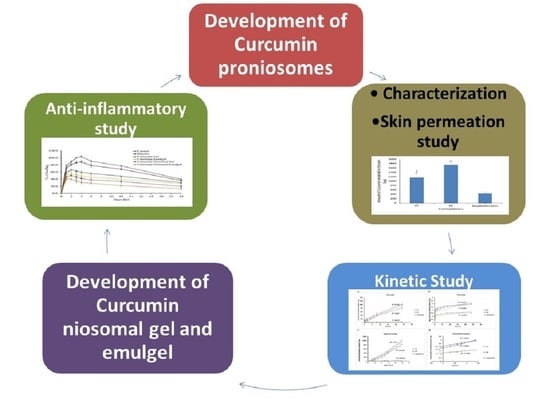
Curcumin Niosomes Prepared from Proniosomal Gels: In Vitro Skin Permeability, Kinetic and In Vivo Studies
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Preparation of Curcumin Proniosomes
2.2.2. Preparation of Curcumin Niosomes
2.3. Microscopic Examination
2.4. Analysis of the Particle Size
2.5. Entrapment Efficiency (EE) Determination
2.6. Ex Vivo Study
2.6.1. Preparation of Rat Skin
2.6.2. Curcumin Skin Permeation Study
2.7. Kinetic Study
2.8. Preparation of Curcumin Gel and Emulgel
2.9. Preparation of Curcumin Niosomal Gel and Emulgel
2.10. Animals
2.11. Anti-Inflammatory Testing of the Prepared Formulae
2.12. Statistical Analysis
3. Results and Discussion
3.1. Microscopic Examination
3.2. Analysis of the Particle Size
3.3. Entrapment Efficiency Determination
3.4. Curcumin Skin Permeation Study
3.5. Kinetic Study
3.6. Anti-Inflammatory Testing of the Prepared Formulae
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Ahmad, R.S.; Hussain, M.B.; Sultan, M.T.; Arshad, M.S.; Waheed, M.; Shariati, M.A.; Plygun, S.; Hashempur, M.H. Biochemistry, Safety, Pharmacological Activities, and Clinical Applications of Turmeric: A Mechanistic Review. Evid. Based Complementary Altern. Med. 2020, 2020, 7656919. [Google Scholar] [CrossRef] [PubMed]
- Chainani-Wu, N. Safety and anti-inflammatory activity of curcumin: A component of tumeric (Curcuma longa). J. Altern. Complement. Med. 2003, 9, 161–168. [Google Scholar] [CrossRef] [Green Version]
- Huang, M.T.; Smart, R.C.; Wong, C.Q.; Conney, A.H. Inhibitory effect of curcumin, chlorogenic acid, caffeic acid, and ferulic acid on tumor promotion in mouse skin by 12-O-tetradecanoylphorbol-13-acetate. Cancer Res. 1988, 48, 5941–5946. [Google Scholar]
- Ravindran, J.; Prasad, S.; Aggarwal, B.B. Curcumin and cancer cells: How many ways can curry kill tumor cells selectively? AAPS J. 2009, 11, 495–510. [Google Scholar] [CrossRef] [PubMed]
- Krausz, A.E.; Adler, B.L.; Cabral, V.; Navati, M.; Doerner, J.; Charafeddine, R.A.; Chandra, D.; Liang, H.; Gunther, L.; Clendaniel, A.; et al. Curcumin-encapsulated nanoparticles as innovative antimicrobial and wound healing agent. Nanomedicine 2015, 11, 195–206. [Google Scholar] [CrossRef] [Green Version]
- Pan, M.H.; Huang, T.M.; Lin, J.K. Biotransformation of curcumin through reduction and glucuronidation in mice. Drug Metab. Dispos. 1999, 27, 486–494. [Google Scholar] [PubMed]
- Allam, A.N.; Komeil, I.A.; Abdallah, O.Y. Curcumin phytosomal softgel formulation: Development, optimization and physicochemical characterization. Acta. Pharm. 2015, 65, 285–297. [Google Scholar] [CrossRef] [Green Version]
- López-Lázaro, M. Anticancer and Carcinogenic properties of curcumin: Considerations for Its clinical development as a cancer chemopreventive and chemotherapeutic agent. Mol. Nutr. Food Res. 2008, 52 (Suppl. 1), S103–S127. [Google Scholar] [CrossRef]
- Baghel, P.; Roy, A.; Verma, S.; Satapathy, T.; Bahadur, S. Amelioration of lipophilic compounds in regards to bioavailability as self-emulsifying drug delivery system (SEDDS). Future J. Pharm. Sci. 2020, 6, 21. [Google Scholar] [CrossRef]
- Shehata, T.; Kimura, T.; Higaki, K.; Ogawara, K.I. In-vivo disposition characteristics of PEG niosome and its interaction with serum proteins. Int. J. Pharm. 2016, 512, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Ge, X.; Wei, M.; He, S.; Yuan, W.-E. Advances of Non-Ionic Surfactant Vesicles (Niosomes) and Their Application in Drug Delivery. Pharmaceutics 2019, 11, 55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arzani, G.; Haeri, A.; Daeihamed, M.; Bakhtiari-Kaboutaraki, H.; Dadashzadeh, S. Niosomal carriers enhance oral bioavailability of carvedilol: Effects of bile salt-enriched vesicles and carrier surface charge. Int. J. Nanomed. 2015, 10, 4797–4813. [Google Scholar] [CrossRef] [Green Version]
- Dahan, A.; Hoffman, A. Evaluation of a chylomicron flow blocking approach to investigate the intestinal lymphatic transport of lipophilic drugs. Eur. J. Pharm. Sci. 2005, 24, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Vora, B.; Khopade, A.J.; Jain, N.K. Proniosome based transdermal delivery of levonorgestrel for effective contraception. J. Control. Release 1998, 54, 149–165. [Google Scholar] [CrossRef]
- Mokhtar, M.; Sammour, O.A.; Hammad, M.A.; Megrab, N.A. Effect of some formulation parameters on flurbiprofen encapsulation and release rates of niosomes prepared from proniosomes. Int. J. Pharm. 2008, 361, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Alsarra, I.A.; Bosela, A.A.; Ahmed, S.M.; Mahrous, G.M. Proniosomes as a drug carrier for transdermal delivery of ketorolac. Eur. J. Pharm. Biopharm. 2005, 59, 485–490. [Google Scholar] [CrossRef]
- Nastiti, C.; Ponto, T.; Abd, E.; Grice, J.E.; Benson, H.A.E.; Roberts, M.S. Topical Nano and Microemulsions for Skin Delivery. Pharmaceutics 2017, 9, 37. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.M.; Shehata, T.M. Tramadol HCl encapsulated niosomes for extended analgesic effect following oral administration. J. Drug Deliv. Sci. Technol. 2018, 46, 14–18. [Google Scholar] [CrossRef]
- Ibrahim, M.M.; Shehata, T.M. The enhancement of transdermal permeability of water soluble drug by niosome-emulgel combination. J. Drug Deliv. Sci. Technol. 2012, 22, 353–359. [Google Scholar] [CrossRef]
- Elsewedy, H.S.; Dhubiab, B.E.A.; Mahdy, M.A.; Elnahas, H.M. Development, optimization, and evaluation of PEGylated brucine-loaded PLGA nanoparticles. Drug Deliv. 2020, 27, 1134–1146. [Google Scholar] [CrossRef] [PubMed]
- Malakar, J.; Sen, S.O.; Nayak, A.K.; Sen, K.K. Formulation, optimization and evaluation of transferosomal gel for transdermal insulin delivery. Saudi Pharm. J. 2012, 20, 355–363. [Google Scholar] [CrossRef] [Green Version]
- Shah, J.; Nair, A.B.; Shah, H.; Jacob, S.; Shehata, T.M.; Morsy, M.A. Enhancement in antinociceptive and anti-inflammatory effects of tramadol by transdermal proniosome gel. Asian J. Pharm. Sci. 2019. [Google Scholar] [CrossRef]
- Morsy, M.A.; Abdel-Latif, R.G.; Nair, A.B.; Venugopala, K.N.; Ahmed, A.F.; Elsewedy, H.S.; Shehata, T.M. Preparation and Evaluation of Atorvastatin-Loaded Nanoemulgel on Wound-Healing Efficacy. Pharmaceutics 2019, 11, 609. [Google Scholar] [CrossRef] [Green Version]
- Damodharan, N.; Mohamed, R. Mathematical Modelling of Dissolution Kinetics in Dosage forms. Res. J. Pharm. Technol. 2020, 13, 1339–1345. [Google Scholar]
- Shehata, T.M.; Nair, A.B.; Al-Dhubiab, B.E.; Shah, J.; Jacob, S.; Alhaider, I.A.; Attimarad, M.; Elsewedy, H.S.; Ibrahim, M.M. Vesicular Emulgel Based System for Transdermal Delivery of Insulin: Factorial Design and in Vivo Evaluation. Appl. Sci. 2020, 10, 5341. [Google Scholar] [CrossRef]
- Khedr, M.A.; Shehata, T.M.; Mohamed, M.E. Repositioning of 2,4-Dichlorophenoxy acetic acid as a potential anti-inflammatory agent: In Silico and Pharmaceutical Formulation study. Eur. J. Pharm. Sci. 2014, 65, 130–138. [Google Scholar] [CrossRef]
- Tønnesen, H.H.; Karlsen, J. Studies on curcumin and curcuminoids. Z. Lebensm Unters. Forsch. 1985, 180, 132–134. [Google Scholar] [CrossRef]
- Varshosaz, J.; Pardakhty, A.; Hajhashemi, V.-I.; Najafabadi, A.R. Development and physical characterization of sorbitan monoester niosomes for insulin oral delivery. Drug Deliv. 2003, 10, 251–262. [Google Scholar] [CrossRef]
- Dash, S.; Murthy, P.N.; Nath, L.; Chowdhury, P. Kinetic modeling on drug release from controlled drug delivery systems. Acta Pol. Pharm. 2010, 67, 217–223. [Google Scholar]
- El-Menshawe, S.F.; Hussein, A.K. Formulation and evaluation of meloxicam niosomes as vesicular carriers for enhanced skin delivery. Pharm. Dev. Technol. 2013, 18, 779–786. [Google Scholar] [CrossRef]
- Soliman, W.E.; Shehata, T.M.; Mohamed, M.E.; Younis, N.S.; Elsewedy, H.S. Enhancement of Curcumin Anti-Inflammatory Effect via Formulation into Myrrh Oil-Based Nanoemulgel. Polymers 2021, 13, 577. [Google Scholar] [CrossRef]







| Formulae | Tween 80 (µmol) | Span 60 (µmol) | Cholesterol (µmol) | PG (mg) | Curcumin (mg) | Proniosome Produced |
|---|---|---|---|---|---|---|
| F1 | 250 | - | 250 | 400 | 50 | Translucent yellow gel |
| F2 | - | 250 | 250 | 400 | 50 | Yellow creamy gel |
| F3 | 125 | 125 | 250 | 400 | 50 | Yellow creamy gel |
| F4 | 750 | - | 750 | 400 | 50 | Translucent yellow gel |
| F5 | - | 750 | 750 | 400 | 50 | Yellow creamy gel |
| F6 | 375 | 375 | 750 | 400 | 50 | Yellow creamy gel |
| F7 | 1000 | - | 1000 | 400 | 50 | Translucent yellow gel |
| F8 | - | 1000 | 1000 | 400 | 50 | Yellow creamy gel |
| F9 | 500 | 500 | 1000 | 400 | 50 | Yellow creamy gel |
| F10 | 1300 | - | 700 | 400 | 50 | Translucent yellow gel |
| F11 | 1500 | - | 500 | 400 | 50 | Translucent yellow gel |
| F12 | - | 1300 | 700 | 400 | 50 | Yellow creamy gel |
| F13 | - | 1500 | 500 | 400 | 50 | Yellow creamy gel |
| Materials | Curcumin Gel | Curcumin NIOSOMAL Gel | Curcumin Emulgel | Curcumin Niosomal Emulgel |
|---|---|---|---|---|
| Curcumin(g) | 0.05 | - | 0.05 | - |
| NaCMC (g) | 0.8 | 0.8 | 0.8 | 0.8 |
| Liquid paraffin (mL) | - | - | 2.5 | 2.5 |
| Tween 80 (mL) | - | - | 0.25 | 0.25 |
| Niosomes loaded curcumin (mL) (best formulation) | - | Q.s | - | Q.s |
| Buffer pH 6.8 to (mL) | 20 | 20 | 20 | 20 |
| Formulae | Vesicle Size * (nm) | PDI | EE% |
|---|---|---|---|
| F1 | 343 ± 18 | 0.880 ± 0.150 | 22.50 ± 0.64 |
| F2 | 481 ± 32 | 0.487 ± 0.128 | 15.75 ± 1.35 |
| F3 | 542 ± 86 | 0.552 ± 0.465 | 19.68 ± 0.98 |
| F4 | 413 ± 21 | 0.207 ± 0.05 | 95.41 ± 1.06 |
| F5 | 810 ± 118 | 0.320 ± 0.04 | 47.81 ± 2.16 |
| F6 | 645 ± 81 | 0.137 ± 0.17 | 64.87 ± 1.09 |
| F7 | 452 ± 24 | 0.44 ± 0.08 | 98.60 ± 2.23 |
| F8 | 1701 ± 97 | 0.373 ± 0.071 | 52.24 ± 1.33 |
| F9 | 746 ± 67 | 0.325 ± 0.12 | 95.18 ± 2.35 |
| F10 | 396 ± 93 | 0.421 ± 0.01 | 96.21 ± 3.21 |
| F11 | 345 ± 12 | 0.240 ± 0.045 | 99.74 ± 5.06 |
| F12 | 1651 ± 95 | 0.654 ± 0.235 | 55.31 ± 1.20 |
| F13 | 1800 ± 105 | 0.954 ± 0.120 | 62.2 ± 3.54 |
| Formula | SSTF a μg/cm2 × h | PC b cm2/h | Enhancement Ratio (ER) c |
|---|---|---|---|
| Curcumin suspension | 0.331 ± 0.087 | 0.00057 ± 0.0002 | 1 |
| F7 | 7.072 ± 0.961 * | 0.0122 ± 0.0016 | 21.86 ± 2.85 |
| F9 | 8.46 ± 1.31 * | 0.0146 ± 0.002 | 27.54 ± 11.52 |
| Formula | Zero Order | First Order | Higauchi Model | Korsmeyer-Peppas | ||||
|---|---|---|---|---|---|---|---|---|
| R2 | K0 | R2 | K1 | R2 | KH | R2 | n | |
| Curcumin suspension | 0.6537 | 1.240 | 0.2707 | 0.0765 | 0.8999 | 7.2453 | 0.9786 | 0.2945 |
| F7 | 0.9827 | 33.577 | 0.3959 | 0.1631 | 0.9538 | 171.86 | 0.9916 | 0.5568 |
| F9 | 0.9754 | 38.468 | 0.3112 | 0.1490 | 0.970 | 199.3 | 0.9821 | 0.7345 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shehata, T.M.; Ibrahim, M.M.; Elsewedy, H.S. Curcumin Niosomes Prepared from Proniosomal Gels: In Vitro Skin Permeability, Kinetic and In Vivo Studies. Polymers 2021, 13, 791. https://doi.org/10.3390/polym13050791
Shehata TM, Ibrahim MM, Elsewedy HS. Curcumin Niosomes Prepared from Proniosomal Gels: In Vitro Skin Permeability, Kinetic and In Vivo Studies. Polymers. 2021; 13(5):791. https://doi.org/10.3390/polym13050791
Chicago/Turabian StyleShehata, Tamer M., Mahmoud M. Ibrahim, and Heba S. Elsewedy. 2021. "Curcumin Niosomes Prepared from Proniosomal Gels: In Vitro Skin Permeability, Kinetic and In Vivo Studies" Polymers 13, no. 5: 791. https://doi.org/10.3390/polym13050791
APA StyleShehata, T. M., Ibrahim, M. M., & Elsewedy, H. S. (2021). Curcumin Niosomes Prepared from Proniosomal Gels: In Vitro Skin Permeability, Kinetic and In Vivo Studies. Polymers, 13(5), 791. https://doi.org/10.3390/polym13050791