HPMA Copolymer-Based Nanomedicines in Controlled Drug Delivery
Abstract
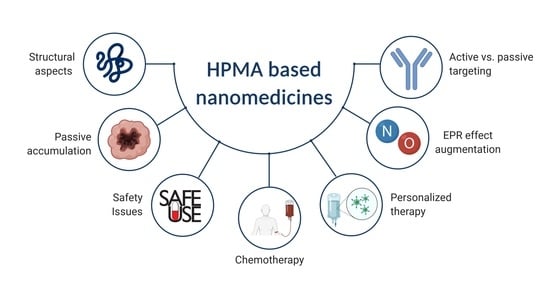
:1. Introduction
2. Safety Features of HPMA Polymers Per Se
3. Structural Aspects
3.1. Linear Polymer Carriers
3.2. Biodegradable HMW Polymer Carriers
3.3. Self-Assembled HMW Polymer Carriers
4. Augmentation of the Passive Accumulation in Solid Tumors
5. Active Targeting Versus Passive Accumulation of pHPMA Nanomedicines
6. Future Prospects
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Farokhzad, O.C.; Langer, R. Impact of nanotechnology on drug delivery. ACS Nano 2009, 3, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Ulbrich, K.; Šubr, V. Structural and chemical aspects of HPMA copolymers as drug carriers. Adv. Drug Deliv. Rev. 2010, 62, 150–166. [Google Scholar] [CrossRef] [PubMed]
- Chytil, P.; Koziolová, E.; Etrych, T.; Ulbrich, K. HPMA Copolymer-Drug Conjugates with Controlled Tumor-Specific Drug Release. Macromol. Biosci. 2018, 18. [Google Scholar] [CrossRef] [PubMed]
- Venditto, V.J.; Szoka, F.C. Cancer nanomedicines: So many papers and so few drugs! Adv. Drug Deliv. Rev. 2013, 65, 80–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chytil, P.; Kostka, L.; Etrych, T. Structural design and synthesis of polymer prodrugs. In Polymers for Biomedicine: Synthesis, Characterization, and Applications; Scholz, C., Ed.; John Wiley and Sons: Hoboken, NJ, USA, 2017; p. 624. [Google Scholar]
- Ulbrich, K.; Holá, K.; Šubr, V.; Bakandritsos, A.; Tuček, J.; Zbořil, R. Targeted Drug Delivery with Polymers and Magnetic Nanoparticles: Covalent and Noncovalent Approaches, Release Control, and Clinical Studies. Chem. Rev. 2016, 116, 5338–5431. [Google Scholar] [CrossRef] [PubMed]
- Bag, M.A.; Valenzuela, L.M. Impact of the Hydration States of Polymers on Their Hemocompatibility for Medical Applications: A Review. Int. J. Mol. Sci. 2017, 18, 1422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, W.; Klein, J. Control of surface forces through hydrated boundary layers. Curr. Opin. Colloid Interface Sci. 2019, 44, 94–106. [Google Scholar] [CrossRef]
- Maeda, H.; Nakamura, H.; Fang, J. The EPR effect for macromolecular drug delivery to solid tumors: Improvement of tumor uptake, lowering of systemic toxicity, and distinct tumor imaging in vivo. Adv. Drug Deliv. Rev. 2013, 65, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Šírová, M.; Mrkvan, T.; Etrych, T.; Chytil, P.; Rossmann, P.; Ibrahimová, M.; Kovář, L.; Ulbrich, K.; Říhová, B. Preclinical Evaluation of Linear HPMA-Doxorubicin Conjugates with pH-Sensitive Drug Release: Efficacy, Safety, and Immunomodulating Activity in Murine Model. Pharm. Res. 2010, 27, 200–208. [Google Scholar] [CrossRef]
- Etrych, T.; Šírová, M.; Starovoytova, L.; Říhová, B.; Ulbrich, K. HPMA Copolymer Conjugates of Paclitaxel and Docetaxel with pH-Controlled Drug Release. Mol. Pharm. 2010, 7, 1015–1026. [Google Scholar] [CrossRef]
- Nakamura, H.; Etrych, T.; Chytil, P.; Ohkubo, M.; Fang, J.; Ulbrich, K.; Maeda, H. Two step mechanisms of tumor selective delivery of N-(2-hydroxypropyl)methacrylamide copolymer conjugated with pirarubicin via an acid-cleavable linkage. J. Control. Release 2014, 174, 81–87. [Google Scholar] [CrossRef]
- Noguchi, Y.; Wu, J.; Duncan, R.; Strohalm, J.; Ulbrich, K.; Akaike, T.; Maeda, H. Early Phase Tumor Accumulation of Macromolecules: A Great Difference in Clearance Rate between Tumor and Normal Tissues. Jpn. J. Cancer Res. 1998, 89, 307–314. [Google Scholar] [CrossRef]
- Etrych, T.; Kovář, L.; Strohalm, J.; Chytil, P.; Říhová, B.; Ulbrich, K. Biodegradable star HPMA polymer-drug conjugates: Biodegradability, distribution and anti-tumor efficacy. J. Control. Release 2011, 154, 241–248. [Google Scholar] [CrossRef]
- Duncan, R.; Vicent, M.J. Polymer therapeutics-prospects for 21st century: The end of the beginning. Adv. Drug Deliv. Rev. 2013, 65, 60–70. [Google Scholar] [CrossRef]
- Seymour, L.W.; Duncan, R.; Strohalm, J.; Kopeček, J. Effect of Molecular-Weight (Mw) of N-(2-Hydroxypropyl)Methacrylamide Copolymers on Body Distribution and Rate of Excretion after Subcutaneous, Intraperitoneal, and Intravenous Administration to Rats. J. Biomed. Mater. Res. 1987, 21, 1341–1358. [Google Scholar] [CrossRef]
- Etrych, T.; Šubr, V.; Strohalm, J.; Šírová, M.; Říhová, B.; Ulbrich, K. HPMA copolymer-doxorubicin conjugates: The effects of molecular weight and architecture on biodistribution and in vivo activity. J. Control. Release 2012, 164, 346–354. [Google Scholar] [CrossRef]
- Drobník, J.; Kopecek , J.; Labský, J.; Rejmanová, P.; Exner, J.; Kálal, J. Preparation of Biologically Active Substances Bearing NH2 Groups in a Form Releasable by Enzymatic Cleavage. U.S. Patent 4 097,470, 27 June 1978. [Google Scholar]
- Kopeček, J.; Ulbrich, K.; Vacík, J.; Strohalm, J.; Chytrý, V.; Drobník, J.; Kálal, J. Copolymers Based on N-Substituted Acrylamides, N-Substituted Methacrylamides and N,N-Disubstituted Acrylamides and the Method of Their Manufacturing. U.S. Patent 4,062,831, 13 December 1977. [Google Scholar]
- Štěrba, O.; Uhlířová, Z.; Petz, R. Duxon—A new Czechoslovak-made infusion solution—An experimental contribution to biological evaluation. Cas. Lek. Cesk. 1980, 119, 994–997. [Google Scholar]
- Šprincl, L.; Exner, J.; Štěrba, O.; Kopeček, J. New types of synthetic infusion solutions. III. Elimination and retention of poly-[N-(2-hydroxypropyl)methacrylamide] in a test organism. J. Biomed. Mater. Res. 1976, 10, 953–963. [Google Scholar] [CrossRef]
- Uhlířová, Z.; Jirásek, A.; Štěrba, O. Newly developed Czechoslovak colloid infusion solution Duxon. Preclinical trial. Cas. Lek. Cesk. 1981, 120, 1553–1556. [Google Scholar]
- Cinátl, J.; Štěrba, O.; Paluska, E. New types of synthetic infusion solutions. The effect of Duxon on the proliferation of cells in vitro. Cesko-Slov. Farm. 1980, 29, 134–138. [Google Scholar]
- Korcáková, L.; Paluska, E.; Hašková, V.; Kopeček, J. A simple test for immunogenicity of colloidal infusion solutions; the draining lymph node activation. Z. Immun. 1976, 151, 219–223. [Google Scholar] [CrossRef]
- Paluska, E.; Cinátl, J.; Korcáková, L.; Štěrba, O.; Kopeček, J.; Hrubá, A.; Nezvalová, J.; Staněk, R. Immunosuppressive Effects of a Synthetic-Polymer Poly N-(2-Hydroxypropyl)Methacrylamide (Duxon). Folia Biol-Prague 1980, 26, 304–311. [Google Scholar]
- Petz, R.; Štěrba, O.; Jirásek, A.; Foltinská, Z.; Kostírová, D.; Kopeček, J. Pharmacological evaluation of the toxicity after repeated administration of synthetic colloid solution of Duxon. Cas. Lek. Cesk. 1988, 127, 553–555. [Google Scholar] [PubMed]
- Štěrba, O.; Paluska, E.; Jozová, O. New types of synthetic infusion solutions. Basic biological properties of poly(N-(2 hydroxypropyl) methacrylamide) (Czech). Cas. Lek. Cesk. 1975, 114, 1268–1270. [Google Scholar] [PubMed]
- Uhlířová, Z.; Štěrba, O.; Petz, R.; Viktora, L. Czechoslovak infusion solution Duxon—Preclinical tests. Effect on the haemogram of some laboratory animals (author‘s transl). Cas. Lek. Cesk. 1980, 119, 1091–1094. [Google Scholar]
- Štěrba, O.; Paluska, E.; Jozová, O.; Spunda, J.; Nezvalová, J.; Šprincl, L.; Kopeček, J.; Cinátl, J. New types of synthetic infusion solutions. Basic biological properties of poly N (2 hydroxypropyl) methacrylamide. Rev. Czech. Med. 1976, 22, 152–156. [Google Scholar]
- Paluska, E.; Hrubá, A.; Štěrba, O.; Kopeček, J. Effect of a synthetic poly N-(2-hydroxypropyl)methacrylamide (Duxon) on haemopoiesis and graft-versus-host reaction. Folia Biol-Prague 1986, 32, 91–102. [Google Scholar]
- Řihová, B.; Kopeček, J.; Ulbrich, K.; Pospíšil, M.; Mančal, P. Effect of the chemical structure of N-(2-hydroxypropyl) methacrylajnide copolymers on their ability to induce antibody formation in inbred strains of mice. Biomaterials 1984, 5, 143–148. [Google Scholar] [CrossRef]
- Hoffmann, S.; Vystrčilová, L.; Ulbrich, K.; Etrych, T.; Caysa, H.; Mueller, T.; Mäder, K. Dual Fluorescent HPMA Copolymers for Passive Tumor Targeting with pH-Sensitive Drug Release: Synthesis and Characterization of Distribution and Tumor Accumulation in Mice by Noninvasive Multispectral Optical Imaging. Biomacromolecules 2012, 13, 652–663. [Google Scholar] [CrossRef]
- Chytil, P.; Hoffmann, S.; Schindler, L.; Kostka, L.; Ulbrich, K.; Caysa, H.; Mueller, T.; Mader, K.; Etrych, T. Dual fluorescent HPMA copolymers for passive tumor targeting with pH- sensitive drug release II: Impact of release rate on biodistribution. J. Control. Release 2013, 172, 504–512. [Google Scholar] [CrossRef]
- Liu, X.-M.; Quan, L.-D.; Tian, J.; Alnouti, Y.; Fu, K.; Thiele, G.; Wang, D. Synthesis and Evaluation of a Well-defined HPMA Copolymer–Dexamethasone Conjugate for Effective Treatment of Rheumatoid Arthritis. Pharm. Res. 2008, 25, 2910–2919. [Google Scholar] [CrossRef] [Green Version]
- Pan, H.; Sima, M.; Kopečková, P.; Wu, K.; Gao, S.; Liu, J.; Wang, D.; Miller, S.C.; Kopeček, J. Biodistribution and Pharmacokinetic Studies of Bone-Targeting N-(2-Hydroxypropyl)methacrylamide Copolymer—Alendronate Conjugates. Mol. Pharm. 2008, 5, 548–558. [Google Scholar] [CrossRef] [Green Version]
- Chytil, P.; Etrych, T.; Kříž, J.; Šubr, V.; Ulbrich, K. N-(2-Hydroxypropyl)methacrylamide-based polymer conjugates with pH-controlled activation of doxorubicin for cell-specific or passive tumour targeting. Synthesis by RAFT polymerisation and physicochemical characterisation. Eur. J. Pharm. Sci. 2010, 41, 473–482. [Google Scholar] [CrossRef] [PubMed]
- Raus, V.; Kostka, L. Optimizing the Cu-RDRP of N-(2-hydroxypropyl) methacrylamide toward biomedical applications. Polym. Chem. 2019, 10, 564–568. [Google Scholar] [CrossRef]
- Chytil, P.; Šírová, M.; Koziolová, E.; Ulbrich, K.; Říhová, B.; Etrych, T. The Comparison of In Vivo Properties of Water-Soluble HPMA-Based Polymer Conjugates with Doxorubicin Prepared by Controlled RAFT or Free Radical Polymerization. Physiol. Res. 2015, 64, S41–S49. [Google Scholar] [CrossRef]
- Koziolová, E.; Goel, S.; Chytil, P.; Janoušková, O.; Barnhart, T.E.; Cai, W.B.; Etrych, T. A tumor-targeted polymer theranostics platform for positron emission tomography and fluorescence imaging. Nanoscale 2017, 9, 10906–10918. [Google Scholar] [CrossRef]
- Randárová, E.; Nakamura, H.; Islam, R.; Studenovský, M.; Mamoru, H.; Fang, J.; Chytil, P.; Etrych, T. Highly effective anti-tumor nanomedicines based on HPMA copolymer conjugates with pirarubicin prepared by controlled RAFT polymerization. Acta Biomater. 2020, 106, 256–266. [Google Scholar] [CrossRef]
- Quan, L.D.; Zhang, Y.J.; Crielaard, B.J.; Dusad, A.; Lele, S.M.; Rijcken, C.J.F.; Metselaar, J.M.; Kostková, H.; Etrych, T.; Ulbrich, K.; et al. Nanomedicines for Inflammatory Arthritis: Head-to-Head Comparison of Glucocorticoid-Containing Polymers, Micelles, and Liposomes. ACS Nano 2014, 8, 458–466. [Google Scholar] [CrossRef] [Green Version]
- Libánská, A.; Randárová, E.; Lager, F.; Renault, G.; Scherman, D.; Etrych, T. Polymer Nanomedicines with pH-Sensitive Release of Dexamethasone for the Localized Treatment of Inflammation. Pharmaceutics 2020, 12, 700. [Google Scholar] [CrossRef]
- Etrych, T.; Šubr, V.; Laga, R.; Říhová, B.; Ulbrich, K. Polymer conjugates of doxorubicin bound through an amide and hydrazone bond: Impact of the carrier structure onto synergistic action in the treatment of solid tumours. Eur. J. Pharm. Sci. 2014, 58, 1–12. [Google Scholar] [CrossRef]
- Zhang, R.; Luo, K.; Yang, J.; Sima, M.; Sun, Y.; Janát-Amsbury, M.M.; Kopeček, J. Synthesis and evaluation of a backbone biodegradable multiblock HPMA copolymer nanocarrier for the systemic delivery of paclitaxel. J. Control. Release 2013, 166, 66–74. [Google Scholar] [CrossRef] [Green Version]
- Luo, K.; Yang, J.; Kopečková, P.; Kopeček, J. Biodegradable Multiblock Poly[N-(2-hydroxypropyl)methacrylamide] via Reversible Addition−Fragmentation Chain Transfer Polymerization and Click Chemistry. Macromolecules 2011, 44, 2481–2488. [Google Scholar] [CrossRef] [Green Version]
- Larson, N.; Yang, J.Y.; Ray, A.; Cheney, D.L.; Ghandehari, H.; Kopeček, J. Biodegradable multiblock poly(N-2-hydroxypropyl)methacrylamide gemcitabine and paclitaxel conjugates for ovarian cancer cell combination treatment. Int. J. Pharm. 2013, 454, 435–443. [Google Scholar] [CrossRef] [Green Version]
- Pan, H.Z.; Yang, J.Y.; Kopečková, P.; Kopeček, J. Backbone Degradable Multiblock N-(2-Hydroxypropyl)methacrylamide Copolymer Conjugates via Reversible Addition-Fragmentation Chain Transfer Polymerization and Thiol-ene Coupling Reaction. Biomacromolecules 2011, 12, 247–252. [Google Scholar] [CrossRef] [Green Version]
- Etrych, T.; Chytil, P.; Mrkvan, T.; Šírová, M.; Říhová, B.; Ulbrich, K. Conjugates of doxorubicin with graft HPMA copolymers for passive tumor targeting. J. Control. Release 2008, 132, 184–192. [Google Scholar] [CrossRef]
- Etrych, T.; Strohalm, J.; Chytil, P.; Černoch, P.; Starovoytova, L.; Pechar, M.; Ulbrich, K. Biodegradable star HPMA polymer conjugates of doxorubicin for passive tumor targeting. Eur. J. Pharm. Sci. 2011, 42, 527–539. [Google Scholar] [CrossRef]
- Wang, D.; Kopečková, P.; Minko, T.; Nanayakkara, V.; Kopeček, J. Synthesis of starlike N-(2-hydroxypropyl)methacrylamide copolymers: Potential drug carriers. Biomacromolecules 2000, 1, 313–319. [Google Scholar] [CrossRef]
- Chytil, P.; Koziolová, E.; Janoušková, O.; Kostka, L.; Ulbrich, K.; Etrych, T. Synthesis and Properties of Star HPMA Copolymer Nanocarriers Synthesised by RAFT Polymerisation Designed for Selective Anticancer Drug Delivery and Imaging. Macromol. Biosci. 2015, 15, 839–850. [Google Scholar] [CrossRef]
- Kostka, L.; Kotrchová, L.; Šubr, V.; Libánská, A.; Ferreira, C.A.; Malátová, I.; Lee, H.J.; Barnhart, T.E.; Engle, J.W.; Cai, W.B.; et al. HPMA-based star polymer biomaterials with tuneable structure and biodegradability tailored for advanced drug delivery to solid tumours. Biomaterials 2020, 235, 119728. [Google Scholar] [CrossRef]
- Pan, H.Z.; Sima, M.; Yang, J.Y.; Kopeček, J. Synthesis of Long-Circulating, Backbone Degradable HPMA CopolymerDoxorubicin Conjugates and Evaluation of Molecular-Weight-Dependent Antitumor Efficacy. Macromol. Biosci. 2013, 13, 155–160. [Google Scholar] [CrossRef] [Green Version]
- Etrych, T.; Tsukigawa, K.; Nakamura, H.; Chytil, P.; Fang, J.; Ulbrich, K.; Otagiri, M.; Maeda, H. Comparison of the pharmacological and biological properties of HPMA copolymer-pirarubicin conjugates: A single-chain copolymer conjugate and its biodegradable tandem-diblock copolymer conjugate. Eur. J. Pharm. Sci. 2017, 106, 10–19. [Google Scholar] [CrossRef]
- Duan, Z.; Zhang, Y.; Zhu, H.; Sun, L.; Cai, H.; Li, B.; Gong, Q.; Gu, Z.; Luo, K. Stimuli-Sensitive Biodegradable and Amphiphilic Block Copolymer-Gemcitabine Conjugates Self-Assemble into a Nanoscale Vehicle for Cancer Therapy. ACS Appl. Mater. Interfaces 2017, 9, 3474–3486. [Google Scholar] [CrossRef] [PubMed]
- Krakovičová, H.; Etrych, T.; Ulbrich, K. HPMA-based polymer conjugates with drug combination. Eur. J. Pharm. Sci. 2009, 37, 405–412. [Google Scholar] [CrossRef]
- Kostková, H.; Etrych, T.; Říhová, B.; Ulbrich, K. Synergistic effect of HPMA copolymer-bound doxorubicin and dexamethasone in vivo on mouse lymphomas. J. Bioact. Compat. Polym. 2011, 26, 270–286. [Google Scholar] [CrossRef]
- Říhová, B.; Etrych, T.; Šírová, M.; Kovář, L.; Hovorka, O.; Kovář, M.; Benda, A.; Ulbrich, K. Synergistic Action of Doxorubicin Bound to the Polymeric Carrier Based on N-(2-Hydroxypropyl)methacrylamide Copolymers through an Amide or Hydrazone Bond. Mol. Pharm. 2010, 7, 1027–1040. [Google Scholar] [CrossRef]
- Yang, J.; Kopeček, J. Macromolecular therapeutics. J. Control. Release 2014, 190, 288–303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, J.; Luo, K.; Pan, H.; Kopečková, P.; Kopeček, J. Synthesis of biodegradable multiblock copolymers by click coupling of RAFT-generated heterotelechelic polyHPMA conjugates. React. Funct. Polym. 2011, 71, 294–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kopeček, J.; Yang, J.Y. Polymer nanomedicines. Adv. Drug Deliv. Rev. 2020, 156, 40–64. [Google Scholar] [CrossRef]
- Yang, J.Y.; Zhang, R.; Pan, H.Z.; Li, Y.L.; Fang, Y.X.; Zhang, L.B.; Kopeček, J. Backbone Degradable N-(2-Hydroxypropyl)methacrylamide Copolymer Conjugates with Gemcitabine and Paclitaxel: Impact of Molecular Weight on Activity toward Human Ovarian Carcinoma Xenografts. Mol. Pharm. 2017, 14, 1384–1394. [Google Scholar] [CrossRef]
- Koziolová, E.; Kostka, L.; Kotrchová, L.; Šubr, V.; Konefal, R.; Nottelet, B.; Etrych, T. N-(2-Hydroxypropyl)methacrylamide-Based Linear, Diblock, and Starlike Polymer Drug Carriers: Advanced Process for Their Simple Production. Biomacromolecules 2018, 19, 4003–4013. [Google Scholar] [CrossRef]
- Kostka, L.; Etrych, T. High-Molecular-Weight HPMA-Based Polymer Drug Carriers for Delivery to Tumor. Physiol. Res. 2016, 65, S179–S190. [Google Scholar] [CrossRef]
- Pearce, A.K.; Anane-Adjei, A.B.; Cavanagh, R.J.; Monteiro, P.F.; Bennett, T.M.; Taresco, V.; Clarke, P.A.; Ritchie, A.A.; Alexander, M.R.; Grabowska, A.M.; et al. Effects of Polymer 3D Architecture, Size, and Chemistry on Biological Transport and Drug Delivery In Vitro and in Orthotopic Triple Negative Breast Cancer Models. Adv. Healthc. Mater. 2020, 9, 2000892. [Google Scholar] [CrossRef] [PubMed]
- Kotrchová, L.; Kostka, L.; Etrych, T. Drug carriers with star polymer structures. Physiol. Res. 2018, 67, S293–S303. [Google Scholar] [CrossRef]
- Kostková, H.; Schindler, L.; Kotrchová, L.; Kovář, M.; Šírová, M.; Kostka, L.; Etrych, T. Star Polymer-Drug Conjugates with pH-Controlled Drug Release and Carrier Degradation. J. Nanomater. 2017, 2017, 8675435. [Google Scholar] [CrossRef]
- Kudláčová, J.; Kotrchová, L.; Kostka, L.; Randárová, E.; Filipová, M.; Janoušková, O.; Fang, J.; Etrych, T. Structure-to-Efficacy Relationship of HPMA-Based Nanomedicines: The Tumor Spheroid Penetration Study. Pharmaceutics 2020, 12, 1242. [Google Scholar] [CrossRef]
- Kotrchová, L.; Etrych, T. Synthesis of Water-Soluble Star Polymers Based on Cyclodextrins. Physiol. Res. 2018, 67, S357–S365. [Google Scholar] [CrossRef]
- Talelli, M.; Rijcken, C.J.F.; van Nostrum, C.F.; Storm, G.; Hennink, W.E. Micelles based on HPMA copolymers. Adv. Drug Deliv. Rev. 2010, 62, 231–239. [Google Scholar] [CrossRef]
- Barz, M.; Tarantola, M.; Fischer, K.; Schmidt, M.; Luxenhofer, R.; Janshoff, A.; Theato, P.; Zentel, R. From Defined Reactive Diblock Copolymers to Functional HPMA-Based Self-Assembled Nanoaggregates. Biomacromolecules 2008, 9, 3114–3118. [Google Scholar] [CrossRef]
- Lele, B.S.; Leroux, J.C. Synthesis and micellar characterization of novel Amphiphilic A-B-A triblock copolymers of N-(2-hydroxypropyl)methacrylamide or N-vinyl-2-pyrrolidone with poly(is an element of-caprolactone). Macromolecules 2002, 35, 6714–6723. [Google Scholar] [CrossRef]
- Barz, M.; Wolf, F.K.; Canal, F.; Koynov, K.; Vicent, M.J.; Frey, H.; Zentel, R. Synthesis, Characterization and Preliminary Biological Evaluation of P(HPMA)-b-P(LLA) Copolymers: A New Type of Functional Biocompatible Block Copolymer. Macromol. Rapid Commun. 2010, 31, 1492–1500. [Google Scholar] [CrossRef]
- Braunová, A.; Kostka, L.; Sivák, L.; Cuchalová, L.; Hvězdová, Z.; Laga, R.; Filippov, S.; Černoch, P.; Pechar, M.; Janoušková, O.; et al. Tumor-targeted micelle-forming block copolymers for overcoming of multidrug resistance. J. Control. Release 2017, 245, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Alfurhood, J.A.; Sun, H.; Kabb, C.P.; Tucker, B.S.; Matthews, J.H.; Luesch, H.; Sumerlin, B.S. Poly(N-(2-hydroxypropyl)methacrylamide)–valproic acid conjugates as block copolymer nanocarriers. Polym. Chem. 2017, 8, 4983–4987. [Google Scholar] [CrossRef] [PubMed]
- Naksuriya, O.; Shi, Y.; van Nostrum, C.F.; Anuchapreeda, S.; Hennink, W.E.; Okonogi, S. HPMA-based polymeric micelles for curcumin solubilization and inhibition of cancer cell growth. Eur. J. Pharm. Biopharm. 2015, 94, 501–512. [Google Scholar] [CrossRef] [PubMed]
- Bláhová, M.; Randárová, E.; Konefal, R.; Nottelet, B.; Etrych, T. Graft copolymers with tunable amphiphilicity tailored for efficient dual drug deliveryviaencapsulation and pH-sensitive drug conjugation. Polym. Chem. 2020, 11, 4438–4453. [Google Scholar] [CrossRef]
- Chytil, P.; Etrych, T.; Koňák, Č.; Šírová, M.; Mrkvan, T.; Bouček, J.; Říhová, B.; Ulbrich, K. New HPMA copolymer-based drug carriers with covalently bound hydrophobic substituents for solid tumour targeting. J. Control. Release 2008, 127, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Chytil, P.; Etrych, T.; Kostka, L.; Ulbrich, K. Hydrolytically Degradable Polymer Micelles for Anticancer Drug Delivery to Solid Tumors. Macromol. Chem. Phys. 2012, 213, 858–867. [Google Scholar] [CrossRef]
- Zhou, Z.; Li, L.; Yang, Y.; Xu, X.; Huang, Y. Tumor targeting by pH-sensitive, biodegradable, cross-linked N-(2-hydroxypropyl) methacrylamide copolymer micelles. Biomaterials 2014, 35, 6622–6635. [Google Scholar] [CrossRef]
- Koziolová, E.; Machová, D.; Pola, R.; Janoušková, O.; Chytil, P.; Laga, R.; Filippov, S.K.; Šubr, V.; Etrych, T.; Pechar, M. Micelle-forming HPMA copolymer conjugates of ritonavir bound via a pH-sensitive spacer with improved cellular uptake designed for enhanced tumor accumulation. J. Mater. Chem. B 2016, 4, 7620–7629. [Google Scholar] [CrossRef] [Green Version]
- Chytil, P.; Šírová, M.; Kudláčová, J.; Říhová, B.; Ulbrich, K.; Etrych, T. Bloodstream Stability Predetermines the Antitumor Efficacy of Micellar Polymer-Doxorubicin Drug Conjugates with pH-Triggered Drug Release. Mol. Pharm. 2018, 15, 3654–3663. [Google Scholar] [CrossRef]
- Jia, Z.; Wong, L.; Davis, T.P.; Bulmus, V. One-Pot Conversion of RAFT-Generated Multifunctional Block Copolymers of HPMA to Doxorubicin Conjugated Acid- and Reductant-Sensitive Crosslinked Micelles. Biomacromolecules 2008, 9, 3106–3113. [Google Scholar] [CrossRef]
- Klepac, D.; Kostková, H.; Petrova, S.; Chytil, P.; Etrych, T.; Kereiche, S.; Raska, I.; Weitz, D.A.; Filippov, S.K. Interaction of spin-labeled HPMA-based nanoparticles with human blood plasma proteins—The introduction of protein-corona-free polymer nanomedicine. Nanoscale 2018, 10, 6194–6204. [Google Scholar] [CrossRef]
- Janisová, L.; Gruzinov, A.; Zaborova, O.V.; Velychkivska, N.; Vaněk, O.; Chytil, P.; Etrych, T.; Janoušková, O.; Zhang, X.H.; Blanchet, C.; et al. Molecular Mechanisms of the Interactions of N-(2-Hydroxypropyl)methacrylamide Copolymers Designed for Cancer Therapy with Blood Plasma Proteins. Pharmaceutics 2020, 12, 106. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.H.; Niebuur, B.J.; Chytil, P.; Etrych, T.; Filippov, S.K.; Kikhney, A.; Wieland, D.C.F.; Svergun, D.I.; Papadakis, C.M. Macromolecular pHPMA-Based Nanoparticles with Cholesterol for Solid Tumor Targeting: Behavior in HSA Protein Environment. Biomacromolecules 2018, 19, 470–480. [Google Scholar] [CrossRef]
- Etrych, T.; Mrkvan, T.; Chytil, P.; Koňák, Č.; Říhová, B.; Ulbrich, K. N-(2-hydroxypropyl)methacrylamide-based polymer conjugates with pH-controlled activation of doxorubicin. I. New synthesis, physicochemical characterization and preliminary biological evaluation. J. Appl. Polym. Sci. 2008, 109, 3050–3061. [Google Scholar] [CrossRef]
- Lomkova, E.A.; Chytil, P.; Janoušková, O.; Mueller, T.; Lucas, H.; Filippov, S.K.; Trhlíková, O.; Aleshunin, P.A.; Skorik, Y.A.; Ulbrich, K.; et al. Biodegradable Micellar HPMA-Based Polymer-Drug Conjugates with Betulinic Acid for Passive Tumor Targeting. Biomacromolecules 2016, 17, 3493–3507. [Google Scholar] [CrossRef]
- Luan, B.; Muir, B.W.; Zhu, J.; Hao, X. A RAFT copolymerization of NIPAM and HPMA and evaluation of thermo-responsive properties of poly(NIPAM-co-HPMA). RSC Adv. 2016, 6, 89925–89933. [Google Scholar] [CrossRef]
- Laga, R.; Janoušková, O.; Ulbrich, K.; Pola, R.; Blažková, J.; Filippov, S.K.; Etrych, T.; Pechar, M. Thermoresponsive Polymer Micelles as Potential Nanosized Cancerostatics. Biomacromolecules 2015, 16, 2493–2505. [Google Scholar] [CrossRef]
- Truong, N.P.; Whittaker, M.R.; Anastasaki, A.; Haddleton, D.M.; Quinn, J.F.; Davis, T.P. Facile production of nanoaggregates with tuneable morphologies from thermoresponsive P(DEGMA-co-HPMA). Polym. Chem. 2016, 7, 430–440. [Google Scholar] [CrossRef]
- Shi, Y.; van den Dungen, E.T.A.; Klumperman, B.; van Nostrum, C.F.; Hennink, W.E. Reversible Addition–Fragmentation Chain Transfer Synthesis of a Micelle-Forming, Structure Reversible Thermosensitive Diblock Copolymer Based on the N-(2-Hydroxy propyl) Methacrylamide Backbone. ACS Macro Lett. 2013, 2, 403–408. [Google Scholar] [CrossRef]
- Maeda, H.; Khatami, M. Analyses of repeated failures in cancer therapy for solid tumors: Poor tumor-selective drug delivery, low therapeutic efficacy and unsustainable costs. Clin. Transl. Med. 2018, 7, 11. [Google Scholar] [CrossRef]
- Sosman, J.A.; Kim, K.B.; Schuchter, L.; Gonzalez, R.; Pavlick, A.C.; Weber, J.S.; McArthur, G.A.; Hutson, T.E.; Moschos, S.J.; Flaherty, K.T.; et al. Survival in BRAF V600–Mutant Advanced Melanoma Treated with Vemurafenib. N. Engl. J. Med. 2012, 366, 707–714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerlinger, M.; Rowan, A.J.; Horswell, S.; Larkin, J.; Endesfelder, D.; Gronroos, E.; Martinez, P.; Matthews, N.; Stewart, A.; Tarpey, P.; et al. Intratumor Heterogeneity and Branched Evolution Revealed by Multiregion Sequencing. N. Engl. J. Med. 2012, 366, 883–892. [Google Scholar] [CrossRef] [Green Version]
- Hernández-Camarero, P.; Amezcua-Hernández, V.; Jiménez, G.; García, M.A.; Marchal, J.A.; Perán, M. Clinical failure of nanoparticles in cancer: Mimicking nature’s solutions. Nanomedicine 2020, 15, 2311–2324. [Google Scholar] [CrossRef]
- He, H.L.; Liu, L.S.; Morin, E.E.; Liu, M.; Schwendeman, A. Survey of Clinical Translation of Cancer Nanomedicines-Lessons Learned from Successes and Failures. Acc. Chem. Res. 2019, 52, 2445–2461. [Google Scholar] [CrossRef]
- Hare, J.I.; Lammers, T.; Ashford, M.B.; Puri, S.; Storm, G.; Barry, S.T. Challenges and strategies in anti-cancer nanomedicine development: An industry perspective. Adv. Drug Deliv. Rev. 2017, 108, 25–38. [Google Scholar] [CrossRef] [Green Version]
- Shi, J.J.; Kantoff, P.W.; Wooster, R.; Farokhzad, O.C. Cancer nanomedicine: Progress, challenges and opportunities. Nat. Rev. Cancer 2017, 17, 20–37. [Google Scholar] [CrossRef] [PubMed]
- Folkman, J. What Is the Evidence That Tumors Are Angiogenesis Dependent? JNCI J. Natl. Cancer Inst. 1990, 82, 4–7. [Google Scholar] [CrossRef] [Green Version]
- Fang, J.; Islam, W.; Maeda, H. Exploiting the dynamics of the EPR effect and strategies to improve the therapeutic effects of nanomedicines by using EPR effect enhancers. Adv. Drug Deliv. Rev. 2020, 157, 142–160. [Google Scholar] [CrossRef] [PubMed]
- Navi, B.B.; Reiner, A.S.; Kamel, H.; Iadecola, C.; Okin, P.M.; Tagawa, S.T.; Panageas, K.S.; DeAngelis, L.M. Arterial thromboembolic events preceding the diagnosis of cancer in older persons. Blood 2019, 133, 781–789. [Google Scholar] [CrossRef] [PubMed]
- Young, A.; Chapman, O.; Connor, C.; Poole, C.; Rose, P.; Kakkar, A.K. Thrombosis and cancer. Nat. Rev. Clin. Oncol. 2012, 9, 437–449. [Google Scholar] [CrossRef]
- Jain, R.K. Transport of molecules across tumor vasculature. Cancer Metastasis Rev. 1987, 6, 559–593. [Google Scholar] [CrossRef]
- Islam, W.; Fang, J.; Imamura, T.; Etrych, T.; Šubr, V.; Ulbrich, K.; Maeda, H. Augmentation of the Enhanced Permeability and Retention Effect with Nitric Oxide–Generating Agents Improves the Therapeutic Effects of Nanomedicines. Mol. Cancer Ther. 2018, 17, 2643–2653. [Google Scholar] [CrossRef] [Green Version]
- Seki, T.; Fang, J.; Maeda, H. Enhanced delivery of macromolecular antitumor drugs to tumors by nitroglycerin application. Cancer Sci. 2009, 100, 2426–2430. [Google Scholar] [CrossRef]
- Jiang, J.; Jordan, S.J.; Barr, D.P.; Gunther, M.R.; Maeda, H.; Mason, R.P. In Vivo Production of Nitric Oxide in Rats after Administration of Hydroxyurea. Mol. Pharm. 1997, 52, 1081–1086. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dozono, H.; Yanazume, S.; Nakamura, H.; Etrych, T.; Chytil, P.; Ulbrich, K.; Fang, J.; Arimura, T.; Douchi, T.; Kobayashi, H.; et al. HPMA Copolymer-Conjugated Pirarubicin in Multimodal Treatment of a Patient with Stage IV Prostate Cancer and Extensive Lung and Bone Metastases. Target Oncol. 2016, 11, 101–106. [Google Scholar] [CrossRef]
- Fang, J.; Islam, R.; Islam, W.; Yin, H.Z.; Šubr, V.; Etrych, T.; Ulbrich, K.; Maeda, H. Augmentation of EPR Effect and Efficacy of Anticancer Nanomedicine by Carbon Monoxide Generating Agents. Pharmaceutics 2019, 11, 343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Studenovský, M.; Sivák, L.; Sedláček, O.; Konefal, R.; Horková, V.; Etrych, T.; Kovář, M.; Říhová, B.; Šírová, M. Polymer nitric oxide donors potentiate the treatment of experimental solid tumours by increasing drug accumulation in the tumour tissue. J. Control. Release 2018, 269, 214–224. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, R.; Ishima, Y.; Chuang, V.T.G.; Nakamura, H.; Fang, J.; Watanabe, H.; Shimizu, T.; Okuhira, K.; Ishida, T.; Maeda, H.; et al. Improved anticancer effects of albumin-bound paclitaxel nanoparticle via augmentation of EPR effect and albumin-protein interactions using S-nitrosated human serum albumin dimer. Biomaterials 2017, 140, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.; Kim, J.; Lee, Y.M.; Im, S.; Park, H.; Kim, W.J. Nitric oxide-releasing polymer incorporated ointment for cutaneous wound healing. J. Control. Release 2015, 220, 624–630. [Google Scholar] [CrossRef]
- Danhier, F.; Feron, O.; Préat, V. To exploit the tumor microenvironment: Passive and active tumor targeting of nanocarriers for anti-cancer drug delivery. J. Control. Release 2010, 148, 135–146. [Google Scholar] [CrossRef]
- Samuli, H.; Catherine, P.; Jean-Pierre, B. Passive and Active Tumour Targeting with Nanocarriers. Curr. Drug Discov. Technol. 2011, 8, 188–196. [Google Scholar] [CrossRef]
- Attia, M.F.; Anton, N.; Wallyn, J.; Omran, Z.; Vandamme, T.F. An overview of active and passive targeting strategies to improve the nanocarriers efficiency to tumour sites. J. Pharm. Pharmacol. 2019, 71, 1185–1198. [Google Scholar] [CrossRef] [Green Version]
- Seymour, L.W.; Miyamoto, Y.; Maeda, H.; Brereton, M.; Strohalm, J.; Ulbrich, K.; Duncan, R. Influence of molecular weight on passive tumour accumulation of a soluble macromolecular drug carrier. Eur. J. Cancer 1995, 31, 766–770. [Google Scholar] [CrossRef]
- Kopeček, J.; Kopečková, P. HPMA copolymers: Origins, early developments, present, and future. Adv. Drug Deliv. Rev. 2010, 62, 122–149. [Google Scholar] [CrossRef] [Green Version]
- Yang, J.; Kopeček, J. Design of smart HPMA copolymer-based nanomedicines. J. Control. Release 2016, 240, 9–23. [Google Scholar] [CrossRef] [Green Version]
- Pola, R.; Böhmová, E.; Filipová, M.; Pechar, M.; Pankrác, J.; Větvička, D.; Olejár, T.; Kabešová, M.; Poučková, P.; Šefc, L.; et al. Targeted Polymer-Based Probes for Fluorescence Guided Visualization and Potential Surgery of EGFR-Positive Head-and-Neck Tumors. Pharmaceutics 2020, 12, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Randárová, E.; Kudláčová, J.; Etrych, T. HPMA copolymer-antibody constructs in neoplastic treatment: An overview of therapeutics, targeted diagnostics, and drug-free systems. J. Control. Release 2020, 325, 304–322. [Google Scholar] [CrossRef]
- Ulbrich, K.; Šubr, V.; Strohalm, J.; Plocová, D.; Jelínková, M.; Říhová, B. Polymeric drugs based on conjugates of synthetic and natural macromolecules I. Synthesis and physico-chemical characterisation. J. Control. Release 2000, 64, 63–79. [Google Scholar] [CrossRef]
- Lidický, O.; Klener, P.; Machová, D.; Vočková, P.; Pokorná, E.; Helman, K.; Mavis, C.; Janoušková, O.; Etrych, T. Overcoming resistance to rituximab in relapsed non-Hodgkin lymphomas by antibody-polymer drug conjugates actively targeted by anti-CD38 daratumumab. J. Control. Release 2020, 328, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Kovář, M.; Mrkvan, T.; Strohalm, J.; Etrych, T.; Ulbrich, K.; Štastný, M.; Říhová, B. HPMA copolymer-bound doxorubicin targeted to tumor-specific antigen of BCL1 mouse B cell leukemia. J. Control. Release 2003, 92, 315–330. [Google Scholar] [CrossRef]
- Kovář, M.; Strohalm, J.; Etrych, T.; Ulbrich, K.; Říhová, B. Star structure of antibody-targeted HPMA copolymer-bound doxorubicin: A novel type of polymeric conjugate for targeted drug delivery with potent antitumor effect. Bioconj. Chem. 2002, 13, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Kunjachan, S.; Pola, R.; Gremse, F.; Theek, B.; Ehling, J.; Moeckel, D.; Hermanns-Sachweh, B.; Pechar, M.; Ulbrich, K.; Hennink, W.E.; et al. Passive versus Active Tumor Targeting Using RGD- and NGR-Modified Polymeric Nanomedicines. Nano Lett. 2014, 14, 972–981. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sindhwani, S.; Syed, A.M.; Ngai, J.; Kingston, B.R.; Maiorino, L.; Rothschild, J.; MacMillan, P.; Zhang, Y.; Rajesh, N.U.; Hoang, T.; et al. The entry of nanoparticles into solid tumours. Nat. Mater. 2020, 19, 566–575. [Google Scholar] [CrossRef] [PubMed]







Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chytil, P.; Kostka, L.; Etrych, T. HPMA Copolymer-Based Nanomedicines in Controlled Drug Delivery. J. Pers. Med. 2021, 11, 115. https://doi.org/10.3390/jpm11020115
Chytil P, Kostka L, Etrych T. HPMA Copolymer-Based Nanomedicines in Controlled Drug Delivery. Journal of Personalized Medicine. 2021; 11(2):115. https://doi.org/10.3390/jpm11020115
Chicago/Turabian StyleChytil, Petr, Libor Kostka, and Tomáš Etrych. 2021. "HPMA Copolymer-Based Nanomedicines in Controlled Drug Delivery" Journal of Personalized Medicine 11, no. 2: 115. https://doi.org/10.3390/jpm11020115
APA StyleChytil, P., Kostka, L., & Etrych, T. (2021). HPMA Copolymer-Based Nanomedicines in Controlled Drug Delivery. Journal of Personalized Medicine, 11(2), 115. https://doi.org/10.3390/jpm11020115