Personalized Treatment Decisions for Traumatic Proximal Finger Amputations: A Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
Statistics
3. Results
3.1. Patient Demographics
3.2. DASH Scores Indicate Higher Reported Quality of Life Following Ray Amputations
3.3. Diverse Functional Outcomes Following Ray Amputation
3.4. Higher Cosmesis Following Ray Amputation
3.5. No Significant Changes in the Affected Hands’ Circulation
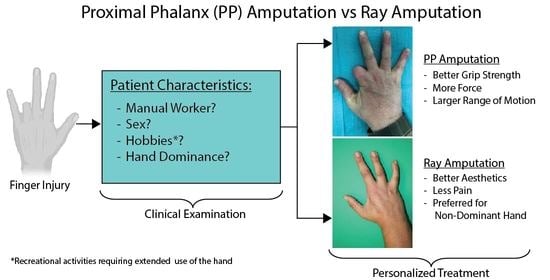
3.6. Flow Chart for Clinical Decision-Making between Ray and Proximal Phalanx Amputations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Conn, J.M.; Annest, J.L.; Ryan, G.W.; Budnitz, D.S. Non–work-related finger amputations in the United States, 2001–2002. Ann. Emerg. Med. 2005, 45, 630–635. [Google Scholar] [CrossRef] [PubMed]
- Reid, D.B.; Shah, K.N.; Eltorai, A.E.; Got, C.C.; Daniels, A.H. Epidemiology of finger amputations in the United States from 1997 to 2016. J. Hand Surg. Glob. Online 2019, 1, 45–51. [Google Scholar] [CrossRef] [Green Version]
- Arazpour, M.; Mardani, M.A.; Bahramizadeh, M.; Layeghi, F.; Zarezadeh, F.; Curran, S. The effect of new method of suspension on quality of life, satisfaction, and suspension in patients with finger prostheses. Prosthet. Orthot. Int. 2015, 39, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Azmat, C.E.; Buckley, C.J. Digit Amputation; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Degreef, I.; De Smet, L. Dupuytren’s disease: A predominant reason for elective finger amputation in adults. Acta Chir. Belg. 2009, 109, 494–497. [Google Scholar] [CrossRef]
- Reavey, P.L.; Stranix, J.T.; Muresan, H.; Soares, M.; Thanik, V. Disappearing digits: Analysis of national trends in amputation and replantation in the United States. Plast. Reconstr. Surg. 2018, 141, 857e–867e. [Google Scholar] [CrossRef]
- Bhat, A.K.; Acharya, A.M.; Narayanakurup, J.; Kumar, B.; Nagpal, P.; Kamath, A. Functional and cosmetic outcome of single-digit ray amputation in hand. Musculoskelet. Surg. 2017, 101, 275–281. [Google Scholar] [CrossRef]
- Schieber, M.H. Motor cortex and the distributed anatomy of finger movements. In Sensorimotor Control of Movement and Posture; Springer: Berlin/Heidelberg, Germany, 2002; pp. 411–416. [Google Scholar]
- Ding, I., Jr.; Zheng, N.-W.; Hsieh, M.-C. Hand gesture intention-based identity recognition using various recognition strategies incorporated with VGG convolution neural network-extracted deep learning features. J. Intell. Fuzzy Syst. 2021, 40, 7775–7788. [Google Scholar] [CrossRef]
- McNeill, D. Why We Gesture: The Surprising Role of Hand Movements in Communication; Cambridge University Press: Cambridge, UK, 2016. [Google Scholar]
- Skoff, H.; Skoff, H. The psychological and somatic consequences of digital amputation. Plast. Reconstr. Surg. Glob. Open 2022, 10, e4387. [Google Scholar] [CrossRef]
- Filippo, C.; Margherita, M.; Alessandro, N.; Cristina, G.; Francesco, P.; Francesco, C. Single ray amputation in traumatic injury of the hand: Review of literature. Acta Bio Med. Atenei Parm. 2019, 90, 14. [Google Scholar]
- Blazar, P.E.; Garon, M.T. Ray resections of the fingers: Indications, techniques, and outcomes. J. Am. Acad. Orthop. Surg. 2015, 23, 476–484. [Google Scholar] [CrossRef]
- Pedrazzini, A.; Calderazzi, F.; Bertoni, N.; Ceccarelli, F. Cosmetic amputation of the fourth ray as possible outcome of the traumatic amputation of the ring finger injury: A case report. Acta Biomed. 2008, 79, 227–232. [Google Scholar]
- Chase, R.A. Functional levels of amputation in the hand. Surg. Clin. North Am. 1960, 40, 415–423. [Google Scholar] [CrossRef]
- Lyall, H.; Elliot, D. Total middle ray amputation. J. Hand Surg. Br. Eur. Vol. 1996, 21, 675–680. [Google Scholar] [CrossRef]
- Elmaraghi, S.; Albano, N.J.; Israel, J.S.; Michelotti, B.F. Targeted muscle reinnervation in the hand: Treatment and prevention of pain after ray amputation. J. Hand Surg. 2020, 45, 884.e1–884.e6. [Google Scholar] [CrossRef]
- Karle, B.; Wittemann, M.; Germann, G. Functional outcome and quality of life after ray amputation versus amputation through the proximal phalanx of the index finger. Handchir. Mikrochir. Plast. Chir. 2002, 34, 30–35. [Google Scholar] [CrossRef]
- Nuzumlali, E.; Orhun, E.; Öztürk, K.; Cepel, S.; Polatkan, S. Results of ray resection and amputation for ring avulsion injuries at the proximal interphalangeal joint. J. Hand Surg. 2003, 28, 578–581. [Google Scholar] [CrossRef]
- Boström, K.J.; de Lussanet, M.H.; Weiss, T.; Puta, C.; Wagner, H. A computational model unifies apparently contradictory findings concerning phantom pain. Sci. Rep. 2014, 4, 5298. [Google Scholar] [CrossRef] [Green Version]
- Hazari, A.; Elliot, D. Treatment of end-neuromas, neuromas-in-continuity and scarred nerves of the digits by proximal relocation. J. Hand Surg. 2004, 29, 338–350. [Google Scholar] [CrossRef]
- Yuan, F.; McGlinn, E.P.; Giladi, A.M.; Chung, K.C. A systematic review of outcomes after revision amputation for treatment of traumatic finger amputation. Plast. Reconstr. Surg. 2015, 136, 99. [Google Scholar] [CrossRef] [Green Version]
- Murray, J.; Carman, W.; MacKenzie, J. Transmetacarpal amputation of the index finger: A clinical assessment of hand strength and complications. J. Hand Surg. 1977, 2, 471–481. [Google Scholar] [CrossRef]
- Bosmans, J.C.; Geertzen, J.H.; Post, W.J.; van der Schans, C.P.; Dijkstra, P.U. Factors associated with phantom limb pain: A 3½-year prospective study. Clin. Rehabil. 2010, 24, 444–453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Melikyan, E.; Beg, M.; Woodbridge, S.; Burke, F. The functional results of ray amputation. Hand Surg. 2003, 8, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Collar III, J.; Smetona, J.; Zhang, J.; Deng, Y.; Clune, J. The Aesthetics of Digit Amputation. HAND 2022, 15589447211065073. [Google Scholar] [CrossRef] [PubMed]
- Gong, H.S.; Shin, S.; Baek, G. Creation of a “dorsal transverse intermetacarpal ligament” to prevent scissoring deformity in central ray amputation. J. Hand Surg. 2008, 33, 163–165. [Google Scholar] [CrossRef]
- Monreal, R. Reconstructive surgery of the amputated ring finger. Int. Orthop. 2017, 41, 1617–1622. [Google Scholar] [CrossRef]
- Shauver, M.J.; Nishizuka, T.; Hirata, H.; Chung, K.C. Traumatic finger amputation treatment preference among hand surgeons in the US and Japan. Plast. Reconstr. Surg. 2016, 137, 1193. [Google Scholar] [CrossRef]
- Szabo, D.; Ujică, A.; Ursu, O. Testing the eye-hand coordination and reaction speed in children aged between 10–14 years old. Geosport Soc. 2021, 15, 110–121. [Google Scholar] [CrossRef]
- MacKay, B.; Wall, H.; Weaver, A.; Sexson, T.; Wall, J.; Blue, M.; Doughty, M. A novel approach to ray resection of the hand. J. Hand Surg. Glob. Online 2020, 2, 46–54. [Google Scholar] [CrossRef]
- Kuret, Z.; Burger, H.; Vidmar, G.; Maver, T. Adjustment to finger amputation and silicone finger prosthesis use. Disabil. Rehabil. 2019, 41, 1307–1312. [Google Scholar] [CrossRef]


| Characteristic | Total (n = 40) | Ray Amputation (n = 20) | Proximal Phalanx Amputation (n = 20) |
|---|---|---|---|
| Age (years) | |||
| Mean | 47.5 | 49.5 | 45.5 |
| Gender: | |||
| Female | 17 (42.5%) | 12 (60%) | 5 (25%) |
| Male | 23 (57.5%) | 8 (40%) | 15 (75%) |
| Hand dominance: | |||
| Dominant | 13 (32.5%) | 7 (35%) | 6 (30%) |
| Non-dominant | 27 (67.5%) | 13 (65%) | 14 (70%) |
| Affected finger: | |||
| Digitus 2 | 17 (42.5%) | 8 (40%) | 9 (45%) |
| Digitus 3 | 6 (15%) | 2 (10%) | 4 (20%) |
| Digitus 4 | 13 (32.5%) | 7 (35%) | 6 (30%) |
| Digitus 5 | 4 (10%) | 3 (15%) | 1 (5%) |
| Mean ± SEM | p-Value | ||
|---|---|---|---|
| Ray Amputation | Proximal Phalanx Amputation | ||
| DASH score | 33.88 ± 2.786 | 50.13 ± 3.625 | 0.001 |
| PRWE score | 10.11 ± 1.772 | 24.11 ± 4.692 | 0.0170 |
| EQ-5D-5L score | 0.8962 ± 0.0262 | 0.8804 ± 0.0270 | 0.6420 |
| EQ-VAS score | 82.89 ± 4.297 | 72.37 ± 3.253 | 0.0419 |
| Characteristic | Mean ± SEM | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Part A | Part B | Part C | |||||||
| Type of employment | RA | PPA | p | RA | PPA | p | RA | PPA | p |
| Manual worker | 32.78 ± 3.281 | 46.62 ± 3.327 | 0.0413 | 33.28 ± 2.310 | 36.22 ± 5.028 | 0.9888 | 26.95 ± 3.966 | 46.43 ± 2.203 | 0.0016 |
| Non-manual worker | 27.90 ± 3.828 | 40.13 ± 6.344 | 0.2923 | 39.47 ± 2.016 | 34.74 ± 3.454 | 0.9595 | 25.40 ± 3.031 | 41.80 ± 4.169 | 0.0721 |
| Sex | |||||||||
| Female | 35.47 ± 2.934 | 48.68 ± 2.753 | 0.0038 | 43.90 ± 1.285 | 43.95 ± 2.936 | 0.999 | 27.39 ± 1.952 | 50.78 ± 2.657 | 0.0001 |
| Male | 37.58 ± 2.534 | 47.54 ± 2.384 | 0.0417 | 44.33 ± 2.642 | 44.95 ± 3.223 | 0.999 | 50.84 ± 3.311 | 51.78 ± 2.557 | 0.999 |
| Affected hand | |||||||||
| Dominant | 26.24 ± 2.091 | 43.47 ± 3.660 | 0.0442 | 41.13 ± 3.970 | 29.74 ± 3.965 | 0.4584 | 37.10 ± 5.869 | 43.47 ± 5.633 | 0.9052 |
| Non-dominant | 32.78 ± 3.281 | 41.48 ± 3.645 | 0.4923 | 31.89 ± 2.787 | 39.89 ± 3.979 | 0.5844 | 28.01 ± 3.890 | 42.11 ± 3.147 | 0.0574 |
| Mean ± SEM | p-Value | ||
|---|---|---|---|
| Ray Amputation | Proximal Phalanx Amputation | ||
| Numeric Pain Rating | |||
| At rest | 1.474 ± 0.2212 | 2.684 ± 0.3672 | 0.0022 |
| At motion | 2.632 ± 0.2883 | 3.947 ± 0.5269 | 0.0094 |
| Grip strength (%) | 68.09 ± 3.026 | 89.74 ± 5.213 | 0.0449 |
| Wrist range of motion (%) | 85 | 100 | . |
| Cold sensitivity (%) | 42 | 75 | |
| Aesthetics (%) | |||
| Excellent | 65 | 30 | |
| Good | 32.5 | 60 | |
| Unsatisfactory | 2.5 | 10 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dastagir, N.; Obed, D.; Dastagir, K.; Vogt, P.M. Personalized Treatment Decisions for Traumatic Proximal Finger Amputations: A Retrospective Cohort Study. J. Pers. Med. 2023, 13, 215. https://doi.org/10.3390/jpm13020215
Dastagir N, Obed D, Dastagir K, Vogt PM. Personalized Treatment Decisions for Traumatic Proximal Finger Amputations: A Retrospective Cohort Study. Journal of Personalized Medicine. 2023; 13(2):215. https://doi.org/10.3390/jpm13020215
Chicago/Turabian StyleDastagir, Nadjib, Doha Obed, Khaled Dastagir, and Peter M. Vogt. 2023. "Personalized Treatment Decisions for Traumatic Proximal Finger Amputations: A Retrospective Cohort Study" Journal of Personalized Medicine 13, no. 2: 215. https://doi.org/10.3390/jpm13020215
APA StyleDastagir, N., Obed, D., Dastagir, K., & Vogt, P. M. (2023). Personalized Treatment Decisions for Traumatic Proximal Finger Amputations: A Retrospective Cohort Study. Journal of Personalized Medicine, 13(2), 215. https://doi.org/10.3390/jpm13020215