Seasonal Stability of SARS-CoV-2 in Biological Fluids
Abstract
:1. Introduction
2. Results
3. Discussion
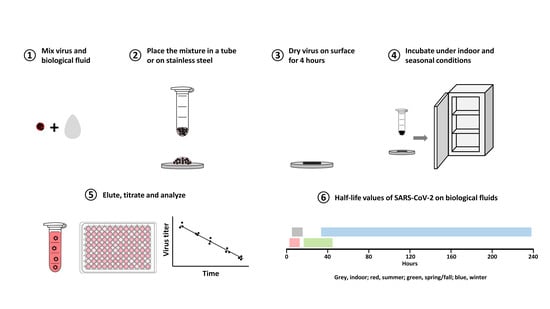
4. Materials and Methods
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclaimer
References
- World Health Organization. Transmission of SARSCoV-2: Implications for Infection Prevention Precautions: Scientific Brief. Available online: https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions (accessed on 9 July 2020).
- Atkinson, J.; Chartier, Y.; Pessoa-Silva, C.L.; Jensen, P.; Li, Y.; Seto, W.H. Natural Ventilation for Infection Control in Health-Care Settings; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Kwon, T.; Gaudreault, N.; Richt, J. Environmental Stability of SARS-CoV-2 on Different Types of Surfaces under Indoor and Seasonal Climate Conditions. Pathogens 2021, 10, 227. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Bushmaker, T.; Lloyd-Smith, J.O.; De Wit, E.; Munster, V.J.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef]
- Colavita, F.; Lapa, D.; Carletti, F.; Lalle, E.; Bordi, L.; Marsella, P.; Nicastri, E.; Bevilacqua, N.; Giancola, M.L.; Corpolongo, A.; et al. SARS-CoV-2 Isolation From Ocular Secretions of a Patient With COVID-19 in Italy With Prolonged Viral RNA Detection. Ann. Intern. Med. 2020, 173, 242–243. [Google Scholar] [CrossRef]
- Sun, J.; Zhu, A.; Li, H.; Zheng, K.; Zhuang, Z.; Chen, Z.; Shi, Y.; Zhang, Z.; Chen, S.-B.; Liu, X.; et al. Isolation of infectious SARS-CoV-2 from urine of a COVID-19 patient. Emerg. Microbes Infect. 2020, 9, 991–993. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Xu, Y.; Gao, R.; Lu, R.; Han, K.; Wu, G.; Tan, W. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA 2020, 323, 1843–1844. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiao, F.; Sun, J.; Xu, Y.; Li, F.; Huang, X.; Li, H.; Zhao, J.; Huang, J.; Zhao, J. Infectious SARS-CoV-2 in Feces of Patient with Severe COVID-19. Emerg. Infect. Dis. 2020, 26, 1920–1922. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chen, C.; Zhu, S.; Shu, C.; Wang, D.; Song, J.; Song, Y.; Zhen, W.; Feng, Z.; Wu, G.; et al. Isolation of 2019-nCoV from a Stool Specimen of a Laboratory-Confirmed Case of the Coronavirus Disease 2019 (COVID-19). China CDC Wkly. 2020, 2, 123–124. [Google Scholar] [CrossRef]
- Prebensen, C.; Hre, P.L.M.; Jonassen, C.; Rangberg, A.; Blomfeldt, A.; Svensson, M.; Omland, T.; Berdal, J.E. SARS-CoV-2 RNA in plasma is associated with ICU admission and mortality in patients hospitalized with COVID-19. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Pham, T.D.; Huang, C.; Wirz, O.F.; Röltgen, K.; Sahoo, M.K.; Layon, M.A.; Pandey, S.; Foung, S.K.; Boyd, S.D.; Pinsky, B.A. SARS-CoV-2 RNAemia in a Healthy Blood Donor 40 Days After Respiratory Illness Resolution. Ann. Intern. Med. 2020, 173, 853–854. [Google Scholar] [CrossRef] [PubMed]
- Groß, R.; Conzelmann, C.; Müller, A.J.; Stenger, S.; Steinhart, K.; Kirchhoff, F.; Münch, J. Detection of SARS-CoV-2 in human breastmilk. Lancet 2020, 395, 1757–1758. [Google Scholar] [CrossRef]
- Costa, S.; Posteraro, B.; Marchetti, S.; Tamburrini, E.; Carducci, B.; Lanzone, A.; Valentini, P.; Buonsenso, D.; Sanguinetti, M.; Vento, G.; et al. Excretion of SARS-CoV-2 in human breast milk. Clin. Microbiol. Infect. 2020, 26, 1430–1432. [Google Scholar] [CrossRef]
- Li, D.; Jin, M.; Bao, P.; Zhao, W.; Zhang, S. Clinical Characteristics and Results of Semen Tests Among Men with Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e208292. [Google Scholar] [CrossRef] [PubMed]
- Chin, A.W.H.; Chu, J.T.S.; Perera, A.M.R.; Hui, K.P.Y.; Yen, H.-L.; Chan, M.C.W.; Peiris, M.; Poon, L.L.M. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe 2020, 1, e10. [Google Scholar] [CrossRef]
- Pastorino, B.; Touret, F.; Gilles, M.; De Lamballerie, X.; Charrel, R.N. Prolonged Infectivity of SARS-CoV-2 in Fomites. Emerg. Infect. Dis. 2020, 26, 2256–2257. [Google Scholar] [CrossRef] [PubMed]
- Riddell, S.; Goldie, S.; Hill, A.; Eagles, D.; Drew, T.W. The effect of temperature on persistence of SARS-CoV-2 on common surfaces. Virol. J. 2020, 17, 1–7. [Google Scholar] [CrossRef]
- Matson, M.J.; Yinda, C.K.; Seifert, S.N.; Bushmaker, T.; Fischer, R.J.; Van Doremalen, N.; Lloyd-Smith, J.O.; Munster, V.J. Effect of Environmental Conditions on SARS-CoV-2 Stability in Human Nasal Mucus and Sputum. Emerg. Infect. Dis. 2020, 26, 2276–2278. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Li, T.; Deng, Y.; Liu, S.; Zhang, D.; Li, H.; Wang, X.; Jia, L.; Han, J.; Bei, Z.; et al. Stability of SARS-CoV-2 on envi-ronmental surfaces and in human excreta. J. Hosp. Infect. 2020. [Google Scholar] [CrossRef]
- Hui, K.P.Y.; Cheung, M.-C.; Perera, R.A.P.M.; Ng, K.-C.; Bui, C.H.T.; Ho, J.C.W.; Ng, M.M.T.; Kuok, D.I.T.; Shih, K.C.; Tsao, S.-W.; et al. Tropism, replication competence, and innate immune responses of the coronavirus SARS-CoV-2 in human respiratory tract and conjunctiva: An analysis in ex-vivo and in-vitro cultures. Lancet Respir. Med. 2020, 8, 687–695. [Google Scholar] [CrossRef]
- Guemes-Villahoz, N.; Burgos-Blasco, B.; Arribi-Vilela, A.; Arriola-Villalobos, P.; Rico-Luna, C.M.; Cuina-Sardina, R.; Delga-do-Iribarren, A.; Garcia-Feijoo, J. Detecting SARS-CoV-2 RNA in conjunctival secretions: Is it a valuable diagnostic method of COVID-19? J. Med. Virol. 2020. [Google Scholar] [CrossRef]
- Xia, J.; Tong, J.; Liu, M.; Shen, Y.; Guo, D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J. Med. Virol. 2020, 92, 589–594. [Google Scholar] [CrossRef] [Green Version]
- McDermott, A.M. Antimicrobial compounds in tears. Exp. Eye Res. 2013, 117, 53–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lang, J.; Yang, N.; Deng, J.; Liu, K.; Yang, P.; Zhang, G.; Jiang, C. Inhibition of SARS Pseudovirus Cell Entry by Lactoferrin Binding to Heparan Sulfate Proteoglycans. PLoS ONE 2011, 6, e23710. [Google Scholar] [CrossRef] [PubMed]
- Clausen, T.M.; Sandoval, D.R.; Spliid, C.B.; Pihl, J.; Perrett, H.R.; Painter, C.D.; Narayanan, A.; Majowicz, S.A.; Kwong, E.M.; McVicar, R.N.; et al. SARS-CoV-2 Infection Depends on Cellular Heparan Sulfate and ACE2. Cell 2020, 183, 1043–1057.e15. [Google Scholar] [CrossRef] [PubMed]
- Bivins, A.; Greaves, J.; Fischer, R.; Yinda, K.C.; Ahmed, W.; Kitajima, M.; Munster, V.J.; Bibby, K. Persistence of SARS-CoV-2 in Water and Wastewater. Environ. Sci. Technol. Lett. 2020, 7, 937–942. [Google Scholar] [CrossRef]
- Hogan, C.A.; Stevens, B.A.; Sahoo, M.K.; Huang, C.; Garamani, N.; Gombar, S.; Yamamoto, F.; Murugesan, K.; Kurzer, J.; Zehnder, J.; et al. High Frequency of SARS-CoV-2 RNAemia and Association With Severe Disease. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Bermejo-Martin, J.F.; González-Rivera, M.; Almansa, R.; Micheloud, D.; Tedim, A.P.; Domínguez-Gil, M.; Resino, S.; Martín-Fernández, M.; Murua, P.R.; Pérez-García, F.; et al. Viral RNA load in plasma is associated with critical illness and a dysregulated host response in COVID-19. Crit. Care 2020, 24, 1–13. [Google Scholar] [CrossRef]
- Cho, H.J.; Koo, J.W.; Roh, S.K.; Kim, Y.K.; Suh, J.S.; Moon, J.H.; Sohn, S.K.; Baek, D.W. COVID-19 transmission and blood transfusion: A case report. J. Infect. Public Health 2020, 13, 1678–1679. [Google Scholar] [CrossRef]
- Owen, D.H. A Review of the Physical and Chemical Properties of Human Semen and the Formulation of a Semen Simulant. J. Androl. 2005, 26, 459–469. [Google Scholar] [CrossRef] [Green Version]
- Klebanoff, S.J.; Kazazi, F. Inactivation of human immunodeficiency virus type 1 by the amine oxidase-peroxidase system. J. Clin. Microbiol. 1995, 33, 2054–2057. [Google Scholar] [CrossRef] [Green Version]
- Martellini, J.A.; Cole, A.L.; Venkataraman, N.; Quinn, G.A.; Svoboda, P.; Gangrade, B.K.; Pohl, J.; Sørensen, O.E.; Cole, A.M. Cationic polypeptides contribute to the anti-HIV-1 activity of human seminal plasma. FASEB J. 2009, 23, 3609–3618. [Google Scholar] [CrossRef] [Green Version]
- Bertino, E.; Moro, G.E.; De Renzi, G.; Viberti, G.; Cavallo, R.; Coscia, A.; Rubino, C.; Tonetto, P.; Sottemano, S.; Campagnoli, M.F.; et al. Detection of SARS-CoV-2 in Milk From COVID-19 Positive Mothers and Follow-Up of Their Infants. Front. Pediatr. 2020, 8, 597699. [Google Scholar] [CrossRef] [PubMed]
- Chambers, C.; Krogstad, P.; Bertrand, K.; Contreras, D.; Tobin, N.H.; Bode, L.; Aldrovandi, G. Evaluation for SARS-CoV-2 in Breast Milk From 18 Infected Women. JAMA 2020, 324, 1347. [Google Scholar] [CrossRef] [PubMed]
- Conzelmann, C.; Zou, M.; Groß, R.; Harms, M.; Röcker, A.; Riedel, C.U.; Münch, J.; Müller, J.A. Storage-Dependent Generation of Potent Anti-ZIKV Activity in Human Breast Milk. Viruses 2019, 11, 591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pfaender, S.; Heyden, J.; Friesland, M.; Ciesek, S.; Ejaz, A.; Steinmann, J.; Steinmann, J.; Malarski, A.; Stoiber, H.; Tsiavaliaris, G.; et al. Inactivation of Hepatitis C Virus Infectivity by Human Breast Milk. J. Infect. Dis. 2013, 208, 1943–1952. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Environmental Condition | 21 °C/60% RH Indoor | 25 °C/70% RH Summer | 13 °C/66% RH Spring/Fall | 5 °C/75% RH Winter | ||||
|---|---|---|---|---|---|---|---|---|
| Setting | Liquid | Surface | Liquid | Surface | Liquid | Surface | Liquid | Surface |
| Nasal mucus | 5.23 (4.03, 7.47) 1 | 6.77 (4.57, 13.01) | 4.59 2 (3.66, 6.17) | 2.58 2 (2.02, 3.59) | 21.74 (15.61, 35.76) | 18.15 (14.66, 23.83) | 53.94 (44.82, 67.71) | 38.55 (30.42, 52.62) |
| Sputum | 8.69 2 (7.11, 11.17) | 14.9 2 (10.72, 24.37) | 3.68 (2.59, 6.37) | 5.55 (4.42, 7.45) | 21.94 2 (16.05, 34.66) | 37.03 2 (27.74, 55.67) | 33.37 2 (22.75, 62.56) | 76.4 2 (60.48, 103.7) |
| Saliva | 7.89 2 (6.38, 10.37) | 12.69 2 (10.36, 16.38) | 6.98 (5.19, 10.65) | 6.44 (4.87, 9.5) | 15.98 2 (12.51, 22.12) | 34.17 2 (27.05, 46.28) | 55.16 (44.28, 73.15) | 69.25 (61.3, 79.57) |
| Tears | 15.1 2 (12.29, 19.56) | 8.3 2 (7.09, 10) | 11.06 2 (8.91, 14.58) | 3.53 2 (2.93, 4.45) | 29.34 (25.75, 34.07) | 24.22 (20.14, 30.38) | 121.83 (91.19, 183.44) | 106.82 (84.44, 145.43) |
| Urine | 11.41 (9.69, 13.88) | N/A 3 | 7.89 (6.74, 9.5) | N/A 3 | 54.34 (36.76, 103.8) | N/A 3 | 57.73 (49.06, 70.15) | N/A 3 |
| Blood | 16.74 (11.64, 29.83) | 16.57 (13.1, 22.53) | 12.57 (9.58, 18.3) | 10.75 (9.16, 13) | 39.25 (28.03, 65.26) | 48.4 (35.79, 74.6) | 102.04 2 (71.93, 175.63) | 235.18 2 (144.52, 631.75) |
| Semen | 7.48 (5.76, 10.65) | 9.51 (7.46, 13.1) | 2.3 2 (1.75, 3.33) | 5.9 2 (4.75, 7.78) | 17.69 2 (13.96, 24.14) | 41.24 2 (29.31, 69.31) | 57.81 2 (47.77, 73.23) | 91.64 2 (75.24, 117.22) |
| Positive control | 15.85 2 (11.81, 24.12) | 7.88 2 (6.48, 10.05) | 7.48 2 (6.7, 8.46) | 2.57 2 (2.21, 3.08) | 48.95 2 (35.25, 80) | 21.5 2 (17.25, 28.56) | 176.66 2 (109.78, 451.39) | 79.64 2 (63.6, 106.48) |
| Environmental Condition | 21 °C/60% RH/Indoor, 25 °C/70% RH/Summer | 13 °C/66% RH/Spring/Fall | 5 °C/75% RH/Winter |
|---|---|---|---|
| Liquid setting | 1 h post-contamination (hpc), 7 hpc, 1 day post-contamination (dpc), 2 dpc, and 3 dpc | 1 hpc, 1 dpc, 3 dpc, 5 dpc, and 7 dpc | 1 hpc, 1 dpc, 3 dpc, 6 dpc, 10 dpc, 15 dpc, and 21 dpc |
| Surface setting | 4 hpc, 8 hpc, 1 dpc, 2 dpc, and 3 dpc | 4 hpc, 1 dpc, 3 dpc, 5 dpc, and 7 dpc | 4 hpc, 1 dpc, 3 dpc, 6 dpc, 10 dpc, 15 dpc, and 21 dpc |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, T.; Gaudreault, N.N.; Richt, J.A. Seasonal Stability of SARS-CoV-2 in Biological Fluids. Pathogens 2021, 10, 540. https://doi.org/10.3390/pathogens10050540
Kwon T, Gaudreault NN, Richt JA. Seasonal Stability of SARS-CoV-2 in Biological Fluids. Pathogens. 2021; 10(5):540. https://doi.org/10.3390/pathogens10050540
Chicago/Turabian StyleKwon, Taeyong, Natasha N. Gaudreault, and Juergen A. Richt. 2021. "Seasonal Stability of SARS-CoV-2 in Biological Fluids" Pathogens 10, no. 5: 540. https://doi.org/10.3390/pathogens10050540
APA StyleKwon, T., Gaudreault, N. N., & Richt, J. A. (2021). Seasonal Stability of SARS-CoV-2 in Biological Fluids. Pathogens, 10(5), 540. https://doi.org/10.3390/pathogens10050540