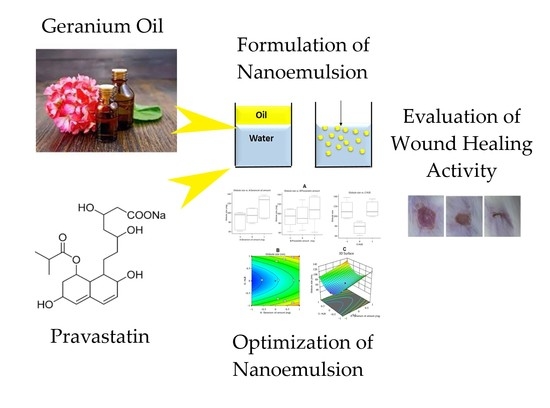
Tailoring of Geranium Oil-Based Nanoemulsion Loaded with Pravastatin as a Nanoplatform for Wound Healing
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Experimental Design and Optimization of Self-Nanoemulsion Formulations
2.2.2. Gr-PV-NEs Preparation
2.2.3. Determination of Globule Size
2.2.4. Assessment of Wound Healing
Animal Handling and Care
Measurement of Burn Wound Diameter
2.3. Optimization of the Gr-PV-NEs
2.4. Characterization of the Optimized Formulation
2.4.1. Determination of Entrapemnt Efficiency
2.4.2. Zeta Potential Determination
2.4.3. Measurement of Burn Wound Diameter and Interlukin-6 Level
2.4.4. Ex-Vivo Permeation Study
2.4.5. Antibacterial Activity Evaluation
2.4.6. Statistical Analysis
3. Results and Discussion
3.1. Assessment of Gr-PV-NE Droplet Size
3.2. Assessment of Wound Healing
3.3. Optimization and Evaluation of Nanoemulsion Formulations
3.3.1. Wound Healing Action Assessment
Burn Wound Diameter Evaluation
IL-6 Level Evaluation
3.3.2. Ex-Vivo Permeation Study
3.3.3. Antibacterial Activity Assessment
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Montagna, W. The Structure and Function of Skin; Elsevier: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Yousef, H.; Alhajj, M.; Sharma, S. Anatomy, Skin (Integument), Epidermis, in StatPearls; StatPearls Publishing LLC: Treasure Island, FL, USA, 2022. [Google Scholar]
- Velnar, T.; Bailey, T.; Smrkolj, V. The Wound Healing Process: An Overview of the Cellular and Molecular Mechanisms. J. Int. Med. Res. 2009, 37, 1528–1542. [Google Scholar] [CrossRef] [PubMed]
- Cañedo-Dorantes, L.; Cañedo-Ayala, M. Skin Acute Wound Healing: A Comprehensive Review. Int. J. Inflamm. 2019, 2019, 3706315. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Dipietro, L.A. Factors affecting wound healing. J. Dent. Res. 2010, 89, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Brem, H.; Tomic-Canic, M. Cellular and molecular basis of wound healing in diabetes. J. Clin. Investig. 2007, 117, 1219–1222. [Google Scholar] [CrossRef] [Green Version]
- Vincent, A.M.; Russell, J.W.; Low, P.; Feldman, E.L. Oxidative stress in the pathogenesis of diabetic neuropathy. Endocr. Rev. 2004, 25, 612–628. [Google Scholar] [CrossRef]
- Schneider, K.L.; Yahia, N. Effectiveness of Arginine Supplementation on Wound Healing in Older Adults in Acute and Chronic Settings: A Systematic Review. Adv. Skin Wound Care 2019, 32, 457–462. [Google Scholar] [CrossRef]
- Garros Ide, C.; Campos, A.C.; Tâmbara, E.M.; Tenório, S.B.; Torres, O.J.; Agulham, M.A.; Araújo, A.C.; Santis-Isolan, P.M.; Oliveira, R.M.; Arruda, E.C. Extract from Passiflora edulis on the healing of open wounds in rats: Morphometric and histological study. Acta Cir. Bras. 2006, 21, 55–65. [Google Scholar]
- Givol, O.; Kornhaber, R.; Visentin, D.; Cleary, M.; Haik, J.; Harats, M. A systematic review of Calendula officinalis extract for wound healing. Wound Repair Regen. 2019, 27, 548–561. [Google Scholar] [CrossRef]
- Grundy, S.M. HMG-CoA reductase inhibitors for treatment of hypercholesterolemia. N. Engl. J. Med. 1988, 319, 24–33. [Google Scholar]
- Toker, S.; Gulcan, E.; Cayc, M.K.; Olgun, E.G.; Erbilen, E.; Ozay, Y. Topical atorvastatin in the treatment of diabetic wounds. Am. J. Med. Sci. 2009, 338, 201–204. [Google Scholar] [CrossRef]
- Ko, J.H.; Kim, P.S.; Zhao, Y.; Hong, S.J.; Mustoe, T.A. HMG-CoA Reductase Inhibitors (Statins) Reduce Hypertrophic Scar Formation in a Rabbit Ear Wounding Model. Plast. Reconstr. Surg. 2012, 129, 252e–261e. [Google Scholar] [CrossRef] [PubMed]
- Bitto, A.; Minutoli, L.; Altavilla, D.; Polito, F.; Fiumara, T.; Marini, H.; Galeano, M.; Calò, M.; Lo Cascio, P.; Bonaiuto, M.; et al. Simvastatin enhances VEGF production and ameliorates impaired wound healing in experimental diabetes. Pharmacol. Res. 2008, 57, 159–169. [Google Scholar] [CrossRef]
- Hoeben, A.; Landuyt, B.; Highley, M.S.; Wildiers, H.; Van Oosterom, A.T.; De Bruijn, E.A. Vascular endothelial growth factor and angiogenesis. Pharmacol. Rev. 2004, 56, 549–580. [Google Scholar] [CrossRef] [PubMed]
- Karadeniz Cakmak, G.; Irkorucu, O.; Ucan, B.H.; Emre, A.U.; Bahadir, B.; Demirtas, C.; Tascilar, O.; Karakaya, K.; Acikgoz, S.; Kertis, G.; et al. Simvastatin improves wound strength after intestinal anastomosis in the rat. J. Gastrointest. Surg. 2009, 13, 1707–1716. [Google Scholar] [CrossRef] [PubMed]
- Fischer, J.; Ganellin, C.R. Analogue-Based Drug Discovery; John Wiley & Sons: Hoboken, NJ, USA, 2006; p. 472. ISBN 9783527607495. [Google Scholar]
- Bourgier, C.; Auperin, A.; Rivera, S.; Boisselier, P.; Petit, B.; Lang, P.; Lassau, N.; Taourel, P.; Tetreau, R.; Azria, D.; et al. Pravastatin Reverses Established Radiation-Induced Cutaneous and Subcutaneous Fibrosis in Patients with Head and Neck Cancer: Results of the Biology-Driven Phase 2 Clinical Trial Pravacur. Int. J. Radiat. Oncol. Biol. Phys. 2019, 104, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Ayad, H.S.; Reda, F.; Abdalla, M.A. Effect of putrescine and zinc on vegetative growth, photosynthetic pigments, lipid peroxidation and essential oil content of geranium (Pelargonium graveolens L.). World J. Agric. Sci. 2010, 6, 601–608. [Google Scholar]
- Lis-Balchin, M. A chemotaxonomic study of the Pelargonium (Geraniaceae) species and their modern cultivars. J. Hortic. Sci. 1997, 72, 791–795. [Google Scholar] [CrossRef]
- Standen, M.D.; Connellan, P.A.; Leach, D.N. Natural killer cell activity and lymphocyte activation: Investigating the effects of a selection of essential oils and components in vitro. Int. J. Aromather. 2006, 16, 133–139. [Google Scholar] [CrossRef]
- Zhuang, S.R.; Chen, S.L.; Tsai, J.H.; Huang, C.C.; Wu, T.C.; Liu, W.S.; Tseng, H.C.; Lee, H.S.; Huang, M.C.; Shane, G.T.; et al. Effect of citronellol and the Chinese medical herb complex on cellular immunity of cancer patients receiving chemotherapy/radiotherapy. Phytother. Res. 2009, 23, 785–790. [Google Scholar] [CrossRef]
- Burke, Y.D.; Stark, M.J.; Roach, S.L.; Sen, S.E.; Crowell, P.L. Inhibition of pancreatic cancer growth by the dietary isoprenoids farnesol and geraniol. Lipids 1997, 32, 151–156. [Google Scholar] [CrossRef]
- Asgarpanah, J.; Ramezanloo, F. An overview on phytopharmacology of Pelargonium graveolens L. Indian J. Tradit. Knowl. 2015, 14, 558–563. [Google Scholar]
- Lohani, A.; Verma, A.; Hema, G.; Pathak, K. Topical Delivery of Geranium/Calendula Essential Oil-Entrapped Ethanolic Lipid Vesicular Cream to Combat Skin Aging. BioMed. Res. Int. 2021, 2021, 4593759. [Google Scholar] [CrossRef] [PubMed]
- Boukhatem, M.N.; Kameli, A.; Ferhat, M.A.; Saidi, F.; Mekarnia, M. Rose geranium essential oil as a source of new and safe anti-inflammatory drugs. Libyan J. Med. 2013, 8, 22520. [Google Scholar] [CrossRef]
- Singh, B.; Bandopadhyay, S.; Kapil, R.; Singh, R.; Katare, O. Self-emulsifying drug delivery systems (SEDDS): Formulation development, characterization, and applications. Crit. Rev. Ther. Drug Carrier Syst. 2009, 26, 427–521. [Google Scholar] [CrossRef] [PubMed]
- Portugal, I.; Jain, S.; Severino, P.; Priefer, R. Micro-and Nano-Based Transdermal Delivery Systems of Photosensitizing Drugs for the Treatment of Cutaneous Malignancies. Pharmaceuticals 2021, 14, 772. [Google Scholar] [CrossRef]
- Mossa, A.H.; Afia, S.I.; Mohafrash, S.M.; Abou-Awad, B.A. Rosemary essential oil nanoemulsion, formulation, characterization and acaricidal activity against the two-spotted spider mite Tetranychus urticae Koch (Acari: Tetranychidae). J. Plant Prot. Res. 2019, 59, 102–112. [Google Scholar]
- Hosny, K.M. Development of Saquinavir Mesylate Nanoemulsion-Loaded Transdermal Films: Two-Step Optimization of Permeation Parameters, Characterization, and Ex Vivo and In Vivo Evaluation. Int. J. Nanomed. 2019, 14, 8589–8601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chae, G.S.; Lee, J.S.; Kim, S.H.; Seo, K.S.; Kim, M.S.; Lee, H.B.; Khang, G. Enhancement of the stability of BCNU using self-emulsifying drug delivery systems (SEDDS) and in vitro antitumor activity of self-emulsified BCNU-loaded PLGA wafer. Int. J. Pharm. 2004, 301, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Odeberg, J.M.; Kaufmann, P.; Kroon, K.G.; Höglund, P. Lipid drug delivery and rational formulation design for lipophilic drugs with low oral bioavailability, applied to cyclosporine. Eur. J. Pharm. Sci. 2003, 20, 375–382. [Google Scholar] [CrossRef]
- Priya, K.; Bhikshapathi, D.V.R.N.; Ramesh, B. Design and Characterization of Self-Nanoemulsifying Drug Delivery System of Lovastatin. Int. J. Pharm. Sci. Nanotechnol. 2018, 11, 4042–4052. [Google Scholar] [CrossRef]
- Harwansh, R.K.; Deshmukh, R.; Rahman, M.A. Nanoemulsion: Promising nanocarrier system for delivery of herbal bioactives. J. Drug Deliv. Sci. Technol. 2019, 51, 224–233. [Google Scholar] [CrossRef]
- N Politis, S.; Colombo, P.; Colombo, G.; M Rekkas, D. Design of experiments (DoE) in pharmaceutical development. Drug. Dev. Ind. Pharm. 2017, 43, 889–901. [Google Scholar] [CrossRef] [PubMed]
- Hosny, K.M.; Alhakamy, N.A.; Sindi, A.M.; Khallaf, R.A. Coconut Oil Nanoemulsion Loaded with a Statin Hypolipidemic Drug for Management of Burns: Formulation and In Vivo Evaluation. Pharmaceutics 2020, 12, 1061. [Google Scholar] [CrossRef] [PubMed]
- Gadekar, R.; Saurabh, M.K.; Saurabh, A. Study of formulation, characterisation and wound healing potential of transdermal patches of Curcumin. Asian J. Pharm. Clin. Res. 2012, 5, 225–230. [Google Scholar]
- Hussein, R.M.; Kandeil, M.A.; Mohammed, N.A.; Khallaf, R.A. Evaluation of the hepatoprotective effect of curcumin-loaded solid lipid nanoparticles against paracetamol overdose toxicity: Role of inducible nitric oxide synthase. J. Liposome Res. 2022, 8, 1–11. [Google Scholar] [CrossRef]
- Salem, H.F.; Nafady, M.M.; Ewees, M.G.E.; Hassan, H.; Khallaf, R.A. Rosuvastatin calcium-based novel nanocubic vesicles capped with silver nanoparticles-loaded hydrogel for wound healing management: Optimization employing Box-Behnken design: In vitro and in vivo assessment. J. Liposome Res. 2022, 32, 45–61. [Google Scholar] [CrossRef]
- Salem, H.F.; El-Menshawe, S.F.; Khallaf, R.A.; Rabea, Y.K. A novel transdermal nanoethosomal gel of lercanidipine HCl for treatment of hypertension: Optimization using Box-Benkhen design, in vitro and in vivo characterization. Drug Deliv. Transl. Res. 2020, 10, 227–240. [Google Scholar] [CrossRef]
- Hosny, K.M.; Khallaf, R.A.; Asfour, H.Z.; Rizg, W.Y.; Alhakamy, N.A.; Sindi, A.M.; Alkhalidi, H.M.; Abualsunun, W.A.; Bakhaidar, R.B.; Almehmady, A.M.; et al. Development and Optimization of Cinnamon Oil Nanoemulgel for Enhancement of Solubility and Evaluation of Antibacterial, Antifungal and Analgesic Effects against Oral Microbiota. Pharmaceutics 2021, 13, 1008. [Google Scholar] [CrossRef]
- Ustündağ Okur, N.; Apaydın, S.; Karabay Yavaşoğlu, N.Ü.; Yavaşoğlu, A.; Karasulu, H.Y. Evaluation of skin permeation and anti-inflammatory and analgesic effects of new naproxen microemulsion formulations. Int. J. Pharm. 2011, 416, 136–144. [Google Scholar] [CrossRef]
- Orafidiya, L.O.; Oladimeji, F.A. Determination of the required HLB values of some essential oils. Int. J. Pharm. 2002, 237, 241–249. [Google Scholar] [CrossRef]
- Hosny, K.; Asfour, H.; Rizg, W.; Alhakamy, N.A.; Sindi, A.; Alkhalidi, H.; Abualsunun, W.; Bakhaidar, R.; Almehmady, A.M.; Akeel, S.; et al. Formulation, Optimization, and Evaluation of Oregano Oil Nanoemulsions for the Treatment of Infections Due to Oral Microbiota. Int. J. Nanomed. 2021, 16, 5465–5478. [Google Scholar] [CrossRef] [PubMed]
- Sienkiewicz, M.; Poznańska-Kurowska, K.; Kaszuba, A.; Kowalczyk, E. The antibacterial activity of geranium oil against Gram-negative bacteria isolated from difficult-to-heal wounds. Burns 2014, 40, 1046–1051. [Google Scholar] [CrossRef] [PubMed]
- Rezvanian, M.; Amin, M.C.I.M.; Ng, S.F. Development and physicochemical characterization of alginate composite film loaded with simvastatin as a potential wound dressing. Carbohydr. Polym. 2016, 137, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Farsaei, S.; Khalili, H.; Farboud, E.S. Potential role of statins on wound healing: Review of the literature. Int. Wound J. 2012, 9, 238–247. [Google Scholar] [PubMed]
- Tanaka, T.; Narazaki, M.; Kishimoto, T. IL-6 in Inflammation, Immunity, and Disease. Cold Spring Harb. Perspect. Biol. 2014, 6, a016295. [Google Scholar] [CrossRef] [PubMed]
- Kolodziejczyk, A.M.; Targosz-Korecka, M.; Szymonski, M. Nanomechanical testing of drug activities at the cellular level: Case study for endothelium-targeted drugs. Pharm. Rep. 2017, 69, 1165–1172. [Google Scholar] [CrossRef] [PubMed]
- Saggini, A.; Anogeianaki, A.; Maccauro, G.; Teté, S.; Salini, V.; Caraffa, A.; Conti, F.; Fulcheri, M.; Galzio, R.; Shaik-Dasthagirisaheb, Y.B. Cholesterol, cytokines and diseases. Int. J. Imm. Pharm. 2011, 24, 567–581. [Google Scholar] [CrossRef] [Green Version]
- Lahera, V.; Goicoechea, M.; de Vinuesa, S.G.; Miana, M.; de las Heras, N.; Cachofeiro, V.; Luño, J. Endothelial dysfunction, oxidative stress and inflammation in atherosclerosis: Beneficial effects of statins. Curr. Med. Chem. 2007, 14, 243–248. [Google Scholar] [CrossRef]
- Abe, S.; Maruyama, N.; Hayama, K.; Inouye, S.; Oshima, H.; Yamaguchi, H. Suppression of neutrophil recruitment in mice by geranium essential oil. Mediat. Inflamm. 2004, 13, 21–24. [Google Scholar] [CrossRef]
- Su, Y.W.; Chao, S.H.; Lee, M.H.; Ou, T.Y.; Tsai, Y.C. Inhibitory effects of citronellol andgeraniol on nitric oxide and prostaglandin E2 production in macrophages. Plant. Med. 2010, 76, 1666–1671. [Google Scholar] [CrossRef]
- Pérez, G.S.; Zavala, S.M.; Arias, G.L.; Ramos, L.M. Anti-inflammatory activity of some essential oils. J. Essent. Oil Res. 2011, 23, 38–44. [Google Scholar] [CrossRef]
- Chen, W.; Viljoen, A.M. Geraniol—A review of a commercially important fragrance material. S. Afr. J. Bot. 2010, 76, 643–651. [Google Scholar] [CrossRef] [Green Version]
- Rizg, W.Y.; Hosny, K.M.; Elgebaly, S.S.; Alamoudi, A.J.; Felimban, R.I.; Tayeb, H.H.; Alharbi, M.; Bukhary, H.A.; Abualsunun, W.A.; Almehmady, A.M.; et al. Preparation and Optimization of Garlic Oil/Apple Cider Vinegar Nanoemulsion Loaded with Minoxidil to Treat Alopecia. Pharmaceutics 2021, 13, 2150. [Google Scholar] [CrossRef] [PubMed]
- Bigos, M.; Wasiela, M.; Kalemba, D.; Sienkiewicz, M. Antimicrobial activity of geranium oil against clinical strains of Staphylococcus aureus. Molecules 2012, 17, 10276–10291. [Google Scholar] [CrossRef] [PubMed] [Green Version]







| Independent Variables | Levels | ||
|---|---|---|---|
| −1 | 0 | 1 | |
| A = Geranium oil amount (mg) | 100 | 200 | 300 |
| B = Pravastatin amount (mg) | 10 | 20 | 40 |
| C = HLB of surfactant mixture | 11 | 12 | 13 |
| Dependent Variables | Goal | ||
| Y1 = Globule size (nm) | Minimize | ||
| Y2 = Mean burned wound diameter (mm) | Minimize | ||
| A | B | C | Y1 | Y2 | ||
|---|---|---|---|---|---|---|
| Run | Geranium Oil Amount (mg) | Pravastatin Amount (mg) | HLB | Droplet Size (nm) | Mean Burned Wound Diameter (mm) | Polydispersity Index |
| 1 | 200 | 10 | 13 | 110 ± 2.0 | 7.5 ± 0.30 | 0.09 ± 0.02 |
| 2 | 300 | 20 | 11 | 128 ± 4.5 | 4.5 ± 0.18 | 0.11 ± 0.03 |
| 3 | 100 | 20 | 11 | 99 ± 7.0 | 8.0 ± 0.90 | 0.15 ± 0.03 |
| 4 | 100 | 10 | 12 | 62 ± 1.5 | 9.0 ± 1.10 | 0.21 ± 0.04 |
| 5 | 300 | 20 | 13 | 129 ± 3.2 | 4.5 ± 0.62 | 0.13 ± 0.02 |
| 6 | 100 | 40 | 12 | 61 ± 1.5 | 5.0 ± 0.51 | 0.32 ± 0.04 |
| 7 | 200 | 20 | 12 | 81 ± 5.0 | 6.5 ± 0.25 | 0.28 ± 0.05 |
| 8 | 200 | 20 | 12 | 80 ± 4.5 | 6.0 ± 0.18 | 0.19 ± 0.04 |
| 9 | 300 | 40 | 12 | 89 ± 3.5 | 3.0 ± 0.09 | 0.22 ± 0.05 |
| 10 | 200 | 10 | 11 | 109 ± 4.0 | 7.5 ± 0.64 | 0.38 ± 0.06 |
| 11 | 200 | 40 | 13 | 108 ± 8.0 | 5.0 ± 0.33 | 0.40 ± 0.05 |
| 12 | 200 | 40 | 11 | 110 ± 2.5 | 4.5 ± 0.21 | 0.10 ± 0.02 |
| 13 | 200 | 20 | 12 | 79 ± 1.9 | 6.0 ± 0.30 | 0.35 ± 0.02 |
| 14 | 100 | 20 | 13 | 99 ± 4.0 | 7.5 ± 0.42 | 0.30 ± 0.04 |
| 15 | 300 | 10 | 12 | 87 ± 3.5 | 5.0 ± 0.17 | 0.29 ± 0.05 |
| 16 | 100 | 10 | 11 | 95 ± 2.9 | 10 ± 1.20 | 0.26 ± 0.05 |
| 17 | 300 | 40 | 13 | 135 ± 5.5 | 3.5 ± 0.09 | 0.18 ± 0.04 |
| 18 | 100 | 10 | 13 | 101 ± 2.1 | 9.5 ± 0.50 | 0.32 ± 0.03 |
| 19 | 100 | 40 | 11 | 97 ± 6.1 | 5.5 ± 0.11 | 0.27 ± 0.05 |
| 20 | 300 | 20 | 12 | 90 ± 1.5 | 4.0 ± 0.30 | 0.19 ± 0.06 |
| 21 | 300 | 40 | 11 | 138 ± 3.1 | 2.5 ± 0.30 | 0.11 ± 0.03 |
| 22 | 100 | 20 | 12 | 65 ± 2.0 | 7.0 ± 1.90 | 0.25 ± 0.05 |
| 23 | 200 | 10 | 12 | 77 ± 1.8 | 7.0 ± 0.21 | 0.39 ± 0.06 |
| Dependent Variables | R2 | Adjusted R2 | Predicted R2 | F-Value | p-Value | Adequate Precision |
|---|---|---|---|---|---|---|
| Y1 | 0.9840 | 0.9729 | 0.9445 | 88.79 | 0.0001 | 30.3760 |
| Y2 | 0.9892 | 0.9817 | 0.9642 | 132.17 | 0.0001 | 38.5081 |
| Run | A: Geranium Oil Amount | B: Pravastatin Amount | C: HLB Value | Pravastatin Permeated % | Inhibition Zone against S. aureus (mm) |
|---|---|---|---|---|---|
| Optimum formulation (Gr-PV-NE) | 275 mg | 40 | 12 | 84% ± 3.1 | 20.0 ± 1.8 |
| Gr-NE | 275 mg | 0 | 12 | 0 | 19.0 ± 1.4 |
| Oleic acid-PV-NE | 0 | 40 | 12 | 64% ± 2.4 | 6.00 ± 0.8 |
| Gr-PV mixture | 275 mg | 40 | 0 | 31% ± 1.2 | 12.0 ± 1.1 |
| PV aqueous dispersion | 0 | 40 | 0 | 11% ± 0.6 | 4.50 ± 0.3 |
| Plain NE | 0 | 0 | 12 | 0 | 5.00 ± 0.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rizg, W.Y.; Hosny, K.M.; Eshmawi, B.A.; Alamoudi, A.J.; Safhi, A.Y.; Murshid, S.S.A.; Sabei, F.Y.; Al Fatease, A. Tailoring of Geranium Oil-Based Nanoemulsion Loaded with Pravastatin as a Nanoplatform for Wound Healing. Polymers 2022, 14, 1912. https://doi.org/10.3390/polym14091912
Rizg WY, Hosny KM, Eshmawi BA, Alamoudi AJ, Safhi AY, Murshid SSA, Sabei FY, Al Fatease A. Tailoring of Geranium Oil-Based Nanoemulsion Loaded with Pravastatin as a Nanoplatform for Wound Healing. Polymers. 2022; 14(9):1912. https://doi.org/10.3390/polym14091912
Chicago/Turabian StyleRizg, Waleed Y., Khaled M. Hosny, Bayan A. Eshmawi, Abdulmohsin J. Alamoudi, Awaji Y. Safhi, Samar S. A. Murshid, Fahad Y. Sabei, and Adel Al Fatease. 2022. "Tailoring of Geranium Oil-Based Nanoemulsion Loaded with Pravastatin as a Nanoplatform for Wound Healing" Polymers 14, no. 9: 1912. https://doi.org/10.3390/polym14091912
APA StyleRizg, W. Y., Hosny, K. M., Eshmawi, B. A., Alamoudi, A. J., Safhi, A. Y., Murshid, S. S. A., Sabei, F. Y., & Al Fatease, A. (2022). Tailoring of Geranium Oil-Based Nanoemulsion Loaded with Pravastatin as a Nanoplatform for Wound Healing. Polymers, 14(9), 1912. https://doi.org/10.3390/polym14091912