PROVE—Pre-Eclampsia Obstetric Adverse Events: Establishment of a Biobank and Database for Pre-Eclampsia
Abstract
:1. Introduction
2. Aims and Objectives
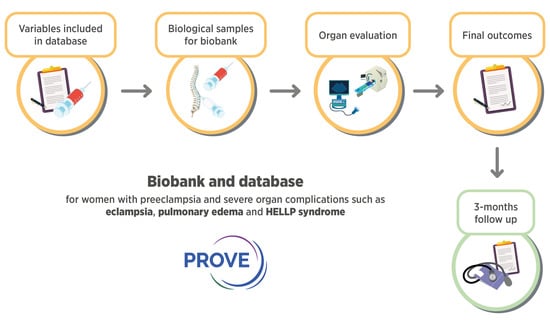
3. Materials and Methods
3.1. Study Design and Population
Inclusion and Exclusion Criteria
3.2. Collection of Clinical Information
3.3. Sample Collection and Storage
3.4. Questionnaires and Biophysical Examinations
3.4.1. Cognitive Function Testing
3.4.2. Brain MRI
3.4.3. Transcranial Doppler
3.4.4. Echocardiography and Cardiac MRI
3.5. Statistics
Power Calculations
3.6. Patient and Public Involvement
3.7. Ethics and Dissemination
4. Collection to Date
5. Discussion
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mol, B.W.J.; Roberts, C.T.; Thangaratinam, S.; Magee, L.A.; de Groot, C.J.M.; Hofmeyr, G.J. Preeclampsia. Lancet 2016, 387, 999–1011. [Google Scholar] [CrossRef]
- Duley, L. The Global Impact of Pre-eclampsia and Eclampsia. Semin. Perinatol. 2009, 33, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Moodley, J. Maternal deaths due to hypertensive disorders of pregnancy. Saving Mothers 2014–2016. In 7th Triennial Report on Confidential Enquiries into Maternal Deaths in South Africa; Department of Health: Pretoria, South Africa, 2018. [Google Scholar]
- Levine, R.J.; Maynard, S.E.; Qian, C.; Lim, K.-H.; England, L.J.; Yu, K.F.; Schisterman, E.F.; Thadhani, R.; Sachs, B.P.; Epstein, F.H.; et al. Circulating Angiogenic Factors and the Risk of Preeclampsia. N. Engl. J. Med. 2004, 350, 672–683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Young, B.C.; Levine, R.J.; Karumanchi, S.A. Pathogenesis of Preeclampsia. Annu. Rev. Pathol. Mech. Dis. 2010, 5, 173–192. [Google Scholar] [CrossRef]
- Ghulmiyyah, L.; Sibai, B. Maternal Mortality from Preeclampsia/Eclampsia. Semin. Perinatol. 2012, 36, 56–59. [Google Scholar] [CrossRef]
- Mackay, A.P.; Berg, C.J.; Atrash, H.K. Pregnancy-Related Mortality from Preeclampsia and Eclampsia. Obstet. Gynecol. 2001, 97, 533–538. [Google Scholar] [CrossRef]
- Melchiorre, K.; Sutherland, G.R.; Watt-Coote, I.; Liberati, M.; Thilaganathan, B. Severe Myocardial Impairment and Chamber Dysfunction in Preterm Preeclampsia. Hypertens. Pregnancy 2010, 31, 454–471. [Google Scholar] [CrossRef]
- Zhang, J.; Meikle, S.; Trumble, A. Severe Maternal Morbidity Associated with Hypertensive Disorders in Pregnancy in the United States. Hypertens. Pregnancy 2003, 22, 203–212. [Google Scholar] [CrossRef]
- Hall, D.R.; Grové, D.; Carstens, E. Early pre-eclampsia: What proportion of women qualify for expectant management and if not, why not? Eur. J. Obstet. Gynecol. Reprod. Biol. 2006, 128, 169–174. [Google Scholar] [CrossRef]
- Sunderland, N.; Hennessy, A.; Makris, A. Animal Models of Pre-eclampsia. Am. J. Reprod. Immunol. 2010, 65, 533–541. [Google Scholar] [CrossRef]
- Hall, D.R.; Odendaal, H.J.; Steyn, D.W.; Grove, D.B. Expectant management of early onset, severe pre-eclampsia: Maternal outcome. BJOG Int. J. Obstet. Gynaecol. 2000, 107, 1252–1257. [Google Scholar] [CrossRef]
- Steyn, D.W.; Odendaal, H.J. Randomised controlled trial of ketanserin and aspirin in prevention of pre-eclampsia. Lancet 1997, 350, 1267–1271. [Google Scholar] [CrossRef]
- Odendaal, H.J.; Pattinson, R.C.; Bam, R.; Grove, D.; Kotze, T.J. Aggressive or expectant management for patients with severe preeclampsia between 28–34 weeks’ gestation: A randomized controlled trial. Obstet. Gynecol. 1990, 76, 1070–1075. [Google Scholar]
- Cluver, C.A.; Hannan, N.J.; van Papendorp, E.; Hiscock, R.; Beard, S.; Mol, B.W.; Theron, G.B.; Hall, D.R.; Decloedt, E.H.; Stander, M.; et al. Esomeprazole to treat women with preterm preeclampsia: A randomized placebo controlled trial. Am. J. Obstet. Gynecol. 2018, 219, 388.e1–388.e17. [Google Scholar] [CrossRef]
- Hall, D.R. Understanding expectant management of pre-eclampsia: Review. Obstet. Gynaecol. Forum 2016, 26, 22–27. [Google Scholar]
- Myatt, L.; Redman, C.W.; Staff, A.C.; Hansson, S.; Wilson, M.L.; Laivuori, H.; Poston, L.; Roberts, J.M. Strategy for Standardization of Preeclampsia Research Study Design. Hypertension 2014, 63, 1293–1301. [Google Scholar] [CrossRef] [Green Version]
- Brown, M.A.; Magee, L.A.; Kenny, L.C.; Karumanchi, S.A.; McCarthy, F.P.; Saito, S.; Hall, D.R.; Warren, C.E.; Adoyi, G.; Ishaku, S. The hypertensive disorders of pregnancy: ISSHP classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2018, 13, 291–310. [Google Scholar]
- Van Veen, T.R.; Panerai, R.B.; Haeri, S.; Griffioen, A.C.; Zeeman, G.G.; Belfort, M.A. Cerebral autoregulation in normal pregnancy and preeclampsia. Obstet Gynecol. 2013, 122, 1064–1069. [Google Scholar] [CrossRef] [Green Version]
- Bergman, L.; Zetterberg, H.; Kaihola, H.; Hagberg, H.; Blennow, K.; Akerud, H. Blood-based cerebral biomarkers in preeclampsia: Plasma concentrations of NfL, tau, S100B and NSE during pregnancy in women who later develop preeclampsia—A nested case control study. PLoS ONE 2018, 13, e0196025. [Google Scholar] [CrossRef]
- Bergman, L.; Torres-Vergara, P.; Penny, J.; Wikström, J.; Nelander, M.; Leon, J.; Tolcher, M.; Roberts, J.M.; Wikström, A.-K.; Escudero, C. Investigating Maternal Brain Alterations in Preeclampsia: The Need for a Multidisciplinary Effort. Curr. Hypertens. Rep. 2019, 21, 72. [Google Scholar] [CrossRef]
- De Oliveira, L.; Dias, M.A.B.; Jeyabalan, A.; Payne, B.; Redman, C.W.; Magee, L.; Poston, L.; Chappell, L.; Seed, P.; von Dadelszen, P.; et al. Creating biobanks in low and middle-income countries to improve knowledge—The PREPARE initiative. Pregnancy Hypertens. 2018, 13, 62–64. [Google Scholar] [CrossRef]
- Leon, L.J.; Solanky, N.; Stalman, S.E.; Demetriou, C.; Abu-Amero, S.; Stanier, P.; Regan, L.; Moore, G.E. A new biological and clinical resource for research into pregnancy complications: The Baby Bio Bank. Placenta 2016, 46, 31–37. [Google Scholar] [CrossRef] [Green Version]
- Antony, K.M.; Hemarajata, P.; Chen, J.; Morris, J.; Cook, C.; Masalas, D.; Gedminas, M.; Brown, A.; Versalovic, J.; Aagaard, K. Generation and validation of a universal perinatal database and biospecimen repository: PeriBank. J. Perinatol. 2016, 36, 921–929. [Google Scholar] [CrossRef]
- Bergman, L.; Sandström, A.; Jacobsson, B.; Hansson, S.; Lindgren, P.; Larsson, A.; Imberg, H.; Conner, P.; Kublickas, M.; Carlsson, Y.; et al. Study for Improving Maternal Pregnancy and Child ouTcomes (IMPACT): A study protocol for a Swedish prospective multicentre cohort study. BMJ Open 2020, 10, e033851. [Google Scholar] [CrossRef]
- Evers, K.S.; Atkinson, A.; Barro, C.; Fisch, U.; Pfister, M.; Huhn, E.A.; Lapaire, O.; Kuhle, J.; Wellmann, S. Neurofilament as Neuronal Injury Blood Marker in Preeclampsia. Hypertension 2018, 71, 1178–1184. [Google Scholar] [CrossRef]
- Elharram, M.; Dayan, N.; Kaur, A.; Landry, T.; Pilote, L. Long-Term Cognitive Impairment After Preeclampsia: A Systematic Review and Meta-analysis. Obstet Gynecol. 2018, 132, 355–364. [Google Scholar] [CrossRef]
- Hastie, R.; Brownfoot, F.C.; Cluver, C.A.; Walker, S.P.; Hesselman, S.; Tong, S.; Bergman, L. The predictive value of the signs and symptoms preceding eclampsia: A systematic review. Pregnancy Hypertens. 2019, 17, S15. [Google Scholar] [CrossRef]
- Zeeman, G.G.; Cunningham, F.G. Posterior reversible encephalopathy syndrome in 46 of 47 patients with eclampsia. Am. J. Obstet. Gynecol. 2014, 210, 378–379. [Google Scholar] [CrossRef] [PubMed]
- Camara-Lemarroy, C.R.; Escobedo-Zúñiga, N.; Villarreal-Garza, E.; García-Valadez, E.; Góngora-Rivera, F.; Villarreal-Velázquez, H.J. Posterior reversible leukoencephalopathy syndrome (PRES) associated with severe eclampsia: Clinical and biochemical features. Pregnancy Hypertens. 2017, 7, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Zlatnik, M.G. Pulmonary edema: Etiology and treatment. Semin. Perinatol. 1997, 21, 298–306. [Google Scholar] [CrossRef]
- Anthony, J.; Damasceno, A.; Ojjii, D. Hypertensive disorders of pregnancy: What the physician needs to know. Cardiovasc. J. Afr. 2016, 27, 104–110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guirguis, G.F.; Aziz, M.M.; Liang, C.B.; Williams, S.F.; Apuzzio, J.J.; Bilinski, R.; Mornan, A.J.; Shah, L.P. Is preeclampsia an independent predictor of diastolic dysfunction? A retrospective cohort study. Pregnancy Hypertens. 2015, 5, 359–361. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, S.; Sun, N.; Park, A.L.; Hladunewich, M.; Silversides, C.K.; Ray, J.G. The Pulmonary Edema Preeclampsia Evaluation (PEPE) Study. J. Obstet. Gynaecol. Can. 2014, 36, 1065–1070. [Google Scholar] [CrossRef] [Green Version]

| Variables at Inclusion | Variables During Hospital Stay | Variables at Discharge and at 3 Months Follow Up |
|---|---|---|
| Demographics Age (c) | Delivery details Gestation at delivery (c) | Discharge Date of discharge (N/A) |
| Date of birth (N/A) | Indication for delivery (n) | Number of days in hospital (c) |
| Hospital folder number (N/A) | Mode of delivery (n) | Adverse maternal outcomes (n) |
| Address (N/A) | Place and supervision of delivery (n) | Eclampsia |
| Contact number (N/A) | Medication used before delivery (n) | Recurrent eclampsia |
| Race (n) | Maternal plasma sample taken (b) | Severe hypertension |
| Marital status (n) | Cerebrospinal fluid sample taken (b) | Stroke |
| Total years of full-time education (o) | PRES syndrome | |
| Current job situation (n) | Neonatal outcomes | Cortical blindness |
| Current living situation (n) | Liveborn (b) | Severe renal impairment |
| Number of people cohabitating (o) | Sex (b) | Dialysis |
| Diagnosis at inclusion (n) | Intubation at birth (b) | Pulmonary edema |
| Singleton pregnancy (b) Plasma sample taken at inclusion (b) | Birth weight (c) APGAR score at 5 min (o) | Inotropic support Signs of bleeding or DIC |
| Medical history Gravidity (o) Parity (o) Number of miscarriages (o) Number of previous terminations (o) Outcome of previous viable pregnancies (n) Previous pre-eclampsia, number of times (o) Previous pre-eclampsia before 34 weeks (b) New paternity (b) Fertility treatment (n) HIV status (b) If HIV positive, viral load (c) Tobacco use (n) Alcohol use (n) Methamphetamine use (b) Diabetes (n) Previous cardiovascular disease (n) Chronic hypertension(b) If chronic hypertensive, number of medications (o) Anaemia (n) Neurological disease (n) Respiratory disease (n) Renal disease (n) Inflammatory bowel disease (b) Autoimmune disease (o) Depression (b) Heredity for pre-eclampsia (o) First degree relative with hypertensive disorders (b) Partner’s heredity for pre-eclampsia (b) Pre-pregnancy weight (c) Pre-pregnancy height (c) Antenatal care (n) Gestation at first presentation for antenatal care (c) Systolic blood pressure at booking (c) Diastolic blood pressure at booking (c) Proteinuria at booking (o) On hypertensive treatment at booking (b) Aspirin use in this pregnancy (b) Gestation aspirin was started (c) Calcium use in this pregnancy (b) Gestation calcium was started (c) Estimated due date (N/A) Estimated due date calculated by (o) | Cord blood taken (b) Neonatal outcome (n) Placental outcomes Placental sample taken (b) Date for placental sample (N/A) Placental weight (c) Daily hospital forms Days since admitted (n) Highest systolic blood pressure (c) Highest diastolic blood pressure (c) Lowest oxygen saturation (c) Highest respiratory rate (c) Intubated (b) CPAP (b) Antihypertensive medication (n) Magnesium sulphate (b) Nitroglycerin/Tridil (b) Diuretic (b) Special investigations performed (n) Seen by other specialities (n) Haemoglobin (c) Platelets (c) Urea (c) Creatinine (c) Arterial pH (c) Arterial pO2 (c) Arterial pCO2 (c) Arterial lactate (c) Magnesium (c) Blood taken for freezing (b) Transcranial doppler Date and time for examination (N/A) Oxygen saturation when start of measurement (c) Pulse at start of examination (c) Systolic blood pressure at start of examination (c) Diastolic blood pressure at start of examination (85) Oxygen (n) End-tidal CO2 (c) Magnesium sulphate at examination (b) Magnesium sulphate before examination (b) If yes, how many hours since finished (o) Nitroglycerin/Tridil at examination (b) Antihypertensive medication at examination (o) | HELLP syndrome Liver enzymes > 500 IU/L Liver rupture or hematoma Admitted to ICU Maternal death PPH Laparotomy for any reason apart from caesarean section Glasgow Coma Score < 13 Myocardial infarction Intubation Sepsis Coma Venous thromboembolism Intrauterine fetal death Perinatal or infant mortality Abruptio placenta Mild to moderate pre-eclampsia without complications None (pregnant control) Cognitive function testing MoCa (scanned) CFQ (c) Long-term outcome 3-12 months Date (N/A) Neonatal death within 6 weeks after expected due date (b) Neonatal death at any point after discharge (b) Maternal systolic blood pressure (c) Maternal diastolic blood pressure (c) Is mother on blood pressure treatment (b) Final hypertensive diagnosis (n) Any persisting neurological symptoms (b) Glasgow Outcome Scale (o) |
| Symptoms before inclusion Edema (n) Visual disturbances (n) Time of onset for visual disturbances (n) Headache (n) Headache onset (n) Epigastric/abdominal pain (n) Tightness in the chest (b) Shortness of breath (b) Focal neurological deficits (n) Tendon reflexes (n) Nausea (b) Vomit (b) Confusion (b) Twitching or jerking arms or legs (b) People around her noticing that she was absent in mind (b) Difficulty concentrating (b) Speech affected (b) Hearing affected (b) Mood changes (n) Anxiety (b) Feel like end of the world was coming (b) Dizziness (b) Weakness/paralysis (b) Other symptoms not listed (free text) Highest blood pressure before inclusion /fit (c) Highest diastolic blood pressure before inclusion /fit (c) Blood pressure recorded before/after fit (n) Date of convulsion if applicable (N/A) Fitted postpartum (b) Proteinuria (o) Lowest platelet count (c) Highest AST (c) Lowest haemoglobin (c) Highest creatinine (c) Blood pressure medication before the event/inclusion (n) Magnesium sulphate before the event/inclusion (b) If eclamptic fit, where did it occur (n) | GCS score at examination (c) Neurological deficits at start of examination (text) Depth left side (c) Systolic velocity left side (c) Mean velocity left side (c) Diastolic velocity left side (c) Cerebral perfusion pressure left side (c) Autoregulatory index left side (c) Depth right side (c) Systolic velocity right side (c) Mean velocity right side (c) Diastolic velocity right side (c) Cerebral perfusion pressure right side (c) Autoregulatory index right side (c) Brain MRI MRI performed (b) Date of MRI (N/A) MR data saved in the electronic radiology system for later entry Echocardiography and MRI heart Diagnosis of pulmonary edema in relation to delivery (n) Date of echocardiography (N/A) Date of cardiac MRI (N/A) Inclusion criteria (o) If pulmonary oedema, how was diagnosis set (o) Blood sample (b) LV diameter in diastole (c) LV end-systolic diameter (c) Interventricular septal thickness in diastole (c) Posterior wall thickness in diastole (c) LV mass (c) LV mass index (c) Relative wall thickness (c) Left ventricular ejection fraction (by Simpson’s biplane) (c) Fractional shortening (c) Tissue doppler SA wave velocity (c) Myocardial performance index (c) Global longitudinal strain (c) Regional wall motion abnormalities (c) E wave height (c) A wave height (c) E:A ratio (c) E wave deceleration time (c) Isovolumetric relaxation time (c) E’ septal (c) E’ lateral (c) E’average (c) E:E’septal (c) E:E’lateral (c) E:E’average (c) Pulmonary vein pulse wave doppler (c) Left atrial diameter (c) Left atrial area (c) Left atrial volume (c) Left atrial volume indexed to BSA (c) |
| Type of Sample | Sampling | Volume | Tubes, Processing |
|---|---|---|---|
| Blood | At inclusion, at delivery, during hospital stay | Maximum of 12 mL/sample | EDTA plasma, spinned, 1 mL aliquots |
| Placenta: foetal surface | At delivery | RNAlater, 4 × 1 cm3 | Removal of RNA later, 2 mL aliquots |
| Placenta: foetal surface | At delivery | Frozen sections 1 cm3 | 2 mL aliquots |
| Placenta: maternal surface | At delivery | RNAlater, 4 × 1 cm3 | Removal of RNA later, 2 mL aliquots |
| Placenta: maternal surface | At delivery | Frozen sections 1 cm3 | 2 mL aliquots |
| Cord Blood (mixed venous–arterial) | At delivery | Maximum 12 mL | EDTA plasma, spinned, 1 mL aliquots |
| Urine | At inclusion | Maximum 12 mL | Sterile tube, spinned, 1 mL aliquots |
| Cerebrospinal fluid | At delivery | Maximum 2 mL | Sterile tube, spinned, 1 mL aliquots |
| Saliva | At inclusion | Stored in a 3 cc cup | 2 mL aliquots |
| Neurology * | Pulmonary Oedema | HELLP/Renal Impairment | Pre-Eclampsia ** | Normotensive | |
|---|---|---|---|---|---|
| n | 86 | 43 | 23 | 54 | 38 |
| AT BASELINE | |||||
| Maternal age (years) | 22.8 (6.1) | 28.8 (6.9) | 29.2 (6.8) | 26.1 (5.8) | 29.1 (6.3) |
| Nulliparous n (%) | 60 (70) | 18 (42) | 7 (30) | 28 (52) | 9 (24) |
| BMI (kg/m2) | 26.4 (8.1) | 32.2 (9.2) | 29.8 (6.4) | 29.1 (7.3) | 27.6 (6.8) |
| Missing *** | 16 | 5 | 7 | 3 | 4 |
| HIV n (%) | 10 (12) | 11 (26) | 6 (26) | 8 (15) | 7 (18) |
| Chronic hypertension n (%) | 7 (8) | 2 (5) | 5 (22) | 9 (17) | 0 (0) |
| Gestation at first presentation for antenatal care (weeks) | 17.4 (8) | 15.3 (7.6) | 18.0 (6.9) | 16.0 (7.4) | 16.6 (7.7) |
| AFTER INCLUSION | |||||
| Gestation at delivery (weeks) | 33.4 (4.3) | 31.8 (5.0) | 30.6 (5.0) | 34.0 (4.2) | 36.1 (3.9) |
| Mode of delivery n (%) | |||||
| Vaginal | 25 (29) | 11 (26) | 8 (35) | 15 (28) | 8 (21) |
| Planned CS | 1 (1) | 2 (5) | 0 (0) | 5 (9) | 24 (63) |
| Emergency CS | 60 (70) | 30 (70) | 15 (65) | 34 (63) | 6 (16) |
| Birthweight (grams) | 2093 (906) | 1748 (969) | 1315 (588) | 2078 (961) | 2761 (877) |
| OUTCOMES n (%) | |||||
| Severe hypertension | 35 (41) | 29 (67) | 16 (70) | 14 (26) | 0 (0) |
| Eclampsia | 82 (95) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Recurrent eclampsia | 26 (30) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| GCS < 13 | 22 (26) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Stroke | 3 (4) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Blindness | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Pulmonary oedema | 5 (6) | 43 (100) | 3 (13) | 0 (0) | 0 (0) |
| HELLP | 19 (22) | 7 (16) | 22 (96) | 1 (2) | 0 (0) |
| Renal impairment | 16 (19) | 5 (12) | 9 (39) | 1 (2) | 0 (0) |
| Admitted to ICU | 10 (12) | 6 (14) | 1 (4) | 0 (0) | 0 (0) |
| Postpartum haemorrhage | 9 (11) | 3 (7) | 2 (13) | 3 (5) | 2 (4) |
| Intubation | 15 (17) | 6 (14) | 1 (4) | 0 (0) | 0 (0) |
| Intrauterine foetal death | 12 (14) | 8 (19) | 7 (30) | 5 (9) | 0 (0) |
| Venous thromboembolism | 2 (2) | 1 (2) | 0 (0) | 0 (0) | 0 (0) |
| Abruptio placentae | 5 (6) | 2 (5) | 2 (9) | 2 (4) | 1 (3) |
| GOS at two months | |||||
| Mild or no disability | 63 (96) | 33 (100) | 10 (100) | 42 (100) | 26 (100) |
| Severe disability | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Death | 2 (3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 20 | 10 | 13 | 12 | 12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bergman, L.; Bergman, K.; Langenegger, E.; Moodley, A.; Griffith-Richards, S.; Wikström, J.; Hall, D.; Joubert, L.; Herbst, P.; Schell, S.; et al. PROVE—Pre-Eclampsia Obstetric Adverse Events: Establishment of a Biobank and Database for Pre-Eclampsia. Cells 2021, 10, 959. https://doi.org/10.3390/cells10040959
Bergman L, Bergman K, Langenegger E, Moodley A, Griffith-Richards S, Wikström J, Hall D, Joubert L, Herbst P, Schell S, et al. PROVE—Pre-Eclampsia Obstetric Adverse Events: Establishment of a Biobank and Database for Pre-Eclampsia. Cells. 2021; 10(4):959. https://doi.org/10.3390/cells10040959
Chicago/Turabian StyleBergman, Lina, Karl Bergman, Eduard Langenegger, Ashley Moodley, Stephanie Griffith-Richards, Johan Wikström, David Hall, Lloyd Joubert, Philip Herbst, Sonja Schell, and et al. 2021. "PROVE—Pre-Eclampsia Obstetric Adverse Events: Establishment of a Biobank and Database for Pre-Eclampsia" Cells 10, no. 4: 959. https://doi.org/10.3390/cells10040959
APA StyleBergman, L., Bergman, K., Langenegger, E., Moodley, A., Griffith-Richards, S., Wikström, J., Hall, D., Joubert, L., Herbst, P., Schell, S., van Veen, T., Belfort, M., Tong, S. Y. C., Walker, S., Hastie, R., & Cluver, C. (2021). PROVE—Pre-Eclampsia Obstetric Adverse Events: Establishment of a Biobank and Database for Pre-Eclampsia. Cells, 10(4), 959. https://doi.org/10.3390/cells10040959