Liquid Biopsy Potential Biomarkers in Prostate Cancer
Abstract
:1. Introduction
2. Current PCa Diagnostics
3. Current PCa Biomarker Tests for Discrimination-Significant and Indolent PCa
3.1. Prostate-Specific Antigen (PSA)
3.2. Prostate Health Index and Derivates
3.3. 4KScore® Test
3.4. Progensa™ (Gen-Probe Inc., San Diego, CA, USA)
3.5. Further Non-Commercial and Integrative Tests
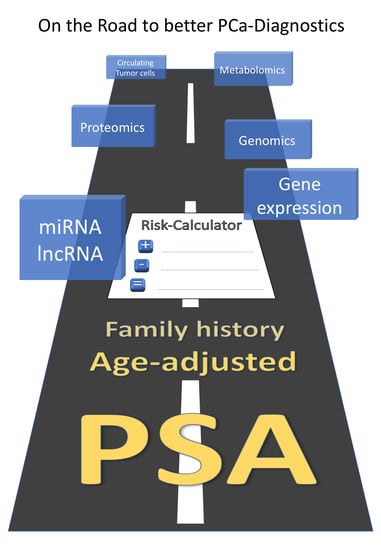
4. Do We Need More Biomarkers, or Do We Need a New, Consistent Concept?
5. Emerging Biomarkers for Detection of Significant PCa
5.1. Polypeptides
5.2. Metabolites
5.3. MicroRNA (miRNA)
5.4. Gene Expression of PCa-Related Genes in Exosomes
5.5. Long Non-Coding RNA (lncRNA)
5.6. Circulating Tumour Cells (CTC)
6. Integrative Scoring Systems/Risk Calculators
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Available online: http://globocan.iarc.fr (accessed on 1 July 2018).
- Chen, W.; Zheng, R.; Baade, P.D.; Zhang, S.; Zeng, H.; Bray, F.; Jemal, A.; Yu, X.Q.; He, J. Cancer statistics in China, 2015. CA Cancer J. Clin. 2016, 66, 115–132. [Google Scholar] [CrossRef] [PubMed]
- Ervik, M.; Lam, F.; Ferlay, J.; Mery, L.; Soerjomataram, I.; Bray, F. Cancer Today. Lyon, France: International Agency for Research on Cancer; Cancer Today: Lyon, France, 2016; Available online: http://gco.iarc.fr/today (accessed on 28 August 2016).
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2016. CA Cancer J. Clin. 2016, 66, 7–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lowrance, W.T.; Murad, M.H.; Oh, W.K.; Jarrard, D.F.; Resnick, M.J.; Cookson, M.S. Castration-Resistant Prostate Cancer: AUA Guideline Amendment 2018. J. Urol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Mottet, N.; Bellmunt, J.; Bolla, M.; Briers, E.; Cumberbatch, M.G.; De Santis, M.; Fossati, N.; Gross, T.; Henry, A.M.; Joniau, S.; et al. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur. Urol. 2017, 71, 618–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carter, H.B. American Urological Association (AUA) guideline on prostate cancer detection: Process and rationale. BJU Int. 2013, 112, 543–547. [Google Scholar] [CrossRef] [PubMed]
- Leyten, G.H.; Hessels, D.; Jannink, S.A.; Smit, F.P.; de Jong, H.; Cornel, E.B.; de Reijke, T.M.; Vergunst, H.; Kil, P.; Knipscheer, B.C.; et al. Prospective multicentre evaluation of PCA3 and TMPRSS2-ERG gene fusions as diagnostic and prognostic urinary biomarkers for prostate cancer. Eur. Urol. 2014, 65, 534–542. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.; Friend, C.; Dreher, A.; Allgar, V.; Macleod, U. The diagnostic test accuracy of rectal examination for prostate cancer diagnosis in symptomatic patients: A systematic review. BMC Fam. Pract. 2018, 19, 79. [Google Scholar] [CrossRef] [PubMed]
- Smeenge, M.; Barentsz, J.; Cosgrove, D.; de la Rosette, J.; de Reijke, T.; Eggener, S.; Frauscher, F.; Kovacs, G.; Matin, S.F.; Mischi, M.; et al. Role of transrectal ultrasonography (TRUS) in focal therapy of prostate cancer: Report from a Consensus Panel. BJU Int. 2012, 110, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Haas, G.P.; Delongchamps, N.B.; Jones, R.F.; Chandan, V.; Serio, A.M.; Vickers, A.J.; Jumbelic, M.; Threatte, G.; Korets, R.; Lilja, H.; et al. Needle biopsies on autopsy prostates: Sensitivity of cancer detection based on true prevalence. J. Natl. Cancer Inst. 2007, 99, 1484–1489. [Google Scholar] [CrossRef] [PubMed]
- Stamey, T.A.; Yang, N.; Hay, A.R.; McNeal, J.E.; Freiha, F.S.; Redwine, E. Prostate-specific antigen as a serum marker for adenocarcinoma of the prostate. N. Engl. J. Med. 1987, 317, 909–916. [Google Scholar] [CrossRef] [PubMed]
- Cooperberg, M.R.; Lubeck, D.P.; Mehta, S.S.; Carroll, P.R. Time trends in clinical risk stratification for prostate cancer: Implications for outcomes (data from CaPSURE). J. Urol. 2003, 170, S21–S27. [Google Scholar] [CrossRef] [PubMed]
- Schröder, F.H.; Hugosson, J.; Roobol, M.J.; Tammela, T.L.; Zappa, M.; Nelen, V.; Kwiatkowski, M.; Lujan, M.; Määttänen, L.; Lilja, H.; et al. Screening and prostate cancer mortality: Results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet 2014, 384, 2027–2035. [Google Scholar] [CrossRef]
- Brawley, O.W. Prostate cancer epidemiology in the United States. World J. Urol. 2012, 30, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Neppl-Huber, C.; Zappa, M.; Coebergh, J.W.; Rapiti, E.; Rachtan, J.; Holleczek, B.; Rosso, S.; Aareleid, T.; Brenner, H.; Gondos, A.; EUNICE Survival Working Group. Changes in incidence, survival and mortality of prostate cancer in Europe and the United States in the PSA era: Additional diagnoses and avoided deaths. Ann. Oncol. 2012, 23, 1325–1334. [Google Scholar] [CrossRef] [PubMed]
- Leidinger, P.; Keller, A.; Milchram, L.; Harz, C.; Hart, M.; Werth, A.; Lenhof, H.P.; Weinhäusel, A.; Keck, B.; Wullich, B.; et al. Combination of Autoantibody Signature with PSA Level Enables a Highly Accurate Blood-Based Differentiation of Prostate Cancer Patients from Patients with Benign Prostatic Hyperplasia. PLoS ONE 2015, 10, e0128235. [Google Scholar] [CrossRef] [PubMed]
- Moyer, V.A.; U.S. Preventive Services Task Force. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 2012, 157, 120–134. [Google Scholar] [CrossRef] [PubMed]
- Howrey, B.T.; Kuo, Y.F.; Lin, Y.L.; Goodwin, J.S. The impact of PSA screening on prostate cancer mortality and overdiagnosis of prostate cancer in the United States. J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Draisma, G.; Etzioni, R.; Tsodikov, A.; Mariotto, A.; Wever, E.; Gulati, R.; Feuer, E.; de Koning, H. Lead time and overdiagnosis in prostate-specific antigen screening: Importance of methods and context. J. Natl. Cancer Inst. 2009, 101, 374–383. [Google Scholar] [CrossRef] [PubMed]
- Heidegger, I.; Skradski, V.; Steiner, E.; Klocker, H.; Pichler, R.; Pircher, A.; Horninger, W.; Bektic, J. High risk of under-grading and -staging in prostate cancer patients eligible for active surveillance. PLoS ONE 2015, 10, e0115537. [Google Scholar] [CrossRef] [PubMed]
- Thompson, I.M.; Pauler, D.K.; Goodman, P.J.; Tangen, C.M.; Lucia, M.S.; Parnes, H.L.; Minasian, L.M.; Ford, L.G.; Lippman, S.M.; Crawford, E.D.; et al. Prevalence of prostate cancer among men with a prostate-specific antigen level < or = 4.0 ng per milliliter. N. Engl. J. Med. 2004, 350, 2239–2246. [Google Scholar] [CrossRef] [PubMed]
- Veltri, R.W.; Miller, M.C.; O’dowd, G.J.; Partin, A.W. Impact of age on total and complexed prostate-specific antigen cutoffs in a contemporary referral series of men with prostate cancer. Urology 2002, 60, 47–52. [Google Scholar] [CrossRef]
- U.S. Preventive Services Task Force. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 2008, 149, 185–191. [Google Scholar] [CrossRef]
- Carter, H.B.; Albertsen, P.C.; Barry, M.J.; Etzioni, R.; Freedland, S.J.; Greene, K.L.; Holmberg, L.; Kantoff, P.; Konety, B.R.; Murad, M.H.; et al. Early detection of prostate cancer: AUA Guideline. J. Urol. 2013, 190, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Auffenberg, G.B.; Meeks, J.J. Application of the 2013 American Urological Association early detection of prostate cancer guideline: Who will we miss. World J. Urol. 2014, 32, 959–964. [Google Scholar] [CrossRef] [PubMed]
- Jemal, A.; Fedewa, S.A.; Ma, J.; Siegel, R.; Lin, C.C.; Brawley, O.; Ward, E.M. Prostate Cancer Incidence and PSA Testing Patterns in Relation to USPSTF Screening Recommendations. JAMA 2015, 314, 2054–2061. [Google Scholar] [CrossRef] [PubMed]
- Vertosick, E.A.; Poon, B.Y.; Vickers, A.J. Relative value of race, family history and prostate specific antigen as indications for early initiation of prostate cancer screening. J. Urol. 2014, 192, 724–728. [Google Scholar] [CrossRef] [PubMed]
- Gershman, B.; Van Houten, H.K.; Herrin, J.; Moreira, D.M.; Kim, S.P.; Shah, N.D.; Karnes, R.J. Impact of Prostate-specific Antigen (PSA) Screening Trials and Revised PSA Screening Guidelines on Rates of Prostate Biopsy and Postbiopsy Complications. Eur. Urol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Alford, A.V.; Brito, J.M.; Yadav, K.K.; Yadav, S.S.; Tewari, A.K.; Renzulli, J. The Use of Biomarkers in Prostate Cancer Screening and Treatment. Rev. Urol. 2017, 19, 221–234. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Li, Z.Z.; Huang, Y.L.; Song, H.J.; Wang, Y.J. Value of free/total prostate-specific antigen (f/t PSA) ratios for prostate cancer detection in patients with total serum prostate-specific antigen between 4 and 10 ng/mL: A. meta-analysis. Medicine 2018, 97, e0249. [Google Scholar] [CrossRef] [PubMed]
- Carter, H.B.; Pearson, J.D.; Metter, E.J.; Brant, L.J.; Chan, D.W.; Andres, R.; Fozard, J.L.; Walsh, P.C. Longitudinal evaluation of prostate-specific antigen levels in men with and without prostate disease. JAMA 1992, 267, 2215–2220. [Google Scholar] [CrossRef] [PubMed]
- Catalona, W.J.; Smith, D.S.; Ratliff, T.L.; Dodds, K.M.; Coplen, D.E.; Yuan, J.J.; Petros, J.A.; Andriole, G.L. Measurement of prostate-specific antigen in serum as a screening test for prostate cancer. N. Engl. J. Med. 1991, 324, 1156–1161. [Google Scholar] [CrossRef] [PubMed]
- Loeb, S.; Sanda, M.G.; Broyles, D.L.; Shin, S.S.; Bangma, C.H.; Wei, J.T.; Partin, A.W.; Klee, G.G.; Slawin, K.M.; Marks, L.S.; et al. The prostate health index selectively identifies clinically significant prostate cancer. J. Urol. 2015, 193, 1163–1169. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Wang, M.; Wang, L.; Adams, T.S.; Tian, Y.; Xu, J. Diagnostic ability of %p2PSA and prostate health index for aggressive prostate cancer: A meta-analysis. Sci. Rep. 2014, 4, 5012. [Google Scholar] [CrossRef] [PubMed]
- Bryant, R.J.; Sjoberg, D.D.; Vickers, A.J.; Robinson, M.C.; Kumar, R.; Marsden, L.; Davis, M.; Scardino, P.T.; Donovan, J.; Neal, D.E.; et al. Predicting high-grade cancer at ten-core prostate biopsy using four kallikrein markers measured in blood in the ProtecT study. J. Natl. Cancer Inst. 2015, 107. [Google Scholar] [CrossRef] [PubMed]
- Schipper, M.; Wang, G.; Giles, N.; Ohrnberger, J. Novel prostate cancer biomarkers derived from autoantibody signatures. Transl. Oncol. 2015, 8, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Yu, J.; Sreekumar, A.; Varambally, S.; Shen, R.; Giacherio, D.; Mehra, R.; Montie, J.E.; Pienta, K.J.; Sanda, M.G.; et al. Autoantibody signatures in prostate cancer. N. Engl. J. Med. 2005, 353, 1224–1235. [Google Scholar] [CrossRef] [PubMed]
- Marks, L.S.; Fradet, Y.; Deras, I.L.; Blase, A.; Mathis, J.; Aubin, S.M.; Cancio, A.T.; Desaulniers, M.; Ellis, W.J.; Rittenhouse, H.; et al. PCA3 molecular urine assay for prostate cancer in men undergoing repeat biopsy. Urology 2007, 69, 532–535. [Google Scholar] [CrossRef] [PubMed]
- Gittelman, M.C.; Hertzman, B.; Bailen, J.; Williams, T.; Koziol, I.; Henderson, R.J.; Efros, M.; Bidair, M.; Ward, J.F. PCA3 molecular urine test as a predictor of repeat prostate biopsy outcome in men with previous negative biopsies: A prospective multicenter clinical study. J. Urol. 2013, 190, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.T.; Feng, Z.; Partin, A.W.; Brown, E.; Thompson, I.; Sokoll, L.; Chan, D.W.; Lotan, Y.; Kibel, A.S.; Busby, J.E.; et al. Can urinary PCA3 supplement PSA in the early detection of prostate cancer. J. Clin. Oncol. 2014, 32, 4066–4072. [Google Scholar] [CrossRef] [PubMed]
- McKiernan, J.; Donovan, M.J.; O’Neill, V.; Bentink, S.; Noerholm, M.; Belzer, S.; Skog, J.; Kattan, M.W.; Partin, A.; Andriole, G.; et al. A Novel Urine Exosome Gene Expression Assay to Predict High-grade Prostate Cancer at Initial Biopsy. JAMA Oncol. 2016, 2, 882–889. [Google Scholar] [CrossRef] [PubMed]
- Tomlins, S.A.; Day, J.R.; Lonigro, R.J.; Hovelson, D.H.; Siddiqui, J.; Kunju, L.P.; Dunn, R.L.; Meyer, S.; Hodge, P.; Groskopf, J.; et al. Urine TMPRSS2:ERG Plus PCA3 for Individualized Prostate Cancer Risk Assessment. Eur. Urol. 2016, 70, 45–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Neste, L.; Hendriks, R.J.; Dijkstra, S.; Trooskens, G.; Cornel, E.B.; Jannink, S.A.; de Jong, H.; Hessels, D.; Smit, F.P.; Melchers, W.J.; et al. Detection of High-grade Prostate Cancer Using a Urinary Molecular Biomarker-Based Risk Score. Eur. Urol. 2016, 70, 740–748. [Google Scholar] [CrossRef] [PubMed]
- Grönberg, H.; Adolfsson, J.; Aly, M.; Nordström, T.; Wiklund, P.; Brandberg, Y.; Thompson, J.; Wiklund, F.; Lindberg, J.; Clements, M.; et al. Prostate cancer screening in men aged 50-69 years (STHLM3): A prospective population-based diagnostic study. Lancet Oncol. 2015, 16, 1667–1676. [Google Scholar] [CrossRef]
- Le, B.V.; Griffin, C.R.; Loeb, S.; Carvalhal, G.F.; Kan, D.; Baumann, N.A.; Catalona, W.J. [–2] Proenzyme prostate specific antigen is more accurate than total and free prostate specific antigen in differentiating prostate cancer from benign disease in a prospective prostate cancer screening study. J. Urol. 2010, 183, 1355–1359. [Google Scholar] [CrossRef] [PubMed]
- Filella, X.; Giménez, N. Evaluation of [–2] proPSA and Prostate Health Index (phi) for the detection of prostate cancer: A systematic review and meta-analysis. Clin. Chem. Lab. Med. 2013, 51, 729–739. [Google Scholar] [CrossRef] [PubMed]
- White, J.; Shenoy, B.V.; Tutrone, R.F.; Karsh, L.I.; Saltzstein, D.R.; Harmon, W.J.; Broyles, D.L.; Roddy, T.E.; Lofaro, L.R.; Paoli, C.J.; et al. Clinical utility of the Prostate Health Index (phi) for biopsy decision management in a large group urology practice setting. Prostate Cancer Prostatic Dis. 2018, 21, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Fossati, N.; Buffi, N.M.; Haese, A.; Stephan, C.; Larcher, A.; McNicholas, T.; de la Taille, A.; Freschi, M.; Lughezzani, G.; Abrate, A.; et al. Preoperative Prostate-specific Antigen Isoform p2PSA and Its Derivatives, %p2PSA and Prostate Health Index, Predict Pathologic Outcomes in Patients Undergoing Radical Prostatectomy for Prostate Cancer: Results from a Multicentric European Prospective Study. Eur. Urol. 2015, 68, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Ploussard, G.; Durand, X.; Xylinas, E.; Moutereau, S.; Radulescu, C.; Forgue, A.; Nicolaiew, N.; Terry, S.; Allory, Y.; Loric, S. Prostate cancer antigen 3 score accurately predicts tumour volume and might help in selecting prostate cancer patients for active surveillance. Eur. Urol. 2011, 59, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Vickers, A.J. Markers for the early detection of prostate cancer: Some principles for statistical reporting and interpretation. J. Clin. Oncol. 2014, 32, 4033–4034. [Google Scholar] [CrossRef] [PubMed]
- Tilki, D.; Evans, C.P. The changing landscape of advanced and castration resistant prostate cancer: Latest science and revised definitions. Can. J. Urol. 2014, 21, 7–13. [Google Scholar] [PubMed]
- Drake, R.R.; Elschenbroich, S.; Lopez-Perez, O.; Kim, Y.; Ignatchenko, V.; Ignatchenko, A.; Nyalwidhe, J.O.; Basu, G.; Wilkins, C.E.; Gjurich, B.; et al. In-depth proteomic analyses of direct expressed prostatic secretions. J. Proteome Res. 2010, 9, 2109–2116. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Ignatchenko, V.; Yao, C.Q.; Kalatskaya, I.; Nyalwidhe, J.O.; Lance, R.S.; Gramolini, A.O.; Troyer, D.A.; Stein, L.D.; Boutros, P.C.; et al. Identification of differentially expressed proteins in direct expressed prostatic secretions of men with organ-confined versus extracapsular prostate cancer. Mol. Cell. Proteom. 2012, 11, 1870–1884. [Google Scholar] [CrossRef] [PubMed]
- Neuhaus, J.; Schiffer, E.; von Wilcke, P.; Bauer, H.W.; Leung, H.; Siwy, J.; Ulrici, W.; Paasch, U.; Horn, L.-C.; Stolzenburg, J.U. Seminal Plasma as a Source of Prostate Cancer Peptide Biomarker Candidates for Detection of Indolent and Advanced Disease. PLoS ONE 2013, 8, e67514. [Google Scholar] [CrossRef] [PubMed]
- Theodorescu, D.; Schiffer, E.; Bauer, H.W.; Douwes, F.; Eichhorn, F.; Polley, R.; Schmidt, T.; Schofer, W.; Zurbig, P.; Good, D.M.; et al. Discovery and validation of urinary biomarkers for prostate cancer. Proteom. Clin. Appl. 2008, 2, 556–570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McDunn, J.E.; Li, Z.; Adam, K.P.; Neri, B.P.; Wolfert, R.L.; Milburn, M.V.; Lotan, Y.; Wheeler, T.M. Metabolomic signatures of aggressive prostate cancer. Prostate 2013, 73, 1547–1560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koutros, S.; Meyer, T.E.; Fox, S.D.; Issaq, H.J.; Veenstra, T.D.; Huang, W.Y.; Yu, K.; Albanes, D.; Chu, L.W.; Andriole, G.; et al. Prospective evaluation of serum sarcosine and risk of prostate cancer in the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial. Carcinogenesis 2013, 34, 2281–2285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sroka, W.D.; Boughton, B.A.; Reddy, P.; Roessner, U.; Słupski, P.; Jarzemski, P.; Dąbrowska, A.; Markuszewski, M.J.; Marszałł, M.P. Determination of amino acids in urine of patients with prostate cancer and benign prostate growth. Eur. J. Cancer Prev. 2017, 26, 131–134. [Google Scholar] [CrossRef] [PubMed]
- Clos-Garcia, M.; Loizaga-Iriarte, A.; Zuñiga-Garcia, P.; Sánchez-Mosquera, P.; Rosa Cortazar, A.; González, E.; Torrano, V.; Alonso, C.; Pérez-Cormenzana, M.; Ugalde-Olano, A.; et al. Metabolic alterations in urine extracellular vesicles are associated to prostate cancer pathogenesis and progression. J. Extracell. Vesicles 2018, 7, 1470442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmidt, J.A.; Fensom, G.K.; Rinaldi, S.; Scalbert, A.; Appleby, P.N.; Achaintre, D.; Gicquiau, A.; Gunter, M.J.; Ferrari, P.; Kaaks, R.; et al. Pre-diagnostic metabolite concentrations and prostate cancer risk in 1077 cases and 1077 matched controls in the European Prospective Investigation into Cancer and Nutrition. BMC Med. 2017, 15, 122. [Google Scholar] [CrossRef] [PubMed]
- Song, C.J.; Chen, H.; Chen, L.Z.; Ru, G.M.; Guo, J.J.; Ding, Q.N. The potential of microRNAs as human prostate cancer biomarkers: A meta-analysis of related studies. J. Cell. Biochem. 2018, 119, 2763–2786. [Google Scholar] [CrossRef] [PubMed]
- Lim, M.; Baird, A.-M.; Aird, J.; Greene, J.; Kapoor, D.; Gray, S.; McDermott, R.; Finn, S. RNAs as Candidate Diagnostic and Prognostic Markers of Prostate Cancer‚ ÄîFrom Cell Line Models to Liquid Biopsies. Diagnostics 2018, 8, 60. [Google Scholar] [CrossRef] [PubMed]
- Walter, B.A.; Valera, V.A.; Pinto, P.A.; Merino, M.J. Comprehensive microRNA Profiling of Prostate Cancer. J. Cancer 2013, 4, 350–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaefer, A.; Jung, M.; Mollenkopf, H.J.; Wagner, I.; Stephan, C.; Jentzmik, F.; Miller, K.; Lein, M.; Kristiansen, G.; Jung, K. Diagnostic and prognostic implications of microRNA profiling in prostate carcinoma. Int. J. Cancer 2010, 126, 1166–1176. [Google Scholar] [CrossRef] [PubMed]
- Stephan, C.; Jung, M.; Rabenhorst, S.; Kilic, E.; Jung, K. Urinary miR-183 and miR-205 do not surpass PCA3 in urine as predictive markers for prostate biopsy outcome despite their highly dysregulated expression in prostate cancer tissue. Clin. Chem. Lab. Med. 2015, 53, 1109–1118. [Google Scholar] [CrossRef] [PubMed]
- Kosaka, N.; Iguchi, H.; Ochiya, T. Circulating microRNA in body fluid: A new potential biomarker for cancer diagnosis and prognosis. Cancer Sci. 2010, 101, 2087–2092. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, P.S.; Parkin, R.K.; Kroh, E.M.; Fritz, B.R.; Wyman, S.K.; Pogosova-Agadjanyan, E.L.; Peterson, A.; Noteboom, J.; O’Briant, K.C.; Allen, A.; et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc. Natl. Acad. Sci. USA 2008, 105, 10513–10518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Porzycki, P.; Ciszkowicz, E.; Semik, M.; Tyrka, M. Combination of three miRNA (miR-141, miR-21, and miR-375) as potential diagnostic tool for prostate cancer recognition. Int. Urol. Nephrol. 2018, 50, 1619–1626. [Google Scholar] [CrossRef] [PubMed]
- Tinay, I.; Tan, M.; Gui, B.; Werner, L.; Kibel, A.S.; Jia, L. Functional roles and potential clinical application of miRNA-345-5p in prostate cancer. Prostate 2018, 78, 927–937. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, M.; Bajo-Santos, C.; Hessvik, N.P.; Lorenz, S.; Fromm, B.; Berge, V.; Sandvig, K.; Linē, A.; Llorente, A. Identification of non-invasive miRNAs biomarkers for prostate cancer by deep sequencing analysis of urinary exosomes. Mol. Cancer 2017, 16, 156. [Google Scholar] [CrossRef] [PubMed]
- Stuopelyte, K.; Daniunaite, K.; Bakavicius, A.; Lazutka, J.R.; Jankevicius, F.; Jarmalaite, S. The utility of urine-circulating miRNAs for detection of prostate cancer. Br. J. Cancer 2016, 115, 707–715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mihelich, B.L.; Maranville, J.C.; Nolley, R.; Peehl, D.M.; Nonn, L. Elevated serum microRNA levels associate with absence of high-grade prostate cancer in a retrospective cohort. PLoS ONE 2015, 10, e0124245. [Google Scholar] [CrossRef] [PubMed]
- Tang, Q.; Hann, S.S. HOTAIR: An Oncogenic Long Non-Coding RNA in Human Cancer. Cell. Physiol. Biochem. 2018, 47, 893–913. [Google Scholar] [CrossRef] [PubMed]
- Huarte, M. The emerging role of lncRNAs in cancer. Nat. Med. 2015, 21, 1253–1261. [Google Scholar] [CrossRef] [PubMed]
- Rinn, J.L.; Chang, H.Y. Genome regulation by long noncoding RNAs. Annu. Rev. Biochem. 2012, 81, 145–166. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Miao, Z.; Xue, B.; Shan, Y.; Weng, G.; Shen, B. Long Non-coding RNAs in Urologic Malignancies: Functional Roles and Clinical Translation. J. Cancer 2016, 7, 1842–1855. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martens-Uzunova, E.S.; Böttcher, R.; Croce, C.M.; Jenster, G.; Visakorpi, T.; Calin, G.A. Long noncoding RNA in prostate, bladder, and kidney cancer. Eur. Urol. 2014, 65, 1140–1151. [Google Scholar] [CrossRef] [PubMed]
- Dong, L.; Ding, H.; Li, Y.; Xue, D.; Liu, Y. LncRNA TINCR is associated with clinical progression and serves as tumor suppressive role in prostate cancer. Cancer Manag. Res. 2018, 10, 2799–2807. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Ren, S.C.; Shi, X.L.; Liu, Y.W.; Zhu, Y.S.; Jing, T.L.; Wang, F.B.; Chen, R.; Xu, C.L.; Wang, H.Q.; et al. A novel urinary long non-coding RNA transcript improves diagnostic accuracy in patients undergoing prostate biopsy. Prostate 2015, 75, 653–661. [Google Scholar] [CrossRef] [PubMed]
- Mehra, R.; Udager, A.M.; Ahearn, T.U.; Cao, X.; Feng, F.Y.; Loda, M.; Petimar, J.S.; Kantoff, P.; Mucci, L.A.; Chinnaiyan, A.M. Overexpression of the Long Non-coding RNA SChLAP1 Independently Predicts Lethal Prostate Cancer. Eur. Urol. 2016, 70, 549–552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, F.; Ren, S.; Chen, R.; Lu, J.; Shi, X.; Zhu, Y.; Zhang, W.; Jing, T.; Zhang, C.; Shen, J.; et al. Development and prospective multicenter evaluation of the long noncoding RNA MALAT-1 as a diagnostic urinary biomarker for prostate cancer. Oncotarget 2014, 5, 11091–11102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pan, J.; Ding, M.; Xu, K.; Yang, C.; Mao, L.J. Exosomes in diagnosis and therapy of prostate cancer. Oncotarget 2017, 8, 97693–97700. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Yuan, T.; Liang, M.; Du, M.; Xia, S.; Dittmar, R.; Wang, D.; See, W.; Costello, B.A.; Quevedo, F.; et al. Exosomal miR-1290 and miR-375 as prognostic markers in castration-resistant prostate cancer. Eur. Urol. 2015, 67, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Wang, J.; Wang, Y.; Zhu, P.; Liu, X.; Li, N.; Liu, J.; Yu, L.; Wang, W. GRP78 Participates in PCA3-regulated Prostate Cancer Progression. Anticancer Res. 2017, 37, 4303–4310. [Google Scholar] [CrossRef] [PubMed]
- de Kok, J.B.; Verhaegh, G.W.; Roelofs, R.W.; Hessels, D.; Kiemeney, L.A.; Aalders, T.W.; Swinkels, D.W.; Schalken, J.A. DD3(PCA3), a very sensitive and specific marker to detect prostate tumors. Cancer Res. 2002, 62, 2695–2698. [Google Scholar] [PubMed]
- Li, Y.; Luo, H.; Xiao, N.; Duan, J.; Wang, Z.; Wang, S. Long Noncoding RNA SChLAP1 Accelerates the Proliferation and Metastasis of Prostate Cancer via Targeting miR-198 and Promoting the MAPK1 Pathway. Oncol. Res. 2018, 26, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Ding, L.; Wang, L.; Zhao, Y.; Sun, Z.; Karnes, R.J.; Zhang, J.; Huang, H. LncRNA MALAT1 enhances oncogenic activities of EZH2 in castration-resistant prostate cancer. Oncotarget 2015, 6, 41045–41055. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gorin, M.A.; Verdone, J.E.; van der Toom, E.; Bivalacqua, T.J.; Allaf, M.E.; Pienta, K.J. Circulating tumour cells as biomarkers of prostate, bladder, and kidney cancer. Nat. Rev. Urol. 2016, 14, 90. [Google Scholar] [CrossRef] [PubMed]
- Scher, H.I.; Lu, D.; Schreiber, N.A.; Louw, J.; Graf, R.P.; Vargas, H.A.; Johnson, A.; Jendrisak, A.; Bambury, R.; Danila, D.; et al. Association of AR-V7 on Circulating Tumor Cells as a Treatment-Specific Biomarker With Outcomes and Survival in Castration-Resistant Prostate Cancer. JAMA Oncol. 2016, 2, 1441–1449. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Gregory, S.G.; Garcia-Blanco, M.A.; Armstrong, A.J. Using circulating tumor cells to inform on prostate cancer biology and clinical utility. Crit. Rev. Clin. Lab. Sci. 2015, 52, 191–210. [Google Scholar] [CrossRef] [PubMed]
- Khurana, K.K.; Grane, R.; Borden, E.C.; Klein, E.A. Prevalence of circulating tumor cells in localized prostate cancer. Curr. Urol. 2013, 7, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Tommasi, S.; Pilato, B.; Carella, C.; Lasorella, A.; Danza, K.; Vallini, I.; De Summa, S.; Naglieri, E. Standardization of CTC AR-V7 PCR assay and evaluation of its role in castration resistant prostate cancer progression. Prostate 2018. [Google Scholar] [CrossRef] [PubMed]
- Wilbaux, M.; Tod, M.; De Bono, J.; Lorente, D.; Mateo, J.; Freyer, G.; You, B.; Hénin, E. A Joint Model for the Kinetics of CTC Count and PSA Concentration during Treatment in Metastatic Castration-Resistant Prostate Cancer. CPT Pharmacomet. Syst. Pharmacol. 2015, 4, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, D.T.; Sequist, L.V.; Lee, R.J. Circulating tumour cells-monitoring treatment response in prostate cancer. Nat. Rev. Clin. Oncol. 2014, 11, 401–412. [Google Scholar] [CrossRef] [PubMed]
- Albino, G.; Vendittelli, F.; Paolillo, C.; Zuppi, C.; Capoluongo, E. Potential usefulness of CTC detection in follow up of prostate cancer patients. A preliminary report obtained by using Adnagene platform. Arch. Ital. Urol. Androl. 2013, 85, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.P.; Pantel, K.; Tennstedt, P.; Stroelin, P.; Schlomm, T.; Heinzer, H.; Riethdorf, S.; Steuber, T. Limited prognostic value of preoperative circulating tumor cells for early biochemical recurrence in patients with localized prostate cancer. Urol. Oncol. 2016, 34, 235.e11–235.e16. [Google Scholar] [CrossRef] [PubMed]
- Murray, N.P.; Aedo, S.; Fuentealba, C.; Reyes, E. 10 Year Biochemical Failure Free Survival of Men with CD82 Positive Primary Circulating Prostate Cells Treated by Radical Prostatectomy. Asian Pac. J. Cancer Prev. 2018, 19, 1577–1583. [Google Scholar] [CrossRef] [PubMed]
- Strobl, A.N.; Vickers, A.J.; Van Calster, B.; Steyerberg, E.; Leach, R.J.; Thompson, I.M.; Ankerst, D.P. Improving patient prostate cancer risk assessment: Moving from static, globally-applied to dynamic, practice-specific risk calculators. J. Biomed. Inform. 2015, 56, 87–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ankerst, D.P.; Hoefler, J.; Bock, S.; Goodman, P.J.; Vickers, A.; Hernandez, J.; Sokoll, L.J.; Sanda, M.G.; Wei, J.T.; Leach, R.J.; et al. Prostate Cancer Prevention Trial risk calculator 2.0 for the prediction of low- vs. high-grade prostate cancer. Urology 2014, 83, 1362–1367. [Google Scholar] [CrossRef] [PubMed]
- Thompson, I.M.; Ankerst, D.P.; Chi, C.; Goodman, P.J.; Tangen, C.M.; Lucia, M.S.; Feng, Z.; Parnes, H.L.; Coltman, C.A. Assessing prostate cancer risk: Results from the Prostate Cancer Prevention Trial. J. Natl. Cancer Inst. 2006, 98, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Roobol, M.J.; Verbeek, J.F.M.; van der Kwast, T.; Kümmerlin, I.P.; Kweldam, C.F.; van Leenders, G.J.L.H. Improving the Rotterdam European Randomized Study of Screening for Prostate Cancer Risk Calculator for Initial Prostate Biopsy by Incorporating the 2014 International Society of Urological Pathology Gleason Grading and Cribriform growth. Eur. Urol. 2017, 72, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Yuri, P.; Wangge, G.; Abshari, F.; Satjakoesoemah, A.I.; Perdana, N.R.; Wijaya, C.D.; Tansol, C.; Tigor, A.; Safriadi, F.; Kadar, D.D.; et al. Indonesian prostate cancer risk calculator (IPCRC): An application for predicting prostate cancer risk (a multicenter study). Acta Med. Indones. 2015, 47, 95–103. [Google Scholar] [PubMed]
- Chiu, P.K.; Roobol, M.J.; Nieboer, D.; Teoh, J.Y.; Yuen, S.K.; Hou, S.M.; Yiu, M.K.; Ng, C.F. Adaptation and external validation of the European randomised study of screening for prostate cancer risk calculator for the Chinese population. Prostate Cancer Prostatic Dis. 2017, 20, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.S.; Zhang, N.; Liu, S.H.; Xu, J.F.; Tong, S.J.; Cai, Y.H.; Zhang, L.M.; Bai, P.D.; Hu, M.B.; Jiang, H.W.; et al. The Huashan risk calculators performed better in prediction of prostate cancer in Chinese population: A training study followed by a validation study. Asian J. Androl. 2016, 18, 925–929. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Xie, L.; Xue, W.; Ye, Z.; Ma, L.; Gao, X.; Ren, S.; Wang, F.; Zhao, L.; Xu, C.; et al. Development and external multicenter validation of Chinese Prostate Cancer Consortium prostate cancer risk calculator for initial prostate biopsy. Urol. Oncol. 2016, 34, 416.e1–416.e7. [Google Scholar] [CrossRef] [PubMed]
- Roehl, K.A.; Antenor, J.A.; Catalona, W.J. Serial biopsy results in prostate cancer screening study. J. Urol. 2002, 167, 2435–2439. [Google Scholar] [CrossRef]
- Seisen, T.; Roudot-Thoraval, F.; Bosset, P.O.; Beaugerie, A.; Allory, Y.; Vordos, D.; Abbou, C.C.; De La Taille, A.; Salomon, L. Predicting the risk of harboring high-grade disease for patients diagnosed with prostate cancer scored as Gleason </= 6 on biopsy cores. World J. Urol. 2015, 33, 787–792. [Google Scholar] [CrossRef] [PubMed]
- Fu, Q.; Moul, J.W.; Banez, L.L.; Sun, L.; Mouraviev, V.; Xie, D.; Polascik, T.J. Association between percentage of tumor involvement and Gleason score upgrading in low-risk prostate cancer. Med. Oncol. 2012, 29, 3339–3344. [Google Scholar] [CrossRef] [PubMed]
- Emwas, A.-H.M.; Salek, R.M.; Griffin, J.L.; Merzaban, J. NMR-based metabolomics in human disease diagnosis: Applications, limitations, and recommendations. Metabolomics 2013, 9, 1048–1072. [Google Scholar] [CrossRef]
- Kimura, T. East meets west: Ethnic differences in prostate cancer epidemiology between East Asians and Caucasians. Chin. J. Cancer 2012, 31, 421. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Wang, H.K.; Qu, Y.Y.; Ye, D.W. Prostate cancer in East Asia: Evolving trend over the last decade. Asian J. Androl. 2015, 17, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Sterling, W.A.; Weiner, J.; Schreiber, D.; Mehta, K.; Weiss, J.P. The impact of African American race on prostate cancer detection on repeat prostate biopsy in a veteran population. Int. Urol. Nephrol. 2016, 48, 2015–2021. [Google Scholar] [CrossRef] [PubMed]
- Kallingal, G.J.; Walker, M.R.; Musser, J.E.; Ward, D.E.; McMann, L.P. Impact of race in using PSA velocity to predict for prostate cancer. Mil. Med. 2014, 179, 329–332. [Google Scholar] [CrossRef] [PubMed]
- Su, L.J.; Arab, L.; Steck, S.E.; Fontham, E.T.; Schroeder, J.C.; Bensen, J.T.; Mohler, J.L. Obesity and prostate cancer aggressiveness among African and Caucasian Americans in a population-based study. Cancer Epidemiol. Biomark. Prev. 2011, 20, 844–853. [Google Scholar] [CrossRef] [PubMed]
- Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, D.K., AWMF). Interdisziplinäre Leitlinie der Qualität S3 zur Früherkennung, Diagnose und Therapie der verschiedenen Stadien des Prostatakarzinoms, Langversion 5.0, 2018, AWMF Registernummer: 043/022OL. 2018. Available online: http://www.leitlinienprogramm-onkolo-gie.de/leitlinien/prostatakarzinom/ (accessed on 15 May 2018).

| Biomarker(s) | Source | Commercial Product | Predict | Avoid Biopsies | Sens. | Spec. | AUC | PPV | NPV | Targeted Patients | Ref. |
|---|---|---|---|---|---|---|---|---|---|---|---|
| PSA | blood (serum) | Tandem-R® monoclonal immunoradiometric assay (Hybritech Inc., San Diego, CA, USA) | PCa on first biopsy | n.a. | 79% at PSA ≥ 4 ng/mL | 59% at PSA ≥ 4 ng/mL | 0.64 | 40% | 89% | age > 50 years PSA ≥ 4 ng/mL | [33] |
| PSA | blood (serum) | Tandem-R® (Hybritech) | PCa (vs. BPH/Controls) | n.a. | 78% at PSA ≥ 4 ng/mL | 60% (PCa vs. BPH); 94% (PCa vs. Control at PSA ≥ 4 ng/mL | n.r. | n.r. | n.r. | age > 60 years | [32] |
| PSA velocity (0.75 ng/mL/year) | blood (serum) | Tandem-R® (Hybritech) | PCa (vs. BPH/Controls) | n.a. | 72% at PSA ≥ 4 ng/mL | 90% (PCa vs. BPH); 100% PCa vs. Control: at PSA ≥ 4 ng/mL | n.r. | n.r. | n.r. | age >60 years | [32] |
| PSA | blood (serum) | Access Hybritech® | Risk of GS ≥ 7 | n.a. | 90% at PSA ≥4.3 ng/mL | 9% at PSA ≥ 4.4 ng/mL | 0.55 | n.r. | n.r. | age ≥ 50 years PSA 4–10 ng/mL, neg. DRE | [34] |
| fPSA/tPSA | blood (serum) | n.r. | PCa (vs. BPH) | n.a. | 70% (pooled data) | 58% (pooled data) | 0.76 (pooled data) | 41% | 86% (1) | PSA 4.0–10.0 ng/mL | meta-analysis [31] |
| PHI (p2PSA/fPSA × √tPSA) | blood (post-DRE serum) | PHI, prostate health index Beckman Coulter, Atlanta, GA, USA) | Risk of GS ≥ 7 | n.r. | 90% (pooled data) | 17% (pooled data) | 0.67 (pooled data) | n.r. | n.r. | age ≥ 50 years PSA 4–10 ng/mL, neg. DRE | meta-analysis [35] |
| p2PSA/fPSA (%p2PSA) | PHI, prostate health index Beckman Coulter, Atlanta, GA, USA) | Risk of GS ≥ 7 | n.r. | 96% (pooled data) | 9% (pooled data) | 0.54 (pooled data) | n.r. | n.r. | age ≥ 50 years PSA 4–10 ng/mL, neg. DRE | meta-analysis [35] | |
| PHI (p2PSA/ fPSA × √tPSA) | blood (post-DRE serum) | PHI, prostate health index Beckman Coulter, Atlanta, GA, USA) | Risk of GS ≥ 7 | 30.1% | 90% (cutoff 29.8) | 30% (cutoff 29.8) | 0.71 | n.r. | n.r. | age ≥ 50 years PSA 4–10 ng/mL, neg. DRE | [34] |
| intact PSA, free PSA, total PSA, kallikrein-related peptidase 2 (hK2) | blood (post-DRE serum) | 4KScore® Test (OPKO Lab, Nashville, TN, USA) | Risk of GS ≥ 7 | 43% | n.r. | n.r. | 0.82 | n.r. | n.r. | PSA ≥ 3 ng/mL; | [36] |
| expression of 8 auto-antibodies against: CSNK2A2, cestrosomal protein 164 kDa, NK3 homeobox 1, aurora kinase interacting protein 1,5′-UTR BMI1, ARF6, chromosome 3′-UTR region Ropporin/RhoEGF, desmocollin 3 | blood (serum) | Apifiny® (Armune Bioscience, Kalamazoo, MI, USA) | Risk of GS ≥ 7 | n.r. | 60% at PSA > 4 ng/mL [37] | 69% at PSA > 4 ng/mL [37] | 0.69 at PSA > 4 ng/mL [37] | 30% [37] | 89% [37] | PSA ≥ 2.5 ng/mL, initial biopsy | [37,38] |
| prostate cancer gene 3 (PCA3) + PSA mRNA ratio | post-DRE urine | Progensa™ (Gen-Probe Inc., San Diego, CA, USA) | PCa | n.r. | 58% [39] 78% [40] 76% [41] | 72% [39] 57% [40] 52% [41] | 0.68 [39] n.r. [40] 0.80 [41] | n.r. [39] 34% [40] n.r. [41] | n.r. [39] 90% [40] 88% [41] | age ≥ 50 years neg. prior biopsy, repeat biopsy | [39,40,41] |
| exosomes (EV) + (SOC: prostate-specific antigen level, age, race, family history); gene expression (targets revealed): SPDEF, ERG and PCA3 | urine | ExoDx® Prostate IntelliScore urine exosome assay (Exosome Diagnostics, Inc., Waltham, MA, USA) | Risk of GS ≥ 7 | n.r. | 92% | 34% | 0.73 | 36% | 91% | PSA 2–20 ng/mL, initial biopsy | [42] |
| serum PSA + urine PCA3 mRNA + urine TMPRSS2:ERG mRNA | blood (serum); post-DRE urine | Progensa™ (Hologic, Bedford, MA, USA); MiPS test; University of Michigan (MLabs) | Risk of GS ≥ 7 | 35–47% | n.r. | n.r. | 0.77 (PSA + T2:ERG + PCA3 | n.r. | n.r. | elevated PSA (initial biopsy), prior negative biopsy (repeat biopsy) | [43] |
| HOXC6 mRNA + DLX1 mRNA + serum PSA + PSA density + DRE status + age + family history | post-DRE urine | SelectMDx (MDx Health, Irvine, CA, USA) | Risk of GS ≥ 7 | 42% of total; 53% of unne-cessary biopsies | 91% (HOXC6 + DLX1) | 36% (HOXC6 + DLX1) | 0.76 (HOXC6 + DLX1); 0.90 + clin. Para-meters | 28% | 98% | PSA > 4 ng/mL; negative index biopsy | [44] |
| STHLM3 risk-based model: PSA, fPSA, iPSA, hK2, β-microseminoprotein (MSMB), macrophage inhibitory cytokine 1 (MIC1), genetic polymorphisms [232 SNPs], age, family history, previous prostate biopsy, DRE, prostate volume | blood | various | Risk of GS ≥ 7 | 32% biopsies (GS ≥ 7); 44% benign biopsies | n.r. | n.r. | n.r. | n.r. | n.r. | PSA ≥ 3 ng/mL; age 50–69 years; highly selected patients; validation in standard populations needed | [45] |
| Reference | Song et al. 2018 [62] | Schaefer et al. 2010 [65] | Walter et al. 2013 [64] | |||
|---|---|---|---|---|---|---|
| Type | Meta-Analysis of 104 Studies | Original Article | Original Article | |||
| Samples | Tissue, Blood, Urine | RPE Frozen Tissue (76 PCa, 79 PCa) | FFPE RPE Tissue (37 PCa) | |||
| Method(s) | Various | miRNA Microarray; 470 miRNAs | PCR Array Profiling | |||
| Measure | Expression in PCa | Expression in PCa | Expr. in GS ≥ 8 vs. GS 6 | |||
| miR-1 ↓ | a | miR-16 ↓ | miR-9 ↑ | i | ||
| miR-18a ↑ | a | miR-31 ↓ | j | miR-27 ↓ | i | |
| miR-21 ↑ | c,l | miR-96 ↑ | e,g,j | miR-30c ↑ | h,l | |
| miR-23b ↓ | a | miR-125b ↓ | k | miR-34 ↑ | i | |
| miR-27b ↓ | a | miR-145 ↓ | miR-92 ↓ | i | ||
| miR-30c ↓ | a,c | miR-149 ↓ | e | miR-96 ↓ | i | |
| miR-31 ↑ | b | miR-181b ↓ | miR-122 ↑ | h,i | ||
| miR-34a ↑ | a | miR-182 ↑ | e | miR-125a ↑ | h | |
| miR-99b ↓ | a | miR-182 * ↑ | miR-125 ↓ | i | ||
| miR-106b ↑ | a | miR-183 ↑ | f | miR-126 ↓ | i | |
| miR-129 ↓ | c | miR-184 ↓ | miR-138 ↑ | i | ||
| miR-139-5p ↓ | a | miR-205 ↓ | e,f,j,k | miR-144 ↑ | i | |
| miR-141 ↑ | a,l | miR-221 ↓ | miR-146b-5p ↑ | h | ||
| miR-145 ↓ | c | miR-222 ↓ | k | miR-148 ↓ | i,m | |
| miR-152 ↓ | a | miR-375 ↑ | e,l,m | miR-181a ↑ | h | |
| miR-182 ↑ | a | miR-181c ↑ | h | |||
| miR-183 ↑ | a | miR-184 ↑ | h,i | |||
| miR-187 ↓ | a | miR-193 ↑ | i | |||
| miR-200a ↑ | a | miR-193b ↑ | h | |||
| miR-200b ↑ | a | miR-198 ↑ | i | |||
| miR-204 ↓ | a | miR-214 ↑ | h | |||
| miR-205 ↓ | a | miR-215 ↑ | i | |||
| miR-224 ↓ | a | miR-222 ↓ | i | |||
| miR-301a ↑ | a | miR-335 ↑ | h,i | |||
| miR-375 ↑ | a,d,l,m | miR-373 ↑ | i | |||
| miR-452 ↓ | a | |||||
| miR-505 ↓ | a | |||||
| let-7c ↓ | a,b,c | |||||
| Name | Function | Diagnostic Value | Reference |
|---|---|---|---|
| PCA3 ↑ (prostate cancer associated 3) | increase of cell proliferation, migration and invasion; inhibition of apoptosis; [85] | predict risk of GS > 7 | [86] |
| TINCR ↓ (Terminal differentiation induced non-coding RNA) | growth inhibition via TRIP13 suppression [79] | not determined | [79] |
| FR0348383 ↑ | unknown | predict PCa-positive biopsy; avoid 52% unnecessary biopsies without missing high-grade PCa | [80] |
| SChLAP1 ↑ (SWI/SNF complex antagonist associated with prostate cancer 1) | increase of cell proliferation, metastasis via downregulation of miRNA-198 and activation of MAPK1 pathway [87] | predict high-risk, lethal PCa; biochemical recurrence after RPE | [81] |
| MALAT1 ↑ (metastasis-associated lung adenocarcinoma transcript 1) | interacts with EZH2, promoting proliferation and invasion [88] | predict PCa-positive biopsy; discriminate between PCa and BPH, PCa and HC | [82] |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neuhaus, J.; Yang, B. Liquid Biopsy Potential Biomarkers in Prostate Cancer. Diagnostics 2018, 8, 68. https://doi.org/10.3390/diagnostics8040068
Neuhaus J, Yang B. Liquid Biopsy Potential Biomarkers in Prostate Cancer. Diagnostics. 2018; 8(4):68. https://doi.org/10.3390/diagnostics8040068
Chicago/Turabian StyleNeuhaus, Jochen, and Bo Yang. 2018. "Liquid Biopsy Potential Biomarkers in Prostate Cancer" Diagnostics 8, no. 4: 68. https://doi.org/10.3390/diagnostics8040068
APA StyleNeuhaus, J., & Yang, B. (2018). Liquid Biopsy Potential Biomarkers in Prostate Cancer. Diagnostics, 8(4), 68. https://doi.org/10.3390/diagnostics8040068