ERK pathway to increase the production of P21. | [69] |
| 3α-acetonyltabersonine | Neural cancer | 3α-acetonyltabersonine hindered DNA damage repair, causing MAPK pathway activation and apoptosis | [70] |
| Isomahanine | Oral cancer | Isomahanine has been found to elicit endoplasmic reticulum stress, leading to the activation of both p38 MAPK-mediated apoptosis and autophagy | [71] |
| Dehydrocrenatidine | Oral cacner | The induction of apoptosis by Dehydrocrenatidine was observed through the stimulation of ERK and c-JNK. | [72] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Amin, M.; Emran, T.B.; Khan, J.; Zehravi, M.; Sharma, I.; Patil, A.; Gupta, J.K.; Jeslin, D.; Krishnan, K.; Das, R.; et al. Research Progress of Indole Alkaloids: Targeting MAP Kinase Signaling Pathways in Cancer Treatment. Cancers 2023, 15, 5311. https://doi.org/10.3390/cancers15225311
Al Amin M, Emran TB, Khan J, Zehravi M, Sharma I, Patil A, Gupta JK, Jeslin D, Krishnan K, Das R, et al. Research Progress of Indole Alkaloids: Targeting MAP Kinase Signaling Pathways in Cancer Treatment. Cancers. 2023; 15(22):5311. https://doi.org/10.3390/cancers15225311
Chicago/Turabian StyleAl Amin, Md., Talha Bin Emran, Jishan Khan, Mehrukh Zehravi, Indu Sharma, Anasuya Patil, Jeetendra Kumar Gupta, D. Jeslin, Karthickeyan Krishnan, Rajib Das, and et al. 2023. "Research Progress of Indole Alkaloids: Targeting MAP Kinase Signaling Pathways in Cancer Treatment" Cancers 15, no. 22: 5311. https://doi.org/10.3390/cancers15225311
APA StyleAl Amin, M., Emran, T. B., Khan, J., Zehravi, M., Sharma, I., Patil, A., Gupta, J. K., Jeslin, D., Krishnan, K., Das, R., Nainu, F., Ahmad, I., & Wilairatana, P. (2023). Research Progress of Indole Alkaloids: Targeting MAP Kinase Signaling Pathways in Cancer Treatment. Cancers, 15(22), 5311. https://doi.org/10.3390/cancers15225311