Emotional Reaction to the First Dose of COVID-19 Vaccine: Postvaccination Decline in Anxiety and Stress among Anxious Individuals and Increase among Individuals with Normal Prevaccination Anxiety Levels
Abstract
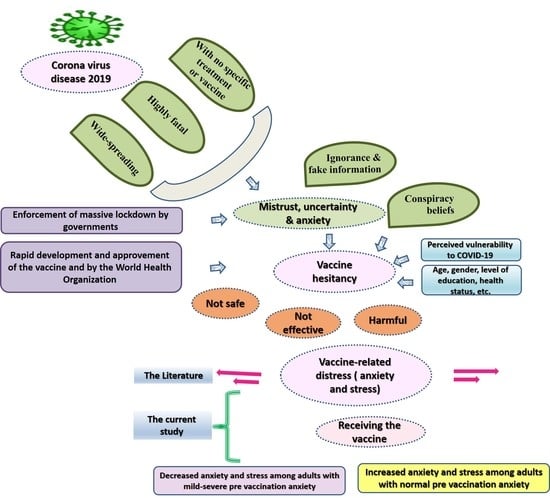
:1. Introduction
2. Materials and Methods
2.1. Design, Setting, and Sampling
2.2. Measurements
2.3. Data Collection Procedure and Ethical Considerations
2.4. Statistical Analysis
3. Results
4. Discussion
Strength, Implications, and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sohrabi, C.; Alsafi, Z.; O’neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.M.; Kunugi, H. Propolis, bee honey, and their components protect against coronavirus disease 2019 (COVID-19): A review of in silico, in vitro, and clinical studies. Molecules 2021, 26, 1232. [Google Scholar] [CrossRef]
- Ali, A.M.; Alkhamees, A.A.; Elhay, E.S.A.; Taha, S.M.; Hendawy, A.O. COVID-19-related psychological trauma and psychological distress among community-dwelling psychiatric patients: People struck by depression and sleep disorders endure the greatest burden . Front. Public Health 2022, 9, 799812. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Rational Use of Personal Protective Equipment for Coronavirus Disease (COVID-19): INTERIM Guidance, 27 February 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Leach, M.; MacGregor, H.; Akello, G.; Babawo, L.; Baluku, M.; Desclaux, A.; Grant, C.; Kamara, F.; Nyakoi, M.; Parker, M.; et al. Vaccine anxieties, vaccine preparedness: Perspectives from Africa in a COVID-19 era. Soc. Sci. Med. 2022, 298, 114826. [Google Scholar] [CrossRef] [PubMed]
- Bono, S.A.; Faria de Moura Villela, E.; Siau, C.S.; Chen, W.S.; Pengpid, S.; Hasan, M.T.; Sessou, P.; Ditekemena, J.D.; Amodan, B.O.; Hosseinipour, M.C.; et al. Factors Affecting COVID-19 Vaccine Acceptance: An International Survey among Low- and Middle-Income Countries. Vaccines 2021, 9, 515. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Marks, F.; Clemens, J.D. Looking beyond COVID-19 vaccine phase 3 trials. Nat. Med. 2021, 27, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Rates of COVID-19 Cases and Deaths by Vaccination Status. Available online: https://covid.cdc.gov/covid-data-tracker/#rates-by-vaccine-status (accessed on 28 February 2022).
- Al-Marshoudi, S.; Al-Balushi, H.; Al-Wahaibi, A.; Al-Khalili, S.; Al-Maani, A.; Al-Farsi, N.; Al-Jahwari, A.; Al-Habsi, Z.; Al-Shaibi, M.; Al-Msharfi, M.; et al. Knowledge, Attitudes, and Practices (KAP) toward the COVID-19 Vaccine in Oman: A Pre-Campaign Cross-Sectional Study. Vaccines 2021, 9, 602. [Google Scholar] [CrossRef]
- Barry, M.; Temsah, M.H.; Alhuzaimi, A.; Alamro, N.; Al-Eyadhy, A.; Aljamaan, F.; Saddik, B.; Alhaboob, A.; Alsohime, F.; Alhasan, K.; et al. COVID-19 vaccine confidence and hesitancy among health care workers: A cross-sectional survey from a MERS-CoV experienced nation. PLoS ONE 2021, 16, e0244415. [Google Scholar] [CrossRef]
- Kashte, S.; Gulbake, A.; El-Amin, S.F., III; Gupta, A. COVID-19 vaccines: Rapid development, implications, challenges and future prospects. Hum. Cell 2021, 34, 711–733. [Google Scholar] [CrossRef]
- Dézsi, L.; Mészáros, T.; Kozma, G.; H-Velkei, M.; Oláh, C.Z.; Szabó, M.; Patkó, Z.; Fülöp, T.; Hennies, M.; Szebeni, M.; et al. A naturally hypersensitive porcine model may help understand the mechanism of COVID-19 mRNA vaccine-induced rare (pseudo) allergic reactions: Complement activation as a possible contributing factor. GeroScience 2022, 44, 597–618. [Google Scholar] [CrossRef]
- Simione, L.; Vagni, M.; Gnagnarella, C.; Bersani, G.; Pajardi, D. Mistrust and Beliefs in Conspiracy Theories Differently Mediate the Effects of Psychological Factors on Propensity for COVID-19 Vaccine. Front. Psychol. 2021, 12, 683684. [Google Scholar] [CrossRef] [PubMed]
- Bell, S.; Clarke, R.; Mounier-Jack, S.; Walker, J.L.; Paterson, P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine 2020, 38, 7789–7798. [Google Scholar] [CrossRef] [PubMed]
- Scrima, F.; Miceli, S.; Caci, B.; Cardaci, M. The relationship between fear of COVID-19 and intention to get vaccinated. The serial mediation roles of existential anxiety and conspiracy beliefs. Pers. Individ Dif. 2022, 184, 111188. [Google Scholar] [CrossRef]
- Qin, C.; Wang, R.; Tao, L.; Liu, M.; Liu, J. Acceptance of a Third Dose of COVID-19 Vaccine and Associated Factors in China Based on Health Belief Model: A National Cross-Sectional Study. Vaccines 2022, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.M.; Al-Amer, R.; Kunugi, H.; Stănculescu, E.; Taha, S.M.; Saleh, M.Y.; Alkhamees, A.A.; Hendawy, A.O. The Arabic version of the Impact of Event Scale—Revised: Psychometric evaluation in psychiatric patients and the general public within the context of COVID-19 outbreak and quaran-tine as collective traumatic events. J. Pers. Med. 2022, 12, 681. [Google Scholar] [CrossRef] [PubMed]
- Lockyer, B.; Islam, S.; Rahman, A.; Dickerson, J.; Pickett, K.; Sheldon, T.; Wright, J.; McEachan, R.; Sheard, L. Understanding COVID-19 misinformation and vaccine hesitancy in context: Findings from a qualitative study involving citizens in Bradford, UK. Health Expect. 2021, 24, 1158–1167. [Google Scholar] [CrossRef]
- Szmyd, B.; Karuga, F.F.; Bartoszek, A.; Staniecka, K.; Siwecka, N.; Bartoszek, A.; Błaszczyk, M.; Radek, M. Attitude and behaviors towards SARS-CoV-2 vaccination among healthcare workers: A cross-sectional study from Poland. Vaccines 2021, 9, 218. [Google Scholar] [CrossRef]
- Wisnivesky, J.P.; Govindarajulu, U.; Bagiella, E.; Goswami, R.; Kale, M.; Campbell, K.N.; Meliambro, K.; Chen, Z.; Aberg, J.A.; Lin, J.J. Association of Vaccination with the Persistence of Post-COVID Symptoms. J. Gen. Intern. Med. 2022, 37, 1748–1753. [Google Scholar] [CrossRef]
- Chen, S.; Aruldass, A.R.; Cardinal, R.N. Mental health outcomes after SARS-CoV-2 vaccination in the United States: A national cross-sectional study. J. Affect. Disord. 2022, 298, 396–399. [Google Scholar] [CrossRef]
- Hause, A.M.; Gee, J.; Johnson, T.; Jazwa, A.; Marquez, P.; Miller, E.; Su, J.; Shimabukuro, T.T.; Shay, D.K. Anxiety-related adverse event clusters after Janssen COVID-19 vaccination—five US mass vaccination sites, April 2021. MMWR Morb. Mortal Wkly. Rep. 2021, 70, 685–688. [Google Scholar] [CrossRef]
- Fadlilah, S.; Setiawan, D.I.; Murdhiono, W.R.; Wiyani, C.; Mindarsih, E.; Lustiyati, E.D.; Susanto, R. The Anxiety Facing the 1st Dose of Covid-19 Vaccination and Related Factors. Int. Med. J. 2022, 29, 38–42. [Google Scholar]
- Zheng, Y.B.; Sun, J.; Liu, L.; Zhao, Y.M.; Yan, W.; Yuan, K.; Su, S.Z.; Lu, Z.A.; Huang, Y.T.; Liu, L.; et al. COVID-19 Vaccine-Related Psychological Stress Among General Public in China. Front. Psychiatry 2021, 12, 774504. [Google Scholar] [CrossRef] [PubMed]
- Takano, T.; Hirose, M.; Yamasaki, Y.; Hara, M.; Okada, T.; Kunishima, H. Investigation of the incidence of immunisation stress-related response following COVID-19 vaccination in healthcare workers. J. Infect. Chemother. 2022, 28, 735–740. [Google Scholar] [CrossRef]
- CDC COVID-19 Response Team; Food and Drug Administration. Allergic Reactions Including Anaphylaxis after Receipt of the First Dose of Moderna COVID-19 Vaccine—United States, December 21 2020–January 10 2021. MMWR Morb. Mortal Wkly. Rep. 2021, 70, 125–129. [Google Scholar] [CrossRef]
- Shimabukuro, T.; Nair, N. Allergic Reactions Including Anaphylaxis after Receipt of the First Dose of Pfizer-BioNTech COVID-19 Vaccine. JAMA 2021, 325, 780–781. [Google Scholar] [CrossRef] [PubMed]
- Siripongsatian, D.; Kunawudhi, A.; Promteangtrong, C.; Kiatkittikul, P.; Jantarato, A.; Choolam, A.; Ponglikitmongkol, K.; Siripongboonsitti, T.; Kaeowirun, T.; Chotipanich, C. Alterations in 18F-FDG PET/MRI and 15O-Water PET Brain Findings in Patients with Neurological Symptoms after COVID-19 Vaccination: A Pilot Study. Clin. Nucl Med. 2022, 47, e230–e239. [Google Scholar] [CrossRef] [PubMed]
- Girish, V.; Lee, C.-K.; PJ, S.; Park, Y.-N. Examining the Feasibility of Vaccine Tourism. Tour. Int. Interdiscip. J. 2022, 70, 136–140. [Google Scholar] [CrossRef]
- Laith Al-Junaidi Jordan Begins COVID-19 Vaccine Rollout. Available online: https://www.aa.com.tr/en/latest-on-coronavirus-outbreak/jordan-begins-covid-19-vaccine-rollout/2108497 (accessed on 6 March 2022).
- United Nations High Commissioner for Refugees (UNHCR). COVID-19 Vaccine: All you need to know about the National Vaccination Campaign in Jordan! Available online: https://help.unhcr.org/jordan/en/frequently-asked-questions-unhcr/covid-19-vaccine/ (accessed on 6 March 2022).
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Ali, A.M.; Hori, H.; Kim, Y.; Kunugi, H. The Depression Anxiety Stress Scale 8-items expresses robust psychometric properties as an ideal shorter version of the Depression Anxiety Stress Scale 21 among healthy respondents from three continents. Front. Psychol. 2022, 13, 799769. [Google Scholar] [CrossRef]
- Ali, A.M.; Alkhamees, A.A.; Hori, H.; Kim, Y.; Kunugi, H. The Depression Anxiety Stress Scale 21: Development and Validation of the Depression Anxiety Stress Scale 8-item in Psychiatric Patients and the General Public for Easier Mental Health Measurement in a Post-COVID-19 World. Int. J. Environ. Res. Public Health 2021, 18, 10142. [Google Scholar] [CrossRef] [PubMed]
- Osman, A.; Wong, J.L.; Bagge, C.L.; Freedenthal, S.; Gutierrez, P.M.; Lozano, G. The Depression Anxiety Stress Scales-21 (DASS-21): Further examination of dimensions, scale reliability, and correlates. J. Clin. Psychol 2012, 68, 1322–1338. [Google Scholar] [CrossRef] [PubMed]
- Dwekat, E.; Al-amer, R.M.; Al-Daraawi, H.; Saleh, M.Y. Prevalence and Correlates of Depression and Anxiety among Jordanian Adolescents: A Cross-Sectional Study. Youth Soc. 2021. [Google Scholar] [CrossRef]
- Hao, F.; Wang, B.; Tan, W.; Husain, S.F.; McIntyre, R.S.; Tang, X.; Zhang, L.; Han, X.; Jiang, L.; Chew, N.W.S.; et al. Attitudes toward COVID-19 vaccination and willingness to pay: Comparison of people with and without mental disorders in China. BJPsych. Open 2021, 7, e146. [Google Scholar] [CrossRef] [PubMed]
- Eyllon, M.; Dang, A.P.; Barnes, J.B.; Buresh, J.; Peloquin, G.D.; Hogan, A.C.; Shimotsu, S.T.; Sama, S.R.; Nordberg, S.S. Associations between psychiatric morbidity and COVID-19 vaccine hesitancy: An analysis of electronic health records and patient survey. Psychiatry Res. 2022, 307, 114329. [Google Scholar] [CrossRef]
- Horiuchi, S.; Sakamoto, H.; Abe, S.K.; Shinohara, R.; Kushima, M.; Otawa, S.; Yui, H.; Akiyama, Y.; Ooka, T.; Kojima, R.; et al. Factors of parental COVID-19 vaccine hesitancy: A cross sectional study in Japan. PLoS ONE 2021, 16, e0261121. [Google Scholar] [CrossRef]
- Wang, Q.; Lv, C.; Han, X.; Shen, M.; Kuang, Y. A Web-Based Survey on Factors for Unvaccination and Adverse Reactions of SARS-CoV-2 Vaccines in Chinese Patients with Psoriasis. J. Inflamm Res. 2021, 14, 6265–6273. [Google Scholar] [CrossRef]
- Perez-Arce, F.; Angrisani, M.; Bennett, D.; Darling, J.; Kapteyn, A.; Thomas, K. COVID-19 vaccines and mental distress. PLoS ONE 2021, 16, e0256406. [Google Scholar] [CrossRef]
- Moccia, G.; Carpinelli, L.; Savarese, G.; Borrelli, A.; Boccia, G.; Motta, O.; Capunzo, M.; De Caro, F. Perception of Health, Mistrust, Anxiety, and Indecision in a Group of Italians Vaccinated against COVID-19. Vaccines 2021, 9, 612. [Google Scholar] [CrossRef]
- Kalinichev, M.; Easterling, K.W.; Plotsky, P.M.; Holtzman, S.G. Long-lasting changes in stress-induced corticosterone response and anxiety-like behaviors as a consequence of neonatal maternal separation in Long–Evans rats. Pharmacol. Biochem. Behav. 2002, 73, 131–140. [Google Scholar] [CrossRef]
- Abu-Hammad, O.; Alduraidi, H.; Abu-Hammad, S.; Alnazzawi, A.; Babkair, H.; Abu-Hammad, A.; Nourwali, I.; Qasem, F.; Dar-Odeh, N. Side Effects Reported by Jordanian Healthcare Workers Who Received COVID-19 Vaccines. Vaccines 2021, 9, 577. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.M.; Hendawy, A.O.; Ahmad, O.; Sabbah, H.A.; Smail, L.; Kunugi, H. The Arabic version of the Cohen perceived stress scale: Factorial validity and measurement invariance. Brain Sci. 2021, 11, 419. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.M.; Ahmed, A.H.; Smail, L. Psychological Climacteric Symptoms and Attitudes toward Menopause among Emirati Women. Int. J. Environ. Res. Public Health 2020, 17, 5028. [Google Scholar] [CrossRef]
- Lichlyter, D.A.; Krumm, Z.A.; Golde, T.A.; Doré, S. Role of CRF and the hypothalamic-pituitary-adrenal axis in stroke: Revisiting temporal considerations and targeting a new generation of therapeutics. FEBS J. 2022. [Google Scholar] [CrossRef]
- Lee, H.; Punt, J.A.; Miller, D.C.; Nagpal, A.; Smith, C.C.; Sayeed, Y.; Patel, J.; Stojanovic, M.P.; Popescu, A.; McCormick, Z.L. Do Corticosteroid Injections for the Treatment of Pain Influence the Efficacy of mRNA COVID-19 Vaccines? Pain Med. 2021, 22, 994–1000. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.M.; Park, Y.W.; Choi, E.J. Steroid injections in pain management: Influence on coronavirus disease 2019 vaccines. Korean J. Pain 2022, 35, 14–21. [Google Scholar] [CrossRef]
- Vollenberg, R.; Tepasse, P.-R.; Lorentzen, E.; Nowacki, T.M. Impaired Humoral Immunity with Concomitant Preserved T Cell Reactivity in IBD Patients on Treatment with Infliximab 6 Month after Vaccination with the SARS-CoV-2 mRNA Vaccine BNT162b2: A Pilot Study. J. Pers. Med. 2022, 12, 694. [Google Scholar] [CrossRef]
- Ali, A.M.; Kunugi, H. Physical frailty/sarcopenia as a key predisposing factor to coronavirus disease 2019 (COVID-19) and its complications in older adults. BioMed 2021, 1, 2. [Google Scholar] [CrossRef]
- Ali, A.M.; Kunugi, H. Apitherapy for age-related skeletal muscle dysfunction (sarcopenia): A review on the effects of royal jelly, propolis, and bee pollen. Foods 2020, 9, 1362. [Google Scholar] [CrossRef]
- Ali, A.M.; Hendawy, A.O.; Almarwani, A.M.; Alzahrani, N.; Ibrahim, N.; Alkhamees, A.A.; Kunugi, H. The Six-item Version of the Internet Addiction Test: Its development, psychometric properties, and measurement invariance among women with eating disorders and healthy school and university students. Int. J. Environ. Res. Public Health 2021, 18, 12341. [Google Scholar] [CrossRef]
- Ali, A.M.; Hori, H.; Kim, Y.; Kunugi, H. Predictors of nutritional status, depression, internet addiction, Facebook addiction, and tobacco smoking among women with eating disorders in Spain. Front. Psychiatry 2021, 12, 2001. [Google Scholar] [CrossRef] [PubMed]
- Sznajder, K.K.; Kjerulff, K.H.; Wang, M.; Hwang, W.; Ramirez, S.I.; Gandhi, C.K. COVID-19 vaccine acceptance and associated factors among pregnant women in Pennsylvania 2020. Prev. Med. Rep. 2022, 26, 101713. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Fighting Misinformation in the Time of COVID-19, One Click at a Time. Available online: https://www.who.int/news-room/feature-stories/detail/fighting-misinformation-in-the-time-of-covid-19-one-click-at-a-time (accessed on 3 May 2022).
- Center for Disease Control and Prevention (CDC). How to Address COVID-19 Vaccine Misinformation. Available online: https://www.cdc.gov/vaccines/covid-19/health-departments/addressing-vaccine-misinformation.html (accessed on 3 May 2022).
- Ali, A.M.; Hendawy, A.O.; Elhay, E.S.A.; Ali, E.M.; Alkhamees, A.A.; Kunugi, H.; Hassan, N.I. The Bergen Facebook Addiction Scale: Its psychometric properties and invariance among women with eating disorders. BMC Women’s Health 2022, 22, 99. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.M.; Al-Amer, R.; Atout, M.; Ali, T.S.; Mansour, A.M.H.; Khatatbeh, H.; Alkhamees, A.A.; Hendawy, A.O. The Nine-Item Internet Gaming Disorder Scale (IGDS9-SF): Its Psychometric Properties among Sri Lankan Students and Measurement Invariance across Sri Lanka, Turkey, Australia, and the USA. Healthcare 2022, 10, 490. [Google Scholar] [CrossRef] [PubMed]
- Bullock, J.; Lane, J.E.; Shults, F.L. What causes COVID-19 vaccine hesitancy? Ignorance and the lack of bliss in the United Kingdom. Humanit. Soc. Sci. Commun. 2022, 9, 1–7. [Google Scholar] [CrossRef]
- Ali, A.M.; Al-Amer, R. Dataset of Emotional reaction to the first dose of COVID-19 vaccine: Post vaccination decline in anxiety and stress among anxious individuals and increase among individuals with normal anxiety levels pre vaccination. Mendeley Data 2022, 1, 2022050082. [Google Scholar] [CrossRef]
| Variable | Before Vaccination n (%) | After Vaccination n (%) |
|---|---|---|
| Stress | ||
| No stress = 0–7 | 185 (74.0) | 217 (86.8) |
| Mild = 8–9 | 13 (5.2) | 12 (4.8) |
| Moderate = 10–12 | 20 (8.0) | 13 (5.2) |
| Severe = 13–16 | 20 (8.0) | 8 (3.2) |
| Extremely severe ≥ 17 | 12 (4.8) | 0 (0.0) |
| Anxiety | ||
| Normal = 0–3 | 126 (50.4) | 97 (38.8) |
| Mild = 4–5 | 31 (12.4) | 40 (16.0) |
| Moderate = 6–7 | 46 (18.4) | 82 (32.8) |
| Severe = 8–9 | 10 (4.0) | 17 (6.8) |
| Extremely severe ≥ 10 | 37 (14.8) | 14 (5.6) |
| Characteristics of the Respondents | n (%) |
|---|---|
| Gender | |
| Male | 70 (28) |
| Female | 180 (72) |
| Marital Status | |
| Single | 46 (18.4) |
| Married | 166 (66.4) |
| Divorce | 15 (6.0) |
| Widow | 23 (9.2) |
| Educational Level | |
| Secondary and less | 72 (28.8) |
| Higher than secondary | 178 (71.2) |
| Age in Years | |
| Mean (SD) | 43.18 (6.34) |
| Range | 18–63 |
| COVID-19 Infection History | |
| Yes | 19 (7.6) |
| No | 231 (92.4) |
| Pain at Injection Site | |
| Mild | 204 (81.6) |
| Moderate | 40 (16.0) |
| Severe | 6 (2.4) |
| Variables | Samples | MD (IQR) before Vaccination | MD (IQR) after Vaccination | z of Wilcoxon Signed-Rank Test | p | r |
|---|---|---|---|---|---|---|
| Stress | Whole sample (n = 250) | 5.0 (1.0–8.0) | 4.0 (1.0–7.0) | −3.81 | 0.001 | 0.17 |
| Anxiety | 3.0 (1.0–7.0) | 5.0 (1.0–7.0) | −0.53 | 0.597 | 0.02 | |
| Stress | Normal anxiety (n = 126) | 2.0 (0.0–4.0) | 4.5 (0.0–6.3) | −3.57 | 0.001 | 0.16 |
| Anxiety | 1.0 (0.0–2.0) | 5.0 (0.0–7.0) | −8.24 | 0.001 | 0.37 | |
| Stress | Mild anxiety (n = 31) | 4.0 (3.0–7.0) | 3.0 (3.0–5.0) | −1.28 | 0.201 | 0.06 |
| Anxiety | 4.0 (4.0–5.0) | 3.0 (3.0–5.0) | −2.70 | 0.007 | 0.12 | |
| Stress | Moderate–severe anxiety (n = 93) | 8.0 (7.0–14.0) | 5.0 (2.0–8.0) | −7.13 | 0.001 | 0.32 |
| Anxiety | 8.0 (7.0–13.0) | 6.0 (1.0–8.0) | −7.27 | 0.001 | 0.33 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Amer, R.; Malak, M.Z.; Burqan, H.M.R.; Stănculescu, E.; Nalubega, S.; Alkhamees, A.A.; Hendawy, A.O.; Ali, A.M. Emotional Reaction to the First Dose of COVID-19 Vaccine: Postvaccination Decline in Anxiety and Stress among Anxious Individuals and Increase among Individuals with Normal Prevaccination Anxiety Levels. J. Pers. Med. 2022, 12, 912. https://doi.org/10.3390/jpm12060912
Al-Amer R, Malak MZ, Burqan HMR, Stănculescu E, Nalubega S, Alkhamees AA, Hendawy AO, Ali AM. Emotional Reaction to the First Dose of COVID-19 Vaccine: Postvaccination Decline in Anxiety and Stress among Anxious Individuals and Increase among Individuals with Normal Prevaccination Anxiety Levels. Journal of Personalized Medicine. 2022; 12(6):912. https://doi.org/10.3390/jpm12060912
Chicago/Turabian StyleAl-Amer, Rasmieh, Malakeh Z. Malak, Hala Mohammad Ramadan Burqan, Elena Stănculescu, Sylivia Nalubega, Abdulmajeed A. Alkhamees, Amin Omar Hendawy, and Amira Mohammed Ali. 2022. "Emotional Reaction to the First Dose of COVID-19 Vaccine: Postvaccination Decline in Anxiety and Stress among Anxious Individuals and Increase among Individuals with Normal Prevaccination Anxiety Levels" Journal of Personalized Medicine 12, no. 6: 912. https://doi.org/10.3390/jpm12060912
APA StyleAl-Amer, R., Malak, M. Z., Burqan, H. M. R., Stănculescu, E., Nalubega, S., Alkhamees, A. A., Hendawy, A. O., & Ali, A. M. (2022). Emotional Reaction to the First Dose of COVID-19 Vaccine: Postvaccination Decline in Anxiety and Stress among Anxious Individuals and Increase among Individuals with Normal Prevaccination Anxiety Levels. Journal of Personalized Medicine, 12(6), 912. https://doi.org/10.3390/jpm12060912