Complications from Stereotactic Body Radiotherapy for Lung Cancer
Abstract
:1. Introduction
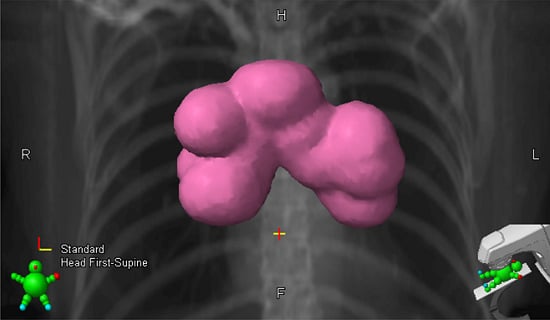
2. Centrally Located Tumors

3. Central Airway Toxicities
4. Esophageal Toxicity
5. Vascular Injury
| Endpoint | Organ | Dosimetric Constraint (Comment) | Study |
|---|---|---|---|
| Vocal Cord Paralysis | Recurrent Laryngeal Nerve (RLN), Vagus Nerve (VN) | Of 12 patients with significant dose to either the RLN or VN, 2 patients developed vocal cord paresis, at a cumulative single fraction equivalent dose (SFED3; α/β = 3 Gy) to VN of 64.5 Gy and 16 Gy and SFED3 to the RLN 15.3 Gy and 19.5 Gy. | Shultz et al., 2014 [34] |
| Aortic Toxicity | Aorta | Recommended dose threshold of 120.0 Gy as a raw dose, 90.0 Gy when dose is corrected for long-term recovery during retreatment interval | Evans et al., 2013 [33] |
| Brachial Plexopathy | Brachial Plexus | Doses >26 Gy in 3–4 fractions resulted in an increased 2 year risk of brachial plexopathy, with similar cutoffs noted for BED >100 Gy3 and SFED-4 >15 Gy | Forquer et al., 2009 [35] |
6. Spontaneous Pneumothorax and Other Pulmonary Toxicities
7. Radiation Pneumonitis
7.1. Dosimetric Predictors of RP
7.2. Diagnostic Predictors of RP
7.3. Patient-Related Predictors
8. Chest Wall and Skin Toxicities
8.1. Chest Wall Pain and Rib Fracture
| Toxicity | Incidence | Timing | Dosimetric Correlates | Study | ||
|---|---|---|---|---|---|---|
| Volume | Dose | Fraction | ||||
| Chest Wall Pain | 30% risk (Range: 10% to 44%) | 12.6 months post-SBRT (Range: 4.3–35.9 months) | 30 cc of chest wall | 30 Gy | 3 (Range:3–5) | Dunlap et al., 2010 [89] Mutter et al., 2012 [84] Creach et al., 2012 [87] |
| Rib Fracture | 5% risk | 19.2 months post-SBRT | 2 cc of rib | 27 Gy | 3 | Pettersson et al., 2009 [88] |
| 50% risk | 2 cc of rib | 50 Gy | 3 | Creach et al., 2012 [87] | ||
| Skin Toxicity | 1.2%–14% | 3–6 weeks post-SBRT | <10 cc volume, volume maximum of 30 Gy | 6 Gy/fraction | 5 | RTOG 0813 [91] Hoppe et al., 2008 [92] |
| maximum point dose of 32 Gy, maximum posterior skin dose ≥50% of actual prescribed dose | 6.4 Gy/fraction | 5 | ||||
8.2. Skin Toxicity
9. Brachial Plexopathy
10. Vagus Nerve Injury
11. Ways to Avoid Complications
11.1. Patient Selection
11.2. Simulation/Motion Management
11.3. Treatment Planning
11.3.1. Dose/Fractionation
| Organ | Endpoint (≥Grade 3) | Dosimetric Constraints | Fractions | Prescription Dose (Gy) | Reference | |
|---|---|---|---|---|---|---|
| Volume | Constraint | |||||
| Esophagus | Stenosis/Fistula | <5 cc | 11.9 Gy | 1 | 34 | RTOG 0915 [112] |
| Max Point Dose | 15.4 Gy | |||||
| Max Point Dose | 27 Gy | 3 | 60 | RTOG 0236 [113] | ||
| <5 cc | 18.8 Gy | 4 | 48 | RTOG 0915 [112] | ||
| Max Point Dose | 30 Gy | |||||
| <5 cc | 27.5 Gy | 5 | 40–60 | RTOG 0813 [91] | ||
| Max Point Dose | 105% of PTV Prescription | |||||
| Brachial Plexus | Neuropathy | <3 cc | 14 Gy | 1 | 34 | RTOG 0915 [112] |
| Max Point Dose | 17.5 Gy | |||||
| Max Point Dose | 24 Gy | 3 | 60 | RTOG 0236 [113] | ||
| <3 cc | 23.6 Gy | 4 | 48 | RTOG 0915 [112] | ||
| Max Point Dose | 27.2 Gy | |||||
| <3 cc | 30 Gy | 5 | 40–60 | RTOG 0813 [91] | ||
| Max Point Dose | 32 Gy | |||||
| Great Vessels | Aneurysm | <10 cc | 31 Gy | 1 | 34 | RTOG 0915 [112] |
| Max Point Dose | 37 Gy | |||||
| <10 cc | 43 Gy | 4 | 48 | RTOG 0915 [112] | ||
| Max Point Dose | 49 Gy | |||||
| <10 cc | 47 Gy | 5 | 40–60 | RTOG 0813 [91] | ||
| Max Point Dose | 105% of PTV Prescription | |||||
| Trachea and Large Bronchus | Stenosis/Fistula | <4 cc | 10.5 Gy | 1 | 34 | RTOG 0915 [112] |
| Max Point Dose | 20.2 Gy | |||||
| Max Point Dose | 30 Gy | 3 | 60 | RTOG 0236 [113] | ||
| <4 cc | 15.6 Gy | 4 | 48 | RTOG 0915 [112] | ||
| Max Point Dose | 34.8 Gy | |||||
| <4 cc | 18 Gy | 5 | 40–60 | RTOG 0813 [91] | ||
| Max Point Dose | 105% of PTV Prescription | |||||
| Rib | Pain or Fracture | <1 cc | 22 Gy | 1 | 34 | RTOG 0915 [112] |
| Max Point Dose | 30 Gy | |||||
| <1 cc | 32 Gy | 4 | 48 | RTOG 0915 [112] | ||
| Max Point Dose | 40 Gy | |||||
| Skin | Ulceration | <10 cc | 23 Gy | 1 | 34 | RTOG 0915 [112] |
| Max Point Dose | 26 Gy | |||||
| <10 cc | 33.2 Gy | 4 | 48 | RTOG 0915 [112] | ||
| Max Point Dose | 40 Gy | |||||
| <10 cc | 30 Gy | 5 | 40–60 | RTOG 0813 [91] | ||
| Max Point Dose | 32 Gy | |||||
| Lung | Basic Lung Function | 1500 cc | 7 Gy | 1 | 34 | RTOG 0915 [112] |
| 1500 cc | 11.6 Gy | 4 | 48 | RTOG 0915 [112] | ||
| 1500 cc | 12.5 Gy | 5 | 40–60 | RTOG 0813 [91] | ||
| Pneumonitis | 1000 cc | 7.4 Gy | 1 | 34 | RTOG 0915 [112] | |
| 1000 cc | 12.4 Gy | 4 | 48 | RTOG 0915 [112] | ||
| 1000 cc | 13.5 Gy | 5 | 40–60 | RTOG 0813 [91] | ||
11.3.2. Target Delineation
11.3.3. Plan Optimization/Beam Arrangement/Weighting
11.3.4. Treatment Delivery
12. Conclusions
Author Contributions
Conflicts of Interest
References
- Senan, S. Stereotactic body radiotherapy: Do central lung tumors still represent a “no-fly zone”? Onkologie 2012, 35, 406–407. [Google Scholar] [CrossRef] [PubMed]
- Haffty, B.G.; Goldberg, N.B.; Gerstley, J.; Fischer, D.B.; Peschel, R.E. Results of radical radiation therapy in clinical stage I, technically operable non-small cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 1988, 15, 69–73. [Google Scholar] [CrossRef]
- Gauden, S.; Ramsay, J.; Tripcony, L. The curative treatment by radiotherapy alone of stage I non-small cell carcinoma of the lung. Chest 1995, 108, 1278–1282. [Google Scholar] [CrossRef] [PubMed]
- Fang, L.C.; Komaki, R.; Allen, P.; Guerrero, T.; Mohan, R.; Cox, J.D. Comparison of outcomes for patients with medically inoperable stage I non-small-cell lung cancer treated with two-dimensional vs. Three-dimensional radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2006, 66, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Rosenzweig, K.E.; Fox, J.L.; Yorke, E.; Amols, H.; Jackson, A.; Rusch, V.; Kris, M.G.; Ling, C.C.; Leibel, S.A. Results of a phase I dose-escalation study using three-dimensional conformal radiotherapy in the treatment of inoperable nonsmall cell lung carcinoma. Cancer 2005, 103, 2118–2127. [Google Scholar] [CrossRef] [PubMed]
- Bradley, J.; Graham, M.V.; Winter, K.; Purdy, J.A.; Komaki, R.; Roa, W.H.; Ryu, J.K.; Bosch, W.; Emami, B. Toxicity and outcome results of rtog 9311: A phase I–II dose-escalation study using three-dimensional conformal radiotherapy in patients with inoperable non-small-cell lung carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2005, 61, 318–328. [Google Scholar] [CrossRef] [PubMed]
- Narayan, S.; Henning, G.T.; Ten Haken, R.K.; Sullivan, M.A.; Martel, M.K.; Hayman, J.A. Results following treatment to doses of 92.4 or 102.9 gy on a phase I dose escalation study for non-small cell lung cancer. Lung Cancer 2004, 44, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Barriger, R.B.; Forquer, J.A.; Brabham, J.G.; Andolino, D.L.; Shapiro, R.H.; Henderson, M.A.; Johnstone, P.A.; Fakiris, A.J. A dose-volume analysis of radiation pneumonitis in non-small cell lung cancer patients treated with stereotactic body radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Timmerman, R.; Papiez, L.; McGarry, R.; Likes, L.; DesRosiers, C.; Frost, S.; Williams, M. Extracranial stereotactic radioablation: Results of a phase I study in medically inoperable stage I non-small cell lung cancer. Chest 2003, 124, 1946–1955. [Google Scholar] [CrossRef] [PubMed]
- Timmerman, R.; McGarry, R.; Yiannoutsos, C.; Papiez, L.; Tudor, K.; DeLuca, J.; Ewing, M.; Abdulrahman, R.; DesRosiers, C.; Williams, M.; et al. Excessive toxicity when treating central tumors in a phase II study of stereotactic body radiation therapy for medically inoperable early-stage lung cancer. J. Clin. Oncol. 2006, 24, 4833–4839. [Google Scholar] [CrossRef] [PubMed]
- Amini, A.; Yeh, N.; Gaspar, L.E.; Kavanagh, B.; Karam, S.D. Stereotactic body radiation therapy (sbrt) for lung cancer patients previously treated with conventional radiotherapy: A review. Radiat. Oncol. 2014, 9. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Schipper, M.; Kidwell, K.; Lin, J.; Reddy, R.; Ren, Y.; Chang, A.; Lv, F.; Orringer, M.; Spring Kong, F.M. Survival outcome after stereotactic body radiation therapy and surgery for stage I non-small cell lung cancer: A meta-analysis. Int. J. Radiat. Oncol. Biol. Phys. 2014, 90, 603–611. [Google Scholar] [CrossRef] [PubMed]
- Crabtree, T.D.; Denlinger, C.E.; Meyers, B.F.; El Naqa, I.; Zoole, J.; Krupnick, A.S.; Kreisel, D.; Patterson, G.A.; Bradley, J.D. Stereotactic body radiation therapy versus surgical resection for stage I non-small cell lung cancer. J. Thorac. Cardiovasc. Surg. 2010, 140, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Lo, S.S.; Fakiris, A.J.; Chang, E.L.; Mayr, N.A.; Wang, J.Z.; Papiez, L.; Teh, B.S.; McGarry, R.C.; Cardenes, H.R.; Timmerman, R.D. Stereotactic body radiation therapy: A novel treatment modality. Nat. Rev. Clin. Oncol. 2010, 7, 44–54. [Google Scholar] [CrossRef] [PubMed]
- Fakiris, A.J.; McGarry, R.C.; Yiannoutsos, C.T.; Papiez, L.; Williams, M.; Henderson, M.A.; Timmerman, R. Stereotactic body radiation therapy for early-stage non-small-cell lung carcinoma: Four-year results of a prospective phase ii study. Int. J. Radiat. Oncol. Biol. Phys. 2009, 75, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Song, S.Y.; Choi, W.; Shin, S.S.; Lee, S.W.; Ahn, S.D.; Kim, J.H.; Je, H.U.; Park, C.I.; Lee, J.S.; Choi, E.K. Fractionated stereotactic body radiation therapy for medically inoperable stage I lung cancer adjacent to central large bronchus. Lung Cancer 2009, 66, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Le, Q.-T.; Loo, B.W.; Ho, A.; Cotrutz, C.; Koong, A.C.; Wakelee, H.; Kee, S.T.; Constantinescu, D.; Whyte, R.I.; Donington, J. Results of a phase I dose-escalation study using single-fraction stereotactic radiotherapy for lung tumors. J. Thorac. Oncol. 2006, 1, 802–809. [Google Scholar] [CrossRef] [PubMed]
- Kelsey, C.R.; Kahn, D.; Hollis, D.R.; Miller, K.L.; Zhou, S.M.; Clough, R.W.; Marks, L.B. Radiation-induced narrowing of the tracheobronchial tree: An in-depth analysis. Lung Cancer 2006, 52, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Speiser, B.L.; Spratling, L. Radiation bronchitis and stenosis secondary to high dose rate endobronchial irradiation. Int. J. Radiat. Oncol. Biol. Phys. 1993, 25, 589–597. [Google Scholar] [CrossRef]
- Karlsson, K.; Nyman, J.; Baumann, P.; Wersall, P.; Drugge, N.; Gagliardi, G.; Johansson, K.A.; Persson, J.O.; Rutkowska, E.; Tullgren, O.; et al. Retrospective cohort study of bronchial doses and radiation-induced atelectasis after stereotactic body radiation therapy of lung tumors located close to the bronchial tree. Int. J. Radiat. Oncol. Biol. Phys. 2013, 87, 590–595. [Google Scholar] [CrossRef] [PubMed]
- Rowe, B.P.; Boffa, D.J.; Wilson, L.D.; Kim, A.W.; Detterbeck, F.C.; Decker, R.H. Stereotactic body radiotherapy for central lung tumors. J. Thorac. Oncol. 2012, 7, 1394–1399. [Google Scholar] [CrossRef] [PubMed]
- Corradetti, M.N.; Haas, A.R.; Rengan, R. Central-airway necrosis after stereotactic body-radiation therapy. N. Engl. J. Med. 2012, 366, 2327–2329. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.J.; Williams, E.; Modh, A.; Foster, A.; Yorke, E.; Rimner, A.; Jackson, A. Dosimetric predictors of esophageal toxicity after stereotactic body radiotherapy for central lung tumors. Radiother. Oncol. 2014, 112, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Onimaru, R.; Shirato, H.; Shimizu, S.; Kitamura, K.; Xu, B.; Fukumoto, S.; Chang, T.C.; Fujita, K.; Oita, M.; Miyasaka, K.; et al. Tolerance of organs at risk in small-volume, hypofractionated, image-guided radiotherapy for primary and metastatic lung cancers. Int. J. Radiat. Oncol. Biol. Phys. 2003, 56, 126–135. [Google Scholar] [CrossRef]
- Palma, D.A.; Senan, S.; Oberije, C.; Belderbos, J.; de Dios, N.R.; Bradley, J.D.; Barriger, R.B.; Moreno-Jimenez, M.; Kim, T.H.; Ramella, S.; et al. Predicting esophagitis after chemoradiation therapy for non-small cell lung cancer: An individual patient data meta-analysis. Int. J. Radiat. Oncol. Biol. Phys. 2013, 87, 690–696. [Google Scholar] [CrossRef] [PubMed]
- Gomez, D.R.; Hunt, M.A.; Jackson, A.; O’Meara, W.P.; Bukanova, E.N.; Zelefsky, M.J.; Yamada, Y.; Rosenzweig, K.E. Low rate of thoracic toxicity in palliative paraspinal single-fraction stereotactic body radiation therapy. Radiother. Oncol. 2009, 93, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Timmerman, R.D. An overview of hypofractionation and introduction to this issue of seminars in radiation oncology. Semin. Radiat. Oncol. 2008, 18, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Abelson, J.A.; Murphy, J.D.; Loo, B.W., Jr.; Chang, D.T.; Daly, M.E.; Wiegner, E.A.; Hancock, S.; Chang, S.D.; Le, Q.T.; Soltys, S.G.; et al. Esophageal tolerance to high-dose stereotactic ablative radiotherapy. Dis. Esophagus 2012, 25, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Werner-Wasik, M.; Pequignot, E.; Leeper, D.; Hauck, W.; Curran, W. Predictors of severe esophagitis include use of concurrent chemotherapy, but not the length of irradiated esophagus: A multivariate analysis of patients with lung cancer treated with nonoperative therapy. Int. J. Radiat. Oncol. Biol. Phys. 2000, 48, 689–696. [Google Scholar] [CrossRef]
- Scappaticci, F.A.; Fehrenbacher, L.; Cartwright, T.; Hainsworth, J.D.; Heim, W.; Berlin, J.; Kabbinavar, F.; Novotny, W.; Sarkar, S.; Hurwitz, H. Surgical wound healing complications in metastatic colorectal cancer patients treated with bevacizumab. J. Surg Oncol. 2005, 91, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Goodgame, B.; Veeramachaneni, N.; Patterson, A.; Govindan, R. Tracheo-esophageal fistula with bevacizumab after mediastinal radiation. J. Thorac. Oncol. 2008, 3, 1080–1081. [Google Scholar] [CrossRef] [PubMed]
- NCT02319889: Pilot Study of SBRT Plus Chemotherapy for Non-Small Cell Lung Carcinoma. Available online: https://clinicaltrials.gov/ct2/show/NCT02319889 (accessed on 3 January 2015).
- Evans, J.; Gomez, D.; Amini, A.; Rebueno, N.; Allen, P.; Martel, M.; Rineer, J.; Ang, K.; McAvoy, S.; Cox, J.; et al. Aortic dose constraints when reirradiating thoracic tumors. Radiother. Oncol. 2013, 106, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Shultz, D.B.; Trakul, N.; Maxim, P.G.; Diehn, M.; Loo, B.W., Jr. Vagal and recurrent laryngeal neuropathy following stereotactic ablative radiation therapy in the chest. Pract. Radiat.Oncol. 2014, 4, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Forquer, J.A.; Fakiris, A.J.; Timmerman, R.D.; Lo, S.S.; Perkins, S.M.; McGarry, R.C.; Johnstone, P.A. Brachial plexopathy from stereotactic body radiotherapy in early-stage NSCLC: Dose-limiting toxicity in apical tumor sites. Radiother. Oncol. 2009, 93, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Ito, M.; Niho, S.; Nihei, K.; Yoh, K.; Ohmatsu, H.; Ohe, Y. Risk factors associated with fatal pulmonary hemorrhage in locally advanced non-small cell lung cancer treated with chemoradiotherapy. BMC Cancer 2012, 12. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-H.; Kim, E.-Y.; Ban, H.-J.; Oh, I.-J.; Kim, K.-S.; Kim, Y.-C.; Ahn, S.-J. Risk factors for fatal hemoptysis after concurrent chemoradiation therapy in patients with non-small cell lung carcinoma. Chonnam Med. J. 2010, 46, 19–24. [Google Scholar] [CrossRef]
- Reck, M.; Barlesi, F.; Crino, L.; Henschke, C.I.; Isla, D.; Stiebeler, S.; Spigel, D.R. Predicting and managing the risk of pulmonary haemorrhage in patients with nsclc treated with bevacizumab: A consensus report from a panel of experts. Ann. Oncol. 2012, 23, 1111–1120. [Google Scholar] [CrossRef] [PubMed]
- Chi, A.; Nguyen, N.P.; Komaki, R. The potential role of respiratory motion management and image guidance in the reduction of severe toxicities following stereotactic ablative radiation therapy for patients with centrally located early stage non-small cell lung cancer or lung metastases. Front. Oncol. 2014, 4. [Google Scholar] [CrossRef] [PubMed]
- Milano, M.T.; Chen, Y.; Katz, A.W.; Philip, A.; Schell, M.C.; Okunieff, P. Central thoracic lesions treated with hypofractionated stereotactic body radiotherapy. Radiother. Oncol. 2009, 91, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Oshiro, Y.; Aruga, T.; Tsuboi, K.; Marino, K.; Hara, R.; Sanayama, Y.; Itami, J. Stereotactic body radiotherapy for lung tumors at the pulmonary hilum. Strahlenther. Onkol. 2010, 186, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Ohnishi, K.; Shioyama, Y.; Nomoto, S.; Sasaki, T.; Ohga, S.; Yoshitake, T.; Toba, T.; Atsumi, K.; Shiinoki, T.; Terashima, H.; et al. Spontaneous pneumothorax after stereotactic radiotherapy for non-small-cell lung cancer. Jpn. J. Radiol. 2009, 27, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Pezner, R.D.; Horak, D.A.; Sayegh, H.O.; Lipsett, J.A. Spontaneous pneumothorax in patients irradiated for hodgkin’s disease and other malignant lymphomas. Int. J. Radiat. Oncol. Biol. Phys. 1990, 18, 193–198. [Google Scholar] [CrossRef]
- Stephans, K.L.; Djemil, T.; Reddy, C.A.; Gajdos, S.M.; Kolar, M.; Machuzak, M.; Mazzone, P.; Videtic, G.M.M. Comprehensive analysis of pulmonary function test (pft) changes after stereotactic body radiotherapy (sbrt) for stage I lung cancer in medically inoperable patients. J. Thorac. Oncol. 2009, 4, 838–844. [Google Scholar] [CrossRef] [PubMed]
- Henderson, M.; McGarry, R.; Yiannoutsos, C.; Fakiris, A.; Hoopes, D.; Williams, M.; Timmerman, R. Baseline pulmonary function as a predictor for survival and decline in pulmonary function over time in patients undergoing stereotactic body radiotherapy for the treatment of stage i non-small-cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2008, 72, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Guckenberger, M.; Kestin, L.L.; Hope, A.J.; Belderbos, J.; Werner-Wasik, M.; Yan, D.; Sonke, J.-J.; Bissonnette, J.P.; Wilbert, J.; Xiao, Y.; et al. Is there a lower limit of pretreatment pulmonary function for safe and effective stereotactic body radiotherapy for early-stage non-small cell lung cancer? J. Thorac. Oncol. 2012, 7, 542–551. [Google Scholar] [CrossRef] [PubMed]
- Ohashi, T.; Takeda, A.; Shigematsu, N.; Kunieda, E.; Ishizaka, A.; Fukada, J.; Deloar, H.M.; Kawaguchi, O.; Takeda, T.; Takemasa, K.; et al. Differences in pulmonary function before vs. 1 year after hypofractionated stereotactic radiotherapy for small peripheral lung tumors. Int. J. Radiat. Oncol. Biol. Phys. 2005, 62, 1003–1008. [Google Scholar] [CrossRef] [PubMed]
- Takeda, A.; Enomoto, T.; Sanuki, N.; Handa, H.; Aoki, Y.; Oku, Y.; Kunieda, E. Reassessment of declines in pulmonary function ≥1 year after stereotactic body radiotherapy. Chest 2013, 143, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Stanic, S.; Paulus, R.; Timmerman, R.D.; Michalski, J.; Barriger, R.B.; Bezjak, A.; Videtic, G.M.; Bradley, J. No clinically significant changes in pulmonary function following stereotactic body radiation therapy (sbrt) among medically inoperable patients with early stage peripheral non-small cell lung cancer: An analysis of RTOG 0236. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84. [Google Scholar] [CrossRef]
- Seppenwoolde, Y.; De Jaeger, K.; Boersma, L.J.; Belderbos, J.S.A.; Lebesque, J.V. Regional differences in lung radiosensitivity after radiotherapy for non–small-cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2004, 60, 748–758. [Google Scholar] [CrossRef] [PubMed]
- Tucker, S.L.; Jin, H.; Wei, X.; Wang, S.; Martel, M.K.; Komaki, R.; Liu, H.H.; Mohan, R.; Chen, Y.; Cox, J.D.; et al. Impact of toxicity grade and scoring system on the relationship between mean lung dose and risk of radiation pneumonitis in a large cohort of patients with non–small cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2010, 77, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Nagata, Y.; Takayama, K.; Matsuo, Y.; Norihisa, Y.; Mizowaki, T.; Sakamoto, T.; Sakamoto, M.; Mitsumori, M.; Shibuya, K.; Araki, N.; et al. Clinical outcomes of a phase I/II study of 48 gy of stereotactic body radiotherapy in 4 fractions for primary lung cancer using a stereotactic body frame. Int. J. Radiat. Oncol. Biol. Phys. 2005, 63, 1427–1431. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, H.; Nakagawa, K.; Nakamura, N.; Koyanagi, H.; Tago, M.; Igaki, H.; Shiraishi, K.; Sasano, N.; Ohtomo, K. Exceptionally high incidence of symptomatic grade 2–5 radiation pneumonitis after stereotactic radiation therapy for lung tumors. Radiat. Oncol. 2007, 2. [Google Scholar] [CrossRef]
- Guckenberger, M.; Heilman, K.; Wulf, J.; Mueller, G.; Beckmann, G.; Flentje, M. Pulmonary injury and tumor response after stereotactic body radiotherapy (sbrt): Results of a serial follow-up ct study. Radiother. Oncol. 2007, 85, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, F.B.; Geinitz, H.; Schill, S.; Thamm, R.; Nieder, C.; Schratzenstaller, U.; Molls, M. Stereotactic hypofractionated radiotherapy in stage I (t1-2 n0 m0) non-small-cell lung cancer (nsclc). Acta Oncol. 2006, 45, 796–801. [Google Scholar] [CrossRef] [PubMed]
- Guckenberger, M.; Baier, K.; Polat, B.; Richter, A.; Krieger, T.; Wilbert, J.; Mueller, G.; Flentje, M. Dose-response relationship for radiation-induced pneumonitis after pulmonary stereotactic body radiotherapy. Radiother. Oncol. 2010, 97, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Lo, S.S.; Sahgal, A.; Chang, E.L.; Mayr, N.A.; Teh, B.S.; Huang, Z.; Schefter, T.E.; Yao, M.; Machtay, M.; Slotman, B.J.; et al. Serious complications associated with stereotactic ablative radiotherapy and strategies to mitigate the risk. Clin. Oncol. (R. Coll. Radiol.) 2013, 25, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Borst, G.R.; Ishikawa, M.; Nijkamp, J.; Hauptmann, M.; Shirato, H.; Onimaru, R.; van den Heuvel, M.M.; Belderbos, J.; Lebesque, J.V.; Sonke, J.J. Radiation pneumonitis in patients treated for malignant pulmonary lesions with hypofractionated radiation therapy. Radiother. Oncol. 2009, 91, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Ong, C.L.; Palma, D.; Verbakel, W.F.; Slotman, B.J.; Senan, S. Treatment of large stage I–II lung tumors using stereotactic body radiotherapy (SBRT): Planning considerations and early toxicity. Radiother. Oncol. 2010, 97, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Kyas, I.; Hof, H.; Debus, J.; Schlegel, W.; Karger, C.P. Prediction of radiation-induced changes in the lung after stereotactic body radiation therapy of non-small-cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2007, 67, 768–774. [Google Scholar] [CrossRef] [PubMed]
- Hope, A.J.; Lindsay, P.E.; El Naqa, I.; Alaly, J.R.; Vicic, M.; Bradley, J.D.; Deasy, J.O. Modeling radiation pneumonitis risk with clinical, dosimetric, and spatial parameters. Int. J. Radiat. Oncol. Biol. Phys. 2006, 65, 112–124. [Google Scholar] [CrossRef] [PubMed]
- Yorke, E.D.; Jackson, A.; Rosenzweig, K.E.; Merrick, S.A.; Gabrys, D.; Venkatraman, E.S.; Burman, C.M.; Leibel, S.A.; Ling, C.C. Dose-volume factors contributing to the incidence of radiation pneumonitis in non-small-cell lung cancer patients treated with three-dimensional conformal radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 2002, 54, 329–339. [Google Scholar] [CrossRef]
- Tucker, S.L.; Liao, Z.X.; Travis, E.L. Estimation of the spatial distribution of target cells for radiation pneumonitis in mouse lung. Int. J. Radiat. Oncol. Biol. Phys. 1997, 38, 1055–1066. [Google Scholar] [CrossRef]
- West, J.B. Respiratory Physiology: The Essentials; Wolters Kluwer Health/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2012. [Google Scholar]
- Matsuo, Y.; Shibuya, K.; Nakamura, M.; Narabayashi, M.; Sakanaka, K.; Ueki, N.; Miyagi, K.; Norihisa, Y.; Mizowaki, T.; Nagata, Y.; et al. Dose-volume metrics associated with radiation pneumonitis after stereotactic body radiation therapy for lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2012, 83, e545–e549. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, H.; Kobayashi-Shibata, S.; Terahara, A.; Okuma, K.; Haga, A.; Wakui, R.; Ohtomo, K.; Nakagawa, K. Prescreening based on the presence of ct-scan abnormalities and biomarkers (kl-6 and sp-d) may reduce severe radiation pneumonitis after stereotactic radiotherapy. Radiat. Oncol. 2010, 5. [Google Scholar] [CrossRef]
- Iwata, H.; Shibamoto, Y.; Baba, F.; Sugie, C.; Ogino, H.; Murata, R.; Yanagi, T.; Otsuka, S.; Kosaki, K.; Murai, T.; et al. Correlation between the serum kl-6 level and the grade of radiation pneumonitis after stereotactic body radiotherapy for stage i lung cancer or small lung metastasis. Radiother. Oncol. 2011, 101, 267–270. [Google Scholar] [CrossRef] [PubMed]
- Kong, F.M.; Ao, X.; Wang, L.; Lawrence, T.S. The use of blood biomarkers to predict radiation lung toxicity: A potential strategy to individualize thoracic radiation therapy. Cancer Control. 2008, 15, 140–150. [Google Scholar] [PubMed]
- Hara, R.; Itami, J.; Komiyama, T.; Katoh, D.; Kondo, T. Serum levels of kl-6 for predicting the occurrence of radiation pneumonitis after stereotactic radiotherapy for lung tumors. Chest 2004, 125, 340–344. [Google Scholar] [CrossRef] [PubMed]
- Takeda, A.; Ohashi, T.; Kunieda, E.; Enomoto, T.; Sanuki, N.; Takeda, T.; Shigematsu, N. Early graphical appearance of radiation pneumonitis correlates with the severity of radiation pneumonitis after stereotactic body radiotherapy (sbrt) in patients with lung tumors. Int. J. Radiat. Oncol. Biol. Phys. 2010, 77, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, S.; Ohguri, T.; Ide, S.; Aoki, T.; Imada, H.; Yahara, K.; Narisada, H.; Korogi, Y. Stereotactic body radiotherapy for lung tumors in patients with subclinical interstitial lung disease: The potential risk of extensive radiation pneumonitis. Lung Cancer 2013, 82, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Palma, D.; Lagerwaard, F.; Rodrigues, G.; Haasbeek, C.; Senan, S. Curative treatment of stage I non-small-cell lung cancer in patients with severe copd: Stereotactic radiotherapy outcomes and systematic review. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, 1149–1156. [Google Scholar] [CrossRef] [PubMed]
- Kimura, T.; Matsuura, K.; Murakami, Y.; Hashimoto, Y.; Kenjo, M.; Kaneyasu, Y.; Wadasaki, K.; Hirokawa, Y.; Ito, K.; Okawa, M. Ct appearance of radiation injury of the lung and clinical symptoms after stereotactic body radiation therapy (SBRT) for lung cancers: Are patients with pulmonary emphysema also candidates for sbrt for lung cancers? Int. J. Radiat. Oncol. Biol. Phys. 2006, 66, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.; Tucker, S.L.; Liu, H.H.; Wei, X.; Yom, S.S.; Wang, S.; Komaki, R.; Chen, Y.; Martel, M.K.; Mohan, R.; et al. Dose-volume thresholds and smoking status for the risk of treatment-related pneumonitis in inoperable non-small cell lung cancer treated with definitive radiotherapy. Radiother. Oncol. 2009, 91, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Takeda, A.; Kunieda, E.; Ohashi, T.; Aoki, Y.; Oku, Y.; Enomoto, T.; Nomura, K.; Sugiura, M. Severe COPD is correlated with mild radiation pneumonitis following stereotactic body radiotherapy. Chest 2012, 141, 858–866. [Google Scholar] [CrossRef] [PubMed]
- Bjermer, L.; Cai, Y.; Nilsson, K.; Hellstrom, S.; Henriksson, R. Tobacco smoke exposure suppresses radiation-induced inflammation in the lung: A study of bronchoalveolar lavage and ultrastructural morphology in the rat. Eur. Respir. J. 1993, 6, 1173–1180. [Google Scholar]
- Bhattathiri, V.N. Possible role of plasma GSH in modulating smoking related radiation pneumonitis. Radiother. Oncol. 1999, 51, 291–292. [Google Scholar] [PubMed]
- Takeda, A.; Ohashi, T.; Kunieda, E.; Sanuki, N.; Enomoto, T.; Takeda, T.; Oku, Y.; Shigematsu, N. Comparison of clinical, tumour-related and dosimetric factors in grade 0–1, grade 2 and grade 3 radiation pneumonitis after stereotactic body radiotherapy for lung tumours. Br. J. Radiol. 2012, 85, 636–642. [Google Scholar] [CrossRef] [PubMed]
- Stephans, K.L.; Djemil, T.; Reddy, C.A.; Gajdos, S.M.; Kolar, M.; Mason, D.; Murthy, S.; Rice, T.W.; Mazzone, P.; Machuzak, M.; et al. A comparison of two stereotactic body radiation fractionation schedules for medically inoperable stage I non-small cell lung cancer: The cleveland clinic experience. J. Thorac. Oncol. 2009, 4, 976–982. [Google Scholar] [CrossRef] [PubMed]
- Andolino, D.L.; Forquer, J.A.; Henderson, M.A.; Barriger, R.B.; Shapiro, R.H.; Brabham, J.G.; Johnstone, P.A.; Cardenes, H.R.; Fakiris, A.J. Chest wall toxicity after stereotactic body radiotherapy for malignant lesions of the lung and liver. Int. J. Radiat. Oncol. Biol. Phys. 2011, 80, 692–697. [Google Scholar] [CrossRef] [PubMed]
- Stephans, K.L.; Djemil, T.; Tendulkar, R.D.; Robinson, C.G.; Reddy, C.A.; Videtic, G.M. Prediction of chest wall toxicity from lung stereotactic body radiotherapy (SBRT). Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, 974–980. [Google Scholar] [CrossRef] [PubMed]
- Welsh, J.; Thomas, J.; Shah, D.; Allen, P.K.; Wei, X.; Mitchell, K.; Gao, S.; Balter, P.; Komaki, R.; Chang, J.Y. Obesity increases the risk of chest wall pain from thoracic stereotactic body radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Voroney, J.P.; Hope, A.; Dahele, M.R.; Purdie, T.G.; Franks, K.N.; Pearson, S.; Cho, J.B.; Sun, A.; Payne, D.G.; Bissonnette, J.P.; et al. Chest wall pain and rib fracture after stereotactic radiotherapy for peripheral non-small cell lung cancer. J. Thorac. Oncol. 2009, 4, 1035–1037. [Google Scholar] [CrossRef] [PubMed]
- Mutter, R.W.; Liu, F.; Abreu, A.; Yorke, E.; Jackson, A.; Rosenzweig, K.E. Dose-volume parameters predict for the development of chest wall pain after stereotactic body radiation for lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, 1783–1790. [Google Scholar] [CrossRef] [PubMed]
- Fajardo, L.F.; Berthrong, M.; Anderson, R.E. Musculoskeletal system. In Radiation Pathology; Oxford University Press: New York, NY, USA, 2001; pp. 365–377. [Google Scholar]
- Bongers, E.M.; Haasbeek, C.J.; Lagerwaard, F.J.; Slotman, B.J.; Senan, S. Incidence and risk factors for chest wall toxicity after risk-adapted stereotactic radiotherapy for early-stage lung cancer. J. Thorac. Oncol. 2011, 6, 2052–2057. [Google Scholar] [CrossRef] [PubMed]
- Creach, K.M.; El Naqa, I.; Bradley, J.D.; Olsen, J.R.; Parikh, P.J.; Drzymala, R.E.; Bloch, C.; Robinson, C.G. Dosimetric predictors of chest wall pain after lung stereotactic body radiotherapy. Radiother. Oncol. 2012, 104, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Pettersson, N.; Nyman, J.; Johansson, K.A. Radiation-induced rib fractures after hypofractionated stereotactic body radiation therapy of non-small cell lung cancer: A dose- and volume-response analysis. Radiother. Oncol. 2009, 91, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Dunlap, N.E.; Cai, J.; Biedermann, G.B.; Yang, W.; Benedict, S.H.; Sheng, K.; Schefter, T.E.; Kavanagh, B.D.; Larner, J.M. Chest wall volume receiving >30 gy predicts risk of severe pain and/or rib fracture after lung stereotactic body radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, 796–801. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Swanick, C.W.; Allen, P.K.; Gomez, D.R.; Welsh, J.W.; Liao, Z.; Balter, P.A.; Chang, J.Y. Stereotactic ablative radiotherapy (SABR) using 70 gy in 10 fractions for non-small cell lung cancer: Exploration of clinical indications. Radiother. Oncol. 2014, 112, 256–261. [Google Scholar] [CrossRef] [PubMed]
- Radiation Therapy Oncology Group. RTOG 0813: Seamless Phase I/II Study of Stereotactic Lung Radiotherapy (SBRT) for Early Stage, Centrally Located, Non-Small Cell Lung Cancer (NSCLC) in Medically Inoperable Patients. Available online: http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=0813 (accessed on 3 January 2015).
- Hoppe, B.S.; Laser, B.; Kowalski, A.V.; Fontenla, S.C.; Pena-Greenberg, E.; Yorke, E.D.; Lovelock, D.M.; Hunt, M.A.; Rosenzweig, K.E. Acute skin toxicity following stereotactic body radiation therapy for stage i non-small-cell lung cancer: Who’s at risk? Int. J. Radiat. Oncol. Biol. Phys. 2008, 72, 1283–1286. [Google Scholar] [CrossRef] [PubMed]
- Schierle, C.; Winograd, J.M. Radiation-induced brachial plexopathy: Review. Complication without a cure. J. Reconstr. Microsurg. 2004, 20, 149–152. [Google Scholar] [PubMed]
- Ferrante, M.A. Brachial plexopathies: Classification, causes, and consequences. Muscle Nerve 2004, 30, 547–568. [Google Scholar] [CrossRef]
- Amini, A.; Yang, J.; Williamson, R.; McBurney, M.L.; Erasmus, J., Jr.; Allen, P.K.; Karhade, M.; Komaki, R.; Liao, Z.; Gomez, D.; et al. Dose constraints to prevent radiation-induced brachial plexopathy in patients treated for lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, e391–e398. [Google Scholar] [CrossRef] [PubMed]
- Kori, S.H.; Foley, K.M.; Posner, J.B. Brachial plexus lesions in patients with cancer: 100 cases. Neurology 1981, 31, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.Y.; Li, Q.Q.; Xu, Q.Y.; Allen, P.K.; Rebueno, N.; Gomez, D.R.; Balter, P.; Komaki, R.; Mehran, R.; Swisher, S.G.; et al. Stereotactic ablative radiation therapy for centrally located early stage or isolated parenchymal recurrences of non-small cell lung cancer: How to fly in a “no fly zone”. Int. J. Radiat. Oncol. Biol. Phys. 2014, 88, 1120–1128. [Google Scholar] [CrossRef] [PubMed]
- Lo, S.S.; Fakiris, A.J.; Wang, J.Z.; Mayr, N.A. In regard to Hoppe et al. (Int. J Radiat. Oncol. Biol. Phys. 2008;72:1283–1286). Int. J. Radiat. Oncol. Biol. Phys. 2009, 74, 977. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhong, R.; Bai, S.; Xu, Q.; Zhao, Y.; Wang, J.; Jiang, X.; Shen, Y.; Xu, F.; Wei, Y. Lung tumor reproducibility with active breath control (ABC) in image-guided radiotherapy based on cone-beam computed tomography with two registration methods. Radiother. Oncol. 2011, 99, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Guckenberger, M.; Kavanagh, A.; Webb, S.; Brada, M. A novel respiratory motion compensation strategy combining gated beam delivery and mean target position concept—A compromise between small safety margins and long duty cycles. Radiother. Oncol. 2011, 98, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Taremi, M.; Hope, A.; Dahele, M.; Pearson, S.; Fung, S.; Purdie, T.; Brade, A.; Cho, J.; Sun, A.; Bissonnette, J.P.; et al. Stereotactic body radiotherapy for medically inoperable lung cancer: Prospective, single-center study of 108 consecutive patients. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Onishi, H.; Araki, T.; Shirato, H.; Nagata, Y.; Hiraoka, M.; Gomi, K.; Yamashita, T.; Niibe, Y.; Karasawa, K.; Hayakawa, K.; et al. Stereotactic hypofractionated high-dose irradiation for stage I nonsmall cell lung carcinoma: Clinical outcomes in 245 subjects in a japanese multiinstitutional study. Cancer 2004, 101, 1623–1631. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.Y.; Balter, P.A.; Dong, L.; Yang, Q.; Liao, Z.; Jeter, M.; Bucci, M.K.; McAleer, M.F.; Mehran, R.J.; Roth, J.A.; et al. Stereotactic body radiation therapy in centrally and superiorly located stage I or isolated recurrent non-small-cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2008, 72, 967–971. [Google Scholar] [CrossRef] [PubMed]
- Nuyttens, J.J.; van der Voort van Zyp, N.C.; Praag, J.; Aluwini, S.; van Klaveren, R.J.; Verhoef, C.; Pattynama, P.M.; Hoogeman, M.S. Outcome of four-dimensional stereotactic radiotherapy for centrally located lung tumors. Radiother. Oncol. 2012, 102, 383–387. [Google Scholar] [CrossRef] [PubMed]
- Lagerwaard, F.J.; Haasbeek, C.J.; Smit, E.F.; Slotman, B.J.; Senan, S. Outcomes of risk-adapted fractionated stereotactic radiotherapy for stage I non-small-cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2008, 70, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Onishi, H.; Shirato, H.; Nagata, Y.; Hiraoka, M.; Fujino, M.; Gomi, K.; Niibe, Y.; Karasawa, K.; Hayakawa, K.; Takai, Y.; et al. Hypofractionated stereotactic radiotherapy (hypofxsrt) for stage I non-small cell lung cancer: Updated results of 257 patients in a japanese multi-institutional study. J. Thorac. Oncol. 2007, 2, S94–S100. [Google Scholar] [CrossRef] [PubMed]
- Uematsu, M.; Shioda, A.; Suda, A.; Fukui, T.; Ozeki, Y.; Hama, Y.; Wong, J.R.; Kusano, S. Computed tomography-guided frameless stereotactic radiotherapy for stage I non-small cell lung cancer: A 5-year experience. Int. J. Radiat. Oncol. Biol. Phys. 2001, 51, 666–670. [Google Scholar] [CrossRef]
- Senan, S.; Haasbeek, N.J.; Smit, E.F.; Lagerwaard, F.J. Stereotactic radiotherapy for centrally located early-stage lung tumors. J. Clin. Oncol. 2007, 25, 464. [Google Scholar] [CrossRef] [PubMed]
- Olsen, J.R.; Robinson, C.G.; El Naqa, I.; Creach, K.M.; Drzymala, R.E.; Bloch, C.; Parikh, P.J.; Bradley, J.D. Dose-response for stereotactic body radiotherapy in early-stage non-small-cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, e299–e303. [Google Scholar] [CrossRef] [PubMed]
- Haasbeek, C.J.; Lagerwaard, F.J.; Slotman, B.J.; Senan, S. Outcomes of stereotactic ablative radiotherapy for centrally located early-stage lung cancer. J. Thorac. Oncol. 2011, 6, 2036–2043. [Google Scholar] [CrossRef] [PubMed]
- Guckenberger, M.; Wulf, J.; Mueller, G.; Krieger, T.; Baier, K.; Gabor, M.; Richter, A.; Wilbert, J.; Flentje, M. Dose-response relationship for image-guided stereotactic body radiotherapy of pulmonary tumors: Relevance of 4d dose calculation. Int. J. Radiat. Oncol. Biol. Phys. 2009, 74, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Radiation Therapy Oncology Group. RTOG 0915: A Randomized Phase ii Study Comparing 2 Stereotactic Body Radiation Therapy (SBRT) Schedules for Medically Inoperable Patients with Stage I Peripheral Non-Small Cell Lung Cancer. Available online: http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=0915 (accessed on 3 January 2015).
- Radiation Therapy Oncology Group. RTOG 0236: A Phase II Trial of Stereotactic Body Radiation Therapy (SBRT) in the Treatment of Patients with Medically Inoperable Stage I/II Non-Small Cell Lung Cancer. Available online: http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=0236 (accessed on 3 January 2015).
- Nagata, Y.; Wulf, J.; Lax, I.; Timmerman, R.; Zimmermann, F.; Stojkovski, I.; Jeremic, B. Stereotactic radiotherapy of primary lung cancer and other targets: Results of consultant meeting of the international atomic energy agency. Int. J. Radiat. Oncol. Biol. Phys. 2011, 79, 660–669. [Google Scholar] [CrossRef] [PubMed]
- Verbakel, W.F.; Senan, S.; Cuijpers, J.P.; Slotman, B.J.; Lagerwaard, F.J. Rapid delivery of stereotactic radiotherapy for peripheral lung tumors using volumetric intensity-modulated arcs. Radiother. Oncol. 2009, 93, 122–124. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Fowler, J.F.; Lamond, J.P.; Lanciano, R.; Feng, J.; Brady, L.W. Red shell: Defining a high-risk zone of normal tissue damage in stereotactic body radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 2010, 77, 903–909. [Google Scholar] [CrossRef] [PubMed]
- Dong, P.; Lee, P.; Ruan, D.; Long, T.; Romeijn, E.; Low, D.A.; Kupelian, P.; Abraham, J.; Yang, Y.; Sheng, K. 4pi noncoplanar stereotactic body radiation therapy for centrally located or larger lung tumors. Int. J. Radiat. Oncol. Biol. Phys. 2013, 86, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Prevost, J.B.; Voet, P.; Hoogeman, M.; Praag, J.; Levendag, P.; Nuyttens, J.J. Four-dimensional stereotactic radiotherapy for early stage non-small cell lung cancer: A comparative planning study. Technol. Cancer Res. Treat. 2008, 7, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Chi, A.; Ma, P.; Fu, G.; Hobbs, G.; Welsh, J.S.; Nguyen, N.P.; Jang, S.Y.; Dai, J.; Jin, J.; Komaki, R. Critical structure sparing in stereotactic ablative radiotherapy for central lung lesions: Helical tomotherapy vs. Volumetric modulated arc therapy. PLoS ONE 2013, 8, e59729. [Google Scholar] [CrossRef] [PubMed]
- Prendergast, B.M.; Dobelbower, M.C.; Bonner, J.A.; Popple, R.A.; Baden, C.J.; Minnich, D.J.; Cerfolio, R.J.; Spencer, S.A.; Fiveash, J.B. Stereotactic body radiation therapy (SBRT) for lung malignancies: Preliminary toxicity results using a flattening filter-free linear accelerator operating at 2400 monitor units per minute. Radiat. Oncol. 2013, 8. [Google Scholar] [CrossRef]
- Kragl, G.; Baier, F.; Lutz, S.; Albrich, D.; Dalaryd, M.; Kroupa, B.; Wiezorek, T.; Knoos, T.; Georg, D. Flattening filter free beams in sbrt and imrt: Dosimetric assessment of peripheral doses. Z. Med. Phys. 2011, 21, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Trakul, N.; Chang, C.N.; Harris, J.; Chapman, C.; Rao, A.; Shen, J.; Quinlan-Davidson, S.; Filion, E.J.; Wakelee, H.A.; Colevas, A.D.; et al. Tumor volume-adapted dosing in stereotactic ablative radiotherapy of lung tumors. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 231–237. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, K.H.; Okoye, C.C.; Patel, R.B.; Siva, S.; Biswas, T.; Ellis, R.J.; Yao, M.; Machtay, M.; Lo, S.S. Complications from Stereotactic Body Radiotherapy for Lung Cancer. Cancers 2015, 7, 981-1004. https://doi.org/10.3390/cancers7020820
Kang KH, Okoye CC, Patel RB, Siva S, Biswas T, Ellis RJ, Yao M, Machtay M, Lo SS. Complications from Stereotactic Body Radiotherapy for Lung Cancer. Cancers. 2015; 7(2):981-1004. https://doi.org/10.3390/cancers7020820
Chicago/Turabian StyleKang, Kylie H., Christian C. Okoye, Ravi B. Patel, Shankar Siva, Tithi Biswas, Rodney J. Ellis, Min Yao, Mitchell Machtay, and Simon S. Lo. 2015. "Complications from Stereotactic Body Radiotherapy for Lung Cancer" Cancers 7, no. 2: 981-1004. https://doi.org/10.3390/cancers7020820
APA StyleKang, K. H., Okoye, C. C., Patel, R. B., Siva, S., Biswas, T., Ellis, R. J., Yao, M., Machtay, M., & Lo, S. S. (2015). Complications from Stereotactic Body Radiotherapy for Lung Cancer. Cancers, 7(2), 981-1004. https://doi.org/10.3390/cancers7020820