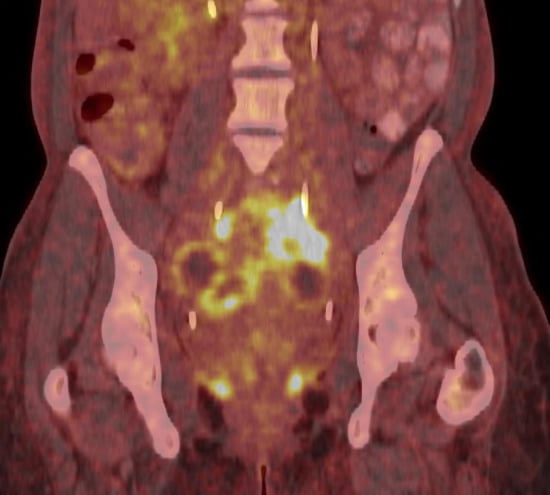
Pelvic Actinomycosis Associated with an Intrauterine Contraceptive Device Demonstrated on F-18 FDG PET/CT
Abstract
:
Author Contributions
Conflicts of Interest
References
- Garner, J.P.; Macdonald, M.; Kumar, P.K. Abdominal actinomycosis. Int. J. Surg. 2007, 5, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Fiorino, A.S. Intrauterine contraceptive device-associated actinomycotic abscess and Actinomyces detection on cervical smear. Obstet. Gynecol. 1996, 87, 142–149. [Google Scholar] [CrossRef]
- Kumar, N.; Das, P.; Kumar, D.; Kriplani, A.; Ray, R. Pelvic actinomycosis mimicking: An advanced ovarian cancer. Indian J. Pathol. Microbiol. 2010, 53, 164–165. [Google Scholar] [PubMed]
- Lely, R.J.; van Es, H.W. Case 85: Pelvic actinomycosis in association with an intrauterine device. Radiology 2005, 236, 492–494. [Google Scholar] [CrossRef] [PubMed]
- Akhan, S.E.; Dogan, Y.; Akhan, S.; Iyibozkurt, A.C.; Topuz, S.; Yalcin, O. Pelvic actinomycosis mimicking ovarian malignancy: Three cases. Eur. J. Gynaecol. Oncol. 2008, 29, 294–297. [Google Scholar] [PubMed]
- Weese, W.C.; Smith, I.M. A study of 57 cases of actinomycosis over a 36-year period. A diagnostic ‘failure’ with good prognosis after treatment. Arch. Intern. Med. 1975, 135, 1562–1568. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, M.S.; Roberts, W.S.; Solomon, P.; Gunasekarin, S.; Cavanagh, D. Advanced actinomycotic pelvic inflammatory disease simulating gynecologic malignancy. A report of two cases. J. Reprod. Med. 1991, 36, 543–545. [Google Scholar] [PubMed]
- Koshiyama, M.; Yoshida, M.; Fujii, H.; Nanno, H.; Hayashi, M.; Tauchi, K.; Kaji, Y. Ovarian actinomycosis complicated by diabetes mellitus simulating an advanced ovarian carcinoma. Eur. J. Obstet. Gynecol. Reprod. Biol. 1999, 87, 95–99. [Google Scholar] [CrossRef]
- Ha, H.K.; Lee, H.J.; Kim, H.; Ro, H.J.; Park, Y.H.; Cha, S.J.; Shinn, K.S. Abdominal actinomycosis: CT findings in 10 patients. AJR Am. J. Roentgenol. 1993, 161, 791–794. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dejanović, D.; Ahnlide, J.A.; Nilsson, C.; Berthelsen, A.K.; Loft, A. Pelvic Actinomycosis Associated with an Intrauterine Contraceptive Device Demonstrated on F-18 FDG PET/CT. Diagnostics 2015, 5, 369-371. https://doi.org/10.3390/diagnostics5030369
Dejanović D, Ahnlide JA, Nilsson C, Berthelsen AK, Loft A. Pelvic Actinomycosis Associated with an Intrauterine Contraceptive Device Demonstrated on F-18 FDG PET/CT. Diagnostics. 2015; 5(3):369-371. https://doi.org/10.3390/diagnostics5030369
Chicago/Turabian StyleDejanović, Danijela, Jan Anders Ahnlide, Cecilia Nilsson, Anne Kiil Berthelsen, and Annika Loft. 2015. "Pelvic Actinomycosis Associated with an Intrauterine Contraceptive Device Demonstrated on F-18 FDG PET/CT" Diagnostics 5, no. 3: 369-371. https://doi.org/10.3390/diagnostics5030369
APA StyleDejanović, D., Ahnlide, J. A., Nilsson, C., Berthelsen, A. K., & Loft, A. (2015). Pelvic Actinomycosis Associated with an Intrauterine Contraceptive Device Demonstrated on F-18 FDG PET/CT. Diagnostics, 5(3), 369-371. https://doi.org/10.3390/diagnostics5030369