Sepsis and Clinical Simulation: What Is New? (and Old)
Abstract
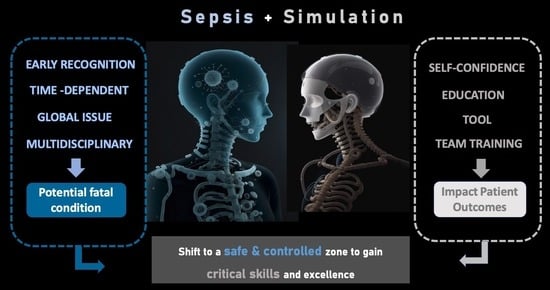
:1. Introduction
2. Sepsis, a Global Education Issue
3. Clinical Simulation: A Toolbox
4. From Theory to Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Rudd, K.E.; Johnson, S.C.; Agesa, K.M.; Shackelford, K.A.; Tsoi, D.; Kievlan, D.R.; Colombara, D.V.; Ikuta, K.S.; Kissoon, N.; Finfer, S.; et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet 2020, 395, 200–211. [Google Scholar] [CrossRef] [PubMed]
- Reinhart, K.; Daniels, R.; Kissoon, N.; Machado, F.R.; Schachter, R.D.; Finfer, S. Recognizing Sepsis as a Global Health Priority —A WHO Resolution. N. Engl. J. Med. 2017, 377, 414–417. [Google Scholar] [CrossRef] [PubMed]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; Mcintyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Intensiv. Care Med. 2021, 47, 1181–1247. [Google Scholar] [CrossRef]
- Trovato, G. SEPSIS. Educational and Best Practice Frontiers. Beyond the Boundaries of Fatality, Enhancing Clinical Skills and Precision Medicine. Ther. Clin. Risk Manag. 2020, 16, 87–93. [Google Scholar] [CrossRef]
- Okuda, Y.; Bryson, E.O.; DeMaria, S.; Jacobson, L.; Quinones, J.; Shen, B.; Levine, A.I. The Utility of Simulation in Medical Education: What Is the Evidence? Utility of simulation in medical education. Mt. Sinai J. Med. J. Transl. Pers. Med. 2009, 76, 330–343. [Google Scholar] [CrossRef] [PubMed]
- Nestel, D.; Groom, J.; Eikeland-Husebø, S.; O’Donnell, J.M. Simulation for Learning and Teaching Procedural Skills: The State of the Science. Simul. Healthc. J. Soc. Simul. Healthc. 2011, 6, S10–S13. [Google Scholar] [CrossRef] [PubMed]
- Vozenilek, J. See One, Do One, Teach One: Advanced Technology in Medical Education. Acad. Emerg. Med. 2004, 11, 1149–1154. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Paz, J.M.; Kennedy, M.; Salas, E.; Wu, A.W.; Sexton, J.B.; Hunt, E.A.; Pronovost, P.J. Beyond “see one, do one, teach one”: Toward a different training paradigm. Postgrad. Med. J. 2009, 85, 244–249. [Google Scholar] [CrossRef]
- Aggarwal, R.; Mytton, O.T.; Derbrew, M.; Hananel, D.; Heydenburg, M.; Issenberg, B.; MacAulay, C.; Mancini, M.E.; Morimoto, T.; Soper, N.; et al. Training and simulation for patient safety. Heart 2010, 19, i34–i43. [Google Scholar] [CrossRef]
- Phrampus, P.E. Simulation and Integration into Patient Safety Systems. Simul. Healthc. J. Soc. Simul. Healthc. 2018, 13, 225–226. [Google Scholar] [CrossRef]
- Bienstock, J.; Heuer, A.P. A review on the evolution of simulation-based training to help build a safer future. Medicine 2022, 101, e29503. [Google Scholar] [CrossRef] [PubMed]
- Goldshtein, D.; Krensky, C.; Doshi, S.; Perelman, V.S. In situ simulation and its effects on patient outcomes: A systematic review. BMJ Simul. Technol. Enhanc. Learn. 2019, 6, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.; Cross, S.; Attoe, C. The Use of in situ Simulation in Healthcare Education: Current Perspectives. Adv. Med. Educ. Pr. 2020, 11, 893–903. [Google Scholar] [CrossRef] [PubMed]
- Qian, J.; Wang, Y.; Zhang, Y.; Zhu, X.; Rong, Q.; Wei, H. A Survey of the First-Hour Basic Care Tasks of Severe Sepsis and Septic Shock in Pediatric Patients and an Evaluation of Medical Simulation on Improving the Compliance of the Tasks. J. Emerg. Med. 2016, 50, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Kessler, D.O.; Walsh, B.; Whitfill, T.; Gangadharan, S.; Gawel, M.; Brown, L.; Auerbach, M. Disparities in Adherence to Pediatric Sepsis Guidelines across a Spectrum of Emergency Departments: A Multicenter, Cross-Sectional Observational In Situ Simulation Study. J. Emerg. Med. 2015, 50, 403–415.e3. [Google Scholar] [CrossRef] [PubMed]
- Leng, O.M.; Rothwell, C.; Buckton, A.; Elmer, C.; Illing, J.; Metcalf, J. Effect of In Situ High-Fidelity Simulation Training on the Emergency management of Pneumonia (INSTEP): A mixed-methods study. BMJ Simul. Technol. Enhanc. Learn. 2018, 4, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Sharara-Chami, R.; Sabouneh, R.; Zeineddine, R.; Banat, R.; Fayad, J.; Lakissian, Z. In Situ Simulation: An Essential Tool for Safe Preparedness for the COVID-19 Pandemic. Simul. Healthc. J. Soc. Simul. Healthc. 2020, 15, 303–309. [Google Scholar] [CrossRef]
- Gordon, M.; Box, H.; Farrell, M.; Stewrt, A. Non-technical skills learning in healthcare through simulation education: Integrating the SECTORS learning model and complexity theory. BMJ Simul. Technol. Enhanc. Learn. 2015, 1, 67–70. [Google Scholar] [CrossRef]
- Fung, L.; Boet, S.; Bould, M.D.; Qosa, H.; Perrier, L.; Tricco, A.; Tavares, W.; Reeves, S. Impact of crisis resource management simulation-based training for interprofessional and interdisciplinary teams: A systematic review. J. Interprofessional Care 2015, 29, 433–444. [Google Scholar] [CrossRef]
- Fleischmann-Struzek, C.; Mellhammar, L.; Rose, N.; Cassini, A.; Rudd, K.E.; Schlattmann, P.; Allegranzi, B.; Reinhart, K. Incidence and mortality of hospital- and ICU-treated sepsis: Results from an updated and expanded systematic review and meta-analysis. Intensiv. Care Med. 2020, 46, 1552–1562. [Google Scholar] [CrossRef]
- Slade, E.; Tamber, P.S.; Vincent, J.L. The Surviving Sepsis Campaign: Raising awareness to reduce mortality. Crit. Care 2003, 7, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Dellinger, R.P.; Carlet, J.M.; Masur, H.; Gerlach, H.; Calandra, T.; Cohen, J.; Gea-Banacloche, J.; Keh, D.; Marshall, J.C.; Parker, M.M.; et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit. Care Med. 2004, 32, 858–873. [Google Scholar] [CrossRef]
- Dellinger, R.P.; Rhodes, A.; Evans, L.; Alhazzani, W.; Beale, R.; Jaeschke, R.; Machado, F.R.; Masur, H.; Osborn, T.; Parker, M.M.; et al. Surviving Sepsis Campaign. Crit. Care Med. 2023, 51, 431–444. [Google Scholar] [CrossRef] [PubMed]
- Levy, M.M.; Dellinger, R.P.; Townsend, S.R.; Linde-Zwirble, W.T.; Marshall, J.C.; Bion, J.; Schorr, C.; Artigas, A.; Ramsay, G.; Beale, R.; et al. The Surviving Sepsis Campaign: Results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med. 2010, 36, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Jozwiak, M.; Monnet, X.; Teboul, J.-L. Implementing sepsis bundles. Ann. Transl. Med. 2016, 4, 332. [Google Scholar] [CrossRef] [PubMed]
- Baghdadi, J.D.; Brook, R.H.; Uslan, D.Z.; Needleman, J.; Bell, D.S.; Cunningham, W.E.; Wong, M.D. Association of a Care Bundle for Early Sepsis Management with Mortality Among Patients With Hospital-Onset or Community-Onset Sepsis. JAMA Intern. Med. 2020, 180, 707–716. [Google Scholar] [CrossRef] [PubMed]
- Levy, M.M.; Pronovost, P.J.; Dellinger, R.P.; Townsend, S.; Resar, R.K.; Clemmer, T.P.; Ramsay, G. Sepsis change bundles: Converting guidelines into meaningful change in behavior and clinical outcome. Crit. Care Med. 2004, 32 (Suppl. S11), S595–S597. [Google Scholar] [CrossRef]
- Deis, A.S.; Whiles, B.B.; Brown, A.R.; Satterwhite, C.L.; Simpson, S.Q. Three-Hour Bundle Compliance and Outcomes in Patients with Undiagnosed Severe Sepsis. Chest 2018, 153, 39–45. [Google Scholar] [CrossRef]
- Damiani, E.; Donati, A.; Serafini, G.; Rinaldi, L.; Adrario, E.; Pelaia, P.; Busani, S.; Girardis, M. Effect of Performance Improvement Programs on Compliance with Sepsis Bundles and Mortality: A Systematic Review and Meta-Analysis of Observational Studies. PLoS ONE 2015, 10, e0125827. [Google Scholar] [CrossRef]
- Cowan, S.; Holland, J.; Kane, A.; Frost, I. What are the barriers to improving care for patients with sepsis? Clin. Med. 2015, 15 (Suppl. S3), S24. [Google Scholar] [CrossRef]
- Watkins, R.R.; Haller, N.; Wayde, M.; Armitage, K.B. A Multicenter Survey of House Staff Knowledge About Sepsis and the “Surviving Sepsis Campaign Guidelines for Management of Severe Sepsis and Septic Shock”. J. Intensiv. Care Med. 2017, 35, 187–190. [Google Scholar] [CrossRef]
- Choy, C.; Liaw, S.; Goh, E.; See, K.; Chua, W. Impact of sepsis education for healthcare professionals and students on learning and patient outcomes: A systematic review. J. Hosp. Infect. 2022, 122, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Fiest, K.M.; Krewulak, K.D.; Brundin-Mather, R.; Leia, M.P.; Fox-Robichaud, A.; Lamontagne, F.; Leigh, J.P.; Canada, F.S. Patient, Public, and Healthcare Professionals’ Sepsis Awareness, Knowledge, and Information Seeking Behaviors: A Scoping Review*. Crit. Care Med. 2022, 50, 1187–1197. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Torres, L.C.; Vega-Peña, N.V. Las pirámides de la educación médica: Una síntesis sobre su conceptualización y utilidad. Rev. Colomb. Obstet. Ginecol. 2023, 74, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Falletta, S. Evaluating Training Programs; Kirkpatrick, D.L., Kirkpatrick, J.D., Eds.; Berrett-Koehler Publishers: San Francisco, CA, USA, 2009. [Google Scholar]
- Frye, A.W.; Hemmer, P.A. Program evaluation models and related theories: AMEE Guide No. 67. Med. Teach. 2012, 34, e288–e299. [Google Scholar] [CrossRef] [PubMed]
- Rababa, M.; Hamad, D.B.; Hayajneh, A.A. Sepsis assessment and management in critically Ill adults: A systematic review. PLoS ONE 2022, 17, e0270711. [Google Scholar] [CrossRef] [PubMed]
- Swanwick, T. Understanding Medical Education. In Understanding Medical Education: Evidence, Theory, and Practice, 2nd ed.; Wiley Blackwell: Hoboken, NJ, USA, 2014. [Google Scholar]
- Ferrer, R. Improvement in Process of Care and Outcome After a Multicenter Severe Sepsis Educational Program in Spain. JAMA. 2008, 299, 2294. [Google Scholar] [CrossRef] [PubMed]
- Li, C.-H.; Kuan, W.-S.; Mahadevan, M.; Daniel-Underwood, L.; Chiu, T.-F.; Nguyen, H.B. A multinational randomised study comparing didactic lectures with case scenario in a severe sepsis medical simulation course. Emerg. Med. J. 2011, 29, 559–564. [Google Scholar] [CrossRef]
- Lucey, C.R.; Johnston, S.C. The Transformational Effects of COVID-19 on Medical Education. JAMA 2020, 324, 1033–1034. [Google Scholar] [CrossRef]
- Cook, D.A.; Garside, S.; Levinson, A.J.; Dupras, D.M.; Montori, V.M. What do we mean by web-based learning? A systematic review of the variability of interventions: What do we mean by web-based learning? Med. Educ. 2010, 44, 765–774. [Google Scholar] [CrossRef]
- Walsh, K. E-learning in medical education: The potential environmental impact. Educ. Prim. Care 2017, 29, 104–106. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; He, J.; Yuan, C.; Chen, B.; Sun, Z. The effects of blended learning on knowledge, skills, and satisfaction in nursing students: A meta-analysis. Nurse Educ. Today 2019, 82, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Van Gaalen, A.E.J.; Brouwer, J.; Schönrock-Adema, J.; Bouwkamp-Timmer, T.; Jaarsma, A.D.C.; Georgiadis, J.R. Gamification of health professions education: A systematic review. Adv. Health Sci. Educ. 2021, 26, 683–711. [Google Scholar] [CrossRef] [PubMed]
- Evans, K.H.; Daines, W.; Tsui, J.; Strehlow, M.; Maggio, P.; Shieh, L. Septris: A Novel, Mobile, Online, Simulation Game That Improves Sepsis Recognition and Management. Acad. Med. 2015, 90, 180–184. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, C.; Monteiro, M.; Hauge, J.B.; Pereira, J.; Antunes, T. Sepsis Fast Track: A simulation game for Clinical education based on the Sepsis Fast Track. protocol. In Proceedings of the 2016 IEEE International Conference on Serious Games and Applications for Health, Orlando, FL, USA, 11–13 May 2016; pp. 1–8. [Google Scholar] [CrossRef]
- Alejandre, C.; Corniero, P.; Claret, G.; Alaez, C.; Esteban, E.; Jordan, I. New Resident Training Strategy Based on Gamification Techniques: An Escape Room on Sepsis in Children. Children 2022, 9, 1503. [Google Scholar] [CrossRef] [PubMed]
- Lighthall, G.K.; Bahmani, D.; Gaba, D. Evaluating the Impact of Classroom Education on the Management of Septic Shock Using Human Patient Simulation. Simul. Heal. J. Soc. Simul. Health 2016, 11, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Breuer, R.K.; Hassinger, A.B. Impact of a Multidisciplinary Sepsis Initiative on Knowledge and Behavior in a Pediatric Center. Pediatr. Qual. Saf. 2020, 5, e267. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.-O.; Medina, D.; Fox-Robichaud, A. Interprofessional sepsis education module: A pilot study. CJEM 2015, 18, 143–145. [Google Scholar] [CrossRef]
- Ventre, R.; Pardoe, C.; Cripps, D. Millennial learners—A blended approach to simulation for sepsis. Futur. Health J. 2020, 7, s108–s109. [Google Scholar] [CrossRef]
- Chua, W.L.; Legido-Quigley, H.; Jones, D.; Hassan, N.B.; Tee, A.; Liaw, S.Y. A call for better doctor–nurse collaboration: A qualitative study of the experiences of junior doctors and nurses in escalating care for deteriorating ward patients. Aust. Crit. Care 2020, 33, 54–61. [Google Scholar] [CrossRef]
- Cory, M.J.; Colman, N.; McCracken, C.E.; Hebbar, K.B. Rapid Cycle Deliberate Practice Versus Reflective Debriefing for Pediatric Septic Shock Training*. Pediatr. Crit. Care Med. 2019, 20, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Turi, S.K.; Von Ah, D. Implementation of Early Goal-directed Therapy for Septic Patients in the Emergency Department: A Review of the Literature. J. Emerg. Nurs. 2013, 39, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Gaba, D.M. The future vision of simulation in health care. BMJ Qual. Saf. 2004, 13, i2–i10. [Google Scholar] [CrossRef]
- Park, C.S.; Clark, L.; Gephardt, G.; Robertson, J.M.; Miller, J.; Downing, D.K.; Koh, B.L.S.; Bryant, K.D.; Grant, D.; Pai, D.R.; et al. Manifesto for healthcare simulation practice. BMJ Simul. Technol. Enhanc. Learn. 2020, 6, 365–368. [Google Scholar] [CrossRef] [PubMed]
- Rudolph, J.W.; Raemer, D.B.; Simon, R. Establishing a Safe Container for Learning in Simulation: The Role of the Presimulation Briefing. Simul. Healthc. J. Soc. Simul. Healthcare 2014, 9, 339–349. [Google Scholar] [CrossRef]
- Deutsch, E.S.; Dong, Y.; Halamek, L.P.; Rosen, M.A.; Taekman, J.M.; Rice, J. Leveraging Health Care Simulation Technology for Human Factors Research: Closing the Gap Between Lab and Bedside. Hum. Factors. 2016, 58, 1082–1095. [Google Scholar] [CrossRef] [PubMed]
- Macrae, C. Imitating Incidents: How Simulation Can Improve Safety Investigation and Learning from Adverse Events. Sim Healthcare 2018, 13, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Burden, A.R. High-Fidelity Simulation Education and Crisis Resource Management. Anesthesiol. Clin. 2020, 38, 745–759. [Google Scholar] [CrossRef]
- Roussin, C.J.; Weinstock, P. SimZones: An Organizational Innovation for Simulation Programs and Centers. Acad. Med. 2017, 92, 1114–1120. [Google Scholar] [CrossRef]
- Fey, M.K.; Roussin, C.J.; Rudolph, J.W.; Morse, K.J.; Palaganas, J.C.; Szyld, D. Teaching, coaching, or debriefing With Good Judgment: A roadmap for implementing “With Good Judgment” across the SimZones. Adv. Simul. 2022, 26, 39. [Google Scholar] [CrossRef]
- Fanning, R.M.; Gaba, D.M. The Role of Debriefing in Simulation-Based Learning. Simul. Healthc. J. Soc. Simul. Healthc. 2007, 2, 115–125. [Google Scholar] [CrossRef] [PubMed]
- Motola, I.; Devine, L.A.; Chung, H.S.; Sullivan, J.E.; Issenberg, S.B. Simulation in healthcare education: A best evidence practical guide. AMEE Guide No. 82. Med. Teach. 2013, 35, e1511–e1530. [Google Scholar] [CrossRef]
- Levine, A.I.; DeMaria, S.; Schwartz, A.D.; Sim, A.J. The Comprehensive Textbook of Healthcare Simulation; Springer: New York, NY, USA, 2013. [Google Scholar]
- Bessmann, E.L.; Østergaard, H.T.; Nielsen, B.U.; Russell, L.; Paltved, C.; Østergaard, D.; Konge, L.; Nayahangan, L.J. Consensus on technical procedures for simulation-based training in anaesthesiology: A Delphi-based general needs assessment. Acta Anaesthesiol. Scand. 2019, 63, 720–729. [Google Scholar] [CrossRef] [PubMed]
- Aherne, M.; Lamble, W.; Davis, P. Continuing medical education, needs assessment, and program development: Theoretical constructs. J. Contin. Educ. Health Prof. 2001, 21, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Zern, S.C.; Marshall, W.J.; Shewokis, P.A.; Vest, M.T. Use of simulation as a needs assessment to develop a focused team leader training curriculum for resuscitation teams. Adv. Simul. 2020, 5, 1–7. [Google Scholar] [CrossRef] [PubMed]
- McKimm, J.; Forrest, K. Essential Simulation in Clinical Education; Wiley Blackwell: Hoboken, NJ, USA, 2013; pp. 1–10. [Google Scholar] [CrossRef]
- Lopreiato, J.O. Healthcare Simulation Dictionary; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2016. [Google Scholar]
- Rutherford-Hemming, T.; Lioce, L.; Breymier, T. Guidelines and Essential Elements for Prebriefing. Simul. Health J. Soc. Simul. Health. 2019, 14, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Eller, S.; Rudolph, J.; Barwick, S.; Janssens, S.; Bajaj, K. Leading change in practice: How “longitudinal prebriefing” nurtures and sustains in situ simulation programs. Adv. Simul. 2023, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Benishek, L.E.; Lazzara, E.H.; Gaught, W.L.; Arcaro, L.L.; Okuda, Y.; Salas, E. The Template of Events for Applied and Critical Healthcare Simulation (TEACH Sim): A Tool for Systematic Simulation Scenario Design. Simul. Healthc. J. Soc. Simul. Healthc. 2015, 10, 21–30. [Google Scholar] [CrossRef]
- Gómez-López, L.; Tena-Blanco, B.; Bergè-Ramos, R.; Coca-Martínez, M.; Forero-Cortés, C.; Gomar-Sancho, C. Nueva plantilla para diseñar escenarios de simulación: Interrelación de elementos en un vistazo. Educ. Méd. 2018, 19, 350–359. [Google Scholar] [CrossRef]
- De Melo, B.C.P.; Falbo, A.R.; Souza, E.S.; Muijtjens, A.M.M.; Van Merriënboer, J.J.G.; Van Der Vleuten, C.P.M. The limited use of instructional design guidelines in healthcare simulation scenarios: An expert appraisal. Adv. Simul. 2022, 7, 30. [Google Scholar] [CrossRef]
- Maestre, J.M.; Sancho, R.; Rábago, J.L.; Martínez, A.; Rojo, E. Diseño y desarrollo de escenarios de simulación clínica: Análisis de cursos para el entrenamiento de anestesiólogos. FEM 2013, 16, 49–57. [Google Scholar] [CrossRef]
- Issenberg, S.B.; Mcgaghie, W.C.; Petrusa, E.R.; Gordon, D.L.; Scalese, R.J. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med. Teach. 2005, 27, 10–28. [Google Scholar] [CrossRef] [PubMed]
- Voyer, S.; Hatala, R. Debriefing and Feedback: Two Sides of the Same Coin? Simul. Healthc. J. Soc. Simul. Healthc. 2015, 10, 67–68. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, T.; Eppich, W.; Brett-Fleegler, M.; Grant, V.; Cheng, A. More Than One Way to Debrief: A Critical Review of Healthcare Simulation Debriefing Methods. Sim. Healthc. 2016, 11, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Capogna, G.; Ingrassia, P.L.; Capogna, E.; Bernardini, M.; Valteroni, E.; Pietrabissa, G.; Nardone, G. Strategic Debriefing for Advanced Simulation; Springer: Berlin/Heidelberg, Germany, 2022. [Google Scholar] [CrossRef]
- Gaba, D.M. Crisis Management in Anesthesia, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2015. [Google Scholar]
- Phillips, E.C.; Smith, S.E.; Tallentire, V.; Blair, S. Systematic review of clinical debriefing tools: Attributes and evidence for use. BMJ Qual. Saf. 2023, 65–87. [Google Scholar] [CrossRef] [PubMed]
- Arriaga, A.F.; Szyld, D.; Pian-Smith, M.C. Real-Time Debriefing After Critical Events. Anesthesiol. Clin. 2020, 38, 801–820. [Google Scholar] [CrossRef] [PubMed]
- Toews, A.J.; Martin, D.E.; Chernomas, W.M. Clinical debriefing: A concept analysis. J. Clin. Nurs. 2021, 30, 1491–1501. [Google Scholar] [CrossRef] [PubMed]
- Twigg, S. Clinical event debriefing: A review of approaches and objectives. Curr. Opin. Pediatr. 2020, 32, 337–342. [Google Scholar] [CrossRef]
- Purdy, E.; Borchert, L.; El-Bitar, A.; Isaacson, W.; Bills, L.; Brazil, V. Taking simulation out of its “safe container”—Exploring the bidirectional impacts of psychological safety and simulation in an emergency department. Adv. Simul. 2022, 7, 1–9. [Google Scholar] [CrossRef]
- Kurup, V.; Matei, V.; Ray, J. Role of in-situ simulation for training in healthcare: Opportunities and challenges. Curr. Opin. Anaesthesiol. 2017, 30, 755–760. [Google Scholar] [CrossRef]
- Wu, Q.; Wang, Y.; Lu, L.; Chen, Y.; Long, H.; Wang, J. Virtual Simulation in Undergraduate Medical Education: A Scoping Review of Recent Practice. Front. Med. 2022, 9, 855403. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.; Grant, V.; Huffman, J.; Burgess, G.; Szyld, D.; Robinson, T.; Eppich, W. Coaching the Debriefer: Peer Coaching to Improve Debriefing Quality in Simulation Programs. Sim. Healthc. 2017, 12, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Ruiz, G.; Maestre, J.M.; Szyld, D.; Del Moral, I.; Rudolph, J.W.; Díaz, G. Sepsis; Springer: New York, NY, USA, 2018; pp. 151–166. [Google Scholar]
- Sackett, D.L.; Rosenberg, W.M.; Gray, J.A.; Haynes, R.B.; Richardson, W.S. Evidence based medicine: What it is and what it isn’t. BMJ 1996, 312, 71–72. [Google Scholar] [CrossRef] [PubMed]
- Leape, L.L.; Berwick, D.M.; Bates, D.W. What Practices Will Most Improve Safety? Evidence-Based Medicine Meets Patient Safety. JAMA 2002, 288, 501. [Google Scholar] [CrossRef] [PubMed]
- Ziv, A.; Wolpe, P.R.; Small, S.D.; Glick, S. Simulation-Based Medical Education: An Ethical Imperative. Simul. Healthc. J. Soc. Simul. Healthc. 2006, 1, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Pope, C.; van Royen, P.; Baker, R. Qualitative methods in research on healthcare quality. Heart 2002, 11, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.B.; Daniel-Underwood, L.; Van Ginkel, C.; Wong, M.; Lee, D.; Lucas, A.S.; Palaganas, J.; Banta, D.; Denmark, T.K.; Clem, K. An educational course including medical simulation for early goal-directed therapy and the severe sepsis resuscitation bundle: An evaluation for medical student training. Resuscitation 2009, 80, 674–679. [Google Scholar] [CrossRef]
- Ottestad, E.; Boulet, J.R.; Lighthall, G.K. Evaluating the management of septic shock using patient simulation. Crit. Care Med. 2007, 35, 769–775. [Google Scholar] [CrossRef]
- Smith, D.; Miller, D.; Cukor, J. Can Simulation Measure Differences in Task-Switching Ability Between Junior and Senior Emergency Medicine Residents? West. J. Emerg. Med. 2016, 17, 149–152. [Google Scholar] [CrossRef]
- Dugan, M.C.; McCracken, C.E.; Hebbar, K.B. Does Simulation Improve Recognition and Management of Pediatric Septic Shock, and If One Simulation Is Good, Is More Simulation Better? Pediatr. Crit. Care Med. 2016, 17, 605–614. [Google Scholar] [CrossRef]
- Palleschi, M.T.; Sirianni, S.; O’Connor, N.; Dunn, D.; Hasenau, S.M. An Interprofessional Process to Improve Early Identification and Treatment for Sepsis. J. Health Qual. 2014, 36, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Edwards, S.; Platt, S.; Lenguerrand, E.; Winter, C.; Mears, J.; Davis, S.; Lucas, G.; Hotton, E.; Fox, R.; Draycott, T.; et al. Effective interprofessional simulation training for medical and midwifery students. BMJ Simul. Technol. Enhanc. Learn. 2015, 1, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Armenia, S.; Thangamathesvaran, L.; Caine, A.D.; King, N.; Kunac, A.; Merchant, A.M. The Role of High-Fidelity Team-Based Simulation in Acute Care Settings: A Systematic Review. Surg. J. 2018, 04, e136–e151. [Google Scholar] [CrossRef] [PubMed]
- Weile, J.; Nebsbjerg, M.A.; Ovesen, S.H.; Paltved, C.; Ingeman, M.L. Simulation-based team training in time-critical clinical presentations in emergency medicine and critical care: A review of the literature. Adv. Simul. 2021, 6, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.H.; Hayes, S.P. Simulation to Manage the Septic Patient in the Intensive Care Unit. Crit. Care Nurs. Clin. North. Am. 2018, 30, 363–377. [Google Scholar] [CrossRef] [PubMed]
- Nishisaki, A.; Hales, R.; Biagas, K.; Cheifetz, I.; Corriveau, C.; Garber, N.; Hunt, E.; Jarrah, R.; McCloskey, J.; Morrison, W.; et al. A multi-institutional high-fidelity simulation “boot camp” orientation and training program for first year pediatric critical care fellows. Pediatr. Crit. Care Med. 2009, 10, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Adler, M.D.; Trainor, J.L.; Siddall, V.J.; McGaghie, W.C. Development and Evaluation of High-Fidelity Simulation Case Scenarios for Pediatric Resident Education. Acad. Pediatr. 2007, 7, 182–186. [Google Scholar] [CrossRef]
- Jenkins, Z.; Laswell, E.; Stute, N. WITHDRAWN: Evaluation of a sepsis teaching rounds simulation for pharmacy students. Curr. Pharm. Teach. Learn. 2019, 11, 936–942. [Google Scholar] [CrossRef]
- Storey, A.; White, K.; Treder, K.; Woodhams, E.; Bell, S.; Cannon, R. First-Trimester Abortion Complications: Simulation Cases for OB/GYN Residents in Sepsis and Hemorrhage. Mededportal 2020, 16, 10995. [Google Scholar] [CrossRef]
- Webb, T.T.; Boyer, T.J.; Mitchell, S.A.; Eddy, C. Intraoperative Sepsis: A Simulation Case for Anesthesiology Residents. MedEdPORTAL 2020, 16, 10886. [Google Scholar] [CrossRef]
- Weil, J.; Cassara, M. Occult Sepsis Masked by Trauma—Exploration of Cognitive Biases Through Simulation with Emergency Medicine Residents. MedEdPORTAL 2020, 16. [Google Scholar] [CrossRef] [PubMed]
- Diaz, D.A.; Anderson, M.; Quelly, S.B.; Clark, K.D.; Talbert, S. Early Recognition of Pediatric Sepsis Simulation Checklist—An Exploratory Study. J. Pediatr. Nurs. 2019, 50, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Anderson, N.B.; Chan, M.-K.; Gutierrez, C.; Kambestad, K.; Walker, V. Identification and Management of Pediatric Sepsis: A Medical Student Curricular Supplement for PICU and NICU Rotations. MedEdPORTAL 2021, 17, 11142. [Google Scholar] [CrossRef] [PubMed]
- Mihaljevic, S.E.D.; Howard, V.M.E. Incorporating Interprofessional Evidenced-Based Sepsis Simulation Education for Certified Nursing Assistants (CNAs) and Licensed Care Providers Within Long-term Care Settings for Process and Quality Improvement. Crit. Care Nurs. Q. 2016, 39, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Ros, N.; Alegre, F.; Huerta, A.; Gil-Alzugaray, B.; Landecho, M.F.; García, N.; Quiroga, J.; Lucena, J.F.M. Acquiring sepsis competencies through simulation-based learning bundle during intermediate care unit internship. Medicine 2021, 100, e24483. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.; Bekiaris, B.; Hansen, G. Mobile emergency simulation training for rural health providers. Rural. Remote. Heal. 2017, 17, 4057. [Google Scholar] [CrossRef] [PubMed]
- Powell, E.S.M.; Bond, W.F.; Barker, L.T.; Cooley, K.R.; Lee, J.; Vincent, A.L.D.; Vozenilek, J.A. In Situ Simulation for Adoption of New Technology to Improve Sepsis Care in Rural Emergency Departments. J. Patient Saf. 2022, 18, 302–309. [Google Scholar] [CrossRef]
- Steiner, M.; Langgartner, M.; Cardona, F.; Waldhör, T.; Schwindt, J.; Haiden, N.; Berger, A. Significant Reduction of Catheter-associated Blood Stream Infections in Preterm Neonates After Implementation of a Care Bundle Focusing on Simulation Training of Central Line Insertion. Pediatr. Infect. Dis. J. 2015, 34, 1193–1196. [Google Scholar] [CrossRef]
- Tofil, N.M.; Lin, Y.; Zhong, J.; Peterson, D.T.; White, M.L.; Grant, V.; Grant, D.J.; Gottesman, R.; Sudikoff, S.N.; Adler, M.; et al. Workload of Team Leaders and Team Members During a Simulated Sepsis Scenario. Pediatr. Crit. Care Med. 2017, 18, e423–e427. [Google Scholar] [CrossRef]
- Meurling, L.; Hedman, L.; Lidefelt, K.-J.; Escher, C.; Felländer-Tsai, L.; Wallin, C.-J. Comparison of high- and low equipment fidelity during paediatric simulation team training: A case control study. BMC Med. Educ. 2014, 14, 221. [Google Scholar] [CrossRef]
- Englert, N.C.; McDermott, D. Back to Fundamentals: Using High- and Low-Fidelity Simulation to Provide Reinforcement of Preventative Measures for Sepsis. Crit. Care Nurs. Q. 2016, 39, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Chua, W.L.; Ooi, S.L.; Chan, G.W.H.; Lau, T.C.; Liaw, S.Y. The Effect of a Sepsis Interprofessional Education Using Virtual Patient Telesimulation on Sepsis Team Care in Clinical Practice: Mixed Methods Study. J. Med. Internet Res. 2022, 24, e35058. [Google Scholar] [CrossRef] [PubMed]
- Toto, R.L.; Vorel, E.S.; Tay, K.-Y.; Good, G.L.; Berdinka, J.M.; Peled, A.; Leary, M.; Chang, T.P.; Weiss, A.K.; Balamuth, F.B. Augmented Reality in Pediatric Septic Shock Simulation: Randomized Controlled Feasibility Trial. JMIR Med. Educ. 2021, 7, e29899. [Google Scholar] [CrossRef] [PubMed]
- McNaughten, B.; Storey, L.; Corkin, D.; Cardwell, P.; Thompson, A.; Bourke, T.; O’Donoghue, D. Familiarity with the clinical environment, achieved by priming, improves time to antibiotic administration in a simulated paediatric sepsis scenario: A randomised control trial. Arch. Dis. Child. 2020, 106, 467–469. [Google Scholar] [CrossRef] [PubMed]
- Geis, G.L.; Wheeler, D.S.; Bunger, A.; Militello, L.G.; Taylor, R.G.; Bauer, J.P.; Byczkowski, T.L.; Kerrey, B.T.; Patterson, M.D. A Validation Argument for a Simulation-Based Training Course Centered on Assessment, Recognition, and Early Management of Pediatric Sepsis. Simul. Heal. J. Soc. Simul. Health 2018, 13, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Hunt, E.A.; Duval-Arnould, J.M.; Nelson-McMillan, K.L.; Bradshaw, J.H.; Diener-West, M.; Perretta, J.S.; Shilkofski, N.A. Pediatric resident resuscitation skills improve after “Rapid Cycle Deliberate Practice” training. Resuscitation 2014, 85, 945–951. [Google Scholar] [CrossRef] [PubMed]
- Aponte-Patel, L.; Salavitabar, A.; Fazzio, P.; Geneslaw, A.S.; Good, P.; Sen, A.I. Implementation of a Formal Debriefing Program After Pediatric Rapid Response Team Activations. J. Grad. Med. Educ. 2018, 10, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Galligan, M.M.; Wolfe, H.A.; Papili, K.E.; Porter, E.; O’shea, K.; Liu, H.; Colfer, A.; Neiswender, K.; Granahan, K.; McGowan, N.; et al. Implementation of a Multidisciplinary Debriefing Process for Pediatric Ward Deterioration Events. Hosp. Pediatr. 2021, 11, 454–461. [Google Scholar] [CrossRef]
- Berchtenbreiter, K.; Innes, K.; Watterson, J.; Nickson, C.P.; Wong, P. Intensive care unit nurses’ perceptions of debriefing after critical incidents: A qualitative descriptive study. Aust. Crit. Care 2023. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuesta-Montero, P.; Navarro-Martínez, J.; Yedro, M.; Galiana-Ivars, M. Sepsis and Clinical Simulation: What Is New? (and Old). J. Pers. Med. 2023, 13, 1475. https://doi.org/10.3390/jpm13101475
Cuesta-Montero P, Navarro-Martínez J, Yedro M, Galiana-Ivars M. Sepsis and Clinical Simulation: What Is New? (and Old). Journal of Personalized Medicine. 2023; 13(10):1475. https://doi.org/10.3390/jpm13101475
Chicago/Turabian StyleCuesta-Montero, Pablo, Jose Navarro-Martínez, Melina Yedro, and María Galiana-Ivars. 2023. "Sepsis and Clinical Simulation: What Is New? (and Old)" Journal of Personalized Medicine 13, no. 10: 1475. https://doi.org/10.3390/jpm13101475
APA StyleCuesta-Montero, P., Navarro-Martínez, J., Yedro, M., & Galiana-Ivars, M. (2023). Sepsis and Clinical Simulation: What Is New? (and Old). Journal of Personalized Medicine, 13(10), 1475. https://doi.org/10.3390/jpm13101475